Abstract
Type 2 diabetes mellitus (DM) patients are at a higher risk for developing lung cancer due to immune dysfunction and chronic inflammation. They also have increased morbidity and mortality related to influenza, and it is recommended that they receive an annual influenza vaccination. In this study, we evaluate whether influenza vaccination could reduce the incidence of lung cancer in DM patients. This cohort study included DM patients (≥55 years old) between 1 January 2002 and 31 December 2012 by using the Taiwan Health Insurance Database. Cox proportional hazard regression method was used to compare the relation between the influenza vaccination and lung cancer incidence after adjusting for potential confounders. Sub-group analyses were done according to vaccination status (unvaccinated, total number of vaccinations: 1, 2–3, ≥4) and evaluated the dose-dependent effects on lung cancer events. Among 22,252 eligible DM patients, 7860 (35.32%) received an influenza vaccination and 67.68% (14392) did not receive an influenza vaccination. Lung cancer incidence was significantly lower in the vaccinated group versus the unvaccinated group (adjusted HR 0.77; 95% CI 0.62–0.95, p < 0.05). Significant protective effects were observed among male sex (adjusted HR 0.72; 95% CI 0.55–0.94, p < 0.05) and 55–64 year (adjusted HR 0.61; 95% CI 0.40–0.94, p < 0.05) and ≥75 year (adjusted HR 0.63; 95% CI 0.42–0.92, p < 0.05) age groups, respectively. A dose-dependent protective effect was noted with a significant protective effect in those that received ≥4 vaccinations (adjusted HR 0.42; 95% CI 0.29–0.61, p < 0.001). In sub-group analysis, elder patients with ≥65 years of age were significantly protected from ≥4 vaccinations (adjusted HR 0.37; 95% CI 0.23–0.62, p < 0.001 in 65–74 years and adjusted HR 0.31; 95% CI 0.15–0.66, p = 0.002 in ≥75 years group, respectively). Male sex with ≥4 vaccinations had a significantly lower risk of lung cancer (adjusted HR 0.35; 95% CI 0.21–0.57, p < 0.001). Patients with comorbid conditions that received ≥4 vaccinations were also protected, and was especially significant among those with CCI ≥ 3 (adjusted HR 0.38; 95% CI 0.18–0.80, p = 0.009) as compared to 1 and 2–3 vaccination groups, including those with hypertension (adjusted HR 0.35; 95% CI 0.22–0.57, p < 0.001). This population-based cohort study demonstrated that annual influenza vaccination significantly reduced the lung cancer risk in DM patients and specifically demonstrates that a higher number of vaccinations is related with a more protective effect. Whether this is due to vaccine booster effects on anti-tumor immune regulation among DM patients still needs to be explored.
1. Introduction
Taiwan’s diabetic population has increased alarmingly in recent years and its prevalence ranges between 4.9% and 9.2%. Patients with type 2 diabetes have a significant risk for a number of cancers, including liver and pancreas [1,2,3,4]. Many cohort studies revealed an elevated risk of lung cancer in diabetic patients especially among women [5,6,7]. Diabetes is regarded as an independent risk factor for lung cancer among non-smokers [8]. Preclinical studies suggested several mechanisms related to diabetes as a risk for lung cancer development and growth. Hyperinsulinemia and insulin resistance promote cancer development through stimulation of insulin-like growth factor and its receptors [9,10]. Hyperglycemia increases oxidative stress and chronic inflammation which further damage the lung structures [11]. Chronic lung damage such as emphysema is known as an independent risk factor for lung cancer development [12]. A recent meta-analysis proved that diabetes independently increased the risk of lung cancer after controlling for age, smoking and alcohol [13]. Furthermore, a meta-analysis also exhibited a relation between DM with poorer prognosis in lung cancer patients [14]. In short, lung cancer is an important and critical issue among diabetic patients.
