Echocardiographic Assessment of Right Ventricular–Arterial Coupling in Predicting Prognosis of Pulmonary Arterial Hypertension Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Population Characteristics
2.2. Echocardiography
2.3. RHC/MRI Hemodynamic Parameters
2.4. Statistical Analysis
3. Results
3.1. General Results
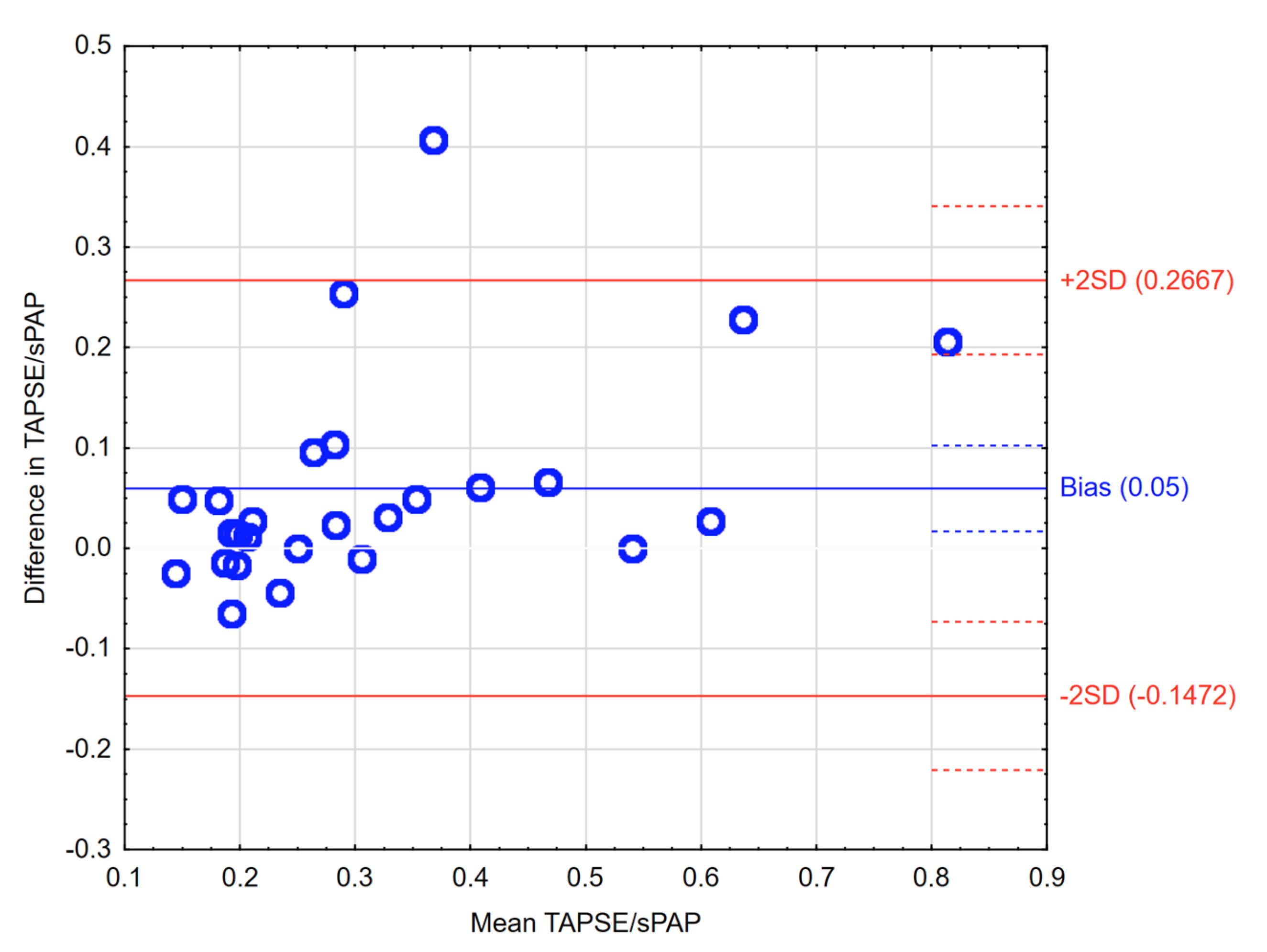
3.2. Echo Parameters and RV Function
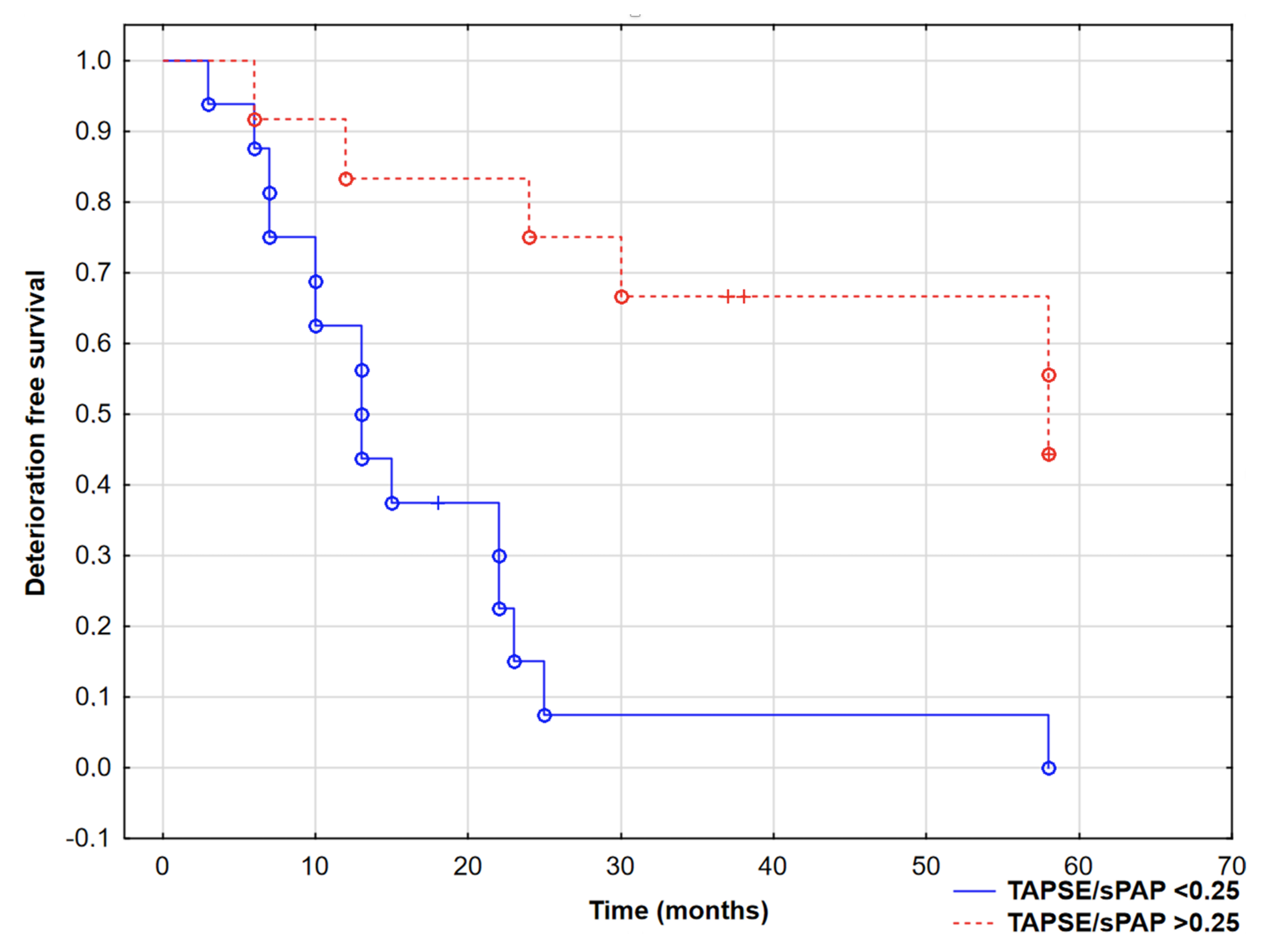
3.3. Survival Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Galiè, N.; Hoeper, M.; Humbert, M.; Torbicki, A.; Vachiery, J.-L.; Barbera, J.A.; Beghetti, M.; Corris, P.; Gaine, S.P.; Gibbs, J.S.; et al. ESC Scientific Document Group. Guidelines for the diagnosis and treatment of pulmonary hypertension: The task force for the diagnosis and treatment of pulmonary hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur. Heart J. 2016, 37, 67–119. [Google Scholar] [PubMed]
- Noordegraaf, A.V.; Chin, K.; Haddad, F.; Hassoun, P.M.; Hemnes, A.R.; Hopkins, S.R.; Kawut, S.M.; Langleben, D.; Lumens, J.; Naeije, R. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: An update. Eur. Respir. 2019, 53, 1801900. [Google Scholar] [CrossRef]
- Noordegraaf, A.V.; Westerhof, B.E.; Westerhof, N. The relationship between the right ventricle and its load in pulmonary hypertension. J. Am. Coll. Cardiol. 2017, 69, 236–243. [Google Scholar] [CrossRef]
- Tello, K.; Dalmer, A.; Axmann, J.; Vanderpool, R.; Ghofrani, A.; Naeije, R.; Roller, F.; Seeger, W.; Sommer, N.; Wilhelm, J.; et al. Reserve of right ventricular-arterial coupling in the setting of chronic overload. Circ. Heart Fail. 2019, 12, e005512. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Bandera, F.; Pelissero, G.; Castelvecchio, S.; Menicanti, L.; Ghio, S.; Temporelli, P.L.; Arena, R. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: An index of right ventricular contractile function and prognosis. Am. J. Physiol. Heart Circ. Physiol. 2013, 305, H1373–H1381. [Google Scholar] [CrossRef]
