The Spectrum of Central Choriocapillaris Abnormalities on Swept-Source Optical Coherence Tomography Angiography in the Fellow Eye of Unilateral Exudative Age-Related Macular Degeneration Patients: From Flow Deficits to Subclinical Non-Exudative Neovascularization
Abstract
1. Introduction
2. Materials and Methods
2.1. Imaging
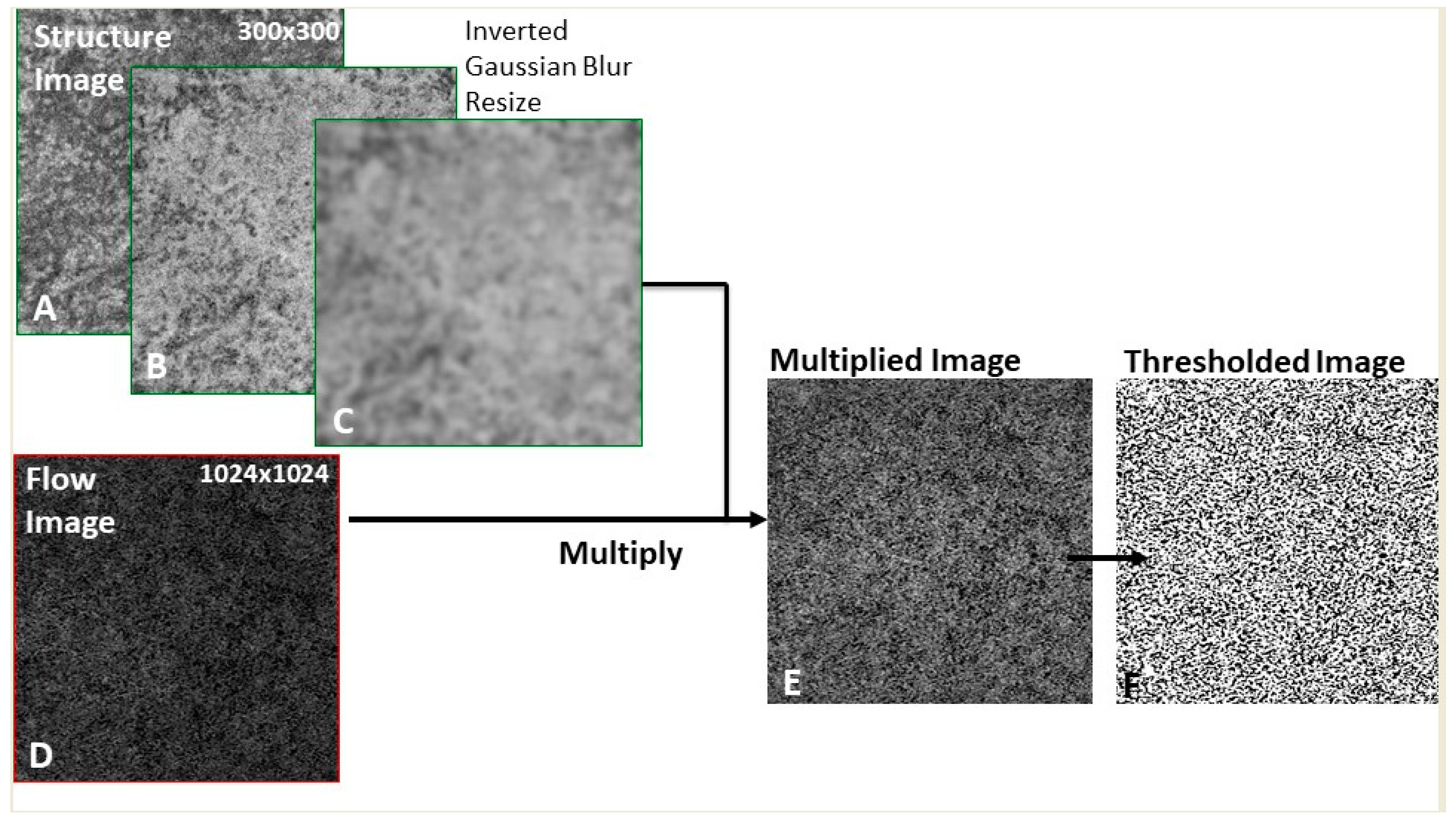
2.2. Image Processing
2.3. Statistical Analysis
3. Results
3.1. Patient Demographics and Clinical Characteristics
3.2. OCTA Spectrum of Choriocapillaris Abnormalities
3.2.1. Neovascularization: Subclinical Non-Exudative MNV
3.2.2. Choriocapillaris Flow Deficits in Non-Neovascular Fellow Eyes
3.2.3. Sensitivity Analysis
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bressler, N.M. Age-related macular degeneration is the leading cause of blindness. JAMA 2004, 291, 1900–1901. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.J.; Agrón, E.; Clemons, T.E.; Domalpally, A.; van Asten, F.; Keenan, T.D.; Cukras, C.; Chew, E.Y.; Age-Related Eye Disease Study 2 Research Group. Natural History of Drusenoid Pigment Epithelial Detachment Associated with Age-Related Macular Degeneration: Age-Related Eye Disease Study 2 Report No. 17. Ophthalmology 2019, 126, 261–273. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Uji, A.; Sarraf, D.; Sadda, S.R. Alterations in the Choriocapillaris in Intermediate Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2017, 58, 4792–4798. [Google Scholar] [CrossRef] [PubMed]
- Ramrattan, R.S.; van der Schaft, T.L.; Mooy, C.M.; de Bruijn, W.C.; Mulder, P.G.; de Jong, P.T. Morphometric analysis of Bruch’s membrane, the choriocapillaris, and the choroid in aging. Investig. Ophthalmol. Vis. Sci. 1994, 35, 2857–2864. [Google Scholar]
- Grunwald, J.E.; Metelitsina, T.I.; Dupont, J.C.; Ying, G.S.; Maguire, M.G. Reduced foveolar choroidal blood flow in eyes with increasing AMD severity. Investig. Ophthalmol. Vis. Sci. 2005, 46, 1033–1038. [Google Scholar] [CrossRef]
- Bhutto, I.; Lutty, G. Understanding age-related macular degeneration (AMD): Relationships between the photoreceptor/retinal pigment epithelium/Bruch’s membrane/choriocapillaris complex. Mol. Asp. Med. 2012, 33, 295–317. [Google Scholar] [CrossRef]
- Spaide, R.F. Choriocapillaris Flow Features Follow a Power Law Distribution: Implications for Characterization and Mechanisms of Disease Progression. Am. J. Ophthalmol. 2016, 170, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Borrelli, E.; Sarraf, D.; Freund, K.B.; Sadda, S.R. OCT angiography and evaluation of the choroid and choroidal vascular disorders. Prog. Retin. Eye Res. 2018, 67, 30–55. [Google Scholar] [CrossRef]
