The Reticulocyte Hemoglobin Equivalent as a Screening Marker for Iron Deficiency and Iron Deficiency Anemia in Children
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Classification of Anemia and Iron Deficiency
2.3. Laboratory Parameters
2.4. Primary Endpoint
2.5. Secondary Endpoints
2.6. Statistical Analysis
3. Results
3.1. Patients’ Characteristics
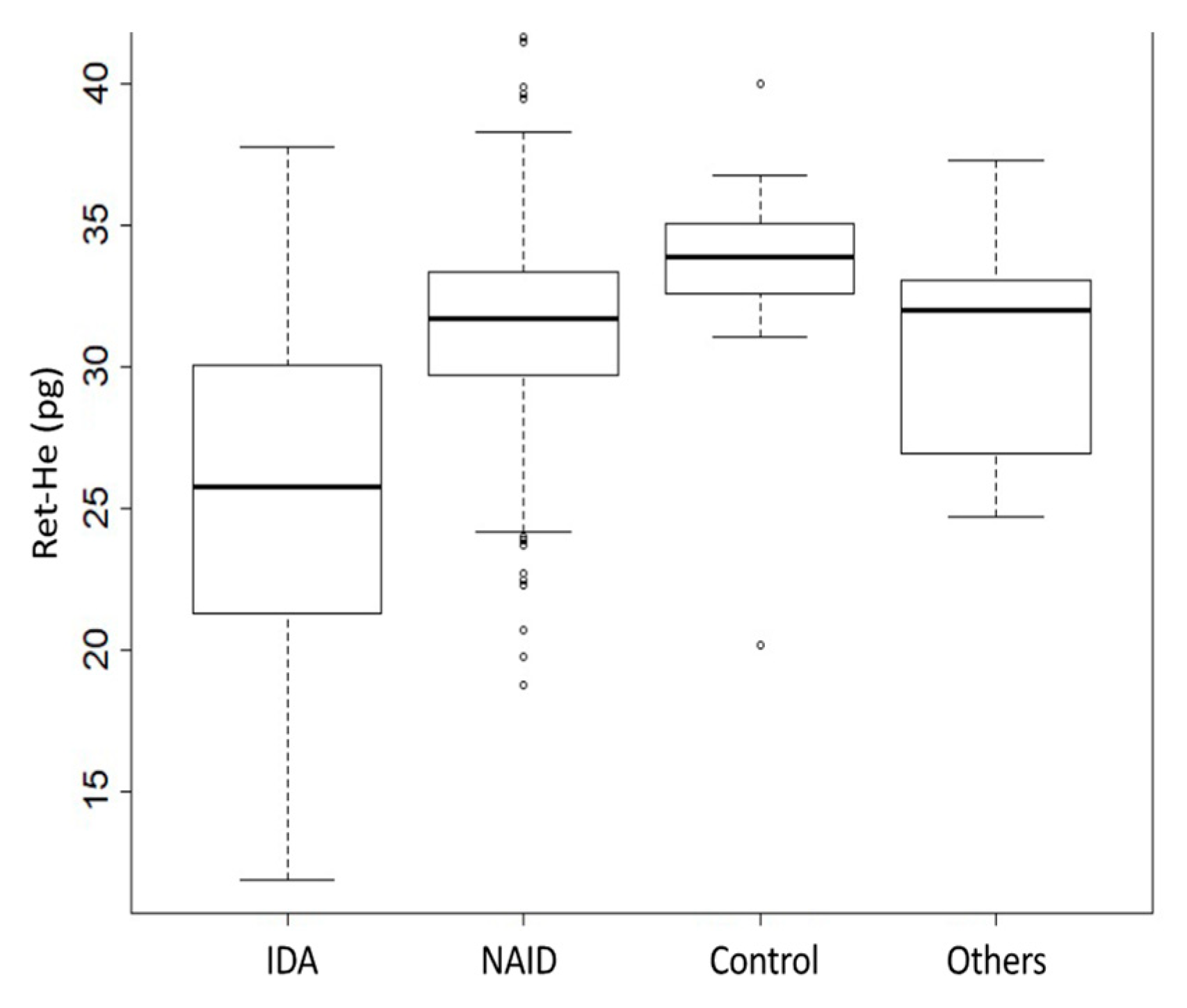
3.2. Comparison of Ret-He Values According to the Iron Status
3.3. Relation of Ret-He with Parameters of Iron Metabolism
3.4. ROC Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McLean, E.; Cogswell, M.; Egli, I.; Wojdyla, D.; De Benoist, B. Worldwide prevalence of anaemia, WHO Vitamin and Mineral Nutrition Information System, 1993–2005. Public Health Nutr. 2009, 12, 444–454. [Google Scholar] [CrossRef] [Green Version]
- Lozoff, B.; Jimenez, E.; Wolf, A.W. Long-Term Developmental Outcome of Infants with Iron Deficiency. N. Engl. J. Med. 1991, 325, 687–694. [Google Scholar] [CrossRef]
- Bruner, A.B.; Joffe, A.; Duggan, A.K.; Casella, J.F.; Brandt, J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet 1996, 348, 992–996. [Google Scholar] [CrossRef]
- World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Meybohm, P.; Richards, T.; Isbister, J.; Hofmann, A.; Shander, A.; Goodnough, L.T.; Muñoz, M.; Gombotz, H.; Weber, C.F.; Choorapoikayil, S.; et al. Patient Blood Management Bundles to Facilitate Implementation. Transfus. Med. Rev. 2017, 31, 62–71. [Google Scholar] [CrossRef] [Green Version]
- Froessler, B.; Palm, P.; Weber, I.; Hodyl, N.A.; Singh, R.; Murphy, E.M. The Important Role for Intravenous Iron in Perioperative Patient Blood Management in Major Abdominal Surgery. Ann. Surg. 2016, 264, 41–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- NICE. Blood Transfusion NICE Guideline. 2015. Available online: https://www.nice.org.uk/guidance/ng24 (accessed on 2 August 2021).
- Brugnara, C.; Schiller, B.; Moran, J. Reticulocyte hemoglobin equivalent (Ret He) and assessment of iron-deficient states. Int. J. Lab. Hematol. 2006, 28, 303–308. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brugnara, C. Use of reticulocyte cellular indices in the diagnosis and treatment of hematological disorders. Int. J. Clin. Lab. Res. 1998, 28, 1–11. [Google Scholar] [CrossRef]
- Buttarello, M.; Temporin, V.; Ceravolo, R.; Farina, G.; Bulian, P. The New Reticulocyte Parameter (RET-Y) of the Sysmex XE 2100: Its Use in the Diagnosis and Monitoring of Posttreatment Sideropenic Anemia. Am. J. Clin. Pathol. 2004, 121, 489–495. [Google Scholar] [CrossRef]
