Asthma, Allergic Rhinitis, and Atopic Dermatitis Incidence in Korean Adolescents before and after COVID-19
Abstract
:1. Introduction
2. Materials and Methods
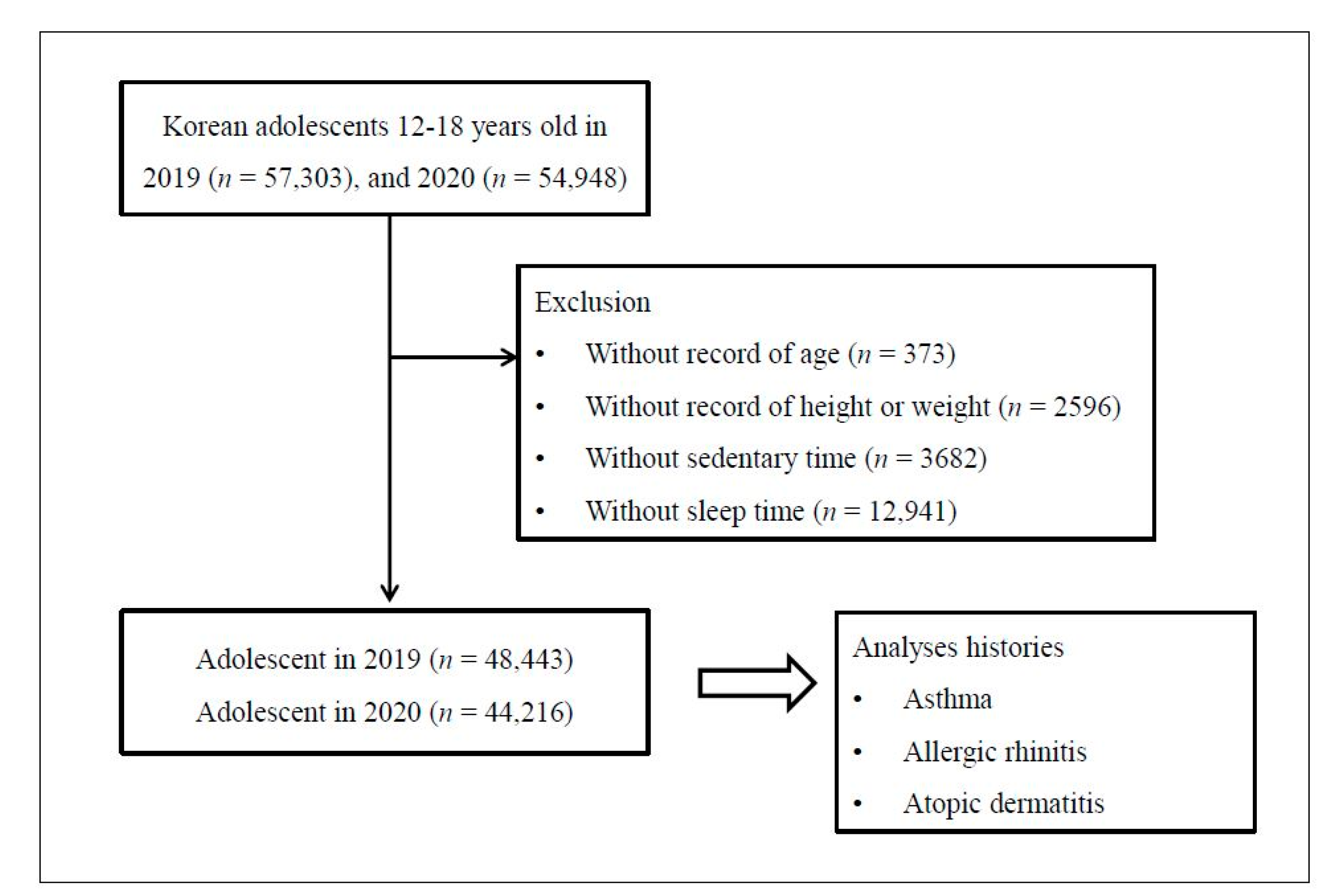
2.1. Study Population and Data Collection
2.2. Survey
2.2.1. Exposure
2.2.2. Outcome
2.2.3. Covariate
- (1)
- unknown, missing or below middle school
- (2)
- high school
- (3)
- college, or over
2.3. Statistical Analysis
3. Results
3.1. General Differences of Variables and Reporting (Incidence) of Allergic Diseases between 2019 and 2020 Korean Adolescent Population
3.2. The Adjusted Odd Ratios for Allergic Diseases in 2020 Compared to 2019 in Korean Adolescents
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pawankar, R. Allergic diseases and asthma: A global public health concern and a call to action. World Allergy Organ. J. 2014, 7, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nicolaou, N.; Siddique, N.; Custovic, A. Allergic disease in urban and rural populations: Increasing prevalence with increasing urbanization. Allergy 2005, 60, 1357–1360. [Google Scholar] [CrossRef]
- Yoo, B.; Park, Y.; Park, K.; Kim, H. A 9-year Trend in the Prevalence of Allergic Disease Based on National Health Insurance Data. J. Prev. Med. Public Health 2015, 48, 301–309. [Google Scholar] [CrossRef] [Green Version]
- Kim, B.K.; Kim, J.Y.; Kang, M.K.; Yang, M.S.; Park, H.W.; Min, K.U.; Cho, S.H.; Kang, H.R. Allergies are still on the rise? A 6-year nationwide population-based study in Korea. Allergol. Int. 2016, 65, 186–191. [Google Scholar] [CrossRef] [Green Version]
- Song, W.J.; Wong, G.W.K. Changing trends and challenges in the management of asthma in Asia. J. Allergy Clin. Immunol. 2017, 140, 1272–1274. [Google Scholar] [CrossRef] [Green Version]