On the other hand, since DM patients have a higher risk of developing complications with influenza infection, the Taiwan government recommends annual influenza vaccinations for diabetic patients as per the Advisory Committee on Immunization Practices (ACIP) [15]. In our previous study, we found that influenza vaccinations reduced the risk of lung cancer among chronic lung disease patients [16]. Since chronic inflammation and immune dysfunction are key shared pathogenesis of both diabetes and chronic lung destruction for lung cancer development, we consider the influenza vaccination might be of benefit to DM patients against lung cancer. Thus, in this population-based cohort study, we evaluate whether the influenza vaccination reduces lung cancer risk among DM patients.
2. Materials and Methods
We used the nationwide database, National Health Insurance Research Database (NHIRD) to analyze the influence of influenza vaccination on lung cancer among diabetic patients. The Taiwan National Health Insurance (NHI) program, established in 1995, is a national comprehensive health insurance provided to all residents of Taiwan and more than 98% of the total population is covered under the NHI program. We screened patients who visited all healthcare facilities with a diagnosis of type 2 diabetes mellitus (DM) (International Classification of Disease, the 9th Revision, Clinical Modification Code) over an 11 year period (n = 151,605) from 1 January, 2002 to 31 December, 2012. Patients with 1. at least two subsequent DM visits or one hospital admission with a diagnosis of DM and 2. at least two incidences of using diabetic medications (n = 85,516) were included in the study. The initial study cohort included 26,957 DM patients after exclusion of those with 1. age <55 years (n = 32,857), 2. diagnosed as DM before 2002 (n = 24,518) and 3. type I DM (n = 1184). The final study cohort included 22,252 DM patients after further exclusion of those 1. diagnosed with any cancer (n = 2807) and 2. that took any vaccination within 6 months (n = 1898) before the date of entry (Figure 1).
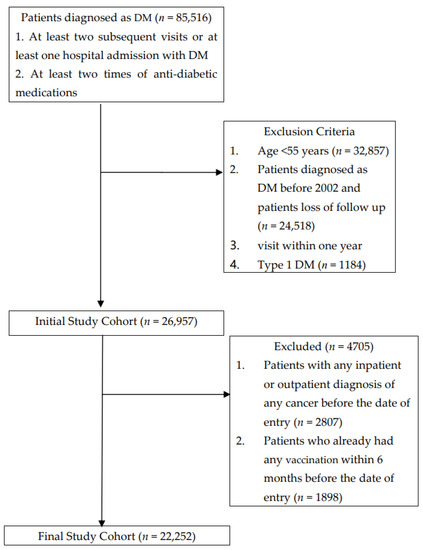
Figure 1.
Data Selection Process.
Taiwan NIH implemented mandatory influenza vaccination among the high-risk elderly population in 1998 (people aged ≥50 years with type 2 diabetes, chronic liver infection of liver cirrhosis, cardiovascular diseases, or chronic pulmonary disease, etc.) and all older people >65 years of age since 2001 [9]. The vaccination status of each study subject was recognized by code V048 and/or the use of vaccine (confirmed by drug codes). The primary endpoints of our study were incidence of lung cancer (ICD-9-CM codes 162.X) in type 2 DM patients. This study was approved by the Joint Institutional Review Board of Taipei Medical University (approval no. N201804043, on 26 April 2018). Each individual’s Charlson Comorbidity Index (CCI) and other comorbid conditions (e.g., hypertension, dyslipidemia, etc.) and the associated medications such as statins, aspirin and anti-hypertensive agents ACEI and ARB were analyzed.
Statistical Analysis
Propensity scores (PS) method was used to reduce the selection bias in the comparison of the vaccinated group and the non-vaccinated group by accounting for the covariates with a logistic regression model [17]. The Chi-square test was used for categorical variables and the t-test was used for continuous variables. The association between influenza vaccination and lung cancer in DM patients was analyzed by Cox proportional hazards regression analysis. The influence of the dose-effect of influenza vaccinations on incidence of lung cancer was determined; DM patients were categorized into four groups according to vaccination status (unvaccinated, total number of vaccinations: 1, 2 and 3, and ≥4). These data were stratified as patients’ age, sex, comorbidity conditions, and chronic medication use. Sensitivity analysis was done to evaluate the differences and consistencies between the influenza vaccination use and the risk of lung cancer in DM patients. All statistical analyses were performed by using SPSS 22.0 and SAS 9.4 software. The significance criterion was set at p < 0.05.
