Risk Categories in COVID-19 Based on Degrees of Inflammation: Data on More Than 17,000 Patients from the Spanish SEMI-COVID-19 Registry
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Patient Selection, and Data Collection
2.2. Categories of Risk
2.3. Outcomes Definition
2.4. Statistical Analysis
3. Results
3.1. General Data and Symptoms
3.2. Lab Tests among Categories
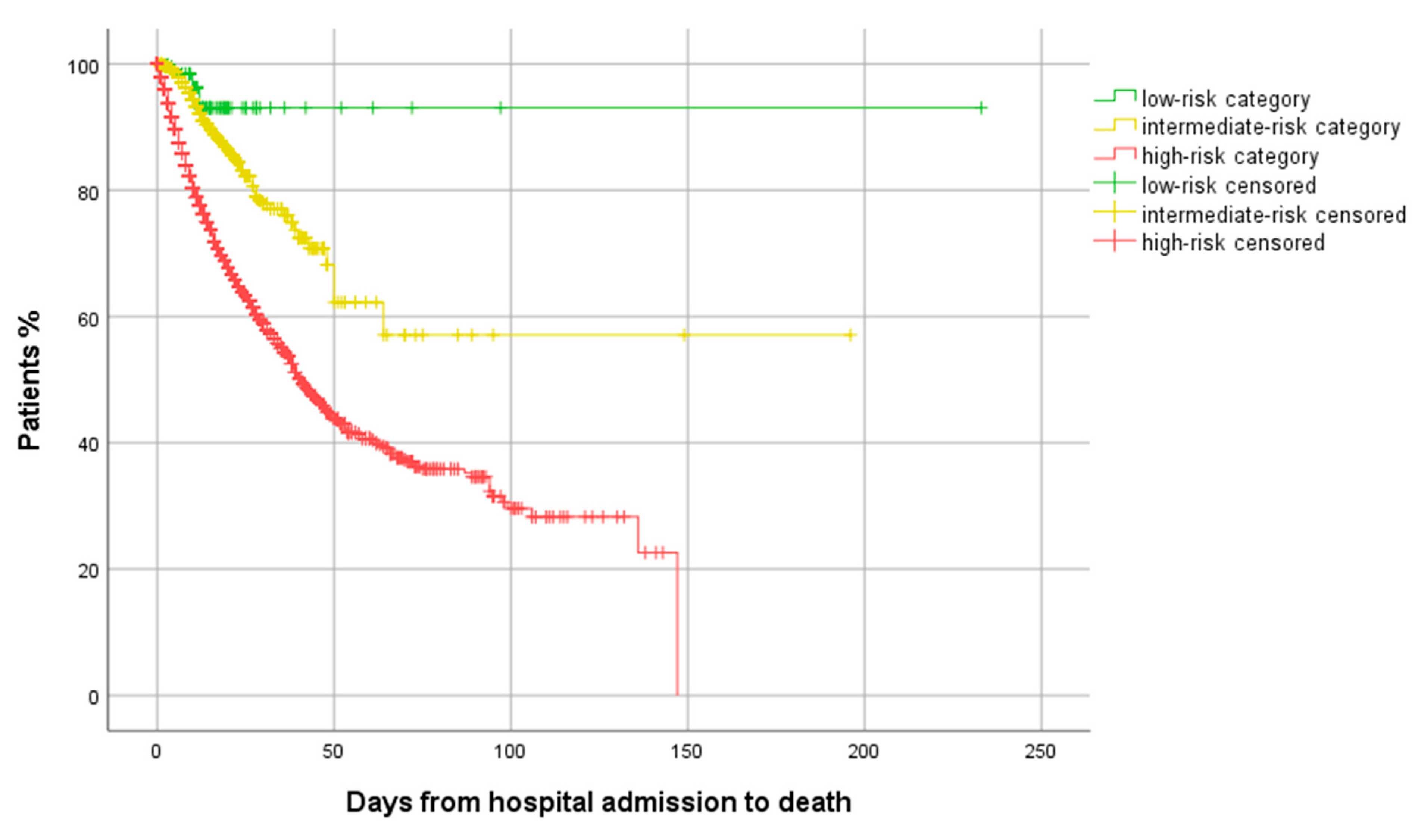
