Influence of the Gingival Condition on the Performance of Different Gingival Displacement Methods—A Randomized Clinical Study
Abstract
:1. Introduction
2. Materials and Methods
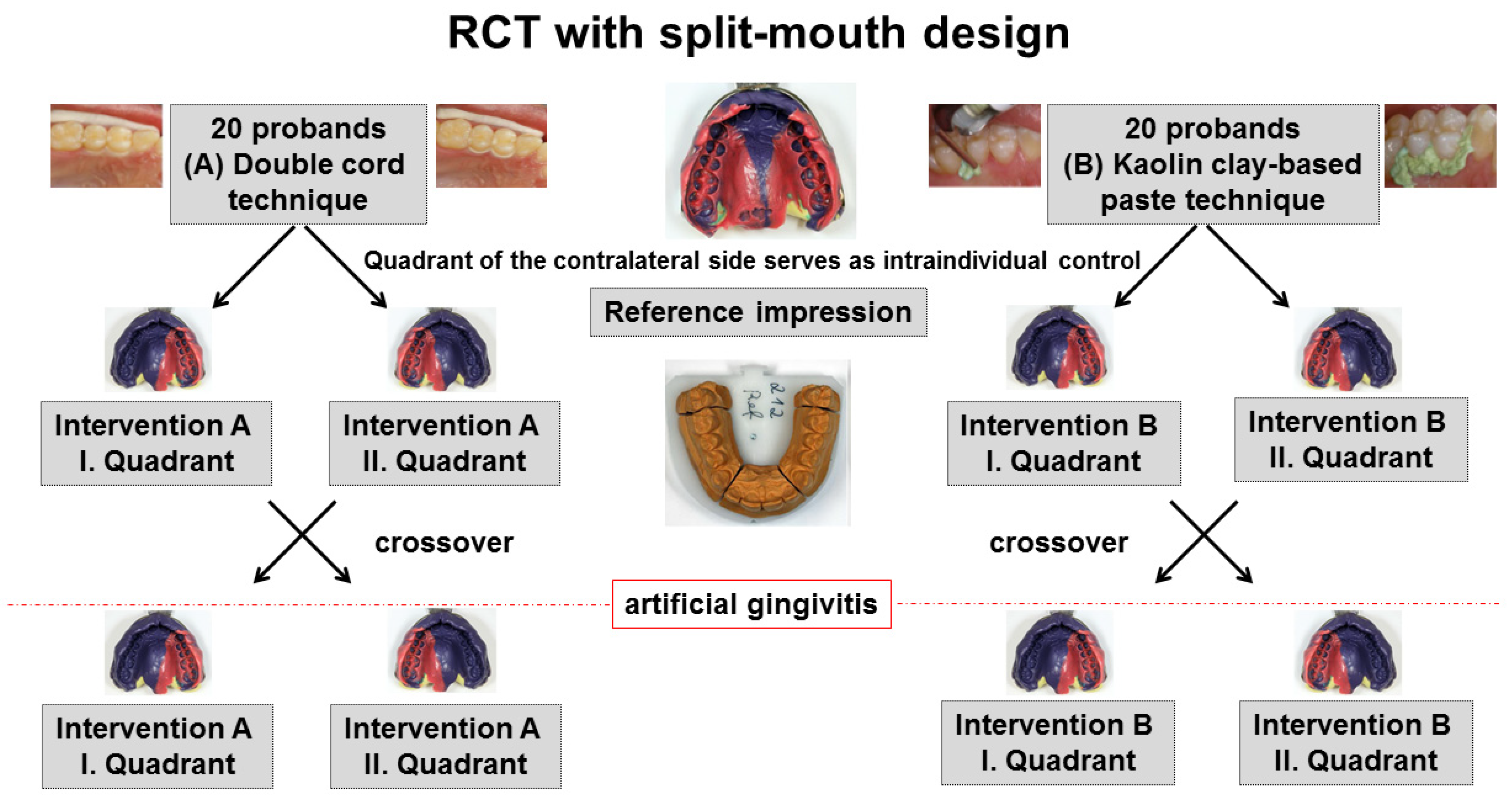
2.1. Trial Design
2.2. Participants
- Between 18 and 80 years of age
- Healthy, not suffering from chronic or acute infections or diseases
- No alcohol or drug abuse
- No known allergies to the materials used (astringent, anesthetics, impression material)
- Presence of both premolars in I. and II. quadrants in the upper jaw with their adjacent teeth
- Premolars and adjacent teeth in upper jaw naturally healthy or restored in a defect-free state with restoration margins located at least 1 mm supragingivally
- Legally competent
- Pregnancy
- Smoker
- Upper premolar restored with full-coverage crown
- Periodontal Screening Index (PSI; definition by the German Society for Periodontology) above 2 in at least one sextant
2.3. Interventions
2.3.1. Intervention A
2.3.2. Intervention B
2.4. Outcomes
2.4.1. Sulcus Representation
2.4.2. Marginal Gingiva Height
2.5. Sample Size
2.6. Randomisation
2.7. Blinding
2.8. Statistical Methods
- Point in time (including the gingival condition (healthy/mildly inflamed))
- Tooth (first/second premolar)
- Quadrant (first/second quadrant)
- Intervention (yes/no)
- Gender (female/male)
- GI-value
- PSI-value
- Maximum pocket depth (out of six-point pocket measurements)
3. Results
3.1. Participant Flow
3.2. Recruitment
3.3. Baseline Data
3.4. Numbers Analyzed
- Two values (both premolars) for the control quadrant for B (paste group) at the 3-month follow-up visit after the second intervention.