- Hong, S.; Son, D.K.; Lim, W.R.; Kim, S.H.; Kim, H.; Yum, H.Y.; Kwon, H. The prevalence of atopic dermatitis, asthma, and allergic rhinitis and the comorbidity of allergic diseases in children. Environ. Health Toxicol. 2012, 27, e2012006. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.; Lee, S.W.; Yon, D.K. Ten-Year trends and prevalence of asthma, allergic rhinitis, and atopic dermatitis among the Korean population, 2008–2017. Clin. Exp. Pediatr. 2020, 63, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Kang, S.Y.; Song, W.J.; Cho, S.H.; Chang, Y.S. Time trends of the prevalence of allergic diseases in Korea: A systematic literature review. Asia Pac. Allergy 2018, 8, e8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Korea Center For Disease Control and Prevention. Available online: http://www.kdca.go.kr/yhs (accessed on 15 May 2021).
- Bae, J.; Joung, H.; Kim, J.Y.; Kwon, K.N.; Kim, Y.T.; Park, S.W. Test-retest reliability of a questionnaire for the Korea Youth Risk Behavior Web-based Survey. J. Prev. Med. Public Health 2010, 43, 403–410. [Google Scholar] [CrossRef]
- Bae, J.; Joung, H.; Kim, J.Y.; Kwon, K.N.; Kim, Y.; Park, S.W. Validity of self-reported height, weight, and body mass index of the Korea Youth Risk Behavior Web-based Survey questionnaire. J. Prev. Med. Public Health 2010, 43, 396–402. [Google Scholar] [CrossRef] [PubMed]
- The Global Asthma Network. The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three Manual. Available online: http://isaac.auckland.ac.nz/resources/tools.php?menu=tools1#quest (accessed on 15 May 2021).
