Risk Factors for and Frequency of CT Scans, Steroid Use, and Repeat Visits in Inflammatory Bowel Disease Patients Seen at a Single-Center Emergency Department: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design/Patient Population
2.2. Data Collection
2.3. Statistical Analysis
2.4. Ethical Considerations
3. Results
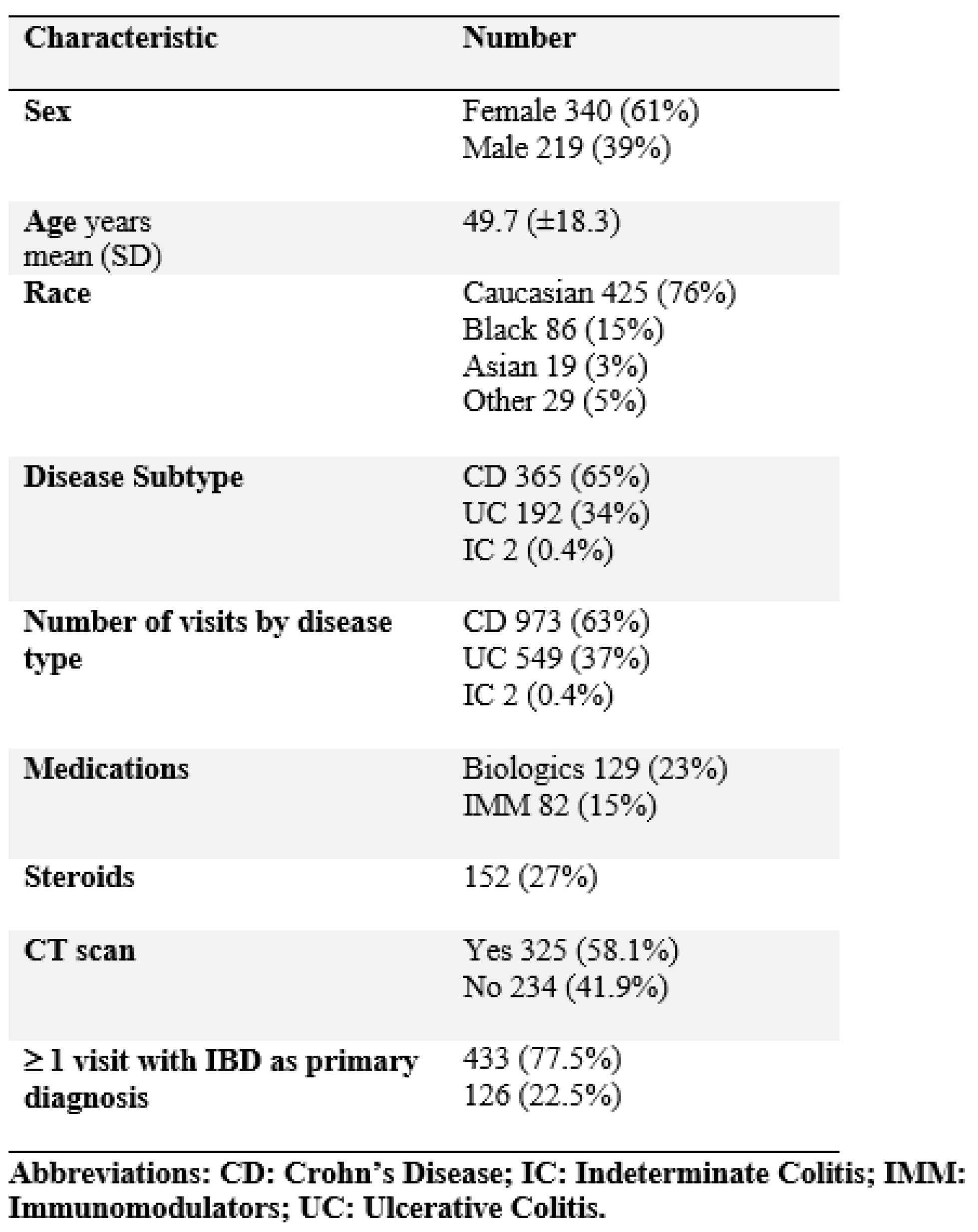
3.1. Patient Characteristics
3.2. Repeated Visits to the Emergency Department
3.3. CT Scans
3.4. Steroid Utilization
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; E Underwood, F.; Tang, W.; I Benchimol, E.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. Lancet 2017, 390, 2769–2778. [Google Scholar] [CrossRef]
- The Facts about Inflammatory Bowel Diseases; Crohn’s and Colitis Foundation of America: New York, NY, USA, 2014; Available online: http://www.crohnscolitisfoundation.org/assets/pdfs/updatedibdfactbook.pdf (accessed on 11 March 2019).
