Improvement of Working Memory and Processing Speed in Patients over 70 with Bilateral Hearing Impairment Following Unilateral Cochlear Implantation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Inclusion Criteria
- Diagnosis of post-lingual, bilateral, and severe hearing loss with speech perception ≤ 60% in the Freiburg Monosyllabic Test (speech perception in quiet) and with best-fitted hearing aids with sound pressure level (SPL) 65 dB, as previously described [55]
- German mother tongue
- Age 70 and above
- Unilateral cochlear implant
- Meeting of the clinical criteria for cochlear implantation:
- ○
- Possibility of using general anesthesia
- ○
- Exclusion of retrocochlear disorder (e.g., vestibular schwannoma)
- ○
- Unremarkable cochlear anatomy
- ○
- Motivation for postoperative audiological rehabilitation
2.2. Exclusion Criteria
- Diagnosed dementia syndrome or mild cognitive impairment in the medical history
- Severe visual impairment in the medical history
- Lost to follow-up (e.g., severe general illness)
2.3. Explanation of the Number of Patients Included in the Study
2.4. Description of Study
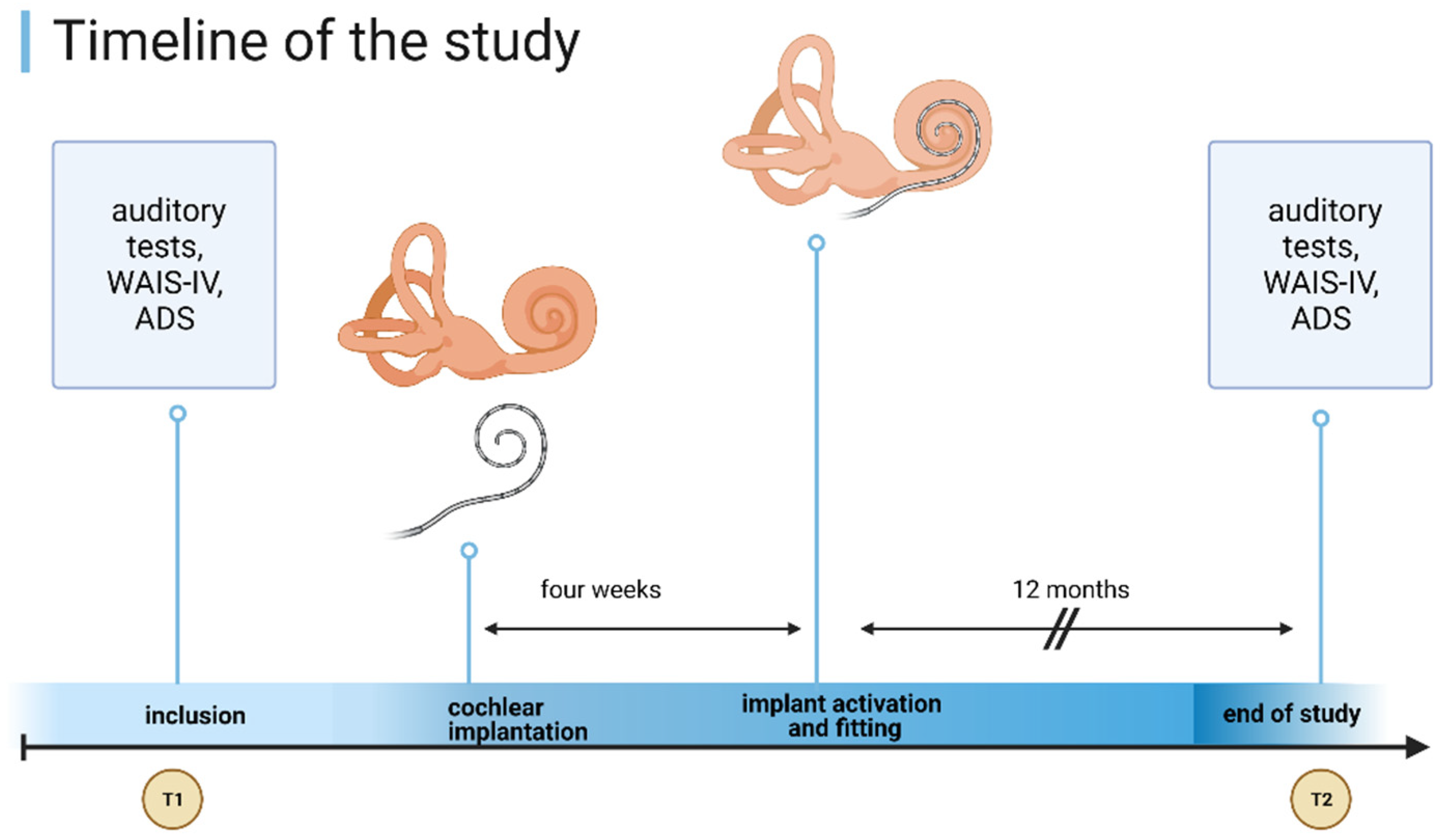
2.5. Audiological Assessment: Speech Perception (SP) in Silence and in Noise
2.6. Audiological Rehabilitation
2.7. Audiological Assessment: Oldenburg Self-Assessment Inventory (OI)
2.8. Screening for Depressiveness: General Depression Scale–Long (ADS-L)
2.9. Cognitive Performance Test (Wechsler Adult Intelligence Scale 4th Edition: WAIS-IV)
2.10. Statistical Evaluation
3. Results
3.1. Patient Data and Age Distribution
3.2. Audiological Assessment
3.2.1. Speech Perception (SP) in Silence (FMT)
3.2.2. Speech Perception (SP) in Noise (OLSA)
3.2.3. Audiological Self-Assessment: Oldenburg Inventory (OI)
3.3. Screening for Depressiveness: General Depression Scale–Long (ADS-L)
3.4. Cognitive Performance Test: Wechsler Adult Intelligence Scale 4th Edition (WAIS-IV)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. Deafness and Hearing Loss. Available online: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss (accessed on 26 November 2020).
- Lin, F.R.; Metter, E.J.; O’Brien, R.J.; Resnick, S.M.; Zonderman, A.B.; Ferrucci, L. Hearing loss and incident dementia. Arch. Neurol. 2011, 68, 214–220. [Google Scholar] [CrossRef] [Green Version]
- Lin, F.R.; Niparko, J.K.; Ferrucci, L. Hearing loss prevalence in the United States. Arch. Intern. Med. 2011, 171, 1851–1852. [Google Scholar] [CrossRef]
- Chien, W.; Lin, F.R. Prevalence of hearing aid use among older adults in the United States. Arch. Intern. Med. 2012, 172, 292–293. [Google Scholar] [CrossRef] [Green Version]
- Foley, D.M.; Frick, K.D.; Lin, F.R. Association between hearing loss and healthcare expenditures in older adults. J. Am. Geriatr. Soc. 2014, 62, 1188–1189. [Google Scholar] [CrossRef] [Green Version]