- Zheng, F.; Zhang, Q.; Shi, Y.; Russell, J.F.; Motulsky, E.H.; Banta, J.T.; Chu, Z.; Zhou, H.; Patel, N.A.; de Sisternes, L.; et al. Age-dependent Changes in the Macular Choriocapillaris of Normal Eyes Imaged with Swept-Source Optical Coherence Tomography Angiography. Am. J. Ophthalmol. 2019, 200, 110–122. [Google Scholar] [CrossRef]
- Borrelli, E.; Shi, Y.; Uji, A.; Balasubramanian, S.; Nassisi, M.; Sarraf, D.; Sadda, S.R. Topographic Analysis of the Choriocapillaris in Intermediate Age-related Macular Degeneration. Am. J. Ophthalmol. 2018, 196, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Green, W.R.; Key, S.N., 3rd. Senile macular degeneration: A histopathologic study. Trans. Am. Ophthalmol. Soc. 1977, 75, 180–254. [Google Scholar]
- Sarks, S.H. New vessel formation beneath the retinal pigment epithelium in senile eyes. Br. J. Ophthalmol. 1973, 57, 951–965. [Google Scholar] [CrossRef] [PubMed]
- Querques, G.; Srour, M.; Massamba, N.; Georges, A.; Ben Moussa, N.; Rafaeli, O.; Souied, E.H. Functional characterization and multimodal imaging of treatment-naive “quiescent” choroidal neovascularization. Investig. Ophthalmol. Vis. Sci. 2013, 54, 6886–6892. [Google Scholar] [CrossRef] [PubMed]
- Carnevali, A.; Cicinelli, M.V.; Capuano, V.; Corvi, F.; Mazzaferro, A.; Querques, L.; Scorcia, V.; Souied, E.H.; Bandello, F.; Querques, G. Optical Coherence Tomography Angiography: A Useful Tool for Diagnosis of Treatment-Naïve Quiescent Choroidal Neovascularization. Am. J. Ophthalmol. 2016, 169, 189–198. [Google Scholar] [CrossRef]
- Roisman, L.; Zhang, Q.; Wang, R.K.; Gregori, G.; Zhang, A.; Chen, C.L.; Durbin, M.K.; An, L.; Stetson, P.F.; Robbins, G.; et al. Optical Coherence Tomography Angiography of Asymptomatic Neovascularization in Intermediate Age-Related Macular Degeneration. Ophthalmology 2016, 123, 1309–1319. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhang, Q.; Motulsky, E.H.; Thulliez, M.; Shi, Y.; Lyu, C.; de Sisternes, L.; Durbin, M.K.; Feuer, W.; Wang, R.K.; et al. Two-Year Risk of Exudation in Eyes with Nonexudative Age-Related Macular Degeneration and Subclinical Neovascularization Detected with Swept Source Optical Coherence Tomography Angiography. Am. J. Ophthalmol. 2019, 208, 1–11. [Google Scholar] [CrossRef]
- García-Layana, A.; Cabrera-López, F.; García-Arumí, J.; Arias-Barquet, L.; Ruiz-Moreno, J.M. Early and intermediate age-related macular degeneration: Update and clinical review. Clin. Interv. Aging 2017, 12, 1579–1587. [Google Scholar] [CrossRef]
- Spaide, R.F. Disease Expression in Nonexudative Age-Related Macular Degeneration Varies with Choroidal Thickness. Retina 2018, 38, 708–716. [Google Scholar] [CrossRef]