3. Results
Among a total of 22,252 eligible DM patients, 7860 (35.32%) received influenza vaccinations and 67.68% (14,392) did not receive influenza vaccinations (Table 1). A significant difference (p < 0.001) between the two groups including distributions of age, sex, use and number of anti-diabetic medications, co-medications, level of urbanization and monthly income was observed (Table 1). The prevalence of certain preexisting medical comorbidities, including CCI index (p < 0.001) and hypertension (p < 0.001), was higher in the vaccinated than the unvaccinated group. The vaccinated group had a higher percentage of anti-diabetic medication use (including insulin and analogues, sulfonamides, alpha glucosidase inhibitors and thiazolidinediones) and of >3 anti-diabetic medications than the unvaccinated group (p < 0.001). Analyzing comorbidities-associated medication use revealed a longer use of statins (p < 0.001), aspirin (p < 0.001), anti-hypertensive agent, angiotensin-converting enzyme (ACE) inhibitor and angiotensin receptor blocker (ARB) (p < 0.001) among the vaccinated group than in the unvaccinated group.

Table 1.
Characteristics of the Study Population.
We analyzed the incidence of lung cancer among DM patients with or without influenza vaccination (Table 2). After adjustment for potential confounders, the incidence of lung cancer was significantly lower in the vaccinated group as compared to the unvaccinated group (adjusted HR 0.77; 95% CI 0.62–0.95, p < 0.05). Significant protective effects were observed among the male sex (adjusted HR 0.72; 95% CI 0.55–0.94, p < 0.05) and the 55–64 years (adjusted HR 0.61; 95% CI 0.40–0.94, p < 0.05) and ≥75 years (adjusted HR 0.63; 95% CI 0.42–0.92, p < 0.05) age groups, respectively (Table 2).

Table 2.
Risk of Lung Cancer among Unvaccinated and Vaccinated DM patients.
The sensitivity analysis adjustments were done to evaluate the association of influenza vaccinated patients with the risk of lung cancer in different models, stratifying by the total number of vaccinations (Table 3). Interestingly, a dose-dependent protective effect was noted in the main model with a significant protective effect in those that received ≥4 vaccinations (adjusted HR 0.42; 95% CI 0.29–0.61, p < 0.001). In sub-group analysis, elder patients over ≥65 years of age were significantly protected from ≥4 vaccinations (adjusted HR 0.37; 95% CI 0.23–0.62, p < 0.001 in 65–74 years and adjusted HR 0.31; 95% CI 0.15–0.66, p = 0.002 in ≥75 years group, respectively). Male sex with ≥4 vaccinations had a significantly lower risk for lung cancer (adjusted HR 0.35; 95% CI 0.21–0.57, p < 0.001). Patients with ≥4 vaccinations were also protected among those with comorbid conditions, especially significant among those with CCI ≥3 (adjusted HR 0.38; 95% CI 0.18–0.80, p = 0.009) as compared to 1 and 2–3 vaccination groups, including those with hypertension (adjusted HR 0.35; 95% CI 0.22–0.57, p < 0.001). However, the protective effects of vaccination doses did not significantly differ with type or number of anti-diabetic medications (Table 3).

Table 3.
Sensitivity Analysis of Adjusted HRs of Vaccination in Risk Reduction of Lung Cancer among DM patients.
4. Discussion
Our DM population revealed that patients in the vaccinated group were older, female prevalent, had higher CCI index scores and related with hypertension more than the unvaccinated group. Significantly more patients in the vaccinated group had more anti-diabetic agents use and longer co-medications use as compared to the unvaccinated group. As per Taiwan government-funded influenza vaccinations policy, all diabetic patients are considered to be at high risk from influenza infection and mortality, and were recommended to take the vaccination [15]. To our knowledge, no previous study has been reported about the influence of influenza vaccinations on lung cancer risk among diabetic patients. This is the first population-based cohort study that revealed the significant reduction of lung cancer risk with influenza vaccination among type 2 DM patients. An impairment of metabolism-immune axis in type 2 DM is believed to relate with development and progression of neoplasm [18,19]. Reduced glycolysis and basal cellular mitochondrial respiration in type 2 diabetes mellitus was related with decreased circulating CD8 + T cells and led to the production impairment of various cytokines [20]. Most of the identified studies state that the immunogenicity of influenza vaccination among DM patients is comparable to healthy or non-diabetic patients [21,22,23]. The seasonal influenza vaccination generates systemic CD8+ T cell-mediated antitumor immunity [24], which also boosts the response to anti-tumor treatment.