- Guazzi, M.; Naeije, R.; Arena, R.; Corrà, U.; Ghio, S.; Forfia, P.; Rossi, A.; Cahalin, L.P.; Bandera, F.; Temporelli, P. Echocardiography of right ventriculoarterial coupling combined with cardiopulmonary exercise testing to predict outcome in heart failure. Chest 2015, 148, 226–234. [Google Scholar] [CrossRef]
- Kazimierczyk, R.; Szumowski, P.; Nekolla, S.G.; Blaszczak, P.; Malek, L.A.; Milosz-Wieczorek, B.; Misko, J.; Jurgilewicz, D.; Hladunski, M.; Knapp, M.; et al. Prognostic role of PET/MRI hybrid imaging in patients with pulmonary arterial hypertension. Heart 2021, 107, 54–60. [Google Scholar] [CrossRef]
- Guazzi, M. Use of TAPSE/PASP ratio in pulmonary arterial hypertension: An easy shortcut in a congested road. Int. J. Cardiol. 2018, 266, 242–244. [Google Scholar] [CrossRef]
- Tello, K.; Axmann, J.; Ghofrani, A.; Naeije, R.; Narcin, N.; Rieth, A.; Seeger, W.; Gall, H.; Richter, M.J. Relevance of the TAPSE/PASP ratio in pulmonary arterial hypertension. Int. J. Cardiol. 2018, 266, 229–235. [Google Scholar] [CrossRef]
- Kazimierczyk, R.; Małek, Ł.A.; Szumowski, P.; Błaszczak, P.; Jurgilewicz, D.; Hładuński, M.; Sobkowicz, B.; Myśliwiec, J.; Grzywna, R.; Musiał, W.J.; et al. Prognostic value of late gadolinium enhancement mass index in patients with pulmonary arterial hypertension. Adv. Med. Sci. 2021, 66, 28–34. [Google Scholar] [CrossRef]
- Kazimierczyk, R.; Malek, L.A.; Szumowski, P.; Nekolla, S.G.; Blaszczak, P.; Jurgilewicz, D.; Hladunski, M.; Sobkowicz, B.; Mysliwiec, J.; Grzywna, R.; et al. Multimodal assessment of right ventricle overload-metabolic and clinical consequences in pulmonary arterial hypertension. J. Cardiovasc. Magn. Reson. 2021, 23, 49. [Google Scholar] [CrossRef]
- Simsek, E.; Nalbantgil, S.; Ceylan, N.; Zoghi, M.; Kemal, H.S.; Engin, C.; Yagdi, T.; Ozbaran, M. Assessment of right ventricular systolic function in heart transplant patients: Correlation between echocardiography and cardiac magnetic resonance imaging. Investigation of the accuracy and reliability of echocardiography. Echocardiography 2017, 10, 1432–1438. [Google Scholar] [CrossRef] [PubMed]
