Analysis of Plantar Pressure Pattern after Metatarsal Head Resection. Can Plantar Pressure Predict Diabetic Foot Reulceration?
Abstract
1. Introduction
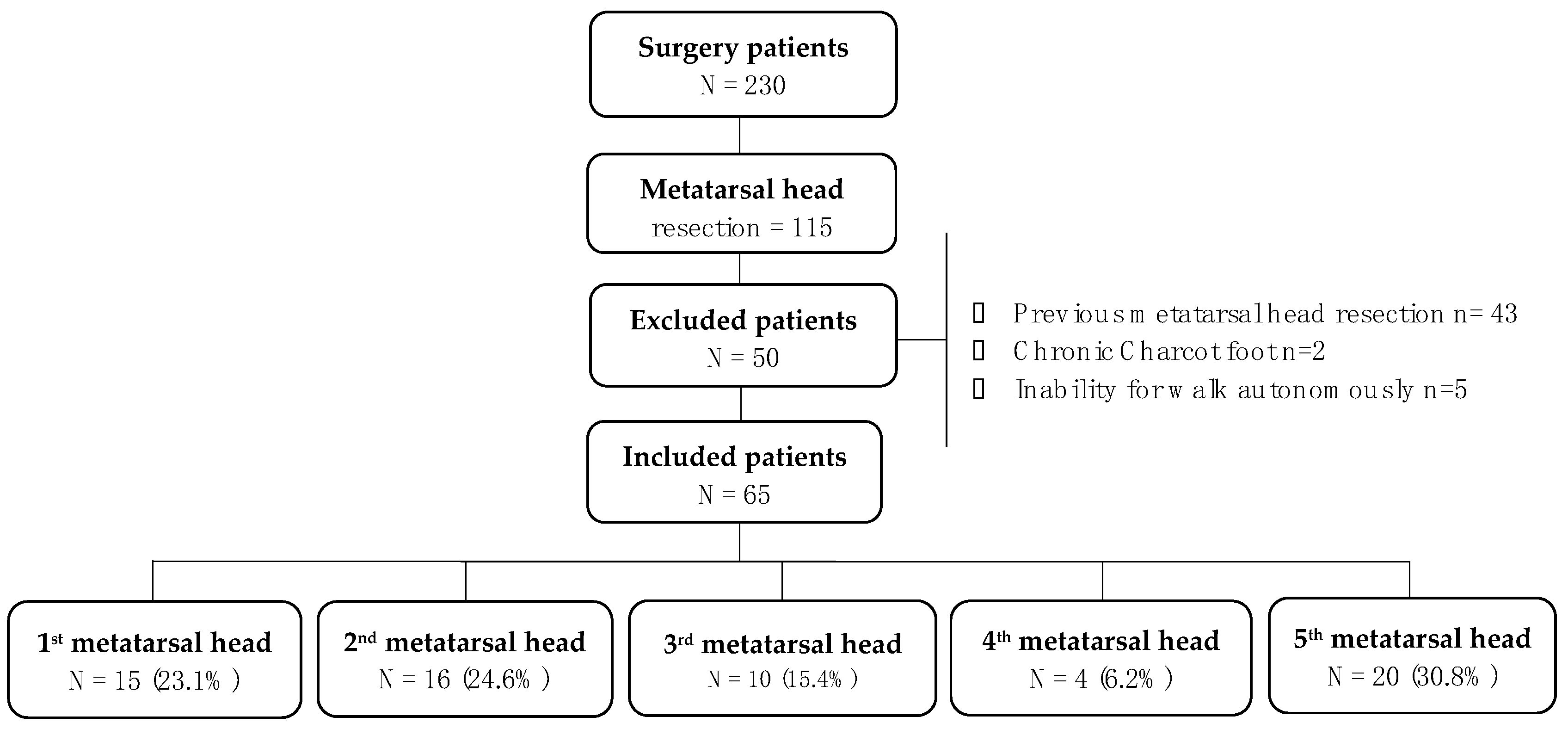
2. Materials and Methods
2.1. Subjects
2.2. Clinical Evaluation
2.3. Biomechanical and Plantar Pressure Assessment
2.4. Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Main Outcome
3.2. Secondary Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Armstrong, D.G.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers and Their Recurrence. N. Engl. J. Med. 2017, 376, 2367–2375. [Google Scholar] [CrossRef]
- Senneville, E.M.; Lipsky, B.A.; Van Asten, S.A.; Peters, E.J. Diagnosing diabetic foot osteomyelitis. Diabetes Metab. Res. Rev. 2020, 36, e3250. [Google Scholar] [CrossRef] [PubMed]
- Aragón-Sánchez, J.; Lázaro-Martínez, J.L.; Hernández-Herrero, C.; Campillo-Vilorio, N.; Quintana-Marrero, Y.; García-Morales, E.; Hernández-Herrero, M.J. Does osteomyelitis in the feet of patients with diabetes really recur after surgical treatment? Natural history of a surgical series. Diabet. Med. 2012, 29, 813–818. [Google Scholar] [CrossRef]
- Fernando, M.; Crowther, R.; Lazzarini, P.; Sangla, K.; Cunningham, M.; Buttner, P.; Golledge, J. Biomechanical characteristics of peripheral diabetic neuropathy: A systematic review and meta-analysis of findings from the gait cycle, muscle activity and dynamic barefoot plantar pressure. Clin. Biomech. 2013, 28, 831–845. [Google Scholar] [CrossRef] [PubMed]
- Fernando, M.E.; Crowther, R.G.; Pappas, E.; Lazzarini, P.A.; Cunningham, M.; Sangla, K.S.; Buttner, P.; Golledge, J. Plantar pressure in diabetic peripheral neuropathy patients with active foot ulceration, previous ulceration and no history of ulceration: A meta-analysis of observational studies. PLoS ONE 2014, 9, e99050. [Google Scholar] [CrossRef]
- Tang, U.H.; Zügner, R.; Lisovskaja, V.; Karlsson, J.; Hagberg, K.; Tranberg, R. Foot deformities, function in the lower extremities, and plantar pressure in patients with diabetes at high risk to develop foot ulcers. Diabet. Foot Ankle 2015, 6, 27593. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Lavery, L.A. Plantar pressures are higher in diabetic patients following partial foot amputation. Ostomy Wound Manag. 1998, 44, 30–36. [Google Scholar]