After adjustments for age, sex, CCI Index, co-morbid conditions, medications use, level of urbanization and monthly income, the lung cancer incidence was significantly lower in the influenza vaccinated group. This trend was reduced in both sexes, however, it was more significant in diabetic men. The higher prevalence of smoking among male patients might explain the significant lung cancer prevention from influenza vaccination over female patients. In Taiwan, the smoking rates for 55 years or older males and females were 20.5% and 2.4% in 2002; 14% and 1.53% in 2012, respectively [25]. The lower smoking rate in females might be related with traditional Chinese culture. Tobacco use has been reported to be the main cause of lung cancers and the risk is 20–40 times higher in smokers than non-smokers [26]. Through damaging the local cellular and humoral immunity in respiratory system [27,28], smoking facilitates influenza viral infection and consequent pneumonia [29,30]. A previous study also revealed that smokers and ex-smokers had an increased risk of influenza related hospitalization and severity [31]. Other studies also revealed a sex difference in antibody response after influenza vaccination [32,33,34]. However, the mechanism underlying such lung cancer protective effects of influenza vaccination on gender difference is not fully understood.
Interestingly, the potential “dose-dependent” protective effect was noted between cumulative doses of influenza shot and the risk of lung cancer among type 2 DM patients. Further analysis revealed that patients of increasing age ≥65 years, regardless of sex and CCI index, those with hypertension and those with fewer anti-diabetic medications were significantly protected by ≥4 vaccination. Higher vaccination dose requirements in elder male patients could be related with their smoking status, since smoking reduced the effectiveness of the influenza vaccination [31]. We couldn’t determine whether the patients received annual vaccinations yearly for more than 4 years or received vaccinations ≥ 4 times over the observation period. However, from our study, its protective effect seemed to be related to the cumulative dose effect. A previous study in the Taiwanese population revealed that cumulative exposure to influenza infection increased the risk of lung cancer [35]. The study revealed a 25% increased risk of lung cancer in patients with ≥5 episodes of influenza infection [35]. This might explain our finding of cumulative anti-influenza shots being related to decreased risk for lung cancer, and the underlying mechanisms might be due to improvements in chronic inflammation and booster immune status against lung cancer among DM patients. Future in vitro and in vivo studies are needed to investigate these underlying mechanisms and broaden the knowledge of influenza vaccination to prevent and treat lung cancer.
This is a population-based study on type 2 DM patients regarding the possible protective effects of influenza vaccine against lung cancer. Several limitations still need to be considered as with other observational studies based on clinical databases. Important environmental risk factors for lung cancer such as smoking status was not available from this database. No cause–relation could derive from such a database, however, we revealed a significant reduction of lung cancer risk in male patients. Since a previous meta-analysis study revealed that diabetes mellitus itself is related to an increased risk for lung cancer after adjusting for smoking status [13], we suppose the use of vaccination in male diabetic patients is still important. Second, the diagnoses of diabetes mellitus, comorbidities and medication use were identified based on the ICD-9 codes or drug codes alone. We used propensity score (PS) matching to reduce the selection bias by accounting for the covariates with a logistic regression mode [17]. We further applied sensitivity analyses and adjustments of confounding factors using a large number of stratifications to compare between the groups to avoid the influence of interference factors. Moreover, as an intrinsic weakness of the database, no biochemical data was available and we couldn’t evaluate the duration or severity of DM in our population. Other unmeasured confounders, including body mass index, alcohol drinking, and use of over-the-counter medications, etc., were not available. We also couldn’t identify which brand of vaccine our population received from such a database; however, in Taiwan, patients over 55 years with diabetes mellitus were eligible and recommended for publicly funded influenza vaccine. Since qualified people received flu shots at public expense free of charge, most of them took similar brands of influenza vaccine. Though we couldn’t detect those without public brands, we believe the number was negligible and might not influence our results. Although these limitations did not seem to compromise the significant findings of our results, we still can’t establish a cause–effect relationship from our study; we still need future prospective randomized studies to verify our findings.