- Ptaszyńska-Kopczyńska, K.; Krentowska, A.; Sawicka, E.; Skoneczny, A.; Jasiewicz, M.; Knapp, M.; Musiał, W.J.; Sobkowicz, B.; Kamiński, K.A. The strengths and weaknesses of non-invasive parameters obtained by echocardiography and cardiopulmonary exercise testing in comparison with the hemodynamic assessment by the right heart catheterization in patients with pulmonary hypertension. Adv. Med. Sci. 2017, 1, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Aubert, R.; Venner, C.; Huttin, O.; Haine, D.; Filippetti, L.; Guillaumot, A.; Mandry, D.; Marie, P.-Y.; Juillière, Y.; Chabot, F.; et al. Three-Dimensional Echocardiography for the Assessment of Right Ventriculo-Arterial Coupling. J. Am. Soc. Echocardiogr. 2018, 8, 905–915. [Google Scholar] [CrossRef]
- Hsiao, S.H.; Lin, S.K.; Wang, W.C.; Yang, S.H.; Gin, P.L.; Liu, C.P. Severe tricuspid regurgitation shows significant impact in the relationship among peak systolic tricuspid annular velocity, tricuspid annular plane systolic excursion, and right ventricular ejection fraction. J. Am. Soc. Echocardiogr. 2006, 7, 902–910. [Google Scholar] [CrossRef]
- Vonk-Noordegraaf, A.; Westerhof, N. Describing right ventricular function. Eur. Respir. J. 2013, 41, 1419–1423. [Google Scholar] [CrossRef] [Green Version]
- Vanderpool, R.R.; Pinsky, M.R.; Naeije, R.; Deible, C.; Kosaraju, V.; Bunner, C.; Mathier, M.A.; Lacomis, J.; Champion, H.C.; Simon, M.A. RV-pulmonary arterial coupling predicts outcome in patients referred for pulmonary hypertension. Heart 2015, 101, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Tello, K.; Wan, J.; Dalmer, A.; Vanderpool, R.; Ghofrani, A.; Naeije, R.; Roller, F.; Mohajerani, E.; Seeger, W.; Herberg, U.; et al. Validation of the Tricuspid Annular Plane Systolic Excursion/Systolic Pulmonary Artery Pressure Ratio for the Assessment of Right Ventricular-Arterial Coupling in Severe Pulmonary Hypertension. Circ. Cardiovasc. Imaging 2019, 9, e009047. [Google Scholar] [CrossRef]
