Clinical and Radiological Results of Hemiarthroplasty and Total Shoulder Arthroplasty for Primary Avascular Necrosis of the Humeral Head in Patients Less Than 60 Years Old
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Operative Technique
2.3. Hemiarthroplasty Group
2.4. Total Anatomic Arthroplasty
2.5. Statistical Analysis
3. Results
3.1. Postoperative Complications
3.2. Reoperations
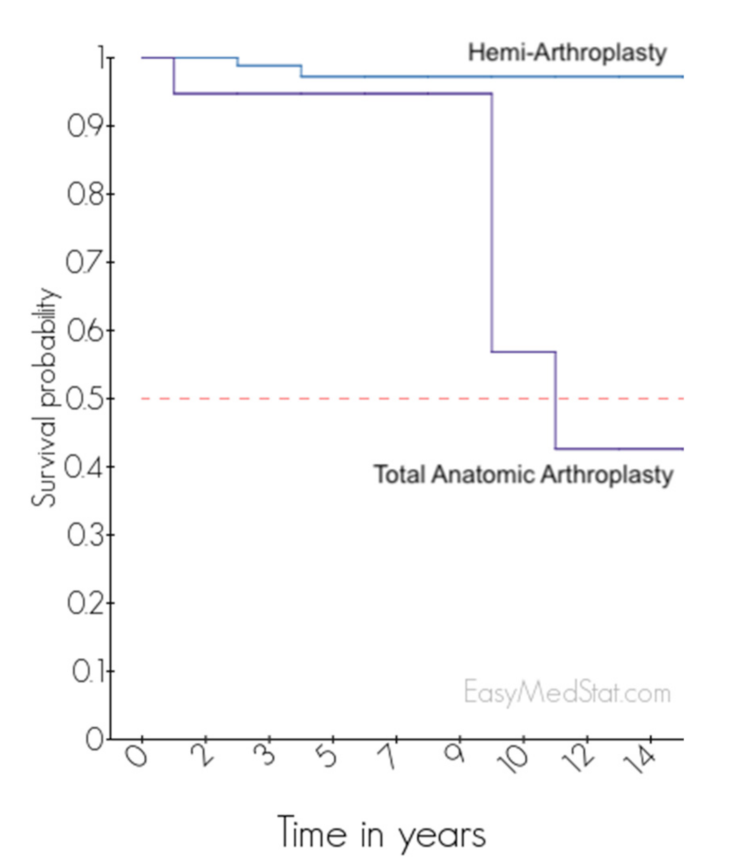
3.3. Revisions
3.4. Clinical Outcomes
3.5. Radiological Analysis
3.6. Comparison between Different Hemi-Arthroplasties
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Feeley, B.T.; Fealy, S.; Dines, D.M.; Warren, R.F.; Craig, E.V. Hemiarthroplasty and Total Shoulder Arthroplasty for Avascular Necrosis of the Humeral Head. J. Shoulder Elb. Surg. 2008, 17, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Mansat, P.; Huser, L.; Mansat, M.; Bellumore, Y.; Rongières, M.; Bonnevialle, P. Shoulder Arthroplasty for Atraumatic Avascular Necrosis of the Humeral Head: Nineteen Shoulders Followed up for a Mean of Seven Years. J. Shoulder Elb. Surg. 2005, 14, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Parsch, D.; Lehner, B.; Loew, M. Shoulder Arthroplasty in Nontraumatic Osteonecrosis of the Humeral Head. J. Shoulder Elb. Surg. 2003, 12, 226–230. [Google Scholar] [CrossRef]
- Schoch, B.S.; Barlow, J.D.; Schleck, C.; Cofield, R.H.; Sperling, J.W. Shoulder Arthroplasty for Atraumatic Osteonecrosis of the Humeral Head. J. Shoulder Elb. Surg. 2016, 25, 238–245. [Google Scholar] [CrossRef]
- Ristow, J.J.; Ellison, C.M.; Mickschl, D.J.; Berg, K.C.; Haidet, K.C.; Gray, J.R.; Grindel, S.I. Outcomes of Shoulder Replacement in Humeral Head Avascular Necrosis. J. Shoulder Elb. Surg. 2019, 28, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.G.; Sperling, J.W.; Cofield, R.H.; Hattrup, S.J.; Schleck, C.D. Shoulder Hemiarthroplasty for Steroid-Associated Osteonecrosis. J. Shoulder Elb. Surg. 2008, 17, 685–688. [Google Scholar] [CrossRef] [PubMed]
- Raiss, P.; Kasten, P.; Baumann, F.; Moser, M.; Rickert, M.; Loew, M. Treatment of Osteonecrosis of the Humeral Head with Cementless Surface Replacement Arthroplasty. J. Bone Jt. Surg. Am. 2009, 91, 340–349. [Google Scholar] [CrossRef]
- Ohl, X.; Nérot, C.; Saddiki, R.; Dehoux, E. Shoulder Hemi Arthroplasty Radiological and Clinical Outcomes at More than Two Years Follow-Up. Orthop. Traumatol. Surg. Res. 2010, 96, 208–215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Uribe, J.W.; Botto-van Bemden, A. Partial Humeral Head Resurfacing for Osteonecrosis. J. Shoulder Elb. Surg. 2009, 18, 711–716. [Google Scholar] [CrossRef] [PubMed]