- Two values (both premolars) for the intervention quadrant for A (cord group) at the 6-month follow-up visit after the second intervention.
- GI value of 2 at the first intervention (A: two probands; B: one proband)
- GI of 1 at the second intervention (A: two probands; B: four probands)
3.5. Outcomes
3.5.1. Sulcus Representation (Primary Outcome), t-Test for Dependent Samples
Influence of an Intervention Performed
Influence of the Gingival Displacement Method
Influence of Gingival Condition
3.5.2. Sulcus Representation (Primary Outcome)-Regression Analysis
Regression Analysis Excluding Cases with Strongly Deviated GI
3.5.3. Marginal Gingiva Height Change (Secondary Outcome)-t-Test for Dependent Samples
3.6. Ancillary Analyses
3.7. Harms
4. Discussion
5. Conclusions
- For healthy gingiva, the cord technique achieved a better gingival displacement in vertical direction (sulcus representation) than the paste technique, with the impression material flowing deeper into the sulcus for the cord technique.
- Mild gingivitis worsened the sulcus representation when using the cord technique but had no influence on the sulcus representation of the paste technique. This means that the advantage of the cord technique with regard to a better sulcus representation was lost to a great extent under the condition of mild gingivitis.
- Neither cord nor paste technique showed—with gentle application in this study—permanent gingival recessions at the palatal study sites up to six months, neither for healthy nor for mildly inflamed gingiva.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benson, B.W.; Bomberg, T.J.; Hatch, R.A.; Hoffman, W., Jr. Tissue displacement methods in fixed prosthodontics. J. Prosthet. Dent. 1986, 55, 175–181. [Google Scholar] [CrossRef]
- Bennani, V.; Aarts, J.M.; Brunton, P. A randomized controlled clinical trial comparing the use of displacement cords and aluminum chloride paste. J. Esthet. Restor. Dent. 2020, 32, 410–415. [Google Scholar] [CrossRef]
- Einarsdottir, E.R.; Lang, N.P.; Aspelund, T.; Pjetursson, B.E. A multicenter randomized, controlled clinical trial comparing the use of displacement cords, an aluminum chloride paste, and a combination of paste and cords for tissue displacement. J. Prosthet. Dent. 2018, 119, 82–88. [Google Scholar] [CrossRef]
- Ferrari Cagidiaco, E.; Zarone, F.; Discepoli, N.; Joda, T.; Ferrari, M. Analysis of The Reproducibility of Subgingival Vertical Margins Using Intraoral Optical Scanning (IOS): A Randomized Controlled Pilot Trial. J. Clin. Med. 2021, 10, 941. [Google Scholar] [CrossRef] [PubMed]
- Safari, S.; Vossoghi, S.M.; Vossoghi, S.M.; Hoseini, G.F.; Hamedi, M. Gingival Retraction Methods for Fabrication of Fixed Partial Denture: Literature Review. J. Dent. Biomater. 2016, 3, 205–213. [Google Scholar]
- Donaldson, M.; Goodchild, J.H. Local and systemic effects of mechanico-chemical retraction. Compend. Contin. Educ. Dent. 2013, 34, 1–7. [Google Scholar]
- Baba, N.Z.; Goodacre, C.J.; Jekki, R.; Won, J. Gingival displacement for impression making in fixed prosthodontics: Contemporary principles, materials, and techniques. Dent. Clin. N. Am. 2014, 58, 45–68. [Google Scholar] [CrossRef]
- Chaudhari, J.; Prajapati, P.; Patel, J.; Sethuraman, R.; Naveen, Y.G. Comparative evaluation of the amount of gingival displacement produced by three different gingival retraction systems: An in vivo study. Contemp. Clin. Dent. 2015, 6. [Google Scholar] [CrossRef]