- Bus, S.A.; Lavery, L.A.; Monteiro-Soares, M.; Rasmussen, A.; Raspovic, A.; Sacco, I.C.; Van Netten, J.J.; on behalf of the International Working Group on the Diabetic Foot. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2019 update). Diabetes Metab. Res. Rev. 2020, 36. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Peters, E.J.; Athanasiou, K.A.; Lavery, L.A. Is there a critical level of plantar foot pressure to identify patients at risk for neuropathic foot ulceration? J. Foot Ankle Surg. 1998, 37, 303–307. [Google Scholar] [CrossRef]
- Lavery, L.A.; Armstrong, D.G.; Wunderlich, R.P.; Tredwell, J.; Boulton, A.J. Predictive Value of Foot Pressure Assessment as Part of a Population-Based Diabetes Disease Management Program. Diabetes Care 2003, 26, 1069–1073. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, D.G.; Frykberg, R.G. Classifying diabetic foot surgery: Toward a rational definition. Diabet. Med. 2003, 20, 329–331. [Google Scholar] [CrossRef] [PubMed]
- Griffiths, G.D.; Wieman, T.J. Metatarsal head resection for diabetic foot ulcers. Arch. Surg. 1990, 125, 832–835. [Google Scholar] [CrossRef] [PubMed]
- Tardáguila-García, A.; Sanz-Corbalán, I.; Molines-Barroso, R.J.; Álvaro-Afonso, F.J.; García-Álvarez, Y.; Lázaro-Martínez, J.L. Complications associated with the approach to metatarsal head resection in diabetic foot osteomyelitis. Int. Wound J. 2018, 16, 467–472. [Google Scholar] [CrossRef]
- Patel, V.G.; Wieman, T.J. Effect of metatarsal head resection for diabetic foot ulcers on the dynamic plantar pressure distribution. Am. J. Surg. 1994, 167, 297–301. [Google Scholar] [CrossRef]
- Borg, I.; Mizzi, S.; Formosa, C. Plantar Pressure Distribution in Patients with Diabetic Peripheral Neuropathy and a First-Ray Amputation. J. Am. Podiatr. Med. Assoc. 2018, 108, 225–230. [Google Scholar] [CrossRef]
- Deschamps, K.; Matricali, G.A.; Roosen, P.; Desloovere, K.; Bruyninckx, H.; Spaepen, P.; Nobels, F.; Tits, J.; Flour, M.; Staes, F. Classification of Forefoot Plantar Pressure Distribution in Persons with Diabetes: A Novel Perspective for the Mechanical Management of Diabetic Foot? PLoS ONE 2013, 8, e79924. [Google Scholar] [CrossRef]
- Richard, J.-L.; Reilhes, L.; Buvry, S.; Goletto, M.; Faillie, J.-L. Screening patients at risk for diabetic foot ulceration: A comparison between measurement of vibration perception threshold and 10-g monofilament test. Int. Wound J. 2012, 11, 147–151. [Google Scholar] [CrossRef]