- Mick, P.; Kawachi, I.; Lin, F.R. The association between hearing loss and social isolation in older adults. Otolaryngol. Head Neck Surg. 2014, 150, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Dawes, P.; Emsley, R.; Cruickshanks, K.J.; Moore, D.R.; Fortnum, H.; Edmondson-Jones, M.; McCormack, A.; Munro, K.J. Hearing loss and cognition: The role of hearing AIDS, social isolation and depression. PLoS ONE 2015, 10, e0119616. [Google Scholar] [CrossRef] [Green Version]
- Shukla, A.; Harper, M.; Pedersen, E.; Goman, A.; Suen, J.J.; Price, C.; Applebaum, J.; Hoyer, M.; Lin, F.R.; Reed, N.S. Hearing loss, loneliness, and social isolation: A systematic review. Otolaryngol. Head Neck Surg. 2020, 162, 622–633. [Google Scholar] [CrossRef]
- Maharani, A.; Pendleton, N.; Leroi, I. Hearing impairment, loneliness, social isolation, and cognitive function: Longitudinal analysis using English longitudinal study on ageing. Am. J. Geriatr. Psychiatry 2019, 27, 1348–1356. [Google Scholar] [CrossRef]
- Wingfield, A. Evolution of models of working memory and cognitive resources. Ear. Hear. 2016, 37 (Suppl. S1), 35S–43S. [Google Scholar] [CrossRef]
- Wayne, R.V.; Johnsrude, I.S. A review of causal mechanisms underlying the link between age-related hearing loss and cognitive decline. Ageing Res. Rev. 2015, 23, 154–166. [Google Scholar] [CrossRef]
- Davies, H.R.; Cadar, D.; Herbert, A.; Orrell, M.; Steptoe, A. Hearing impairment and incident dementia: Findings from the English Longitudinal Study of Ageing. J. Am. Geriatr. Soc. 2017, 65, 2074–2081. [Google Scholar] [CrossRef] [Green Version]
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet 2020, 396, 413–446. [Google Scholar] [CrossRef]
- Chern, A.; Golub, J.S. Age-related hearing loss and dementia. Alzheimer Dis. Assoc. Disord. 2019, 33, 285–290. [Google Scholar] [CrossRef]
- Peelle, J.E.; Wingfield, A. The neural consequences of age-related hearing loss. Trends Neurosci. 2016, 39, 486–497. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wortmann, M. Dementia: A global health priority—highlights from an ADI and World Health Organization report. Alzheimers Res. Ther. 2012, 4, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whalley, L.J.; Deary, I.J.; Appleton, C.L.; Starr, J.M. Cognitive reserve and the neurobiology of cognitive aging. Ageing Res. Rev. 2004, 3, 369–382. [Google Scholar] [CrossRef]
- Ronnberg, J.; Lunner, T.; Zekveld, A.; Sorqvist, P.; Danielsson, H.; Lyxell, B.; Dahlstrom, O.; Signoret, C.; Stenfelt, S.; Pichora-Fuller, M.K.; et al. The Ease of Language Understanding (ELU) model: Theoretical, empirical, and clinical advances. Front. Syst. Neurosci. 2013, 7, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, F.R.; Albert, M. Hearing loss and dementia—Who is listening? Aging Ment. Health 2014, 18, 671–673. [Google Scholar] [CrossRef] [Green Version]