- Benza, R.L.; Miller, D.P.; Gomberg-Maitland, M.; Frantz, R.P.; Foreman, A.J.; Coffey, C.S.; Frost, A.; Barst, R.J.; Badesch, D.B.; Elliott, C.G.; et al. Predicting survival in pulmonary arterial hypertension: Insights from the Registry to Evaluate Early and Long-Term Pulmonary Arterial Hypertension Disease Management (REVEAL). Circulation 2010, 2, 164–172. [Google Scholar] [CrossRef] [Green Version]
- Amsallem, M.; Sternbach, J.M.; Adigopula, S.; Kobayashi, Y.; Vu, T.A.; Zamanian, R.; Liang, D.; Dhillon, G.; Schnittger, I.; McConnell, M.V.; et al. Addressing the controversy of estimating pulmonary arterial pressure by echocardiography. J. Am. Soc. Echocardiogr. 2016, 29, 93–102. [Google Scholar] [CrossRef]
- Kjaergaard, J.; Akkan, D.; Iversen, K.K.; Køber, L.; Torp-Pedersen, C.; Hassager, C. Right ventricular dysfunction as an independent predictor of short- and long-term mortality in patients with heart failure. Eur. J. Heart Fail. 2007, 9, 610–616. [Google Scholar] [CrossRef] [PubMed]
- Damy, T.; Kallvikbacka-Bennett, A.; Goode, K.; Khaleva, O.; Lewinter, C.; Hobkirk, J.; Nikitin, N.P.; Dubois-Randé, J.-L.; Hittinger, L.; Clark, A.L.; et al. Prevalence of, associations with, and prognostic value of tricuspid annular plane systolic excursion (TAPSE) among out-patients referred for the evaluation of heart failure. J. Card. Fail. 2012, 18, 216–225. [Google Scholar] [CrossRef] [PubMed]

| PAH Group | Control Group | |
|---|---|---|
| Patients, n | 28 | 12 |
| Age (years) | 49.5 ± 15.5 | 44.75 ± 13.51 |
| Female sex, % (n) | 60 (17) | 67 (8) |
| BMI (kg/m2) | 24.5 ± 3.7 | 25.2 ± 3.6 |
| 6MWD (m) | 392 (322–453) * | 525 (497–550) |
| BNP (pg/mL) | 310.8 (54–3654) * | 27.2 (13–42) |
| Aetiology | ||
| IPAH/HPAH, % (n) | 67 (19) | |
| CTDPH, % (n) | 14 (4) | |
| CHDPH, % (n) | 19 (5) | |
| Therapy | ||
| PDE5 inhibitors, % (n) | 38 (10) | |
| Prostacyclins, % (n) | 20 (5) | |
| ERA, % (n) | 11 (3) | |
| Dual PDE5 inhibitor + ERA, % (n) | 31 (8) | |
| Echo parameters | ||
| RV basal diameter (cm) | 6.6 * | 3.6 ± 0.6 |
| RAA (cm2) | 25 (19–32) * | 10 (9–12) |