- Hinchliffe, R.J.; Forsythe, R.O.; Apelqvist, J.; Boyko, E.J.; Fitridge, R.; Hong, J.P.; Katsanos, K.; Mills, J.L.; Nikol, S.; Reekers, J.; et al. Guidelines on diagnosis, prognosis, and management of peripheral artery disease in patients with foot ulcers and diabetes (IWGDF 2019 update). Diabetes Metab. Res. Rev. 2020, 36, e3276. [Google Scholar] [CrossRef]
- van Netten, J.J.; Bus, S.A.; Apelqvist, J.; Lipsky, B.A.; Hinchliffe, R.J.; Game, F.; Rayman, G.; Lazzarini, P.A.; Forsythe, R.O.; Peters, E.J.; et al. Definitions and criteria for diabetic foot dis-ease. Diabetes Metab. Res. Rev. 2020, 36, e3268. [Google Scholar]
- Lázaro-Martínez, J.L.; Aragón-Sánchez, J.; Álvaro-Afonso, F.J.; García-Morales, E.; García-Álvarez, Y.; Molines-Barroso, R.J. The best way to reduce reulcerations: If you understand biomechanics of the diabetic foot, you can do it. Int. J. Low Extrem. Wounds 2014, 13, 294–319. [Google Scholar] [CrossRef]
- Bus, S.A.; de Lange, A. A comparison of the 1-step, 2-step, and 3-step protocols for obtaining barefoot plantar pressure data in the diabetic neuropathic foot. Clin. Biomech. 2005, 20, 892–899. [Google Scholar] [CrossRef] [PubMed]
- Zwaferink, J.B.; Custers, W.; Paardekooper, I.; Berendsen, H.A.; Bus, S.A. Optimizing footwear for the diabetic foot: Data-driven custom-made footwear concepts and their effect on pressure relief to prevent diabetic foot ulceration. PLoS ONE 2020, 15, e0224010. [Google Scholar] [CrossRef] [PubMed]
- López-Moral, M.; Lázaro-Martínez, J.L.; García-Morales, E.; García-Álvarez, Y.; Álvaro-Afonso, F.J.; Molines-Barroso, R.J. Clin-ical efficacy of therapeutic footwear with a rigid rocker sole in the prevention of recurrence in patients with diabetes mellitus and diabetic polineuropathy: A randomized clinical trial. PLoS ONE 2019, 14, e0219537. [Google Scholar] [CrossRef] [PubMed]
- van Netten, J.J.; Price, P.E.; Lavery, L.A.; Monteiro-Soares, M.; Rasmussen, A.; Jubiz, Y.; Bus, S.A. Prevention of foot ulcers in the at-risk patient with diabetes: A systematic review. Diabetes Metab. Res. Rev. 2016, 32, 84–98. [Google Scholar] [CrossRef]
- Molines-Barroso, R.J.; Lázaro-Martínez, J.L.; Aragón-Sánchez, J.; García-Morales, E.; Beneit-Montesinos, J.V.; Álvaro-Afonso, F.J. Analysis of transfer lesions in patients who underwent surgery for diabetic foot ulcers located on the plantar aspect of the metatarsal heads. Diabet. Med. 2013, 30, 973–976. [Google Scholar] [CrossRef]