- Ellwood, P.; Asher, M.I.; Beasley, R.; Clayton, T.O.; Stewart, A.W.; Committee, I.S. The international study of asthma and allergies in childhood (ISAAC): Phase three rationale and methods. Int. J. Tuberc. Lung Dis. 2005, 9, 10–16. [Google Scholar] [PubMed]
- Chen, W.; Mempel, M.; Schober, W.; Behrendt, H.; Ring, J. Gender difference, sex hormones, and immediate type hypersensitivity reactions. Allergy 2008, 63, 1418–1427. [Google Scholar] [CrossRef] [PubMed]
- Stanton, R.; To, Q.G.; Khalesi, S.; Williams, S.L.; Alley, S.J.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. Depression, Anxiety and Stress during COVID-19: Associations with Changes in Physical Activity, Sleep, Tobacco and Alcohol Use in Australian Adults. Int. J. Environ. Res. Public Health 2020, 17, 4065. [Google Scholar] [CrossRef]
- Giustino, V.; Parroco, A.M.; Gennaro, A.; Musumeci, G.; Palma, A.; Battaglia, G. Physical Activity Levels and Related Energy Expenditure during COVID-19 Quarantine among the Sicilian Active Population: A Cross-Sectional Online Survey Study. Sustainability 2020, 12, 4356. [Google Scholar] [CrossRef]
- Scarmozzino, F.; Visioli, F. Covid-19 and the Subsequent Lockdown Modified Dietary Habits of Almost Half the Population in an Italian Sample. Foods 2020, 9, 675. [Google Scholar] [CrossRef]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Firrincieli, V.; Keller, A.; Ehrensberger, R.; Platts-Mills, J.; Shufflebarger, C.; Geldmaker, B.; Platts-Mills, T. Decreased physical activity among head start children with a history of wheezing: Use of an accelerometer to measure activity. Pediatr. Pulm. 2005, 40, 57–63. [Google Scholar] [CrossRef]
- Tsai, H.J.; Tsai, A.C.; Nriagu, J.; Ghosh, D.; Gong, M.; Sandretto, A. Associations of BMI, TV-watching time, and physical activity on respiratory symptoms and asthma in 5th grade schoolchildren in taipei, taiwan. J. Asthma. 2007, 44, 397–401. [Google Scholar] [CrossRef]
- Jones, S.E.; Merkle, S.L.; Fulton, J.E.; Wheeler, L.S.; Mannino, D.M. Relationship between asthma, overweight, and physical activity among US high school students. J. Commun. Health 2006, 31, 469–478. [Google Scholar] [CrossRef]
- Lu, K.D.; Forno, E.; Radom-Aizik, S.; Cooper, D.M. Low fitness and increased sedentary time are associated with worse asthma-The National Youth Fitness Survey. Pediatr. Pulm. 2020, 55, 1116–1123. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Tu, Y.K.; Huang, K.C.; Chen, P.C.; Chu, D.C.; Lee, Y.L. Pathway from Central Obesity to Childhood Asthma Physical Fitness and Sedentary Time Are Leading Factors. Am. J. Respir. Crit. Care 2014, 189, 1194–1203. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S. The epidemiology of obesity and asthma. J. Allergy Clin. Immun. 2005, 115, 897–909. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Rennie, D.; Cormier, Y.; Dosman, J. Association between Obesity and Atopy in Adults. Int. Arch. Allergy Imm. 2010, 153, 372–377. [Google Scholar] [CrossRef]
- Shore, S.A.; Johnston, R.A. Obesity and asthma. Pharmacol. Ther. 2006, 110, 83–102. [Google Scholar] [CrossRef]
