1. Introduction
Implant-supported fixed dental prostheses function similar to natural teeth, but unlike natural teeth they consist of a fixture, abutment, and upper prosthesis [
1,
2,
3]. Implant-supported fixed dental prostheses are classified as screw-retained or cement-retained according to the methods used to retain the upper prosthesis. Screw-retained prostheses achieve stability and retention due to the clamping force exerted by screw tightening, whereas cement-retained prostheses achieve stability due to adhesive effects [
2,
3]. Both implant-supported fixed prosthesis types have high success rates. However, they have relative advantages and disadvantages, which can affect the incidences of biomechanical complications [
2,
3,
4,
5].
Screw-retained prostheses are easily removed and repair and hygiene management are straightforward and free of complications such as peri-implantitis, swelling, and ulcers caused by residual cement surrounding the implant prostheses and abutments [
6,
7,
8]. However, screw-retained prostheses require a high degree of precision to ensure a passive fit [
9,
10] and possess mechanical complications such as screw loosening and fractures [
3,
11]. In addition, screw-retained prostheses have a hole for screw access [
7,
12,
13] and this interferes with natural occlusion and the continuity of porcelain veneer on occlusal surfaces [
7,
14,
15,
16].
On the other hand, a passive fit can be easily achieved by using cement-retained prostheses because the cement layer compensates for errors in the manufacturing process and transmits stress uniformly to prostheses, implants, and the alveolar bone [
6,
15,
17,
18]. In addition, since cement-retained prostheses do not possess a screw access hole, aesthetics and proper occlusion are easily achieved [
14,
17,
19]. Furthermore, the laboratory processing of cement-retained prostheses is similar to that which is required for tooth-retained prostheses [
19]. However, retention control is an issue for cement-retained prostheses and difficulties may be experienced in achieving appropriate retention when the intermaxillary space is insufficient or in retrieving the prostheses for repair and maintenance [
5,
6,
19,
20]. In addition, subgingival cement removal may damage the abutment and residual cement may cause biological complications such as peri-implantitis [
6,
19,
20,
21].
In order to address the problems associated with screw and cement-retained prostheses, a screw and cement-retained prosthesis (SCRP) was developed that combines the advantages of these prostheses types [
9,
22,
23]. SCRPs are cement-retained prostheses with a screw hole on the occlusal surface and a specially designed abutment [
9]; these can achieve passive fit and reduce prosthesis detachment associated with the use of permanent cement [
10,
24]. The abutment and prosthesis are permanently cemented and can be removed from the fixture. Moreover, the residual cement can be completely removed from outside the oral cavity [
24]. Therefore, it is possible to reduce abutment scratches that may occur when cement is removed after prosthesis cementation and to minimize the risk of peri-implantitis due to residual cement [
8,
21]. However, this method also requires a screw hole in the occlusal surface [
9,
24].
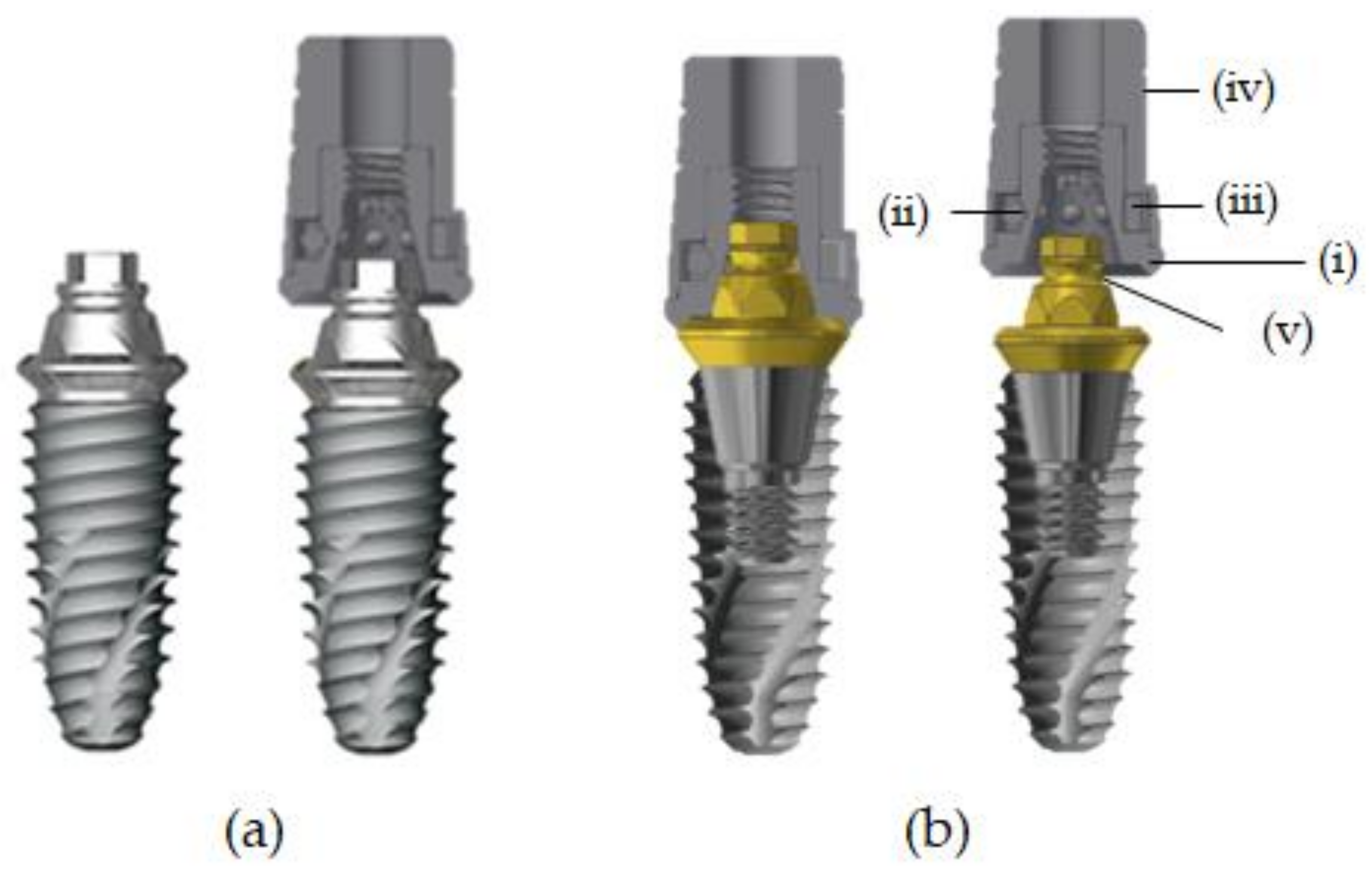
Recently, a new type of implant prosthesis retention system was introduced by Samwon DMP (Yangsan, Korea) in order to overcome the shortcomings of existing implant prostheses and allow operators to easily attach and detach prostheses when desired [