- Zhang, Q.; Zheng, F.; Motulsky, E.H.; Gregori, G.; Chu, Z.; Chen, C.L.; Li, C.; de Sisternes, L.; Durbin, M.; Rosenfeld, P.J.; et al. A Novel Strategy for Quantifying Choriocapillaris Flow Voids Using Swept-Source OCT Angiography. Investig. Ophthalmol. Vis. Sci. 2018, 59, 203–211. [Google Scholar] [CrossRef]
- Chu, Z.; Cheng, Y.; Zhang, Q.; Zhou, H.; Dai, Y.; Shi, Y.; Gregori, G.; Rosenfeld, P.J.; Wang, R.K. Quantification of Choriocapillaris with Phansalkar Local Thresholding: Pitfalls to Avoid. Am. J. Ophthalmol. 2020, 213, 161–176. [Google Scholar] [CrossRef]
- Sacconi, R.; Borrelli, E.; Corbelli, E.; Capone, L.; Rabiolo, A.; Carnevali, A.; Casaluci, M.; Gelormini, F.; Querques, L.; Bandello, F.; et al. Quantitative changes in the ageing choriocapillaris as measured by swept source optical coherence tomography angiography. Br. J. Ophthalmol. 2019, 103, 1320–1326. [Google Scholar] [CrossRef]
- Spaide, R.F. Improving the Age-Related Macular Degeneration Construct: A New Classification System. Retina 2018, 38, 891–899. [Google Scholar] [CrossRef]
- Nassisi, M.; Baghdasaryan, E.; Tepelus, T.; Asanad, S.; Borrelli, E.; Sadda, S.R. Topographic distribution of choriocapillaris flow deficits in healthy eyes. PLoS ONE 2018, 13, e0207638. [Google Scholar] [CrossRef] [PubMed]
- Uji, A.; Balasubramanian, S.; Lei, J.; Baghdasaryan, E.; Al-Sheikh, M.; Sadda, S.R. Choriocapillaris Imaging Using Multiple En Face Optical Coherence Tomography Angiography Image Averaging. JAMA Ophthalmol. 2017, 135, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Byon, I.; Nassisi, M.; Borrelli, E.; Sadda, S.R. Impact of Slab Selection on Quantification of Choriocapillaris Flow Deficits by Optical Coherence Tomography Angiography. Am. J. Ophthalmol. 2019, 208, 397–405. [Google Scholar] [CrossRef]
- Chu, Z.; Gregori, G.; Rosenfeld, P.J.; Wang, R.K. Quantification of Choriocapillaris with Optical Coherence Tomography Angiography: A Comparison Study. Am. J. Ophthalmol. 2019, 208, 111–123. [Google Scholar] [CrossRef]
- Nassisi, M.; Baghdasaryan, E.; Borrelli, E.; Ip, M.; Sadda, S.R. Choriocapillaris flow impairment surrounding geographic atrophy correlates with disease progression. PLoS ONE 2019, 14, e0212563. [Google Scholar] [CrossRef] [PubMed]
- Treister, A.D.; Nesper, P.L.; Fayed, A.E.; Gill, M.K.; Mirza, R.G.; Fawzi, A.A. Prevalence of Subclinical CNV and Choriocapillaris Nonperfusion in Fellow Eyes of Unilateral Exudative AMD on OCT Angiography. Transl. Vis. Sci. Technol. 2018, 7, 19. [Google Scholar] [CrossRef]
- de Oliveira Dias, J.R.; Zhang, Q.; Garcia, J.M.B.; Zheng, F.; Motulsky, E.H.; Roisman, L.; Miller, A.; Chen, C.L.; Kubach, S.; de Sisternes, L.; et al. Natural History of Subclinical Neovascularization in Nonexudative Age-Related Macular Degeneration Using Swept-Source OCT Angiography. Ophthalmology 2018, 125, 255–266. [Google Scholar] [CrossRef]