- Beuther, D.A.; Sutherland, E.R. Overweight, obesity, and incident asthma—A meta-analysis of prospective epidemiologic studies. Am. J. Respir. Crit. Care 2007, 175, 661–666. [Google Scholar] [CrossRef] [Green Version]
- Vlaski, E.; Stavric, K.; Isjanovska, R.; Seckova, L.; Kimovska, M. Overweight hypothesis in asthma and eczema in young adolescents. Allergol. Immunopathol. 2006, 34, 199–205. [Google Scholar] [CrossRef] [Green Version]
- Paller, A.; Jaworski, J.C.; Simpson, E.L.; Boguniewicz, M.; Russell, J.J.; Block, J.K.; Tofte, S.; Dunn, J.D.; Feldman, S.R.; Clark, A.R.; et al. Major Comorbidities of Atopic Dermatitis: Beyond Allergic Disorders. Am. J. Clin. Dermatol. 2018, 19, 821–838. [Google Scholar] [CrossRef] [PubMed]
- Tajima, H.; Pawankar, R. Obesity and adiposity indicators in asthma and allergic rhinitis in children. Curr. Opin. Allergy Clin. Immunol. 2019, 19, 7–11. [Google Scholar] [CrossRef]
- Zhou, J.B.; Luo, F.Q.; Han, Y.P.; Lou, H.F.; Tang, X.Y.; Zhang, L. Obesity/overweight and risk of allergic rhinitis: A meta-analysis of observational studies. Allergy 2020, 75, 1272–1275. [Google Scholar] [CrossRef]
- Tanaka, K.; Miyake, Y.; Arakawa, M.; Sasaki, S.; Ohya, Y. U-Shaped Association between Body Mass Index and the Prevalence of Wheeze and Asthma, but not Eczema or Rhinoconjunctivitis: The Ryukyus Child Health Study. J. Asthma 2011, 48, 804–810. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, E.A.; Beasley, R.; Bjorksten, B.; Crane, J.; Garcia-Marcos, L.; Keil, U.; Grp, I.P.T.S. The association between BMI, vigorous physical activity and television viewing and the risk of symptoms of asthma, rhinoconjunctivitis and eczema in children and adolescents: ISAAC Phase Three. Clin. Exp. Allergy 2013, 43, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Parsons, J.P.; Hallstrand, T.S.; Mastronarde, J.G.; Kaminsky, D.A.; Rundell, K.W.; Hull, J.H.; Storms, W.W.; Weiler, J.M.; Cheek, F.M.; Wilson, K.C.; et al. An official American Thoracic Society clinical practice guideline: Exercise-induced bronchoconstriction. Am. J. Respir. Crit. Care Med. 2013, 187, 1016–1027. [Google Scholar] [CrossRef]
- Jayasinghe, H.; Kopsaftis, Z.; Carson, K. Asthma Bronchiale and Exercise-Induced Bronchoconstriction. Respiration 2015, 89, 505–512. [Google Scholar] [CrossRef]
- Park, S.; Michelow, I.C.; Choe, Y.J. Shifting patterns of respiratory virus activity following social distancing measures for COVID-19 in South Korea. J. Infect. Dis. 2021. [Google Scholar] [CrossRef]
- Lee, H.; Lee, H.; Song, K.H.; Kim, E.S.; Park, J.S.; Jung, J.; Ahn, S.; Jeong, E.K.; Park, H.; Kim, H.B. Impact of Public Health Interventions on Seasonal Influenza Activity During the SARS-CoV-2 Outbreak in Korea. Clin. Infect. Dis. 2021, 73, e132–e140. [Google Scholar] [CrossRef]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Kuitunen, I.; Artama, M.; Makela, L.; Backman, K.; Heiskanen-Kosma, T.; Renko, M. Effect of Social Distancing Due to the COVID-19 Pandemic on the Incidence of Viral Respiratory Tract Infections in Children in Finland During Early 2020. Pediatric Infect. Dis. J. 2020, 39, E423–E427. [Google Scholar] [CrossRef] [PubMed]