5. Conclusions
Our study demonstrated the importance of administering influenza vaccinations among diabetic patients for preventing lung cancer. We recommend influenza vaccination in all diabetic patients regardless of age, sex and co-morbid conditions and specifically believe that these patients might need more influenza vaccinations to boost its protective effects against lung cancer. Why and how cumulative doses of influenza vaccinations should be enough for these population is still unclear and needs to be explored through future prospective trials.
Author Contributions
Conceptualization, J.-Q.Z. and C.-C.C. (Chun-Chao Chen); methodology, J.-Q.Z.; software, Y.-F.L.; validation, J.-Q.Z., C.-C.C. (Chun-Chao Chen) and C.-C.C. (Chun-Chih Chiu); formal analysis, T.Y.Y.; investigation, J.-Q.Z. and W.-R.H.; resources, M.-H.H.; data curation, Y.-A.F.; writing—original draft preparation, J.-Q.Z.; writing—review and editing, K.-Y.L.; visualization, C.-C.C. (Chun-Chao Chen); supervision, K.-Y.L.; project administration, C.-H.L.; funding acquisition, J.-C.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the Ministry of Science and Technology of the Republic of China (MOST 108-2314-B-038-016, MOST 109-2314-B-038-086), Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan, and granted by Ministry of Health and Welfare (MOHW110-TDU-B-212-124007).
Institutional Review Board Statement
This study was approved by the Joint Institutional Review Board of Taipei Medical University (approval no. N201804043, on 26 April 2018).
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors report no conflict of interest.
References
- Song, S.; Wang, B.; Zhang, X.; Hao, L.; Hu, X.; Li, Z.; Sun, S. Long-Term Diabetes Mellitus Is Associated with an Increased Risk of Pancreatic Cancer: A Meta-Analysis. PLoS ONE 2015, 10, e0134321. [Google Scholar] [CrossRef] [PubMed]
- Sasazuki, S.; Charvat, H.; Hara, A.; Wakai, K.; Nagata, C.; Nakamura, K.; Tsuji, I.; Sugawara, Y.; Tamakoshi, A.; Matsuo, K.; et al. Diabetes mellitus and cancer risk: Pooled analysis of eight cohort studies in Japan. Cancer Sci. 2013, 104, 1499–1507. [Google Scholar] [CrossRef]
- Hope, C.; Robertshaw, A.; Cheung, K.L.; Idris, I.; English, E. Relationship between HbA1c and cancer in people with or without diabetes: A systematic review. Diabet. Med. 2016, 33, 1013–1025. [Google Scholar] [CrossRef] [PubMed]
- Agache, A.; Mustatea, P.; Mihalache, O.; Bobirca, F.T.; Georgescu, D.E.; Jauca, C.M.; Birligea, A.; Doran, H.; Patrascu, T. Diabetes Mellitus as a Risk-factor for Colorectal Cancer Literature Review-Current Situation and Future Perspectives. Chirurgia 2018, 113, 603–610. [Google Scholar] [CrossRef]
- Kuriki, K.; Hirose, K.; Tajima, K. Diabetes and cancer risk for all and specific sites among Japanese men and women. Eur. J. Cancer Prev. 2007, 16, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Luo, J.; Chlebowski, R.; Wactawski-Wende, J.; Schlecht, N.F.; Tinker, L.; Margolis, K.L. Diabetes and lung cancer among postmenopausal women. Diabet. Care 2012, 35, 1485–1491. [Google Scholar] [CrossRef]