- Cattell, R.B. Theory of fluid and crystallized intelligence: A critical experiment. J. Educ. Psychol. 1963, 54, 1–22. [Google Scholar] [CrossRef]
- World Health Organization. Global Costs of Unaddressed Hearing Loss and Cost-Effectiveness of Interventions: A WHO Report, 2017; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Yumba, W.K. Cognitive processing speed, working memory, and the intelligibility of hearing aid-processed speech in persons with hearing impairment. Front. Psychol. 2017, 8, 1308. [Google Scholar] [CrossRef] [Green Version]
- Pickora-Fuller, M.K. Processing speed and timing in aging adults: Psychoacoustics, speech perception, and comprehension. Int. J. Audiol. 2003, 42 (Suppl. S1), S59–S67. [Google Scholar] [CrossRef]
- Wendt, D.; Kollmeier, B.; Brand, T. How hearing impairment affects sentence comprehension: Using eye fixations to investigate the duration of speech processing. Trends Hear. 2015, 19. [Google Scholar] [CrossRef] [Green Version]
- Lally, J.W.; Adams, J.K.; Wilkerson, B.J. The use of cochlear implantation in the elderly. Curr. Opin. Otolaryngol. Head Neck Surg. 2019, 27, 387–391. [Google Scholar] [CrossRef]
- Knopke, S.; Haussler, S.; Grabel, S.; Wetterauer, D.; Ketterer, M.; Fluger, A.; Szczepek, A.J.; Olze, H. Age-dependent psychological factors influencing the outcome of cochlear implantation in elderly patients. Otol. Neurotol. 2019, 40, e441–e453. [Google Scholar] [CrossRef] [PubMed]
- Knopke, S.; Olze, H. Hearing rehabilitation with cochlear implants and cognitive abilities. HNO 2018, 66, 364–368. [Google Scholar] [CrossRef]
- Bruggemann, P.; Szczepek, A.J.; Klee, K.; Grabel, S.; Mazurek, B.; Olze, H. In patients undergoing cochlear implantation, psychological burden affects tinnitus and the overall outcome of auditory rehabilitation. Front. Hum. Neurosci. 2017, 11, 226. [Google Scholar] [CrossRef] [PubMed]
- Knopke, S.; Szczepek, A.J.; Haussler, S.M.; Grabel, S.; Olze, H. Cochlear Implantation of bilaterally deafened patients with tinnitus induces sustained decrease of tinnitus-related distress. Front. Neurol. 2017, 8, 158. [Google Scholar] [CrossRef] [Green Version]
- Olze, H.; Knopke, S.; Grabel, S.; Szczepek, A.J. Rapid positive influence of cochlear implantation on the quality of life in adults 70 years and older. Audiol. Neurootol. 2016, 21 (Suppl. S1), 43–47. [Google Scholar] [CrossRef]
- Knopke, S.; Grabel, S.; Forster-Ruhrmann, U.; Mazurek, B.; Szczepek, A.J.; Olze, H. Impact of cochlear implantation on quality of life and mental comorbidity in patients aged 80 years. Laryngoscope 2016, 126, 2811–2816. [Google Scholar] [CrossRef]
- Olze, H.; Grabel, S.; Forster, U.; Zirke, N.; Huhnd, L.E.; Haupt, H.; Mazurek, B. Elderly patients benefit from cochlear implantation regarding auditory rehabilitation, quality of life, tinnitus, and stress. Laryngoscope 2012, 122, 196–203. [Google Scholar] [CrossRef]