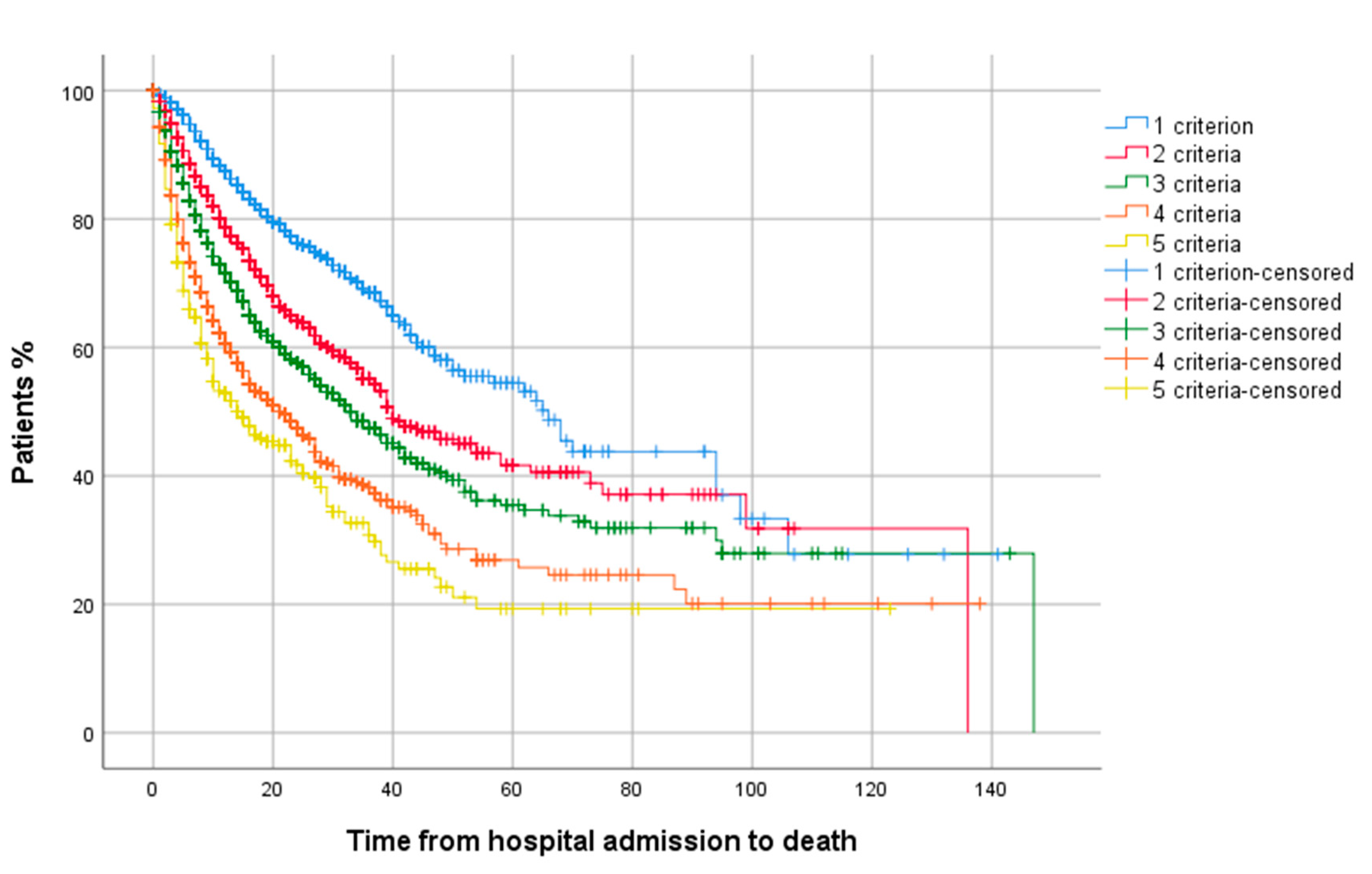
3.3. Outcomes
3.4. Risk Factors for HFNC, NIMV, IMV, ICU Admission and in-Hospital Mortality
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar]
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)—China, 2020. China CDC Weekly 2020, 2, 113–122. Available online: http://weekly.chinacdc.cn/en/article/id/e53946e2-c6c4-41e9-9a9b-fea8db1a8f51 (accessed on 12 March 2020).