25]. The screw-integrated abutment is tightened to the installed fixture and then a ready-made cylinder is mounted above on the abutment and an upper prosthesis is attached to this cylinder by resin cementation. A spring made of nickel-titanium shaped memory alloy applies a continuous and constant force on the zirconia ball inside the cylinder placed in the retention groove of an abutment. The micro-locking abutment (the MLA system, Samwon DMP, Yangsan, Korea) is described as a freely removable system because it can achieve retention without a screw or cement between the final prosthesis and implant abutment [
26]. Furthermore, this system is aesthetic and advantageous for forming occlusal points because no screw access hole is required. When it is difficult to remove an MLA prosthesis due to strong retention, it can be easily removed by using a dedicated driver by forming a hole, which can be smaller than the existing screw access hole. Since this implant fixture is freely removable, it is possible to remove excess cement from outside the mouth, which can prevent biological complications such as peri-implantitis and has considerable maintenance advantages [
18,
27,
28].
An in vitro pilot study on the retention of the MLA system showed it has a low retention loss rate at 12 months and provides stable retention thereafter [
25]. In addition, several case reports and retrospective clinical studies have reported successful clinical applications of the system. Previous case reports and clinical studies used a two-piece ML system incorporated into the abutment. The MLA system is connected to fixtures by using an abutment screw, such as the conventional screw-retained implant prostheses, and this connection method is easily applied to existing implant systems. However, complications such as the screw loosening or screw fractures are possible [
25,
26,
27,
28,
29].
The one-piece micro-locking implant system (the MLF system), which was designed to prevent mechanical complications, combines fixture and abutment and, thus, screw-related mechanical complications are circumvented by the lack of a screw component [
30]. In order to exclude screw-related mechanical complications, an implant fixture including an ML system that is similar to a one-piece implant was developed. To date, few clinical studies have been conducted on implant fixtures such as the MLA or MLF systems [
25,
26,
27,
28,
29] and, in order to establish a scientific basis, long-term clinical trials are required for the one-piece ML system. In the present study, marginal bone loss and complications were evaluated by prospective clinical examination and radiological analysis in patients fitted with a screw-free one-piece MLF or a two-piece MLA system. The purpose of this study was to evaluate and compare the clinical usefulness and complications associated with the newly developed one-piece MLF and a two-piece MLA.
4. Discussion
Screw-retained prostheses are widely used in clinical practice but can cause complications such as screw loosening, screw fracture, and abutment fracture [
38]. Cement-retained prostheses also have some limitations, such as infection and marginal bone resorption by residual cement. In addition, the prosthetic margin may be positioned below soft tissue due to aesthetic requirements and the removal of residual cement in such cases may damage the soft tissue around implants [
39].