- Sweet, S.J.; Takara, T.; Ho, L.; Tibone, J.E. Primary Partial Humeral Head Resurfacing: Outcomes with the HemiCAP Implant. Am. J. Sports Med. 2015, 43, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Soudy, K.; Szymanski, C.; Lalanne, C.; Bourgault, C.; Thiounn, A.; Cotten, A.; Maynou, C. Results and Limitations of Humeral Head Resurfacing: 105 Cases at a Mean Follow-up of 5 Years. Orthop. Traumatol. Surg. Res. 2017, 103, 415–420. [Google Scholar] [CrossRef] [PubMed]
- Sowa, B.; Thierjung, H.; Bülhoff, M.; Loew, M.; Zeifang, F.; Bruckner, T.; Raiss, P. Functional Results of Hemi- and Total Shoulder Arthroplasty According to Diagnosis and Patient Age at Surgery. Acta Orthop. 2017, 88, 310–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Orfaly, R.M.; Rockwood, C.A.; Esenyel, C.Z.; Wirth, M.A. Shoulder Arthroplasty in Cases with Avascular Necrosis of the Humeral Head. J. Shoulder Elb. Surg. 2007, 16, S27–S32. [Google Scholar] [CrossRef] [PubMed]
- Constant, C.R.; Murley, A.H. A Clinical Method of Functional Assessment of the Shoulder. Clin. Orthop. Relat. Res. 1994, 160–164. [Google Scholar] [CrossRef]
- Gerber, C.; Vinh, T.S.; Hertel, R.; Hess, C.W. Latissimus Dorsi Transfer for the Treatment of Massive Tears of the Rotator Cuff. A Preliminary Report. Clin. Orthop. Relat. Res. 1992, 232, 51–61. [Google Scholar] [CrossRef]
- Ficat, P.; Arlet, J. Pre-radiologic stage of femur head osteonecrosis: Diagnostic and therapeutic possibilities. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1973, 59 (Suppl. S1), 26–38. [Google Scholar]
- Cruess, R.L. Steroid-Induced Avascular Necrosis of the Head of the Humerus. Natural History and Management. J. Bone Jt. Surg. Br. 1976, 58, 313–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molé, D.; Roche, O.; Riand, N.; Lévigne, C.; Walch, G. Cemented Glenoid Component: Results in Osteoarthritis and Rheumatoid Arthritis. In Shoulder Arthroplasty; Springer: Berlin/Heidelberg, Germany, 1999; pp. 163–171. ISBN 978-3-642-63554-0. [Google Scholar]
- Collin, P.; Matsumura, N.; Lädermann, A.; Denard, P.J.; Walch, G. Relationship between Massive Chronic Rotator Cuff Tear Pattern and Loss of Active Shoulder Range of Motion. J. Shoulder Elb. Surg. 2014, 23, 1195–1202. [Google Scholar] [CrossRef] [PubMed]
- Herschel, R.; Wieser, K.; Morrey, M.E.; Ramos, C.H.; Gerber, C.; Meyer, D.C. Risk Factors for Glenoid Erosion in Patients with Shoulder Hemiarthroplasty: An Analysis of 118 Cases. J. Shoulder Elb. Surg. 2017, 26, 246–252. [Google Scholar] [CrossRef]
- Al-Hadithy, N.; Domos, P.; Sewell, M.D.; Naleem, A.; Papanna, M.C.; Pandit, R. Cementless Surface Replacement Arthroplasty of the Shoulder for Osteoarthritis: Results of Fifty Mark III Copeland Prosthesis from an Independent Center with Four-Year Mean Follow-Up. J. Shoulder Elb. Surg. 2012, 21, 1776–1781. [Google Scholar] [CrossRef] [PubMed]



 |  |  |  |  | |
| n = | 0 | 4 (3.3%) | 38 (31.4%) | 40 (33%) | 39 (3.3%) |
| Forward Elevation (°) | External Rotation (°) | Internal Rotation (/10) | CS (/100) | SSV (%) | |