- Chinudomwong, P.; Binyasing, A.; Trongsakul, R.; Paisooksantivatana, K. Diagnostic performance of reticulocyte hemoglobin equivalent in assessing the iron status. J. Clin. Lab. Anal. 2020, 34, e23225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, S.; Schapkaitz, E. The clinical utility of new reticulocyte and erythrocyte parameters on the Sysmex XN 9000 for iron deficiency in pregnant patients. Int. J. Lab. Hematol. 2018, 40, 683–690. [Google Scholar] [CrossRef]
- Buttarello, M.; Pajola, R.; Novello, E.; Mezzapelle, G.; Plebani, M. Evaluation of the hypochromic erythrocyte and reticulocyte hemoglobin content provided by the Sysmex XE-5000 analyzer in diagnosis of iron deficiency erythropoiesis. Clin. Chem. Lab. Med. 2016, 54, 1939–1945. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, A.K.; Bhardwaj, G.; Arora, D.; Aggarwal, G.; Pabbi, S.; Dara, R.C.; Sachdev, R.; Raizada, A.; Sethi, M. Applying newer parameter Ret-He (reticulocyte haemoglobin equivalent) to assess latent iron deficiency (LID) in blood donors–study at a tertiary care hospital in India. Vox Sang. 2018, 113, 639–646. [Google Scholar] [CrossRef]
- Thomas, L.; Franck, S.; Messinger, M.; Linssen, J.; Thomé, M.; Thomas, C. Reticulocyte hemoglobin measurement–Comparison of two methods in the diagnosis of iron-restricted erythropoiesis. Clin. Chem. Lab. Med. 2005, 43, 1193–1202. [Google Scholar] [CrossRef]
- Thomas, C.; Thomas, L. Biochemical Markers and Hematologic Indices in the Diagnosis of Functional Iron Deficiency. Clin. Chem. 2002, 48, 1066–1076. [Google Scholar] [CrossRef] [Green Version]
- Toki, Y.; Ikuta, K.; Kawahara, Y.; Niizeki, N.; Kon, M.; Enomoto, M.; Tada, Y.; Hatayama, M.; Yamamoto, M.; Ito, S.; et al. Reticulocyte hemoglobin equivalent as a potential marker for diagnosis of iron deficiency. Int. J. Hematol. 2017, 106, 116–125. [Google Scholar] [CrossRef] [Green Version]
- Uçar, M.A.; Falay, M.; Dağdas, S.; Ceran, F.; Urlu, S.M.; Özet, G. The importance of RET-He in the diagnosis of iron deficiency and iron deficiency anemia and the evaluation of response to oral iron therapy. J. Med. Biochem. 2019, 38, 496–502. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Amer, A.; Abu-Madi, M.; El Dabbagh, M.; Kamal, M.; Shebl, F.; Al Marzouqi, S.; Al Mulla, S.; Osman, M.; Abdulsalam, W. Early Diagnosis of Iron Deficiency in School Children: A Qatari Experience. J. Hematol. Thromboembolic Dis. 2015, 3, 03. [Google Scholar] [CrossRef] [Green Version]
- Ullrich, C.; Wu, A.; Armsby, C.; Rieber, S.; Wingerter, S.; Brugnara, C.; Shapiro, D.; Bernstein, H.H. Screening Healthy Infants for Iron Deficiency Using Reticulocyte Hemoglobin Content. JAMA 2005, 294, 924–930. [Google Scholar] [CrossRef]