| TAPSE (mm) | 19.84 ± 4.28 * | 26 ± 3.4 |
| emPAP (mmHg) | 47.29 ± 15.3 * | 12.2 ± 3.8 |
| AcT (ms) | 82 ± 22 * | 130 ± 28 |
| TAPSE/sPAP (echo) | 0.34 ± 0.19 * | 1.51 ± 0.22 |
| RHC parameters | ||
| sPAP, mmHg | 79.6 ± 30.72 | |
| dPAP, mmHg | 31.9 ± 13.54 | |
| mPAP, mmHg | 48.95 ± 18.77 | |
| PAWP, mmHg | 10.5 ± 2.03 | |
| DPG, mmHg | 21.85 ± 13.08 | |
| CI, L/min/m2 | 2.65 ± 0.60 | |
| RAP, mmHg | 8.2 ± 2.92 | |
| PVR, Wood Units | 9.17 ± 5.69 | |
| MRI parameters | ||
| RVEF, % | 44.91 ± 7.9 * | 63.8 ± 5.8 |
| RV EDV/BSA, mL/m2 | 118.2 ± 21.7 * | 73.6 ± 12.2 |
| RV ESV/BSA, mL/m2 | 65.9 ± 20.3 * | 28.2 ± 9.6 |
| RV mass/BSA, g/m2 | 38.8 ± 13.9 * | 23.8 ± 4.9 |
| LVEF, % | 60.3 ± 9.9 | 67.1 ± 4.4 |
| LV mass/BSA, g/m2 | 58.3 ± 14.4 | 59.7 ± 18.3 |
| RV thickness, mm | 5.8 ± 1.5 * | 2.58 ± 0.4 |
| IVS, mm | 8.3 ± 1.5 | 7.7 ± 1.2 |
| TAPSE, mm | 18.9 ± 4.4 * | 24.9 ± 2.9 |
| CEP (+) Patients | CEP (−) Patients | p-Value | |
|---|---|---|---|
| Patients, n | 21 | 7 | |
| BNP, pg/mL | 269 (73–410) | 62 (46–258) | 0.60 |
| 6MWT distance, m | 394.9 ± 92.5 | 413.6 ± 71.4 | 0.04 |
| Echo parameters | |||
| LVIDd, cm | 4.38 ± 0.39 | 4.57 ± 0.55 | 0.50 |
| IVSd, cm | 0.93 ± 0.08 | 1.24 ± 0.82 | 0.76 |
| PWd, cm | 0.91 ± 0.13 | 0.90 ± 0.17 | 0.79 |
| RVIDd, cm | 3.44 ± 0.59 | 3.41 ± 0.51 | 0.81 |
| RAA, cm2 | 24.72 ± 8.63 | 20.42 ± 6.8 | 0.27 |
| sPAP, mmHg | 72.86 ± 32.74 | 58.50 ± 21.78 | 0.12 |
| mPAP, mmHg | 53.11 ± 17.11 | 34.86 ± 8.49 | 0.03 |
| TAPSE, mm | 19.23 ± 4.58 | 21.17 ± 3.87 | 0.06 |
| AcT, ms | 98.81 ± 32.2 | 100.71 ± 26.49 | 0.72 |
| TAPSE/sPAP | 0.30 ± 0.17 | 0.43 ± 0.21 | 0.04 |
| RHC parameters | |||
| sPAP, mmHg | 85.44 ± 28.11 | 62.61 ± 18.63 | 0.04 |
| mPAP, mmHg | 54.94 ± 16.95 | 37.21 ± 10.84 | 0.006 |
| PVR, Wood Units | 10.39 ± 5.59 | 5.74 ± 3.3 | 0.01 |
| CI, L/min/m2 | 2.49 ± 0.66 | 2.92 ± 0.84 | 0.01 |
| MRI parameters | |||
| RVEF, % | 42.05 ± 9.53 | 50.32 ± 9.11 | 0.01 |
| RV mass/BSA, g/m2 | 46.27 ± 17.41 | 36.71 ± 14.25 | 0.04 |
| RV thickness, mm | 6.22 ± 1.35 | 4.8 ± 1.2 | 0.04 |