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar]
- Du, R.-H.; Liang, L.-R.; Yang, C.-Q.; Wang, W.; Cao, T.-Z.; Li, M.; Guo, G.-Y.; Du, J.; Zheng, C.-L.; Zhu, Q.; et al. Predictors of Mortality for Patients with COVID-19 Pneumonia Caused by SARS-CoV-2: A Prospective Cohort Study. Eur. Respir. J. 2020, 55, 2000524. [Google Scholar]
- Rodilla, E.; López-Carmona, M.D.; Cortes, X.; Cobos-Palacios, L.; Canales, S.; Sáez, M.C.; Escudero, S.C.; Rubio-Rivas, M.; Manglano, J.D.; Castro, S.J.F.; et al. Impact of arterial stiffness on all-cause mortality in patients hospitalized with COVID-19 in Spain. Hypertension 2020, 77, 856–867. [Google Scholar] [CrossRef]
- Pérez-Belmonte, L.M.; Torres-Peña, J.D.; López-Carmona, M.D.; Ayala-Gutiérrez, M.M.; Fuentes-Jiménez, F.; Huerta, L.J.; Muñoz, J.A.; Rubio-Rivas, M.; Madrazo, M.; Garcia, M.G.; et al. Mortality and other adverse outcomes in patients with type 2 diabetes mellitus admitted for COVID-19 in association with glucose-lowering drugs: A nationwide cohort study. BMC Med. 2020, 18, 359. [Google Scholar]
- Ramos-Rincon, J.-M.; Buonaiuto, V.; Ricci, M.; Martín-Carmona, J.; Paredes-Ruíz, D.; Calderón-Moreno, M.; Rubio-Rivas, M.; Beato-Pérez, J.-L.; Arnalich-Fernández, F.; Monge-Monge, D.; et al. Clinical Characteristics and Risk Factors for Mortality in Very Old Patients Hospitalized with COVID-19 in Spain. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2021, 76, e28–e37. [Google Scholar] [CrossRef]
- Wang, B.; Li, R.; Lu, Z.; Huang, Y. Does comorbidity increase the risk of patients with covid-19: Evidence from meta-analysis. Aging 2020, 12, 6049–6057. [Google Scholar]
- Rubio-Rivas, M.; Corbella, X.; Mora-Luján, J.M.; Loureiro-Amigo, J.; Sampalo, A.L.; Bergua, C.Y.; Atiénzar, P.J.E.; García, L.F.D.; Ferrer, R.G.; Canteli, S.P.; et al. Predicting Clinical Outcome with Phenotypic Clusters in COVID-19 Pneumonia: An Analysis of 12,066 Hospitalized Patients from the Spanish Registry SEMI-COVID-19. J. Clin. Med. 2020, 9, 3488. [Google Scholar]
- Hu, B.; Huang, S.; Yin, L. The cytokine storm and COVID-19. J. Med. Virol. 2021, 93, 250–256. [Google Scholar] [CrossRef]
- Casas-Rojo, J.; Antón-Santos, J.; Millán-Núñez-Cortés, J.; Lumbreras-Bermejo, C.; Ramos-Rincón, J.; Roy-Vallejo, E.; Artero-Mora, A.; Arnalich-Fernández, F.; García-Bruñén, J.; Vargas-Núñez, J.; et al. Clinical characteristics of patients hospitalized with COVID-19 in Spain: Results from the SEMI-COVID-19 Registry. Rev. Clín. Esp. 2020, 220, 480–494. [Google Scholar] [CrossRef]
- Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; Elmahi, E.; et al. Dexamethasone in Hospitalized Patients with Covid-19—Preliminary Report. N. Engl. J. Med. 2020. [Google Scholar] [CrossRef]