| Patient | Gender | Age | BCVA (logMAR) | BCVA (Snellen Equivalent) | Small Drusen | Large Drusen | Drusenoid PED | Atrophy | Reticular Pseudodrusen | CMT (µm) | CT (µm) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 72 | 0.1 | 20/25 | 1 | 1 | 1 | 0 | 1 | 252 | 257 |
| 2 | Female | 78 | 0.0 | 20/20 | 0 | 0 | 1 | 0 | 0 | 211 | 139 |
| 3 | Male | 80 | 0.2 | 20/32 | 0 | 0 | 1 | 0 | 0 | 338 | 136 |
| 4 | Male | 82 | 0.1 | 20/25 | 0 | 0 | 0 | 0 | 0 | 249 | 289 |
| 5 | Female | 91 | 0.3 | 20/40 | 1 | 1 | 1 | 0 | 1 | 264 | 243 |
| 6 | Female | 72 | 0.1 | 20/25 | 1 | 1 | 1 | 0 | 1 | 244 | 382 |
| 7 | Female | 89 | 0.2 | 20/32 | 0 | 0 | 1 | 0 | 1 | 239 | 268 |
| 8 | Female | 88 | 0.0 | 20/20 | 0 | 1 | 1 | 0 | 0 | 204 | 102 |
| Non-Neovascular Study Eyes (n = 89) | Neovascular † Study Eyes (n = 8) | p-Value | |
|---|---|---|---|
| Mean Age (years) | 79 (±7.70) | 82 (±7.41) | 0.41 * |
| BCVA (logMAR) | 0.18 (±0.46) | 0.12 (±0.10) | 0.21 * |
| Small drusen (n,%) | 59 (66.29%) | 3 (37.5%) | 0.13 ** |
| Large drusen (n,%) | 65 (73.03%) | 4 (50%) | 0.22 ** |
| Drusenoid PED (n,%) | 37 (41.57%) | 7 (87.50%) | 0.021 ** |
| Reticular pseudodrusen (n,%) | 50 (56.18%) | 4 (50%) | 1.0 ** |
| Atrophy (n,%) | 19 (21.35%) | 0 (0%) | 0.34 ** |
| CMT (µm) | 231.95 (±43.74) | 250.13 (±40.95) | 0.20 * |
| CT (µm) | 209.09 (±83.04) | 227 (±94.38) | 0.63 * |
| Mean (SD) | |
|---|---|
| Percentage of flow deficits (%) | 45.84 (±11.63) |
| Number of flow deficits | 1964.74 (±1063.19) |
| Size of flow deficits (µm2) | 5076.49 µm2 (±9984.51) |
| Area of flow deficits (mm2) | 4.19 (±1.12) |
| Linear Regression on | Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|---|
| Coef. † | Std. Err. | p Value | Coef. † | Std. Err. | p Value | ||
| Percentage of flow deficits * | Age * | 0.77 | 0.26 | 0.004 | 0.62 | 0.26 | 0.02 |
| CMT * | −0.04 | 0.07 | 0.59 | ||||
| CT * | −0.16 | 0.05 | 0.003 | ||||
| Small drusen | 0.03 | 0.05 | 0.55 | −0.13 | 0.05 | 0.017 | |
| Large drusen | 0.12 | 0.06 | 0.03 | ||||
| Drusenoid PED | 0.09 | 0.05 | 0.09 | ||||
| Atrophy | 0.14 | 0.06 | 0.02 | ||||
| RPD | 0.14 | 0.05 | 0.007 | ||||
| Size of flow deficits * | Age * | 3.44 | 1.13 | 0.003 | 2.69 | 1.13 | 0.019 |
| CMT * | −0.15 | 0.32 | 0.64 | ||||
| CT * | −0.81 | 0.23 | 0.001 | −0.68 | 0.23 | 0.005 | |
| Small drusen | 0.16 | 0.24 | 0.49 | ||||
| Large drusen | 0.47 | 0.25 | 0.07 | ||||
| Drusenoid PED | 0.34 | 0.23 | 0.13 | ||||
| Atrophy | 0.61 | 0.27 | 0.029 | ||||
| RPD | 0.53 | 0.22 | 0.02 | ||||
| Number of flow deficits * | Age * | −2.74 | 0.80 | 0.001 | −2.25 | 0.80 | 0.007 |