- Choe, Y.J.; Lee, J.K. The Impact of Social Distancing on the Transmission of Influenza Virus, South Korea, 2020. Osong Public Health Res. Perspect. 2020, 11, 91–92. [Google Scholar] [CrossRef]
- Soo, R.J.J.; Chiew, C.J.; Ma, S.; Pung, R.; Lee, V. Decreased Influenza Incidence under COVID-19 Control Measures, Singapore. Emerg. Infect. Dis. 2020, 26, 1933–1935. [Google Scholar] [CrossRef]
- Gern, J.E. Viral respiratory infection and the link to asthma. Pediatr. Infect. Dis. J. 2008, 27, S97–S103. [Google Scholar] [CrossRef]
- Carroll, K.N.; Wu, P.; Gebretsadik, T.; Griffin, M.R.; Dupont, W.D.; Mitchel, E.F.; Hartert, T.V. The severity-dependent relationship of infant bronchiolitis on the risk and morbidity of early childhood asthma. J. Allergy Clin. Immunol. 2009, 123, 1055–1061.e1. [Google Scholar] [CrossRef] [Green Version]
- Nicholson, K.G.; Kent, J.; Ireland, D.C. Respiratory viruses and exacerbations of asthma in adults. BMJ 1993, 307, 982–986. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnston, S.L.; Pattemore, P.K.; Sanderson, G.; Smith, S.; Lampe, F.; Josephs, L.; Symington, P.; O′Toole, S.; Myint, S.H.; Tyrrell, D.A.; et al. Community study of role of viral infections in exacerbations of asthma in 9–11 year old children. BMJ 1995, 310, 1225–1229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chinratanapisit, S.; Suratannon, N.; Pacharn, P.; Sritipsukho, P.; Vichyanond, P. Prevalence and risk factors of allergic rhinitis in children in Bangkok area. Asian Pac. J. Allergy Immunol. 2019, 37, 232–239. [Google Scholar] [CrossRef] [PubMed]
- Kansen, H.M.; Lebbink, M.A.; Mul, J.; van Erp, F.C.; van Engelen, M.; de Vries, E.; Prevaes, S.; Le, T.M.; van der Ent, C.K.; Verhagen, L.M. Risk factors for atopic diseases and recurrent respiratory tract infections in children. Pediatr. Pulmonol. 2020, 55, 3168–3179. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Marshak, T.; Layous, E.; Zigron, A.; Shivatzki, S.; Morozov, N.G.; Taiber, S.; Alon, E.E.; Ronen, O.; et al. Reduction of allergic rhinitis symptoms with face mask usage during the COVID-19 pandemic. J. Allergy Clin. Immunol. Pract. 2020, 8, 3590–3593. [Google Scholar] [CrossRef]
- Cherrie, J.W.; Apsley, A.; Cowie, H.; Steinle, S.; Mueller, W.; Lin, C.; Horwell, C.J.; Sleeuwenhoek, A.; Loh, M. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup Environ. Med. 2018, 75, 446–452. [Google Scholar] [CrossRef]
- Skotnicka, M.; Karwowska, K.; Klobukowski, F.; Wasilewska, E.; Malgorzewicz, S. Dietary Habits before and during the COVID-19 Epidemic in Selected European Countries. Nutrients 2021, 13, 1690. [Google Scholar] [CrossRef] [PubMed]
- Gornicka, M.; Drywien, M.E.; Zielinska, M.A.; Hamulka, J. Dietary and Lifestyle Changes During COVID-19 and the Subsequent Lockdowns among Polish Adults: A Cross-Sectional Online Survey PLifeCOVID-19 Study. Nutrients 2020, 12, 2324. [Google Scholar] [CrossRef] [PubMed]
- Wasilewska, E.; Malgorzewicz, S.; Gruchala-Niedoszytko, M.; Skotnicka, M.; Jassem, E. Dietary Habits in Children with Respiratory Allergies: A Single-Center Polish Pilot Study. Nutrients 2020, 12, 1521. [Google Scholar] [CrossRef]