- Volter, C.; Gotze, L.; Haubitz, I.; Muther, J.; Dazert, S.; Thomas, J.P. Impact of cochlear implantation on neurocognitive subdomains in adult cochlear implant recipients. Audiol. Neurootol. 2021, 1–10. [Google Scholar] [CrossRef]
- Volter, C.; Gotze, L.; Haubitz, I.; Dazert, S.; Thomas, J.P. Benefits of cochlear implantation in middle-aged and older adults. Clin. Interv. Aging 2020, 15, 1555–1568. [Google Scholar] [CrossRef]
- Amieva, H.; Ouvrard, C.; Giulioli, C.; Meillon, C.; Rullier, L.; Dartigues, J.F. Self-reported hearing loss, hearing aids, and cognitive decline in elderly adults: A 25-year study. J. Am. Geriatr. Soc. 2015, 63, 2099–2104. [Google Scholar] [CrossRef]
- Mosnier, I.; Bebear, J.P.; Marx, M.; Fraysse, B.; Truy, E.; Lina-Granade, G.; Mondain, M.; Sterkers-Artieres, F.; Bordure, P.; Robier, A.; et al. Improvement of cognitive function after cochlear implantation in elderly patients. JAMA Otolaryngol. Head Neck Surg. 2015, 141, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Zhan, K.Y.; Lewis, J.H.; Vasil, K.J.; Tamati, T.N.; Harris, M.S.; Pisoni, D.B.; Kronenberger, W.G.; Ray, C.; Moberly, A.C. Cognitive functions in adults receiving cochlear implants: Predictors of speech recognition and changes after implantation. Otol. Neurotol. 2020, 41, e322–e329. [Google Scholar] [CrossRef] [PubMed]
- Mertens, G.; Andries, E.; Claes, A.J.; Topsakal, V.; Van de Heyning, P.; Van Rompaey, V.; Calvino, M.; Sanchez Cuadrado, I.; Munoz, E.; Gavilan, J.; et al. Cognitive Improvement after cochlear implantation in older adults with severe or profound hearing impairment: A prospective, longitudinal, controlled, multicenter study. Ear Hear. 2020, 42, 606–614. [Google Scholar] [CrossRef]
- Humes, L.E. Associations between measures of auditory function and brief assessments of cognition. Am. J. Audiol. 2020, 29, 825–837. [Google Scholar] [CrossRef]
- Akeroyd, M.A. Are individual differences in speech reception related to individual differences in cognitive ability? A survey of twenty experimental studies with normal and hearing-impaired adults. Int. J. Audiol. 2008, 47 (Suppl. S2), S53–S71. [Google Scholar] [CrossRef]
- Meister, H.; Rahlmann, S.; Walger, M.; Margolf-Hackl, S.; Kiessling, J. Hearing aid fitting in older persons with hearing impairment: The influence of cognitive function, age, and hearing loss on hearing aid benefit. Clin. Interv. Aging 2015, 10, 435–443. [Google Scholar] [CrossRef] [Green Version]
- Martini, A.; Castiglione, A.; Bovo, R.; Vallesi, A.; Gabelli, C. Aging, cognitive load, dementia and hearing loss. Audiol. Neurootol. 2014, 19 (Suppl. S1), 2–5. [Google Scholar] [CrossRef]
- Lin, F.R. Hearing loss and cognition among older adults in the United States. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 1131–1136. [Google Scholar] [CrossRef] [Green Version]