- Park, K.T.; Ehrlich, O.G.; I Allen, J.; Meadows, P.; Szigethy, E.M.; Henrichsen, K.; Kim, S.C.; Lawton, R.C.; Murphy, S.M.; Regueiro, M.; et al. The cost of inflammatory bowel disease: An initiative from the Crohn’s and Colitis foundation. Inflamm. Bowel Dis. 2019, 26, izz104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loftus, E.V., Jr.; Shivashankar, R.; Tremaine, W.J.; Harmsen, W.S.; Zinsmeiseter, A.R. Updated incidence and prevalence of Crohn’s Disease and ulcerative colitis in Olmsted County, Minnesota (1970–2011). In Proceedings of the ACG 2014 Annual Scientific Meeting, Philadelphia, PA, USA, 17–22 October 2014. [Google Scholar]
- Kappelman, M.D.; Rifas–Shiman, S.L.; Porter, C.Q.; Ollendorf, D.A.; Sandler, R.S.; Galanko, J.A.; Finkelstein, J.A. Direct Health Care Costs of Crohn’s Disease and Ulcerative Colitis in US Children and Adults. Gastroenterology 2008, 135, 1907–1913. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peery, A.F.; Crockett, S.D.; Murphy, C.C.; Lund, J.L.; Dellon, E.S.; Williams, J.L.; Jensen, E.T.; Shaheen, N.J.; Barritt, A.S.; Lieber, S.R.; et al. Burden and Cost of Gastrointestinal, Liver, and Pancreatic Diseases in the United States: Update 2018. Gastroenterology 2019, 156, 254–272.e11. [Google Scholar] [CrossRef] [Green Version]
- Ruhl, C.E.; Sayer, B.; Byrd-Holt, D.D.; Brown, D.M.; Everhart, J.E. (Eds.) The Burden of Digestive Diseases in the United States. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; NIH Publication No. 09-6443; US Government Printing Office: Washington, DC, USA, 2008; pp. 137–147.
- Ballou, S.; Hirsch, W.; Singh, P.; Rangan, V.; Nee, J.; Iturrino, J.; Sommers, T.; Zubiago, J.; Sengupta, N.; Bollom, A.; et al. Emergency department utilization for inflammatory bowel disease in the United States from 2006 to 2014. Aliment. Pharmacol. Ther. 2018, 47, 913–921. [Google Scholar] [CrossRef] [Green Version]
- Nugent, Z.; Singh, H.; Targownik, L.E.; Strome, T.; Snider, C.; Bernstein, C.N. Predictors of Emergency Department Use by Persons with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2016, 22, 2907–2916. [Google Scholar] [CrossRef] [Green Version]
- Huh, G.; Yoon, H.; Choi, Y.J.; Shin, C.M.; Park, Y.S.; Kim, N.; Lee, D.H.; Kim, J.S. Trends in emergency department visits and hospitalization rates for inflammatory bowel disease in the era of biologics. PLoS ONE 2019, 14, e0210703. [Google Scholar] [CrossRef]
- Yarur, A.J.; Mandalia, A.B.; Dauer, R.M.; Czul, F.; Deshpande, A.R.; Kerman, D.H.; Abreu, M.T.; A Sussman, D. Predictive factors for clinically actionable computed tomography findings in inflammatory bowel disease patients seen in the emergency department with acute gastrointestinal symptoms. J. Crohns.Colitis. 2014, 8, 504–512. [Google Scholar] [CrossRef] [Green Version]
- Israeli, E.; Ying, S.; Henderson, B.; Mottola, J.; Strome, T.; Bernstein, C.N. The impact of abdominal computed tomography in a tertiary referral centre emergency department on the management of patients with inflammatory bowel disease. Aliment. Pharmacol. Ther. 2013, 38, 513–521. [Google Scholar] [CrossRef]
- Jung, Y.S.; Park, D.I.; Hong, S.N.; Kim, E.R.; Kim, Y.H.; Cheon, J.H.; Eun, C.S.; Han, D.S.; Lee, C.K.; Kim, J.H.; et al. Predictors of urgent findings on abdominopelvic CT in patients with Crohn’s disease presenting to the emergency department. Dig. Dis. Sci. 2015, 60, 929–935. [Google Scholar] [CrossRef]
- Kerner, C.; Carey, K.; Mills, A.M.; Yang, W.; Synnestvedt, M.B.; Hilton, S.; Weiner, M.G.; Lewis, J.D. Use of abdominopelvic computed tomography in emergency departments and rates of urgent diagnoses in Crohn’s disease. Clin. Gastroenterol. Hepatol. 2012, 10, 52–57. [Google Scholar] [CrossRef] [Green Version]