- Rubio-Rivas, M.; Ronda, M.; Padulles, A.; Mitjavila, F.; Riera-Mestre, A.; García-Forero, C.; Iriarte, A.; Mora, J.M.; Padulles, N.; Gonzalez, M.; et al. Beneficial effect of corticosteroids in preventing mortality in patients receiving tocilizumab to treat severe COVID-19 illness. Int. J. Infect. Dis. 2020, 101, 290–297. [Google Scholar]
- Stone, J.H.; Frigault, M.J.; Serling-Boyd, N.J.; Fernandes, A.D.; Harvey, L.; Foulkes, A.S.; Horick, N.K.; Healy, B.C.; Shah, R.; Bensaci, A.M.; et al. Efficacy of Tocilizumab in Patients Hospitalized with Covid-19. N. Engl. J. Med. 2020, 383, 2333–2344. [Google Scholar]
- Salvarani, C.; Dolci, G.; Massari, M.; Franco Merlo, D.; Cavuto, S.; Savoldi, L.; Bruzzi, P.; Boni, F.; Braglia, L.; Turrà, C.; et al. Effect of Tocilizumab vs Standard Care on Clinical Worsening in Patients Hospitalized With COVID-19 Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021, 181, 24–31. [Google Scholar]
- Hermine, O.; Mariette, X.; Tharaux, P.L.; Resche-Rigon, M.; Porcher, R.; Ravaud, P. CORIMUNO-19 Collaborative Group. Effect of Tocilizumab vs Usual Care in Adults Hospitalized With COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021, 181, 32–40. [Google Scholar]
- Salama, C.; Han, J.; Yau, L.; Reiss, W.G.; Kramer, B.; Neidhart, J.D.; Criner, G.J.; Kaplan-Lewis, E.; Baden, R.; Pandit, L.; et al. Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N. Engl. J. Med. 2021, 384, 20–30. [Google Scholar]
| Low Risk | Intermediate Risk | High Risk | |
|---|---|---|---|
| Lymphocyte count ×106/L | >1150 | 760–1150 | <760 |
| CRP (mg/L) | <31.8 | 31.8–101.5 | >101.5 |
| LDH (U/L) | <271 | 271–394 | >394 |
| Ferritin (mcg/L) | <572.9 | 572.9–1359.9 | >1359.9 |
| D-dimer (ng/mL) | <539 | 539–1580 | >1580 |
| Low Risk | Intermediate Risk | High Risk | p-Value | |
|---|---|---|---|---|
| N | 352 | 3018 | 13,752 | |
| Age, median (IQR) | 57.9 (43.7–71.3) | 64.2 (51.7–76.5) | 70.4 (57.8–80.3) | <0.001 |
| Gender (males) | 132 (37.5) | 1416 (46.9) | 8264 (60.1) | <0.001 |
| Days from onset to admission, median (IQR) | 6 (3–10) | 7 (4–9) | 6 (3–9) | 0.005 |
| Smoking behaviour | <0.001 | |||
| Never smoker | 254 (72.2) | 2201 (72.9) | 9485 (69) | |
| Former smoker | 71 (20.2) | 664 (22) | 3582 (26) | |
| Current smoker | 27 (7.7) | 153 (5.1) | 685 (5) | |
| Degree of dependency | <0.001 | |||
| None or mild | 314 (89.2) | 2595 (86) | 11,423 (83.1) | |
| Moderate | 24 (6.8) | 231 (7.7) | 1329 (9.7) | |
| Severe | 14 (4) | 192 (6.4) | 1000 (7.3) | |
| Arterial hypertension | 130 (36.9) | 1365 (45.2) | 7260 (52.8) | <0.001 |
| Dyslipidemia | 100 (28.4) | 1118 (37) | 5584 (40.6) | <0.001 |
| Diabetes mellitus | 42 (11.9) | 516 (17.1) | 2822 (20.5) | <0.001 |
| Ischaemic cardiopathy | 13 (3.7) | 196 (6.5) | 1151 (8.4) | <0.001 |
| Chronic heart failure | 12 (3.4) | 158 (5.2) | 1045 (7.6) | <0.001 |
| Chronic liver disease | 4 (1.1) | 91 (3) | 537 (3.9) | 0.002 |
| Severe chronic renal failure | 8 (2.3) | 108 (3.6) | 920 (6.7) | <0.001 |
| Cancer | 23 (6.5) | 216 (7.2) | 1521 (11.1) | <0.001 |