- Huang, C.; Somar, M.; Li, K.; Mohadeb, J.V.N. Efficiency of Cordless Versus Cord Techniques of Gingival Retraction: A Systematic Review. J. Prosthodont. 2017, 26, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Martins, F.V.; Santana, R.B.; Fonseca, E.M. Efficacy of conventional cord versus cordless techniques for gingival displacement: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 46–55. [Google Scholar] [CrossRef]
- Shrivastava, K.J.; Bhoyar, A.; Agarwal, S.; Shrivastava, S.; Parlani, S.; Murthy, V. Comparative clinical efficacy evaluation of three gingival displacement systems. J. Nat. Sci. Biol. Med. 2015, 6, S53–S57. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Fan, F.; Li, X.; Zhou, Q.; He, B.; Huang, X.; Ma, J. Influence of gingival retraction paste versus cord on periodontal health: A systematic review and meta-analysis. Quintessence Int. 2019, 50, 234–244. [Google Scholar] [CrossRef]
- Jain, A.R.; Nallaswamy, D. Comparison of gingival retraction produced by retraction cord and expasyl retraction systems—An in vivo study. Drug. Invention Today 2018, 10, 35–41. [Google Scholar]
- Kazemi, M.; Memarian, M.; Loran, V. Comparing the Effectiveness of Two Gingival Retraction Procedures on Gingival Recession and Tissue Displacement: Clinical Study. Res. J. Biol. Sci. 2009, 4, 335–339. [Google Scholar]
- Yang, J.-C.; Tsai, C.-M.; Chen, M.-S.; Wei, J.Y.; Lee, S.-Y.; Lin, C.-T. Clinical study of a newly developed injection-type gingival retraction material. Chin. Dent. J. 2005, 24, 147–151. [Google Scholar] [CrossRef]
- Sarmento, H.R.; Leite, F.R.; Dantas, R.V.; Ogliari, F.A.; Demarco, F.F.; Faot, F. A double-blind randomised clinical trial of two techniques for gingival displacement. J. Oral Rehabil. 2014, 41, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Chandra, S.; Singh, A.; Gupta, K.K.; Chandra, C.; Arora, V. Effect of gingival displacement cord and cordless systems on the closure, displacement, and inflammation of the gingival crevice. J. Prosthet. Dent. 2016, 115, 177–182. [Google Scholar] [CrossRef]
- Gajbhiye, V.; Banerjee, R.; Jaiswal, P.; Chandak, A.; Radke, U. Comparative evaluation of three gingival displacement materials for efficacy in tissue management and dimensional accuracy. J. Indian Prosthodont. Soc. 2019, 19, 173–179. [Google Scholar] [CrossRef]
- Goutham, G.B.; Jayanti, I.; Jalaluddin, M.; Avijeeta, A.; Ramanna, P.K.; Joy, J. Clinical Assessment of Gingival Sulcus Width using Various Gingival Displacement Materials. J. Contemp. Dent. Pract. 2018, 19, 502–506. [Google Scholar] [CrossRef] [PubMed]
- Kesari, Z.I.; Karani, J.T.; Mistry, S.S.; Pai, A.R. A comparative evaluation of amount of gingival displacement produced by four different gingival displacement agents—An in vivo study. J. Indian Prosthodont. Soc. 2019, 19, 313–323. [Google Scholar] [CrossRef]
- Mehta, S.; Virani, H.; Memon, S.; Nirmal, N. A Comparative Evaluation of Efficacy of Gingival Retraction Using Polyvinyl Siloxane Foam Retraction System, Vinyl Polysiloxane Paste Retraction System, and Copper Wire Reinforced Retraction Cord in Endodontically Treated Teeth: An in vivo Study. Contemp. Clin. Dent. 2019, 10, 428–432. [Google Scholar] [CrossRef]
- Tabassum, S.; Adnan, S.; Khan, F.R. Gingival Retraction Methods: A Systematic Review. J. Prosthodont. 2017, 26, 637–643. [Google Scholar] [CrossRef]