- Park, S.Y.; Kim, M.J.; Sikandaner, H.; Kim, D.K.; Yeo, S.W.; Park, S.N. A causal relationship between hearing loss and cognitive impairment. Acta Otolaryngol. 2016, 136, 480–483. [Google Scholar] [CrossRef]
- Lin, F.R.; Yaffe, K.; Xia, J.; Xue, Q.L.; Harris, T.B.; Purchase-Helzner, E.; Satterfield, S.; Ayonayon, H.N.; Ferrucci, L.; Simonsick, E.M.; et al. Hearing loss and cognitive decline in older adults. JAMA Intern. Med. 2013, 173, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Maharani, A.; Dawes, P.; Nazroo, J.; Tampubolon, G.; Pendleton, N.; SENSE-Cog WP1 Group. Longitudinal relationship between hearing aid use and cognitive function in older Americans. J. Am. Geriatr. Soc. 2018, 66, 1130–1136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, C.F.B.; Rabelo, C.M.; Silagi, M.L.; Mansur, L.L.; Bamiou, D.E.; Schochat, E. Auditory processing performance of the middle-aged and elderly: Auditory or cognitive decline? J. Am. Acad. Audiol. 2018, 29, 5–14. [Google Scholar] [CrossRef]
- Armstrong, N.M.; An, Y.; Ferrucci, L.; Deal, J.A.; Lin, F.R.; Resnick, S.M. Temporal sequence of hearing impairment and cognition in the baltimore longitudinal study of aging. J. Gerontol. A Biol. Sci. Med. Sci. 2020, 75, 574–580. [Google Scholar] [CrossRef]
- Humes, L.E.; Busey, T.A.; Craig, J.; Kewley-Port, D. Are age-related changes in cognitive function driven by age-related changes in sensory processing? Atten. Percept. Psychophys. 2013, 75, 508–524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ronnberg, J.; Lunner, T.; Ng, E.H.; Lidestam, B.; Zekveld, A.A.; Sorqvist, P.; Lyxell, B.; Traff, U.; Yumba, W.; Classon, E.; et al. Hearing impairment, cognition and speech understanding: Exploratory factor analyses of a comprehensive test battery for a group of hearing aid users, the n200 study. Int. J. Audiol. 2016, 55, 623–642. [Google Scholar] [CrossRef]
- Uchida, Y.; Nishita, Y.; Tange, C.; Sugiura, S.; Otsuka, R.; Ueda, H.; Nakashima, T.; Ando, F.; Shimokata, H. The longitudinal impact of hearing impairment on cognition differs according to cognitive domain. Front. Aging Neurosci. 2016, 8, 201. [Google Scholar] [CrossRef] [Green Version]
- Ronnberg, J.; Holmer, E.; Rudner, M. Cognitive hearing science and ease of language understanding. Int. J. Audiol. 2019, 58, 247–261. [Google Scholar] [CrossRef]
- Uhlmann, R.F.; Larson, E.B.; Rees, T.S.; Koepsell, T.D.; Duckert, L.G. Relationship of hearing impairment to dementia and cognitive dysfunction in older adults. JAMA 1989, 261, 1916–1919. [Google Scholar] [CrossRef] [PubMed]
- Boake, C. From the Binet-Simon to the Wechsler-Bellevue: Tracing the history of intelligence testing. J. Clin. Exp. Neuropsychol. 2002, 24, 383–405. [Google Scholar] [CrossRef] [PubMed]
- Präsidium der DGHNO. Weißbuch: Cochlea-Implantat(CI)-Versorgung; Präsidium der DGHNO: Bonn, Germany, 2018. [Google Scholar]