- Jee, S.H.; Ohrr, H.; Sull, J.W.; Yun, J.E.; Ji, M.; Samet, J.M. Fasting serum glucose level and cancer risk in Korean men and women. JAMA 2005, 293, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Pallis, A.G.; Syrigos, K.N. Lung cancer in never smokers: Disease characteristics and risk factors. Crit. Rev. Oncol. Hematol. 2013, 88, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Argiles, J.M.; Lopez-Soriano, F.J. Insulin and cancer (Review). Int. J. Oncol. 2001, 18, 683–687. [Google Scholar] [CrossRef]
- Strickler, H.D.; Wylie-Rosett, J.; Rohan, T.; Hoover, D.R.; Smoller, S.; Burk, R.D.; Yu, H. The relation of type 2 diabetes and cancer. Diabetes. Technol. Ther. 2001, 3, 263–274. [Google Scholar] [CrossRef] [PubMed]
- Forgiarini, L.A., Jr.; Kretzmann, N.A.; Porawski, M.; Dias, A.S.; Marroni, N.A. Experimental diabetes mellitus: Oxidative stress and changes in lung structure. J. Bras. Pneumol. 2009, 35, 788–791. [Google Scholar] [CrossRef]
- Lee, G.; Walser, T.C.; Dubinett, S.M. Chronic inflammation, chronic obstructive pulmonary disease, and lung cancer. Curr. Opin. Pulm. Med. 2009, 15, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.Y.; Jeon, I.; Lee, J.M.; Yoon, J.M.; Park, S.M. Diabetes mellitus as an independent risk factor for lung cancer: A meta-analysis of observational studies. Eur. J. Cancer 2013, 49, 2411–2423. [Google Scholar] [CrossRef]
- Zhu, L.; Cao, H.; Zhang, T.; Shen, H.; Dong, W.; Wang, L.; Du, J. The Effect of Diabetes Mellitus on Lung Cancer Prognosis: A PRISMA-compliant Meta-analysis of Cohort Studies. Medicine 2016, 95, e3528. [Google Scholar] [CrossRef]
- Chan, T.C.; Fu, Y.C.; Wang, D.W.; Chuang, J.H. Determinants of receiving the pandemic (H1N1) 2009 vaccine and intention to receive the seasonal influenza vaccine in Taiwan. PLoS ONE 2014, 9, e101083. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.Y.; Wu, S.M.; Liu, J.C.; Lee, K.Y. Effect of annual influenza vaccination on reducing lung cancer in patients with chronic obstructive pulmonary disease from a population-based cohort study. Medicine 2019, 98, e18035. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, R.B., Jr. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. Med. 1998, 17, 2265–2281. [Google Scholar] [CrossRef]
- Allard, R.; Leclerc, P.; Tremblay, C.; Tannenbaum, T.N. Diabetes and the severity of pandemic influenza A (H1N1) infection. Diabetes Care 2010, 33, 1491–1493. [Google Scholar] [CrossRef] [PubMed]
- Wilking, H.; Buda, S.; von der Lippe, E.; Altmann, D.; Krause, G.; Eckmanns, T.; Haas, W. Mortality of 2009 pandemic influenza A(H1N1) in Germany. Euro. Surveill. 2010, 15, 19741. [Google Scholar] [CrossRef]
- Nojima, I.; Eikawa, S.; Tomonobu, N.; Hada, Y.; Kajitani, N.; Teshigawara, S.; Miyamoto, S.; Tone, A.; Uchida, H.A.; Nakatsuka, A.; et al. Dysfunction of CD8 + PD-1 + T cells in type 2 diabetes caused by the impairment of metabolism-immune axis. Sci. Rep. 2020, 10, 14928. [Google Scholar] [CrossRef]
- Sheridan, P.A.; Paich, H.A.; Handy, J.; Karlsson, E.A.; Schultz-Cherry, S.; Hudgens, M.; Weir, S.; Noah, T.; Beck, M.A. The antibody response to influenza vaccination is not impaired in type 2 diabetics. Vaccine 2015, 33, 3306–3313. [Google Scholar] [CrossRef] [PubMed]
- Seo, Y.B.; Baek, J.H.; Lee, J.; Song, J.Y.; Lee, J.S.; Cheong, H.J.; Kim, W.J. Long-Term Immunogenicity and Safety of a Conventional Influenza Vaccine in Patients with Type 2 Diabetes. Clin. Vaccine Immunol. 2015, 22, 1160–1165. [Google Scholar] [CrossRef] [PubMed]