- Thimmappa, M.; Bhatia, M.; Somani, P.; Kumar, D.R.V. Comparative evaluation of three noninvasive gingival displacement systems: An in vivo study. J. Indian Prosthodont. Soc. 2018, 18, 122–130. [Google Scholar] [CrossRef]
- Loe, H. The Gingival Index, the Plaque Index and the Retention Index Systems. J. Periodontol. 1967, 38, 610–616. [Google Scholar] [CrossRef]
- Sorensen, J.A.; Doherty, F.M.; Newman, M.G.; Flemmig, T.F. Gingival enhancement in fixed prosthodontics. Part. I: Clinical findings. J. Prosthet. Dent. 1991, 65, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Luthardt, R.G.; Stossel, M.; Hinz, M.; Vollandt, R. Clinical performance and periodontal outcome of temporary crowns and fixed partial dentures: A randomized clinical trial. J. Prosthet. Dent. 2000, 83, 32–39. [Google Scholar] [CrossRef]
- Gupta, A.; Prithviraj, D.R.; Gupta, D.; Shruti, D.P. Clinical evaluation of three new gingival retraction systems: A research report. J. Indian Prosthodont. Soc. 2013, 13, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Rayyan, M.M.; Hussien, A.N.M.; Sayed, N.M.; Abdallah, R.; Osman, E.; El Saad, N.A.; Ramadan, S. Comparison of four cordless gingival displacement systems: A clinical study. J. Prosthet. Dent. 2019, 121, 265–270. [Google Scholar] [CrossRef]
- Shivasakthy, M.; Ali, S.A. Comparative Study on the Efficacy of Gingival Retraction using Polyvinyl Acetate Strips and Conventional Retraction Cord—An in Vivo Study. J. Clin. Diagn. Res. 2013, 7, 2368–2371. [Google Scholar] [CrossRef]
- Acar, O.; Erkut, S.; Ozcelik, T.B.; Ozdemir, E.; Akcil, M. A clinical comparison of cordless and conventional displacement systems regarding clinical performance and impression quality. J. Prosthet. Dent. 2014, 111, 388–394. [Google Scholar] [CrossRef]
- Zemouri, C.; Jakubovics, N.S.; Crielaard, W.; Zaura, E.; Dodds, M.; Schelkle, B.; Loos, B.G. Resistance and resilience to experimental gingivitis: A systematic scoping review. BMC Oral Health 2019, 19, 212. [Google Scholar] [CrossRef]
- Bostanci, N.; Silbereisen, A.; Bao, K.; Grossmann, J.; Nanni, P.; Fernandez, C.; Lopez, R. Salivary proteotypes of gingivitis tolerance and resilience. J. Clin. Periodontol. 2020, 47, 1304–1316. [Google Scholar] [CrossRef]
- Jonsson, D.; Ramberg, P.; Demmer, R.T.; Kebschull, M.; Dahlen, G.; Papapanou, P.N. Gingival tissue transcriptomes in experimental gingivitis. J. Clin. Periodontol. 2011, 38, 599–611. [Google Scholar] [CrossRef]
- Nascimento, G.G.; Danielsen, B.; Baelum, V.; Lopez, R. Identification of inflammatory response patterns in experimental gingivitis studies. Eur. J. Oral Sci. 2019, 127, 33–39. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Offenbacher, S.; Barros, S.; Mendoza, L.; Mauriello, S.; Preisser, J.; Moss, K.; Aspiras, M. Changes in gingival crevicular fluid inflammatory mediator levels during the induction and resolution of experimental gingivitis in humans. J. Clin. Periodontol. 2010, 37, 324–333. [Google Scholar] [CrossRef] [Green Version]
- Wellappuli, N.C.; Fine, N.; Lawrence, H.P.; Goldberg, M.; Tenenbaum, H.C.; Glogauer, M. Oral and Blood Neutrophil Activation States during Experimental Gingivitis. JDR Clin. Trans. Res. 2018, 3, 65–75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baharav, H.; Laufer, B.Z.; Langer, Y.; Cardash, H.S. The effect of displacement time on gingival crevice width. Int. J. Prosthodont. 1997, 10, 248–253. [Google Scholar] [PubMed]