- Bailer, M.; Hautzinger, M.; Hofmeister, D.; Keller, F. Allgemeine Depressionsskala (ADS); Hogrefe: Göttingen, Germany, 2012. [Google Scholar]
- Wagener, K.; Brand, T.; Kollmeier, B. Entwicklung und Evaluation eines Satztests für die deutsche Sprache III: Evaluation des Oldenburger Satztests. Z. Audiol. 1999, 38, 86–95. [Google Scholar]
- Holube, I.; Kollmeier, B. ModifIkation eines Fragebogens zur Erlassung des subjektiven Hörvermögens und dessen Beziehung zur Sprachverständlichkeit in Ruhe und unter Störgeräuschen. Audiol. Akust. 1994, 33, 22–35. [Google Scholar]
- Stemmler, M.; Petermann, F.; Daseking, M.; Siebert, J.; Schott, H.; Lehfeld, H.; Horn, R. The assessment and course of development of cognitive abilities in the elderly. Gesundheitswesen 2013, 75, 761–767. [Google Scholar] [CrossRef]
- Lepach, A.C.; Petermann, F. Gedächtnisdiagnostik mit der Wechsler Memory Scale–Fourth Edition. Z. Neuropsychol. 2012, 23, 123–132. [Google Scholar] [CrossRef]
- Daseking, M.; Petermann, F. Analyse von Querschnittsdaten zur Intelligenzentwicklung im Erwachsenenalter: Eine Studie zur deutschsprachigen Version der WAIS-IV. Z. Neuropsychol. 2013, 24, 149–160. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 2013. [Google Scholar]
- Gignac, G.E.; Szodorai, E.T. Effect size guidelines for individual differences researchers. Personal. Individ. Differ. 2016, 102, 74–78. [Google Scholar] [CrossRef]
- Olze, H.; Szczepek, A.J.; Haupt, H.; Forster, U.; Zirke, N.; Grabel, S.; Mazurek, B. Cochlear implantation has a positive influence on quality of life, tinnitus, and psychological comorbidity. Laryngoscope 2011, 121, 2220–2227. [Google Scholar] [CrossRef]
- Haussler, S.M.; Knopke, S.; Wiltner, P.; Ketterer, M.; Grabel, S.; Olze, H. Long-term benefit of unilateral cochlear implantation on quality of life and speech perception in bilaterally deafened patients. Otol. Neurotol. 2019, 40, e430–e440. [Google Scholar] [CrossRef]
- Heinrich, A.; Henshaw, H.; Ferguson, M.A. The relationship of speech intelligibility with hearing sensitivity, cognition, and perceived hearing difficulties varies for different speech perception tests. Front. Psychol. 2015, 6, 782. [Google Scholar] [CrossRef] [Green Version]
- Buchman, C.A.; Gifford, R.H.; Haynes, D.S.; Lenarz, T.; O’Donoghue, G.; Adunka, O.; Biever, A.; Briggs, R.J.; Carlson, M.L.; Dai, P.; et al. Unilateral Cochlear implants for severe, profound, or moderate sloping to profound bilateral sensorineural hearing loss: A systematic review and consensus statements. JAMA Otolaryngol. Head Neck Surg. 2020, 146, 942–953. [Google Scholar] [CrossRef]
- Hoppe, U.; Hast, A.; Hocke, T. Audiometry-based screening procedure for cochlear implant candidacy. Otol. Neurotol. 2015, 36, 1001–1005. [Google Scholar] [CrossRef] [PubMed]