Various methods have been devised to overcome these shortcomings. A prosthesis retaining system using shape memory alloy was introduced and has been reported to be clinically successful. The Smileloc
® system (Rodo Medical, San Jose, CA, USA) is a typical example of this type of system and provides retrievability by using a shape memory nickel-titanium sleeve. Thus, cement-related peri-implant complications can be reduced and the structural integrity of the prosthesis can be improved by eliminating the occlusal screw access hole [
18,
40]. Another method to retain the prosthesis without cement uses a tight fit between a customized abutment and zirconia with a resin-coated inner surface. However, there is always a possibility of screw-related mechanical complications because these newly developed methods also rely on a screw to connect the implant fixture and abutment [
41].
The ML system was developed to address these shortcomings. Initially, an abutment including an ML system was commercialized to facilitate application in existing implant systems. Several laboratory studies, case reports, and clinical studies have suggested the possible successful clinical application of the ML system [
26,
27,
28]. However, in a 1 year prospective clinical study, the cumulative survival rate of implants in MLF was reported to be 100%, which indicates that changing the implant prosthesis connection method would not significantly affect implant survival [
29].
A systematic review of clinical comparison of one piece versus two piece implants reported marginal bone resorption rates of 0.39 to 1.8 mm and 0.56 to 1.6 mm, respectively [
42]. In the present study, the mean marginal bone resorptions at 6 months and 12 months after prosthesis placement in the MLF group were 0.43 ± 0.24 mm and 0.44 ± 0.25 mm, respectively, and the corresponding values in the MLA group were 0.31 ± 0.24 and 0.33 ± 0.34 mm, which concurs with the results of a systematic review of clinical comparisons of one piece versus two piece implants [
42]. In the present study, no significant intergroup differences or changes were observed at 6 or 12 months after prosthesis placement.
An up to 6 month pilot clinical study of the Smileloc
® system found that the probing depth was less than 3 mm at all sites for all participants throughout the observation period [
40]. In the present study, the mean probe depths at 6 and 12 months in the MLF group were 2.12 ± 0.66 and 2.22 ± 0.56 mm, respectively, and the corresponding values in the MLA group were 2.37 ± 0.53 and 2.49 ± 0.45. These results are similar to those obtained in the clinical study of the Smileloc
® system. In the present study, no significant intergroup difference or intragroup change was observed at 6 months or 12 months after prosthesis placement.
In a study that compared cement-retained and screw-retained prostheses, cement-retained prostheses generally showed more plaque deposits and bleeding [
43]. Periodontal indices of cement-retained prostheses remained high during a three-year observation period, while the screw-retained prostheses showed a stable plaque deposit rate and bleeding level after 6 months. In the present study, a comparison of soft tissue statuses in the two groups using mPI and mBI measurements showed that the MLF group had the better periodontal condition at 12 months, but no significant differences were observed between the two groups at 6 months. This result indicates that implants in the MLF group were more compatible with soft tissue around implants. One piece implants have the advantage of fewer biological complications because no micro gap exists and no micromotion occurs at the connection between the abutment and fixture [
30]. One piece implants in the MLF group were structurally simpler than the two piece implants in the MLA group and the MLF implants had no micro-gap; thus, it seems that this design has a beneficial effect on soft tissue.
Screw loosening, porcelain fracture, resin dropout from an access hole, and abutment fracture have been reported to be major complications of screw-retained prostheses and screw loosening, porcelain fracture, abutment fracture, and decementation of prostheses have been reported as complications of cement-retained prosthesis [
38,
44,
45,
46,
47,
48]. We also observed screw loosening, gingival swelling, prosthesis detachment, and food impaction. In the MLF group, food impaction was the main complication and, in the MLA group, the complications (in decreasing order) were screw loosening, prosthesis detachment, and food impaction at 6 months. Since the prostheses used in the MLF group had a screw-free design, screw loosening was not an issue, which is an advantage shared with one piece implants without a screw component [
30].
The main complication in the MLF group was food impaction, which is affected by occlusal relationships, implant location in the arch, marginal ridge height difference versus proximal teeth, tightness of fit with proximal teeth, and the mobility of proximal teeth rather than the method used to connect the fixture and prosthesis [
49]. It could be reasonably considered that food impaction as a complication can appear regardless of the prosthetic connection method used for most common implant prostheses. In order to reduce food impaction, a healthy proximal tooth without mobility or caries and a prosthesis with an appropriate contact point and tightness is required [
50]. In this study, prosthesis detachment was observed in all groups. We suggest that additional studies with more samples be undertaken and that retention control should be considered.
Screw loosening in the MLA group occurred in 5.3% of patients 12 months after prosthetic cementation. The micro-locking abutment is manufactured to be compatible with the morse taper fixtures of various companies, but slight displacements may occur at the implant–abutment connection [
29]. Therefore, the use of a micro-locking one-piece fixture is considered an attractive alternative.
In this prospective clinical study, MLF and MLA groups were compared over one year and the study failed to reveal significant differences between the clinical indices of the micro-locking one-piece fixtures and micro locking abutments. Therefore, we suggest that long-term clinical studies be conducted to identify complications not found in this study and to establish the clinical efficacy of the micro-locking one-piece fixture.