- Dalla Paola, L.; Faglia, E.; Caminiti, M.; Clerici, G.; Ninkovic, S.; Deanesi, V. Ulcer recurrence following first ray amputation in diabetic patients: A cohort prospective study. Diabetes Care 2003, 26, 1874–1878. [Google Scholar] [CrossRef]
- Molines-Barroso, R.J.; Lázaro-Martínez, J.L.; Aragón-Sánchez, J.; García-Morales, E.; Carabantes-Alarcón, D.; Álvaro-Afonso, F.J. The Influence of the Length of the First Metatarsal on the Risk of Reulceration in the Feet of Patients With Diabetes. Int. J. Low. Extrem. Wounds 2014, 13, 27–32. [Google Scholar] [CrossRef]
- Yavuz, M.; Master, H.; Garrett, A.; Lavery, L.A.; Adams, L.S. Peak Plantar Shear and Pressure and Foot Ulcer Locations: A Call to Revisit Ulceration Pathomechanics. Diabetes Care 2015, 38, e184–e185. [Google Scholar] [CrossRef]
| Baseline Characteristics | Patients (N = 65) |
|---|---|
| Male/Female, n (%) | 61 (93.8%)/4 (6.2%) |
| Type 1/Type 2 Diabetes, n (%) | 15 (23.1%)/50 (76.9%) |
| Retinopathy, n (%) | 30 (46.2%) |
| Hypertension, n (%) | 55 (84.6%) |
| Nephropathy, n (%) | 16 (24.6%) |
| Cardiopathy, n (%) | 21 (32.3%) |
| Diabetic polyneuropathy, n (%) | 65 (100%) |
| PAD, n (%) | 23(35.4%) |
| Mean age ± SD (years) | 64.28 ± 10.74 |
| Body mass index (kg/m2), mean ± SD | 28.27 ± 6.0 |
| Diabetes mellitus (years), mean ± SD | 23.06 ±11.38 |
| Glycated hemoglobin (%), mean ± SD | 7.78 ± 1.42 |
| Foot Characteristics | |
| Previous partial toe amputation, n (%) | 40 (61.5%) |
| Hallux abductus valgus, n (%) | 6 (9.2%) |
| Taylor´s bunion, n (%) | 14 (21.5%) |
| Hammer toe, n (%) | 47 (72.3%) |
| Metatarsal prominence, n (%) | 49 (75.4%) |
| Baseline pressure distribution | |
| PPP forefoot area (N/cm2) (1st to 5th metatarsal heads) PTI forefoot area (N/cm2/s) (1st to 5th metatarsal heads) | 72.92 ± 26.94 28.77 ± 13.26 |
| Metatarsal Head Resected | Peak Plantar Pressure N/cm2 | p Value (95% CI) | ||||
|---|---|---|---|---|---|---|
| 1st Metatarsal | 2nd Metatarsal | 3rd Metatarsal | 4th Metatarsal | 5th Metatarsal | ||
| 1st MHR | - | 22.53 [31.20–16.70] * | 12.14 [16.26–8.26] | 9.46 [21.60–2.93] | 6.66 [10.10–0.60] | <0.001 * (18.01–31.42) |
| 2nd MHR | 25.93 [31.57–14.99] * | - | 13.40 [25.42–7.33] | 9.0 [17.77–5.16] | 5.46 [11.50–2.35] | 0.001 * (17.41–31.66) |
| 3rd MHR | 26.42 [29.14–22.57] * | 16.65 [27.28–8.70] | - | 14.30 [15.96–12.95] | 5.08 [15.62–1.51] | 0.001 * (22–32.83) |
| 4th MHR | 8.93 [14–4.81] | 27.21 [30.66–24.53] * | 25.93 [27.46–18.20] | - | 16.10 [18.81–11.70] | 0.009 * (22.40–32.54) |