- Davidkova, S.; Prestidge, T.D.; Reed, P.W.; Kara, T.; Wong, W.; Prestidge, C. Comparison of reticulocyte hemoglobin equivalent with traditional markers of iron and erythropoiesis in pediatric dialysis. Pediatr. Nephrol. 2015, 31, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Torsvik, I.K.; Markestad, T.; Ueland, P.M.; Nilsen, R.M.; Midttun, Ø.; Monsen, A.-L.B. Evaluating iron status and the risk of anemia in young infants using erythrocyte parameters. Pediatr. Res. 2012, 73, 214–220. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brugnara, C.; Zurakowski, D.; DiCanzio, J.; Boyd, T.; Platt, O. Reticulocyte Hemoglobin Content to Diagnose Iron Deficiency in Children. JAMA 1999, 281, 2225–2230. [Google Scholar] [CrossRef]
- Muñoz, M.; Acheson, A.G.; Auerbach, M.; Besser, M.; Habler, O.; Kehlet, H.; Liumbruno, G.M.; Lasocki, S.; Meybohm, P.; Baikady, R.R.; et al. International consensus statement on the peri-operative management of anaemia and iron deficiency. Anaesthesia 2016, 72, 233–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Muñoz, M.; Gómez-Ramírez, S.; Besser, M.; Pavía, J.; Gomollón, F.; Liumbruno, G.M.; Bhandari, S.; Cladellas, M.; Shander, A.; Auerbach, M. Current misconceptions in diagnosis and management of iron deficiency. Blood Transfus. Trasfus. Del Sangue 2017, 15, 422–437. [Google Scholar] [CrossRef]
- Anker, S.D.; Comin Colet, J.; Filippatos, G.; Willenheimer, R.; Dickstein, K.; Drexler, H.; Lüscher, T.F.; Bart, B.; Banasiak, W.; Niegowska, J.; et al. Ferric Carboxymaltose in Patients with Heart Failure and Iron Deficiency. N. Engl. J. Med. 2009, 361, 2436–2448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dignass, A.U.; Gasche, C.; Bettenworth, D.; Birgegård, G.; Danese, S.; Gisbert, J.P.; Gomollon, F.; Iqbal, T.; Katsanos, K.; Koutroubakis, I.; et al. European Consensus on the Diagnosis and Management of Iron Deficiency and Anaemia in Inflammatory Bowel Diseases. J. Crohn’s Colitis 2015, 9, 211–222. [Google Scholar] [CrossRef]
- Thomas, D.W.; Hinchliffe, R.F.; Briggs, C.; MacDougall, I.C.; Littlewood, T.; Cavill, I.; British Comm Stand British Committee for Standards in Haematology. Guideline for the laboratory diagnosis of functional iron deficiency. Br. J. Haematol. 2013, 161, 639–648. [Google Scholar] [CrossRef]