- Sutherland, K.; Chessman, J.; Zhao, J.; Sara, G.; Shetty, A.; Smith, S.; Went, A.; Dyson, S.; Levesque, J.F. Impact of COVID-19 on healthcare activity in NSW, Australia. Public Health Res. Pract. 2020, 30, 3042030. [Google Scholar] [CrossRef] [PubMed]
- Oreskovic, N.M.; Kinane, T.B.; Aryee, E.; Kuhlthau, K.A.; Perrin, J.M. The Unexpected Risks of COVID-19 on Asthma Control in Children. J. Allergy Clin. Immunol. Pract. 2020, 8, 2489–2491. [Google Scholar] [CrossRef] [PubMed]
- Rutter, M.D.; Brookes, M.; Lee, T.J.; Rogers, P.; Sharp, L. Impact of the COVID-19 pandemic on UK endoscopic activity and cancer detection: A National Endoscopy Database Analysis. Gut 2021, 70, 537–543. [Google Scholar] [CrossRef] [PubMed]
| General Characteristics | Participated Year | ||
|---|---|---|---|
| 2019 | 2020 | p-Value | |
| Total number, n (% *) | 48,443 (100.0) | 44,216 (100.0) | |
| Age (years, mean * (SD)) | 15.0 (1.7) | 15.1 (1.7) | <0.001 † |
| BMI (kg/m2, mean * (SD)) | 21.4 (3.5) | 21.6 (3.7) | <0.001 † |
| Physical exercise (days/week, mean * (SD)) | 2.0 (2.1) | 1.9 (2.1) | <0.001 † |
| Sedentary time for study (hour/day, mean * (SD)) | 6.6 (3.7) | 6.0 (3.3) | <0.001 † |
| Sedentary time for leisure (hour/day, mean * (SD)) | 3.3 (2.2) | 4.2 (2.7) | <0.001 † |
| Sleep time (hour/day, mean * (SD)) | 7.0 (1.5) | 6.9 (1.5) | <0.001 † |
| Sex, n (% *) | 0.498 | ||
| Male | 24,917 (51.3) | 23,103 (52.5) | |
| Female | 23,526 (48.7) | 21,113 (47.5) | |
| Economic level, n (% *) | 0.322 | ||
| High | 18,992 (39.6) | 17,381 (40.3) | |
| Middle | 23,376 (48.1) | 21,228 (47.5) | |
| Low | 6075 (12.3) | 5607 (12.2) | |
| Educational level of father, n (% *) | <0.001 ‡ | ||
| Unknown, missing, below middle school | 23,775 (48.3) | 17,957 (39.7) | |
| High school | 7385 (14.8) | 7519 (16.2) | |
| College or over | 17,283 (36.8) | 18,740 (44.0) | |
| Educational level of mother, n (% *) | <0.001 ‡ | ||
| Unknown, missing, below middle school | 23,050 (47.0) | 16,925 (37.5) | |
| High school | 8637 (17.7) | 8941 (19.6) | |
| College or over | 16,756 (35.3) | 18,350 (42.9) | |
| Subjective health status, n (% *) | 0.071 | ||
| Very healthy | 12,911 (26.4) | 12,283 (27.3) | |
| Healthy | 21,444 (44.2) | 19,131 (43.4) | |
| Normal | 10,749 (22.4) | 9742 (22.2) | |
| Unhealthy | 3339 (70.) | 3060 (7.1) | |
| Stress level, n (% *) | <0.001 ‡ | ||
| No stress | 1805 (3.6) | 1597 (3.5) | |
| Little | 7579 (15.4) | 8128 (18.2) | |
| A little | 20,090 (41.6) | 19,907 (45.2) | |
| Severe | 13,605 (28.3) | 11,231 (25.7) | |
| Very severe | 5364 (11.1) | 3353 (7.5) | |
| Asthma, n (% *) | 713 (1.5) | 448 (1.0) | <0.001 ‡ |
| Allergic rhinitis, n (% *) | 9450 (20.1) | 7220 (16.8) | <0.001 ‡ |
| Atopic dermatitis, n (% *) | 3121 (6.4) | 2807 (6.4) | 0.739 |
| Asthma | Event/Total (n, %) | OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | Crude | p-Value | Adjusted † | p-Value | |
| Total participants (n = 92,659) | 713/48,443 (1.5) | 448/44,216 (1.0) | 0.69 (0.61–0.78) | <0.001 * | 0.68 (0.60–0.77) | <0.001 * |
| Sex | ||||||
| Men (n = 48,020) | 413/24,917 (1.7) | 263/23,103 (1.1) | 0.67 (0.57–0.79) | <0.001 * | 0.64 (0.54–0.76) | <0.001 * |
| Women (n = 44,639) | 300/23,526 (1.3) | 185/21,113 (0.9) | 0.70 (0.58–0.85) | <0.001 * | 0.73 (0.60–0.89) | 0.002 * |