| IVS, mm | 8.55 ± 1.54 | 8.77 ± 2.43 | 0.71 |
| TAPSE, mm | 17.72 ± 4.14 | 21.75 ± 3.73 | 0.04 |
| Parameter | AUC (95% Confidence Interval) | p-Value |
|---|---|---|
| sPAP (echo) | 0.71 (0.48–0.94) | p = 0.06 |
| sPAP (RHC) | 0.70 (0.55–0.92) | p = 0.01 |
| TAPSE (echo) | 0.65 (0.39–0.92) | p = 0.21 |
| TAPSE (MRI) | 0.67 (0.38–0.95) | p = 0.23 |
| TAPSE/sPAP (echo) | 0.72 (0.61–0.92) | p = 0.02 |
| TAPSE/sPAP (MRI/RHC) | 0.76 (0.59–0.94) | p = 0.003 |
| PVR (RHC) | 0.71 (0.50–0.91) | p = 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kazimierczyk, R.; Kazimierczyk, E.; Knapp, M.; Sobkowicz, B.; Malek, L.A.; Blaszczak, P.; Ptaszynska-Kopczynska, K.; Grzywna, R.; Kaminski, K.A. Echocardiographic Assessment of Right Ventricular–Arterial Coupling in Predicting Prognosis of Pulmonary Arterial Hypertension Patients. J. Clin. Med. 2021, 10, 2995. https://doi.org/10.3390/jcm10132995
Kazimierczyk R, Kazimierczyk E, Knapp M, Sobkowicz B, Malek LA, Blaszczak P, Ptaszynska-Kopczynska K, Grzywna R, Kaminski KA. Echocardiographic Assessment of Right Ventricular–Arterial Coupling in Predicting Prognosis of Pulmonary Arterial Hypertension Patients. Journal of Clinical Medicine. 2021; 10(13):2995. https://doi.org/10.3390/jcm10132995
Chicago/Turabian StyleKazimierczyk, Remigiusz, Ewelina Kazimierczyk, Malgorzata Knapp, Bozena Sobkowicz, Lukasz A. Malek, Piotr Blaszczak, Katarzyna Ptaszynska-Kopczynska, Ryszard Grzywna, and Karol A. Kaminski. 2021. "Echocardiographic Assessment of Right Ventricular–Arterial Coupling in Predicting Prognosis of Pulmonary Arterial Hypertension Patients" Journal of Clinical Medicine 10, no. 13: 2995. https://doi.org/10.3390/jcm10132995
APA StyleKazimierczyk, R., Kazimierczyk, E., Knapp, M., Sobkowicz, B., Malek, L. A., Blaszczak, P., Ptaszynska-Kopczynska, K., Grzywna, R., & Kaminski, K. A. (2021). Echocardiographic Assessment of Right Ventricular–Arterial Coupling in Predicting Prognosis of Pulmonary Arterial Hypertension Patients. Journal of Clinical Medicine, 10(13), 2995. https://doi.org/10.3390/jcm10132995