- Goodnough, L.; Maniatis, A.; Earnshaw, P.; Benoni, G.; Beris, P.; Bisbe, E.; Fergusson, D.; Gombotz, H.; Habler, O.; Monk, T.; et al. Detection, evaluation, and management of preoperative anaemia in the elective orthopaedic surgical patient: NATA guidelines. Br. J. Anaesth. 2011, 106, 13–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vernet, M. Immunochemical assay of transferrin and iron saturation in serum. Clin. Chem. 1993, 39, 2352–2353. [Google Scholar] [CrossRef]
- Hönemann, C.; Hagemann, O.; Doll, D.; Luedi, M.M.; Ruebsam, M.L.; Meybohm, P. Reticulocyte Haemoglobin as a Routine Parameter in Preoperative Iron Deficiency Assessment. Endocrinol. Metab. 2021, 5, 154. [Google Scholar]
- Guyatt, G.H.; Oxman, A.D.; Ali, M.; Willan, A.; McIlroy, W.; Patterson, C. Laboratory diagnosis of iron-deficiency anemia. J. Gen. Intern. Med. 1992, 7, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Tantawy, A.; Ragab, I.A.; Ismail, E.A.; Ebeid, F.; Al-Bshkar, R.M. Reticulocyte Hemoglobin Content (Ret He): A Simple Tool for Evaluation of Iron Status in Childhood Cancer. J. Pediatr. Hematol. 2020, 42, e147–e151. [Google Scholar] [CrossRef]
- Di Pinto, D.; Paz, M.; Adragna, M.; López, L. Clinical usefulness of the reticulocyte hemoglobin equivalent in children on hemodialysis. Arch. Argent. Pediatr. 2020, 118, 411–417. [Google Scholar] [CrossRef] [PubMed]
- Chuang, C.-L.; Liu, R.-S.; Wei, Y.-H.; Huang, T.-P.; Tarng, D.-C. Early prediction of response to intravenous iron supplementation by reticulocyte haemoglobin content and high-fluorescence reticulocyte count in haemodialysis patients. Nephrol. Dial. Transplant. 2003, 18, 370–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maconi, M.; Cavalca, L.; Danise, P.; Cardarelli, F.; Brini, M. Erythrocyte and reticulocyte indices in iron deficiency in chronic kidney disease: Comparison of two methods. Scand. J. Clin. Lab. Investig. 2009, 69, 365–370. [Google Scholar] [CrossRef] [PubMed]




| All Patients n (%) 970 (100.0) | IDA n (%) 278 (28.7) | NAID n (%) 332 (34.2) | Control n (%) 302 (31.1) | Others n (%) 58 (6.0) | |
|---|---|---|---|---|---|
| Age (years) * # | 11.2 (±4.9) 12.0 (7.0; 15.0) | 11.3 (±5.1) 13.0 (7.3; 16.0) | 10.3 (±4.9) 11.0 (6.0; 15.0) | 11.9 (±4.3) 13.0 (8.3; 16.0) | 11.8 (±5.3) 14.0 (6.5; 16.0) |
| Male n (%) | 506 (52.2) | 147 (52.9) | 180 (54.2) | 151 (50.0) | 28 (48.3) |
| Hb (g/dL) # | 12.3 (11.2; 13.3) | 10.5 (9.6; 11.3) | 12.6 (12.1; 13.5) | 13.3 (12.6; 14.1) | 10.8 (9.4; 11.7) |
| Ret-He (pg) # | 30.8 (27.2; 32.9) | 25.2 (20.5; 29.1) | 30.7 (28.6; 32.5) | 32.8 (31.4; 34.2) | 30.2 (25.8; 33.5) |
| Ferritin (ng/mL) # | 27 (13; 49) | 11.0 (7.0; 23.82) | 27 (16; 42) | 42.5 (27.0; 65.8) | 75.0 (23.0; 198.0) |