- Holmes, E.; Griffiths, T.D. ‘Normal’ hearing thresholds and fundamental auditory grouping processes predict difficulties with speech-in-noise perception. Sci. Rep. 2019, 9, 16771. [Google Scholar] [CrossRef] [Green Version]
- Hopkins, K.; Moore, B.C. The effects of age and cochlear hearing loss on temporal fine structure sensitivity, frequency selectivity, and speech reception in noise. J. Acoust. Soc. Am. 2011, 130, 334–349. [Google Scholar] [CrossRef] [PubMed]
- Moberly, A.C.; Lowenstein, J.H.; Nittrouer, S. Word recognition variability with cochlear implants: “Perceptual attention” versus “auditory sensitivity”. Ear Hear. 2016, 37, 14–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schneider, W.J.; McGrew, K.S. The Cattell-Horn-Carroll model of intelligence. In Contemporary Intellectual Assessment: Theories, Tests, and Issues, 3rd ed.; The Guilford Press: New York, NY, USA, 2012; pp. 99–144. [Google Scholar]
- Vega, A. Present neuropsychological status of subjects implanted with auditory prostheses. Ann. Otol. Rhinol. Laryngol. 1977, 86, 57–60. [Google Scholar] [CrossRef]
- Crary, W.G.; Wexler, M.; Berliner, K.I.; Miller, L.W. Psychometric studies and clinical interviews with cochlear implant patients. Ann. Otol. Rhinol. Laryngol. 1982, 91, 55–58. [Google Scholar]
- Miller, G.; Miller, C.; Marrone, N.; Howe, C.; Fain, M.; Jacob, A. The impact of cochlear implantation on cognition in older adults: A systematic review of clinical evidence. BMC Geriatr. 2015, 15, 16. [Google Scholar] [CrossRef] [Green Version]
- Aplin, D.Y. Psychological assessment of multi-channel cochlear implant patients. J. Laryngol. Otol. 1993, 107, 298–304. [Google Scholar] [CrossRef]
- Livingston, G.; Sommerlad, A.; Orgeta, V.; Costafreda, S.G.; Huntley, J.; Ames, D.; Ballard, C.; Banerjee, S.; Burns, A.; Cohen-Mansfield, J.; et al. Dementia prevention, intervention, and care. Lancet 2017, 390, 2673–2734. [Google Scholar] [CrossRef] [Green Version]
- Mosnier, I.; Vanier, A.; Bonnard, D.; Lina-Granade, G.; Truy, E.; Bordure, P.; Godey, B.; Marx, M.; Lescanne, E.; Venail, F.; et al. Long-term cognitive prognosis of profoundly deaf older adults after hearing rehabilitation using cochlear implants. J. Am. Geriatr. Soc. 2018, 66, 1553–1561. [Google Scholar] [CrossRef] [PubMed]
- Völter, C.; Götze, L.; Dazert, S.; Falkenstein, M.; Thomas, J.P. Can cochlear implantation improve neurocognition in the aging population? Clin. Interv. Aging 2018, 13, 701–712. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Volter, C.; Gotze, L.; Falkenstein, M.; Dazert, S.; Thomas, J.P. Application of a computer-based neurocognitive assessment battery in the elderly with and without hearing loss. Clin. Interv. Aging 2017, 12, 1681–1690. [Google Scholar] [CrossRef] [Green Version]