| COPD | 20 (5.7) | 163 (5.4) | 972 (7.1) | 0.003 |
| Asthma | 40 (11.4) | 279 (9.2) | 895 (7.1) | <0.001 |
| OSAS | 16 (4.5) | 188 (6.2) | 839 (6.1) | 0.455 |
| Low Risk | Intermediate Risk | High Risk | p-Value | |
|---|---|---|---|---|
| Cough, n (%) | 258 (73.3) | 2269 (75.2) | 9950 (72.4) | 0.007 |
| Arthromyalgias, n (%) | 108 (30.7) | 1027 (34) | 4011 (29.2) | <0.001 |
| Ageusia, n (%) | 39 (11.1) | 343 (11.4) | 1070 (7.8) | <0.001 |
| Anosmia, n (%) | 43 (12.2) | 303 (10) | 926 (6.7) | <0.001 |
| Sore throat, n (%) | 50 (14.2) | 344 (11.4) | 1237 (9) | <0.001 |
| Headache, n (%) | 58 (16.5) | 448 (14.8) | 1499 (10.9) | <0.001 |
| Fever, n (%) | 251 (71.3) | 2506 (83) | 11,592 (84.3) | <0.001 |
| Dyspnea, n (%) | 184 (52.3) | 1542 (51.1) | 8121 (59.1) | <0.001 |
| Diarrhea, n (%) | 83 (23.6) | 790 (26.2) | 3224 (23.4) | 0.006 |
| Vomiting, n (%) | 12 (3.4) | 235 (7.8) | 1097 (8) | 0.007 |
| Abdominal pain, n (%) | 26 (7.4) | 195 (6.5) | 894 (6.5) | 0.795 |
| Heart rate, bpm median (IQR) | 85.5 (75–98) | 85 (75–97) | 88 (77–100) | <0.001 |
| Respiratory rate >20 rpm, n (%) | 45 (12.8) | 579 (19.2) | 4809 (35) | <0.001 |
| Low Risk | Intermediate Risk | High Risk | p-Value | |
|---|---|---|---|---|
| Lymphocytes ×106/L, median (IQR) | 1605 (1340–2100) | 1180 (960–1500) | 860 (600–1200) | <0.001 |
| CRP mg/L, median (IQR) | 6.3 (2.2–14.9) | 30 (10.7–57) | 81.5 (28.2–151) | <0.001 |
| LDH U/L, median (IQR) | 203 (175–230) | 261 (213–312) | 360 (267–486.4) | <0.001 |
| Ferritin mcg/L, median (IQR) | 220.3 (103.5–371) | 534 (259.2–891) | 1144.7 (532–1834.5) | <0.001 |
| D-dimer ng/mL, median (IQR) | 286.5 (210.8–400) | 490 (280–776.3) | 1131 (510–4347.8) | <0.001 |
| Low Risk | Intermediate Risk | High Risk | p-Value | |
|---|---|---|---|---|
| HFNC, n (%) | 11 (3.1) | 132 (4.4) | 1319 (9.7) | <0.001 |
| NIMV, n (%) | 3 (0.9) | 90 (3) | 857 (6.3) | <0.001 |
| IMV, n (%) | 2 (0.6) | 80 (2.7) | 1195 (8.7) | <0.001 |
| ICU admission, n (%) | 3 (0.9) | 109 (3.6) | 1453 (10.6) | <0.001 |
| In-hospital mortality, n (%) | 8 (2.3) | 186 (6.2) | 3291 (23.9) | <0.001 |
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Age | 1.08 (1.08–1.09) | <0.001 | 1.07 (1.07–1.08) | <0.001 |
| Gender (female) | 0.76 (0.70–0.82) | <0.001 | 0.67 (0.61–0.74) | <0.001 |
| Smoking behaviour | ||||
| Never smoker | 1 ref. | 1 ref. | ||
| Former smoker | 1.57 (1.45–1.70) | <0.001 | 1.12 (1.00–1.24) | 0.052 |
| Current smoker | 1.06 (0.89–1.26) | 0.540 | 1.27 (1.03–1.58) | 0.025 |
| Degree of dependency | ||||
| None or mild | 1 ref. | 1 ref. | ||
| Moderate | 4.20 (3.77–4.69) | <0.001 | 1.60 (1.41–1.83) | <0.001 |
| Severe | 4.99 (4.42–5.63) | <0.001 | 2.01 (1.73–2.33) | <0.001 |
| Arterial hypertension | 2.77 (2.56–3.00) | <0.001 | - | NS |
| Dyslipidemia | 1.77 (1.64–1.91) | <0.001 | - | NS |