| TSAT (%) # | 14.4 (77.7; 22.5) | 6.0 (4.1; 9.9) | 12.8 (9.0; 16.2) | 26.1 (22.3; 33.0) | 21.8 (20.9; 28.3) |
| Serum Iron (µg/dL) # | 58 (31; 91) | 27.0 (18.0; 40.0) | 53.0 (38.0; 67.0) | 103.0 (88.0; 123.8) | 89.5 (45.0; 111.8) |
| Transferrin (mg/dL) # | 292 (259; 324.8) | 315.5 (288; 355.8) | 295 (268.8; 324.0) | 272.0 (250.0; 305.0) | 240.5 (191.8; 279.0) |
| sTfR (mg/L) # | 4.0 (3.1; 5.6) | 6.5 (4.7; 10.2) | 4.2 (3.4; 5.0) | 3.1 (2.6; 3.6) | 4.0 (3.0; 5.8) |
| MCH (pg) # | 26.8 (24.3; 28.4) | 22.9 (20.4; 25.4) | 27.0 (25.4; 28.3) | 28.4 (27.2; 29.5) | 25.3 (23.1; 27.6) |
| MCV (fl) # | 78.2 (73.1; 82.2) | 72.1 (66.2; 77.4) | 78.3 (74.8; 81.9) | 81.6 (78.4; 84.8) | 76.2 (71.9; 80.4) |
| RCDW (%) # | 13.5 (12.5; 15.4) | 16.1 (14.6; 18.8) | 13.2 (12.5; 14.1) | 12.5 (12.1; 13.2) | 15.5 (13.6; 18.4) |
| Patients | n | Cut-Off-Value | AUC | Sensitivity | Specificity | Reference |
|---|---|---|---|---|---|---|
| Children on chronic dialysis | 45 | 28.9 pg | 0.870 | 90% | 75% | Davidkova et al. [21] |
| Healthy 9–12 months old infants | 202 | 27.5 pg | 0.850 | 83% | 72% | Ullrich C et al. [20] |
| General pediatric outpatient | 210 | 26.0 pg | * | 70% | 78% | Brugnara et al. [23] |
| Children on hemodialysis | 40 | 29.0 pg | * | 90% | 75% | Di Pinto et al. [34] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neef, V.; Schmitt, E.; Bader, P.; Zierfuß, F.; Hintereder, G.; Steinbicker, A.U.; Zacharowski, K.; Piekarski, F. The Reticulocyte Hemoglobin Equivalent as a Screening Marker for Iron Deficiency and Iron Deficiency Anemia in Children. J. Clin. Med. 2021, 10, 3506. https://doi.org/10.3390/jcm10163506
Neef V, Schmitt E, Bader P, Zierfuß F, Hintereder G, Steinbicker AU, Zacharowski K, Piekarski F. The Reticulocyte Hemoglobin Equivalent as a Screening Marker for Iron Deficiency and Iron Deficiency Anemia in Children. Journal of Clinical Medicine. 2021; 10(16):3506. https://doi.org/10.3390/jcm10163506
Chicago/Turabian StyleNeef, Vanessa, Elke Schmitt, Peter Bader, Frank Zierfuß, Gudrun Hintereder, Andrea U. Steinbicker, Kai Zacharowski, and Florian Piekarski. 2021. "The Reticulocyte Hemoglobin Equivalent as a Screening Marker for Iron Deficiency and Iron Deficiency Anemia in Children" Journal of Clinical Medicine 10, no. 16: 3506. https://doi.org/10.3390/jcm10163506
APA StyleNeef, V., Schmitt, E., Bader, P., Zierfuß, F., Hintereder, G., Steinbicker, A. U., Zacharowski, K., & Piekarski, F. (2021). The Reticulocyte Hemoglobin Equivalent as a Screening Marker for Iron Deficiency and Iron Deficiency Anemia in Children. Journal of Clinical Medicine, 10(16), 3506. https://doi.org/10.3390/jcm10163506