- Sarant, J.; Harris, D.; Busby, P.; Maruff, P.; Schembri, A.; Dowell, R.; Briggs, R. The effect of cochlear implants on cognitive function in older adults: Initial baseline and 18-month follow up results for a prospective international longitudinal study. Front. Neurosci. 2019, 13, 789. [Google Scholar] [CrossRef] [Green Version]
- Randolph, C.; Tierney, M.C.; Mohr, E.; Chase, T.N. The Repeatable Battery for the Assessment of Neuropsychological Status (RBANS): Preliminary clinical validity. J. Clin. Exp. Neuropsychol. 1998, 20, 310–319. [Google Scholar] [CrossRef] [PubMed]
| Before Implantation | 12 Months after Implantation | Level of Sig. Two-Tailed | |
|---|---|---|---|
| OI-total | 2.29 ± 0.60 | 3.02 ± 0.63 | p < 0.01 |
| OI-quiet | 2.62 ± 0.75 | 3.37 ± 0.85 | p < 0.01 |
| OI-noise | 1.81 ± 0.57 | 2.66 ± 0.65 | p < 0.01 |
| OI-localization | 2.63 ± 0.99 | 3.03 ± 0.94 | p < 0.05 |
| Before Implantation | 12 Months after First CI Fitting | Level of Significance | Effect Size | |||
|---|---|---|---|---|---|---|
| MV ± SD | Range | MV ± SD | Range | Two-tailed | ||
| Subtest Scaled Score | ||||||
| Digit Span | 22.9 ± 5.9 | 14–34 | 24.1 ± 5.5 | 15–38 | p = 0.51 | |
| Arithmetic | 12.5 ± 3.4 | 5–18 | 13.3 ± 3.6 | 8–22 | p = 0.12 | |
| Symbol Search | 19.3 ± 7.0 | 6–33 | 21.0 ± 7.1 | 7–38 | p = 0.14 | |
| Coding | 46.8 ± 14.7 | 23–74 | 49.6 ± 16.9 | 20–82 | p = 0.09 | |
| Composite Score | ||||||
| Working Memory | 92.7 ± 15.2 | 63–120 | 98.1 ± 15.3 | 74–139 | p < 0.05 | r = 0.33 |
| Processing Speed | 97.2 ± 16.2 | 70–133 | 101.9 ± 15.8 | 70–126 | p < 0.05 | r = 0.35 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knopke, S.; Schubert, A.; Häussler, S.M.; Gräbel, S.; Szczepek, A.J.; Olze, H. Improvement of Working Memory and Processing Speed in Patients over 70 with Bilateral Hearing Impairment Following Unilateral Cochlear Implantation. J. Clin. Med. 2021, 10, 3421. https://doi.org/10.3390/jcm10153421
Knopke S, Schubert A, Häussler SM, Gräbel S, Szczepek AJ, Olze H. Improvement of Working Memory and Processing Speed in Patients over 70 with Bilateral Hearing Impairment Following Unilateral Cochlear Implantation. Journal of Clinical Medicine. 2021; 10(15):3421. https://doi.org/10.3390/jcm10153421
Chicago/Turabian StyleKnopke, Steffen, Arvid Schubert, Sophia Marie Häussler, Stefan Gräbel, Agnieszka J. Szczepek, and Heidi Olze. 2021. "Improvement of Working Memory and Processing Speed in Patients over 70 with Bilateral Hearing Impairment Following Unilateral Cochlear Implantation" Journal of Clinical Medicine 10, no. 15: 3421. https://doi.org/10.3390/jcm10153421
APA StyleKnopke, S., Schubert, A., Häussler, S. M., Gräbel, S., Szczepek, A. J., & Olze, H. (2021). Improvement of Working Memory and Processing Speed in Patients over 70 with Bilateral Hearing Impairment Following Unilateral Cochlear Implantation. Journal of Clinical Medicine, 10(15), 3421. https://doi.org/10.3390/jcm10153421