- Desmond, A.N.; O’Regan, K.; Curran, C.; McWilliams, S.; Fitzgerald, T.; Maher, M.M.; Shanahan, F. Crohn’s disease: Factors associated with exposure to high levels of diagnostic radiation. Gut 2008, 57, 1524–1529. [Google Scholar] [CrossRef]
- Kerner, C.; Carey, K.; Baillie, C.; Mills, A.M.; Yang, W.; Hilton, S.; Synnestvedt, M.B.; Weiner, M.G.; Lewis, J.D. Clinical predictors of urgent findings on abdominopelvic CT in emergency department patients with Crohn’s disease. Inflamm. Bowel Dis. 2013, 19, 1179–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Longobardi, T.; Jacobs, P.; Bernstein, C.N. Utilization of health care resources by individuals with inflammatory bowel disease in the United States: A profile of time since diagnosis. Am. J. Gastroenterol. 2004, 99, 650–655. [Google Scholar] [CrossRef] [PubMed]
- Kappelman, M.D.; Porter, C.Q.; Galanko, J.A.; Rifas-Shiman, S.L.; Ollendorf, D.A.; Sandler, R.S.; Finkelstein, J.A. Utilization of healthcare resources by U.S. children and adults with inflammatory bowel disease. Inflamm. Bowel Dis. 2011, 17, 62–68. [Google Scholar] [CrossRef]
- Meltzer, A.C.; Pines, J.M.; Richards, L.; Mullins, P.; Mazer-Amirshahi, M. US emergency department visits for adults with abdominal and pelvic pain (2007–13): Trends in demographics, resource utilization and medication usage. Am. J. Emerg. Med. 2017, 35, 1966–1969. [Google Scholar] [CrossRef] [PubMed]
- Brenner, D.J.; Hall, E.J. Computed tomography—An increasing source of radiation exposure. N. Engl. J. Med. 2007, 357, 2277–2284. [Google Scholar] [CrossRef] [Green Version]
- Preston, D.L.; Pierce, D.A.; Shimizu, Y.; Cullings, H.M.; Fujita, S.; Funamoto, S.; Kodama, K. Effect of recent changes in atomic bomb survivor dosimetry on cancer mortality risk estimates. Radiat. Res. 2004, 162, 377–389. [Google Scholar] [CrossRef]
- Preston, D.L.; Ron, E.; Tokuoka, S.; Funamoto, S.; Nishi, N.; Soda, M.; Mabuchi, K.; Kodama, K. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat. Res. 2007, 168, 1–64. [Google Scholar] [CrossRef]
- Preston, D.L.; Shimizu, Y.; Pierce, D.A.; Suyama, A.; Mabuchi, K. Studies of mortality of atomic bomb survivors. Report 13: Solid cancer and noncancer disease mortality: 1950–1997. Radiat. Res. 2003, 160, 381–407. [Google Scholar] [CrossRef]
- Linet, M.S.; Slovis, T.L.; Miller, D.L.; Kleinerman, R.; Lee, C.; Rajaraman, P.; De Gonzalez, A.B. Cancer risks associated with external radiation from diagnostic imaging procedures. CA Cancer J. Clin. 2012, 62, 75–100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, W.; Tang, Y.; Nong, L.; Sun, Y. Risk factors for postoperative intra-abdominal septic complications after surgery in Crohn’s disease: A meta-analysis of observational studies. J. Crohns Colitis 2015, 9, 293–301. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agrawal, A.; Durrani, S.; Leiper, K.; Ellis, A.; Morris, A.I.; Rhodes, J.M. Effect of systemic corticosteroid therapy on risk for intra-abdominal or pelvic abscess in non-operated Crohn’s disease. Clin. Gastroenterol. Hepatol. 2005, 3, 1215–1220. [Google Scholar] [CrossRef]
- Nguyen, G.C.; A LaVeist, T.; Harris, M.L.; Wang, M.-H.; Datta, L.W.; Brant, S.R. Racial disparities in utilization of specialist care and medications in inflammatory bowel disease. Am. J. Gastroenterol. 2010, 105, 2202–2208. [Google Scholar] [CrossRef] [PubMed]
- Rahman, A.; Jairath, V.; Feagan, B.G.; Khanna, R.; Shariff, S.Z.; Allen, B.N.; Jenkyn, K.B.; Vinden, C.; Jeyarajah, J.; Mosli, M.; et al. Declining hospitalization and surgical intervention rates in patients with Crohn’s disease: A population-based cohort. Aliment. Pharmacol. Ther. 2019, 50, 1086–1093. [Google Scholar] [CrossRef]