| 5th MHR | 10.13 [17.10–5.76] | 19.10 [22.89–10.00] | 23.19 [25.96–18.95] * | 14.65 [16.91–13.09] | - | <0.001 * (20.59–24.86) |
| Metatarsal Head Resected | Pressure Time Integral N/cm2/s | p Value (95% CI) | ||||
|---|---|---|---|---|---|---|
| 1st Metatarsal | 2nd Metatarsal | 3rd Metatarsal | 4th Metatarsal | 5th Metatarsal | ||
| 1st MHR | - | 6.73 [12.30–1.93] * | 6.33 [12.30–1.93] | 3.13 [5.86–0.96] | 2.16 [3.86–0.16] | 0.003 * (3.95–10.06) |
| 2nd MHR | 8.75 [14.56–3.70] * | - | 5.06 [10.69–3.43] | 3.41 [6.75–2.57] | 1.85 [6.87–1.04] | 0.02 * (5.90–13.13) |
| 3rd MHR | 11.86 [14.86–9.26] * | 4.51 [8.07–2.14] | - | 6.82 [7.70–5.90] | 1.96 [6.65–0.37] | <0.001 * (8.81–18.33) |
| 4th MHR | 2.10 [4.96–0.75] | 14.25 [16.45–12.65] * | 7.83 [12.80–1.65] | - | 10.93 [14.54–4.60] | 0.02 * (11.26–17.63) |
| 5th MHR | 3.41 [4.75–1.44] | 4.76 [6.45–2.26] | 11.33 [13.15–9.67] * | 5.00 [7.97–2.90] | - | <0.001 * (10.2–12.39) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Madrid, M.; García-Álvarez, Y.; Álvaro-Afonso, F.J.; García-Morales, E.; Tardáguila-García, A.; Lázaro-Martínez, J.L. Analysis of Plantar Pressure Pattern after Metatarsal Head Resection. Can Plantar Pressure Predict Diabetic Foot Reulceration? J. Clin. Med. 2021, 10, 2260. https://doi.org/10.3390/jcm10112260
García-Madrid M, García-Álvarez Y, Álvaro-Afonso FJ, García-Morales E, Tardáguila-García A, Lázaro-Martínez JL. Analysis of Plantar Pressure Pattern after Metatarsal Head Resection. Can Plantar Pressure Predict Diabetic Foot Reulceration? Journal of Clinical Medicine. 2021; 10(11):2260. https://doi.org/10.3390/jcm10112260
Chicago/Turabian StyleGarcía-Madrid, Marta, Yolanda García-Álvarez, Francisco Javier Álvaro-Afonso, Esther García-Morales, Aroa Tardáguila-García, and José Luis Lázaro-Martínez. 2021. "Analysis of Plantar Pressure Pattern after Metatarsal Head Resection. Can Plantar Pressure Predict Diabetic Foot Reulceration?" Journal of Clinical Medicine 10, no. 11: 2260. https://doi.org/10.3390/jcm10112260
APA StyleGarcía-Madrid, M., García-Álvarez, Y., Álvaro-Afonso, F. J., García-Morales, E., Tardáguila-García, A., & Lázaro-Martínez, J. L. (2021). Analysis of Plantar Pressure Pattern after Metatarsal Head Resection. Can Plantar Pressure Predict Diabetic Foot Reulceration? Journal of Clinical Medicine, 10(11), 2260. https://doi.org/10.3390/jcm10112260