|---|---|---|---|---|---|
| Hemi-arthroplasty (n = 83) | |||||
| Preoperative | 105 ± 37 (30–180) | 22 ± 18 (−10–70) | 4.7 ± 2.5 (0–10) | 37 ± 14 (10–71) | 39 ±17 (5–70) |
| Last FU | 154 ± 23 (90–180) | 39 ± 19 (−10–85) | 7.1 ± 1.9 (2–10) | 76 ± 11 (50–96) | 87 ± 13 (60–100) |
| p-Value a | <0.001 * | <0.001 * | <0.001 * | <0.001 * | <0.001 * |
| Total Anatomic Arthroplasty (n = 9) | |||||
| Preoperative | 112 ± 29 (80–160) | 14 ± 19 (−10–45) | 4.2 ± 2.9 (0–10) | 43 ± 11 (28–55) | 33 ± 14 (20–50) |
| Last FU | 142 ± 33 (90–170) | 39 ± 18 (10–60) | 6.2 ± 2.9 (2–10) | 71 ± 20 (43–94) | 73 ± 6 (70–80) |
| p-Value a | 0.055 | <0.01 * | 0.022 * | <0.01 * | <0.001 * |
| Metal-Head (n = 67) | Pyrocarbon (n = 6) | Resurfacing (n = 16) | Interposition Sphere (n = 19) | p-Value | |
|---|---|---|---|---|---|
| Postoperative Complication (%) | 6% | 0% | 6% | 5% | 1 |
| Revision surgery (%) | 1% | 0% | 6% | 0% | 0.40 |
| Metal-Head (n = 47) | Pyrocarbon (n = 5) | Resurfacing (n = 13) | Interposition Sphere (n = 18) | p-Value | |
| Forward Elevation (°) | 155 ± 22 (90–180) | 148 ± 27 (110–170) | 149 ± 27 (100–180) | 154 ± 23 (110–180) | 0.98 |
| External Rotation (°) | 35 ± 18 (−10–70) | 53 ± 15 (45–80) | 44 ± 16 (20–70) | 42 ± 21 (−10–85) | 0.09 |
| Internal Rotation (/10) | 6.6 ± 2.0 (2–10) | 8.4 ± 1.7 (6–10) | 6.8 ± 2.4 (4–10) | 7.7 ± 1.5 (4–10) | 0.14 |
| Constant Score (/100) | 73 ± 14 (30–91) | 75 ± 10 (61–89) | 75 ± 13 (54–96) | 78 ± 10 (61–95) | 0.79 |
| SSV (%) | 82 ± 21 (40–100) | 86 ± 9 (80–100) | 82 ± 11 (60–100) | 89 ± 12 (65–100) | 0.46 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hervé, A.; Chelli, M.; Boileau, P.; Walch, G.; Favard, L.; Levigne, C.; Sirveaux, F.; Clavert, P.; Bonnevialle, N.; Collin, P. Clinical and Radiological Results of Hemiarthroplasty and Total Shoulder Arthroplasty for Primary Avascular Necrosis of the Humeral Head in Patients Less Than 60 Years Old. J. Clin. Med. 2021, 10, 3081. https://doi.org/10.3390/jcm10143081
Hervé A, Chelli M, Boileau P, Walch G, Favard L, Levigne C, Sirveaux F, Clavert P, Bonnevialle N, Collin P. Clinical and Radiological Results of Hemiarthroplasty and Total Shoulder Arthroplasty for Primary Avascular Necrosis of the Humeral Head in Patients Less Than 60 Years Old. Journal of Clinical Medicine. 2021; 10(14):3081. https://doi.org/10.3390/jcm10143081
Chicago/Turabian StyleHervé, Anthony, Mickael Chelli, Pascal Boileau, Gilles Walch, Luc Favard, Christophe Levigne, François Sirveaux, Philippe Clavert, Nicolas Bonnevialle, and Philippe Collin. 2021. "Clinical and Radiological Results of Hemiarthroplasty and Total Shoulder Arthroplasty for Primary Avascular Necrosis of the Humeral Head in Patients Less Than 60 Years Old" Journal of Clinical Medicine 10, no. 14: 3081. https://doi.org/10.3390/jcm10143081