| CMT * | 0.12 | 0.23 | 0.59 | ||||
| CT * | 0.57 | 0.17 | 0.001 | 0.46 | 0.17 | 0.008 | |
| Small drusen | −0.05 | 0.17 | 0.76 | ||||
| Large drusen | −0.24 | 0.18 | 0.19 | ||||
| Drusenoid PED | −0.21 | 0.16 | 0.21 | ||||
| Atrophy | −0.43 | 0.19 | 0.03 | ||||
| RPD | −0.33 | 0.16 | 0.048 | ||||
| Mean (SD) Radius 4 | Mean (SD) Radius 8 | Mean (SD) Radius 10 | Mean (SD) Radius 15 Pixel | |
|---|---|---|---|---|
| Percentage of flow deficits (%) | 41.74 (±15.26) | 44.81 (±12.43) | 45.52 (±12.01) | 45.84 (±11.63) |
| Number of flow deficits | 3381.08 (±1735.01) | 2405.87 (±1347.19) | 2151.26 (±1218.96) | 1964.74 (±1063.19) |
| Size of flow deficits (µm2) | 4198.77 (±14,929.13) | 5253.17 (±13,861.42) | 5548.82 (±13,471.32) | 5076.49 (±9984.51) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khorrami Kashi, A.; Souied, E.; Fares, S.; Borrelli, E.; Capuano, V.; Jung, C.; Querques, G.; Mouallem, A.; Miere, A. The Spectrum of Central Choriocapillaris Abnormalities on Swept-Source Optical Coherence Tomography Angiography in the Fellow Eye of Unilateral Exudative Age-Related Macular Degeneration Patients: From Flow Deficits to Subclinical Non-Exudative Neovascularization. J. Clin. Med. 2021, 10, 2658. https://doi.org/10.3390/jcm10122658
Khorrami Kashi A, Souied E, Fares S, Borrelli E, Capuano V, Jung C, Querques G, Mouallem A, Miere A. The Spectrum of Central Choriocapillaris Abnormalities on Swept-Source Optical Coherence Tomography Angiography in the Fellow Eye of Unilateral Exudative Age-Related Macular Degeneration Patients: From Flow Deficits to Subclinical Non-Exudative Neovascularization. Journal of Clinical Medicine. 2021; 10(12):2658. https://doi.org/10.3390/jcm10122658
Chicago/Turabian StyleKhorrami Kashi, Alexis, Eric Souied, Selim Fares, Enrico Borrelli, Vittorio Capuano, Camille Jung, Giuseppe Querques, Alexandra Mouallem, and Alexandra Miere. 2021. "The Spectrum of Central Choriocapillaris Abnormalities on Swept-Source Optical Coherence Tomography Angiography in the Fellow Eye of Unilateral Exudative Age-Related Macular Degeneration Patients: From Flow Deficits to Subclinical Non-Exudative Neovascularization" Journal of Clinical Medicine 10, no. 12: 2658. https://doi.org/10.3390/jcm10122658
APA StyleKhorrami Kashi, A., Souied, E., Fares, S., Borrelli, E., Capuano, V., Jung, C., Querques, G., Mouallem, A., & Miere, A. (2021). The Spectrum of Central Choriocapillaris Abnormalities on Swept-Source Optical Coherence Tomography Angiography in the Fellow Eye of Unilateral Exudative Age-Related Macular Degeneration Patients: From Flow Deficits to Subclinical Non-Exudative Neovascularization. Journal of Clinical Medicine, 10(12), 2658. https://doi.org/10.3390/jcm10122658