| Economic level | ||||||
| High (n = 36,373) | 305/18,992 (1.6) | 186/17,381 (1.1) | 0.63 (0.52–0.76) | <0.001 * | 0.60 (0.50–0.73) | <0.001 * |
| Middle (n = 44,604) | 312/23,376 (1.3) | 203/21,228 (1.0) | 0.74 (0.62–0.89) | 0.001 * | 0.76 (0.63–0.93) | 0.006 * |
| Low (n = 11,682) | 96/6075 (1.6) | 59/5607 (1.1) | 0.70 (0.50–0.98) | 0.036 * | 0.71 (0.50–1.00) | 0.047 * |
| Allergic Rhinitis | Event/Total (n, %) | OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | Crude | p-Value | Adjusted † | p-Value | |
| Total participants (n = 92,659) | 9450/48,443 (19.5) | 7220/44,216 (16.3) | 0.80 (0.77–0.84) | <0.001 * | 0.82 (0.78–0.85) | <0.001 * |
| Sex | ||||||
| Men (n = 48,020) | 4554/24,917 (18.3) | 3611/23,103 (15.6) | 0.84 (0.79–0.89) | <0.001 * | 0.84 (0.79–0.89) | <0.001 * |
| Women (n = 44,639) | 4896/23,526 (20.8) | 3609/21,113 (17.1) | 0.77 (0.73–0.82) | <0.001 * | 0.79 (0.74–0.83) | <0.001 * |
| Economic level | ||||||
| High (n = 36,373) | 3985/18,992 (21.0) | 3038/17,381 (17.5) | 0.80 (0.75–0.84) | <0.001 * | 0.80 (0.76–0.85) | <0.001 * |
| Middle (n = 44,604) | 4280/23,376 (18.3) | 3249/21,228 (15.3) | 0.81 (0.77–0.86) | <0.001 * | 0.82 (0.77–0.87) | <0.001 * |
| Low (n = 11,682) | 1185/6075 (19.5) | 933/5607 (16.6) | 0.80 (0.73–0.89) | <0.001 * | 0.83 (0.75–0.92) | <0.001 * |
| Atopic Dermatitis | Event/Total (n, %) | OR (95% CI) | ||||
|---|---|---|---|---|---|---|
| 2019 | 2020 | Crude | p-Value * | Adjusted † | p-Value * | |
| Total participants (n = 92,659) | 3121/48,443 (6.4) | 2870/44,216 (6.3) | 0.94 (0.94–1.05) | 0.739 | 0.99 (0.94–1.05) | 0.750 |
| Sex | ||||||
| Men (n = 48,020) | 1364/24,917 (5.5) | 1246/23,103 (5.4) | 0.99 (0.92–1.08) | 0.852 | 0.98 (0.90–1.06) | 0.546 |
| Women (n = 44,639) | 1757/23,526 (7.5) | 1561/21,113 (7.4) | 1.00 (0.93–1.07) | 0.924 | 1.00 (0.93–1.08) | 0.939 |
| Economic level | ||||||
| High (n = 36,373) | 1205/18,992 (6.3) | 1099/17,381 (6.3) | 0.99 (0.91–1.07) | 0.776 | 1.00 (0.92–1.08) | 0.966 |
| Middle (n = 44,604) | 1458/23,376 (6.2) | 1293/21,228 (6.1) | 0.98 (0.91–1.06) | 0.648 | 0.98 (0.90–1.06) | 0.976 |
| Low (n = 11,682) | 458/6075 (7.5) | 415/5607 (7.4) | 1.03 (0.89–1.19) | 0.722 | 1.02 (0.88–1.17) | 0.829 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, H.G.; Kong, I.G. Asthma, Allergic Rhinitis, and Atopic Dermatitis Incidence in Korean Adolescents before and after COVID-19. J. Clin. Med. 2021, 10, 3446. https://doi.org/10.3390/jcm10153446
Choi HG, Kong IG. Asthma, Allergic Rhinitis, and Atopic Dermatitis Incidence in Korean Adolescents before and after COVID-19. Journal of Clinical Medicine. 2021; 10(15):3446. https://doi.org/10.3390/jcm10153446
Chicago/Turabian StyleChoi, Hyo Geun, and Il Gyu Kong. 2021. "Asthma, Allergic Rhinitis, and Atopic Dermatitis Incidence in Korean Adolescents before and after COVID-19" Journal of Clinical Medicine 10, no. 15: 3446. https://doi.org/10.3390/jcm10153446
APA StyleChoi, H. G., & Kong, I. G. (2021). Asthma, Allergic Rhinitis, and Atopic Dermatitis Incidence in Korean Adolescents before and after COVID-19. Journal of Clinical Medicine, 10(15), 3446. https://doi.org/10.3390/jcm10153446