- Govani, S.M.; Higgins, P.D.R.; Rubenstein, J.H.; Stidham, R.W.; Waljee, A.K. CT utilization abruptly increases at age 18 among patients with inflammatory bowel diseases in the hospital. PLoS ONE 2018, 13, e0195022. [Google Scholar] [CrossRef]
- De González, A.B.; Mahesh, M.; Kim, K.-P.; Bhargavan, M.; Lewis, R.; Mettler, F.; Land, C. Projected Cancer Risks From Computed Tomographic Scans Performed in the United States in 2007. Arch. Intern. Med. 2009, 169, 2071–2077. [Google Scholar] [CrossRef]
- Shao, Y.-H.; Tsai, K.; Kim, S.; Wu, Y.-J.; Demissie, K. Exposure to Tomographic Scans and Cancer Risks. JNCI Cancer Spectr. 2020, 4, pkz072. [Google Scholar] [CrossRef]
- Griffey, R.T.; Fowler, K.J.; Theilen, A.; Gutierrez, A. Considerations in Imaging Among Emergency Department Patients With Inflammatory Bowel Disease. Ann. Emerg. Med. 2017, 69, 587–599. [Google Scholar] [CrossRef]
- Benchimol, E.I.; Seow, C.H.; Steinhart, A.H.; Griffiths, A.M. Traditional corticosteroids for induction of remission in Crohn’s disease. Cochrane Database Syst. Rev. 2008, 2008, CD006792. [Google Scholar] [CrossRef]
- Nguyen, N.H.; Fumery, M.; Dulai, P.S.; Prokop, L.J.; Sandborn, W.J.; Murad, M.H.; Singh, S. Comparative efficacy and tolerability of pharmacological agents for management of mild to moderate ulcerative colitis: A systematic review and network meta-analyses. Lancet Gastroenterol. Hepatol. 2018, 3, 742–753. [Google Scholar] [CrossRef]
- Rezaie, A.; Kuenzig, M.E.; I Benchimol, E.; Griffiths, A.M.; Otley, A.R.; Steinhart, A.H.; Kaplan, G.G.; Seow, C.H. Budesonide for induction of remission in Crohn’s disease. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- E Sherlock, M.; Macdonald, J.K.; Griffiths, A.M.; Steinhart, A.H.; Seow, C.H. Oral budesonide for induction of remission in ulcerative colitis. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Rice, J.B.; White, A.G.; Scarpati, L.M.; Wan, G.; Nelson, W.W. Long-term Systemic Corticosteroid Exposure: A Systematic Literature Review. Clin. Ther. 2017, 39, 2216–2229. [Google Scholar] [CrossRef] [Green Version]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Euers, L.; Abughazaleh, S.; Glassner, K.; Gajula, P.; Jones-Pauley, M.; Ezeana, C.; Puppala, M.; Wang, L.; Wong, S.; Oglat, A.; et al. Risk Factors for and Frequency of CT Scans, Steroid Use, and Repeat Visits in Inflammatory Bowel Disease Patients Seen at a Single-Center Emergency Department: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 2679. https://doi.org/10.3390/jcm10122679
Euers L, Abughazaleh S, Glassner K, Gajula P, Jones-Pauley M, Ezeana C, Puppala M, Wang L, Wong S, Oglat A, et al. Risk Factors for and Frequency of CT Scans, Steroid Use, and Repeat Visits in Inflammatory Bowel Disease Patients Seen at a Single-Center Emergency Department: A Retrospective Cohort Study. Journal of Clinical Medicine. 2021; 10(12):2679. https://doi.org/10.3390/jcm10122679
Chicago/Turabian StyleEuers, Lindsay, Shaadi Abughazaleh, Kerri Glassner, Prianka Gajula, Michelle Jones-Pauley, Chika Ezeana, Mamta Puppala, Lin Wang, Stephen Wong, Ayah Oglat, and et al. 2021. "Risk Factors for and Frequency of CT Scans, Steroid Use, and Repeat Visits in Inflammatory Bowel Disease Patients Seen at a Single-Center Emergency Department: A Retrospective Cohort Study" Journal of Clinical Medicine 10, no. 12: 2679. https://doi.org/10.3390/jcm10122679
APA StyleEuers, L., Abughazaleh, S., Glassner, K., Gajula, P., Jones-Pauley, M., Ezeana, C., Puppala, M., Wang, L., Wong, S., Oglat, A., Nickerson, S., & Abraham, B. P. (2021). Risk Factors for and Frequency of CT Scans, Steroid Use, and Repeat Visits in Inflammatory Bowel Disease Patients Seen at a Single-Center Emergency Department: A Retrospective Cohort Study. Journal of Clinical Medicine, 10(12), 2679. https://doi.org/10.3390/jcm10122679