| Diabetes mellitus | 1.97 (1.81–2.15) | <0.001 | 1.21 (1.09–1.34) | <0.001 |
| Ischaemic cardiopathy | 2.41 (2.14–2.71) | <0.001 | 1.25 (1.08–1.44) | 0.002 |
| Chronic heart failure | 3.32 (2.94–3.74) | <0.001 | - | NS |
| Chronic liver disease | 1.49 (1.24–1.78) | <0.001 | 1.32 (1.07–1.63) | 0.011 |
| Severe chronic renal failure | 3.19 (2.80–3.62) | <0.001 | 1.50 (1.29–1.76) | <0.001 |
| Cancer | 2.04 (1.83–2.27) | <0.001 | 1.54 (1.35–1.75) | <0.001 |
| COPD | 2.53 (2.24–2.87) | <0.001 | - | NS |
| Asthma | 0.62 (0.52–0.73) | <0.001 | - | NS |
| OSAS | 1.36 (1.18–1.57) | <0.001 | - | NS |
| Respiratory rate > 20 rpm | 3.91 (3.62–4.22) | <0.001 | 3.21 (2.94–3.51) | <0.001 |
| Three risk categories | ||||
| Low risk | 1 ref. | 1 ref. | ||
| Intermediate risk | 2.82 (1.38–5.78) | 0.005 | 1.91 (0.90–4.05) | 0.093 |
| High risk | 13.53 (6.7–27.30) | <0.001 | 7.31 (3.49–15.28) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubio-Rivas, M.; Corbella, X.; Formiga, F.; Menéndez Fernández, E.; Martín Escalante, M.D.; Baños Fernández, I.; Arnalich Fernández, F.; Del Corral-Beamonte, E.; Lalueza, A.; Parra Virto, A.; et al. Risk Categories in COVID-19 Based on Degrees of Inflammation: Data on More Than 17,000 Patients from the Spanish SEMI-COVID-19 Registry. J. Clin. Med. 2021, 10, 2214. https://doi.org/10.3390/jcm10102214
Rubio-Rivas M, Corbella X, Formiga F, Menéndez Fernández E, Martín Escalante MD, Baños Fernández I, Arnalich Fernández F, Del Corral-Beamonte E, Lalueza A, Parra Virto A, et al. Risk Categories in COVID-19 Based on Degrees of Inflammation: Data on More Than 17,000 Patients from the Spanish SEMI-COVID-19 Registry. Journal of Clinical Medicine. 2021; 10(10):2214. https://doi.org/10.3390/jcm10102214
Chicago/Turabian StyleRubio-Rivas, Manuel, Xavier Corbella, Francesc Formiga, Estela Menéndez Fernández, María Dolores Martín Escalante, Isolina Baños Fernández, Francisco Arnalich Fernández, Esther Del Corral-Beamonte, Antonio Lalueza, Alejandro Parra Virto, and et al. 2021. "Risk Categories in COVID-19 Based on Degrees of Inflammation: Data on More Than 17,000 Patients from the Spanish SEMI-COVID-19 Registry" Journal of Clinical Medicine 10, no. 10: 2214. https://doi.org/10.3390/jcm10102214
APA StyleRubio-Rivas, M., Corbella, X., Formiga, F., Menéndez Fernández, E., Martín Escalante, M. D., Baños Fernández, I., Arnalich Fernández, F., Del Corral-Beamonte, E., Lalueza, A., Parra Virto, A., Roy Vallejo, E., Loureiro-Amigo, J., Álvarez Suárez, A. M., Abadía-Otero, J., Navarro De La Chica, M., Estévez González, R., Hernández Milián, A., Areses Manrique, M., Blázquez Encinar, J. C., ... on behalf of the SEMI-COVID-19 Network. (2021). Risk Categories in COVID-19 Based on Degrees of Inflammation: Data on More Than 17,000 Patients from the Spanish SEMI-COVID-19 Registry. Journal of Clinical Medicine, 10(10), 2214. https://doi.org/10.3390/jcm10102214