- McElhaney, J.E.; Garneau, H.; Camous, X.; Dupuis, G.; Pawelec, G.; Baehl, S.; Tessier, D.; Frost, E.H.; Frasca, D.; Larbi, A.; et al. Predictors of the antibody response to influenza vaccination in older adults with type 2 diabetes. BMJ Open. Diabetes Res. Care 2015, 3, e000140. [Google Scholar] [CrossRef]
- Newman, J.H.; Chesson, C.B.; Herzog, N.L.; Bommareddy, P.K.; Aspromonte, S.M.; Pepe, R.; Estupinian, R.; Aboelatta, M.M.; Buddhadev, S.; Tarabichi, S.; et al. Intratumoral injection of the seasonal flu shot converts immunologically cold tumors to hot and serves as an immunotherapy for cancer. Proc. Natl. Acad. Sci. USA 2020, 117, 1119–1128. [Google Scholar] [CrossRef] [PubMed]
- Chang, F.C.; Sung, H.Y.; Zhu, S.H.; Chiou, S.T. Impact of the 2009 Taiwan tobacco hazards prevention act on smoking cessation. Addiction 2014, 109, 140–146. [Google Scholar] [CrossRef]
- Ozlu, T.; Bulbul, Y. Smoking and lung cancer. Tuberk. Toraks 2005, 53, 200–209. [Google Scholar] [PubMed]
- Murin, S.; Bilello, K.S. Respiratory tract infections: Another reason not to smoke. Cleve Clin. J. Med. 2005, 72, 916–920. [Google Scholar] [CrossRef]
- Feng, Y.; Kong, Y.; Barnes, P.F.; Huang, F.F.; Klucar, P.; Wang, X.; Samten, B.; Sengupta, M.; Machona, B.; Donis, R.; et al. Exposure to cigarette smoke inhibits the pulmonary T-cell response to influenza virus and Mycobacterium tuberculosis. Infect. Immun. 2011, 79, 229–237. [Google Scholar] [CrossRef]
- Epstein, M.A.; Reynaldo, S.; El-Amin, A.N. Is smoking a risk factor for influenza hospitalization and death? J. Infect. Dis. 2010, 201, 794–795. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Almirall, J.; Bolibar, I.; Serra-Prat, M.; Roig, J.; Hospital, I.; Carandell, E.; Agusti, M.; Ayuso, P.; Estela, A.; Torres, A.; et al. New evidence of risk factors for community-acquired pneumonia: A population-based study. Eur. Respir. J. 2008, 31, 1274–1284. [Google Scholar] [CrossRef] [PubMed]
- Godoy, P.; Castilla, J.; Soldevila, N.; Mayoral, J.M.; Toledo, D.; Martin, V.; Astray, J.; Egurrola, M.; Morales-Suarez-Varela, M.; Dominguez, A.; et al. Smoking may increase the risk of influenza hospitalization and reduce influenza vaccine effectiveness in the elderly. Eur J. Public Health 2018, 28, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Chambers, C.; Skowronski, D.M.; Rose, C.; Serres, G.; Winter, A.L.; Dickinson, J.A.; Jassem, A.; Gubbay, J.B.; Fonseca, K.; Drews, S.J.; et al. Should Sex Be Considered an Effect Modifier in the Evaluation of Influenza Vaccine Effectiveness? Open. Forum. Infect. Dis. 2018, 5, ofy211. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Pekosz, A. Sex-based biology and the rational design of influenza vaccination strategies. J. Infect. Dis. 2014, 209, S114–S119. [Google Scholar] [CrossRef]
- Gabriel, G.; Arck, P.C. Sex, immunity and influenza. J. Infect. Dis. 2014, 209, S93–S99. [Google Scholar] [CrossRef] [PubMed]
- Weng, C.F.; Chen, L.J.; Lin, C.W.; Chen, H.M.; Lee, H.H.; Ling, T.Y.; Hsiao, F.Y. Association between the risk of lung cancer and influenza: A population-based nested case-control study. Int. J. Infect. Dis. 2019, 88, 8–13. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).