- Laufer, B.-Z.; Baharav, H.; Langer, Y.; Cardash, H.S. The closure of the gingival crevice following gingival retraction for impression making. J. Oral Rehabil. 1997, 24, 629–635. [Google Scholar] [CrossRef] [PubMed]
- Luthardt, R.G.; Koch, R.; Rudolph, H.; Walter, M.H. Qualitative computer aided evaluation of dental impressions in vivo. Dent. Mater. 2006, 22, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, H.; Rohl, A.; Walter, M.H.; Luthardt, R.G.; Quaas, S. Performance of fast-setting impression materials in the reproduction of subgingival tooth surfaces without soft tissue retraction. Int. J. Prosthodont. 2014, 27, 366–375. [Google Scholar] [CrossRef] [PubMed] [Green Version]








| Group A (Cord; n = 20) (Mean ± SD) | Group B (Paste; n = 20) (Mean ± SD) | p-Value * | |
|---|---|---|---|
| Age (baseline) | 25.85 ± 6.82 | 27.40 ± 9.91 | 0.57 (n.s.) |
| PSI (baseline) | 1.65 ± 0.49 | 1.55 ± 0.61 | 0.57 (n.s.) |
| GI (first intervention, healthy gingiva) | 0.75 ± 0.64 | 0.55 ± 0.61 | 0.32 (n.s.) |
| GI (second intervention; artificial gingivitis) | 1.90 ± 0.31 | 1.80 ± 0.41 | 0.39 (n.s.) |
| Healthy Gingiva | Artificial Gingivitis | |||||
|---|---|---|---|---|---|---|
| Gingival Displacement Method (HG: n = 40; AG: n = 40) | Mean Difference [mm] | LL 95%CI | UL 95%CI | Mean Difference [mm] | LL 95%CI | UL 95%CI |
| Cord | −0.37 | −0.50 | −0.24 | −0.18 | −0.26 | −0.10 |
| Paste | −0.10 | −0.20 | −0.00 | −0.07 | −0.15 | 0.01 |
| Group A (Cord; n = 20) HG versus AG | Group B (Paste; n = 20) HG versus AG | |||
|---|---|---|---|---|
| First premolar | Second premolar | First Premolar | Second Premolar | |
| p-value * | 0.02 | 0.07 (n.s.) | 0.37 (n.s.) | 0.74 (n.s.) |
| Sulcus Representation | Marginal Gingiva Height Change | |
|---|---|---|
| Mean RMS Error ± SD | 14.6 µm ± 4.5 | 20.5 µm ± 8.2 |
| Percentage of RMS Errors Below the Threshold of 32 µm | 100% | 96.3% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuhn, K.; Rudolph, H.; Zügel, D.; Just, B.A.; Hrusa, M.; Martin, T.; Schnutenhaus, S.; Dreyhaupt, J.; Luthardt, R.G. Influence of the Gingival Condition on the Performance of Different Gingival Displacement Methods—A Randomized Clinical Study. J. Clin. Med. 2021, 10, 2747. https://doi.org/10.3390/jcm10132747
Kuhn K, Rudolph H, Zügel D, Just BA, Hrusa M, Martin T, Schnutenhaus S, Dreyhaupt J, Luthardt RG. Influence of the Gingival Condition on the Performance of Different Gingival Displacement Methods—A Randomized Clinical Study. Journal of Clinical Medicine. 2021; 10(13):2747. https://doi.org/10.3390/jcm10132747
Chicago/Turabian StyleKuhn, Katharina, Heike Rudolph, David Zügel, Benjamin A. Just, Michael Hrusa, Thomas Martin, Sigmar Schnutenhaus, Jens Dreyhaupt, and Ralph G. Luthardt. 2021. "Influence of the Gingival Condition on the Performance of Different Gingival Displacement Methods—A Randomized Clinical Study" Journal of Clinical Medicine 10, no. 13: 2747. https://doi.org/10.3390/jcm10132747
APA StyleKuhn, K., Rudolph, H., Zügel, D., Just, B. A., Hrusa, M., Martin, T., Schnutenhaus, S., Dreyhaupt, J., & Luthardt, R. G. (2021). Influence of the Gingival Condition on the Performance of Different Gingival Displacement Methods—A Randomized Clinical Study. Journal of Clinical Medicine, 10(13), 2747. https://doi.org/10.3390/jcm10132747








