Poor Correction Capacity of Preexisting Ankle Valgus Deformity after Total Knee Arthroplasty
Abstract
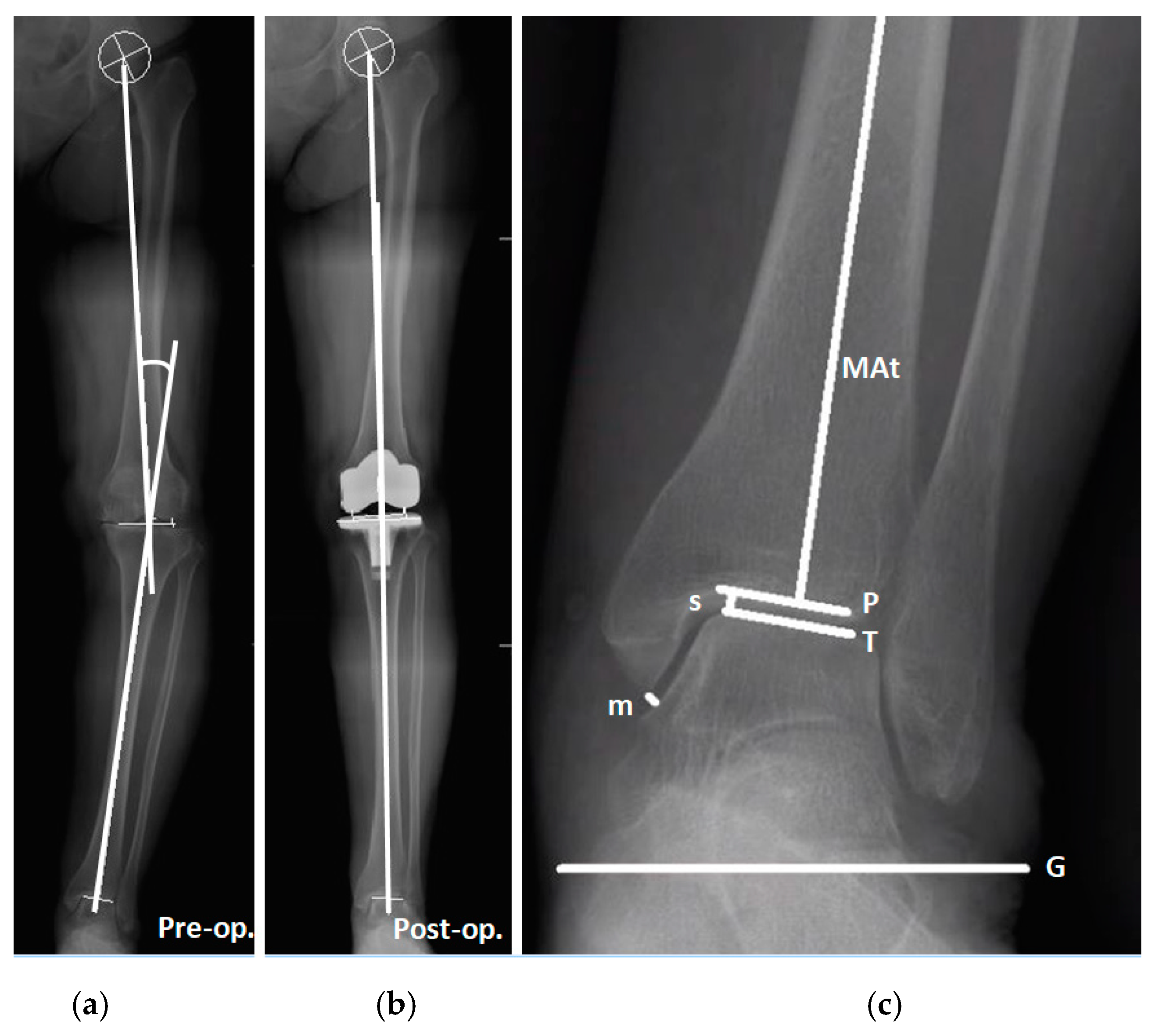
:1. Introduction
2. Materials and Methods
2.1. Patient Enrollment
2.2. Study Grouping and Parameters of Knee and Ankle
2.3. Radiographic Measurements
2.4. Statistical Analysis
3. Results
3.1. Radiographic Parameters of the Knee and Ankle Joint Change after Total Knee Arthroplasty in Patients with Different Preexisting Ankle Deformity
3.2. Correlation between Ankle Parameter Changes and HKA Changes in Patients with Different Preexisting Ankle Deformity
3.3. Correlation between Ankle Parameter Changes and Preoperative HKA in Patients with Different Preexisting Ankle Deformity
3.4. Between Group Comparison of Radiographic Parameters in Patients with Different Preexisting Ankle Deformity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, J.G.; Wixson, R.L.; Tsai, D.; Stulberg, S.D.; Chang, R.W. Functional outcome and patient satisfaction in total knee patients over the age of 75. J. Arthroplast. 1996, 11, 831–840. [Google Scholar] [CrossRef]
- Hawker, G.; Wright, J.; Coyte, P.; Paul, J.; Dittus, R.; Croxford, R.; Katz, B.; Bombardier, C.; Heck, D.; Freund, D. Health-related quality of life after knee replacement. Results of the knee replacement patient outcomes research team study. J. Bone Jt. Surg. Am. 1998, 80, 163–173. [Google Scholar] [CrossRef]
- Lee, J.H.; Jeong, B.O. Radiologic changes of ankle joint after total knee arthroplasty. Foot Ankle Int. 2012, 33, 1087–1092. [Google Scholar] [CrossRef]
- Tallroth, K.; Harilainen, A.; Kerttula, L.; Sayed, R. Ankle osteoarthritis is associated with knee osteoarthritis. Conclusions based on mechanical axis radiographs. Arch Orthop. Trauma Surg. 2008, 128, 555–560. [Google Scholar] [CrossRef]
- Chang, C.B.; Jeong, J.H.; Chang, M.J.; Yoon, C.; Song, M.K.; Kang, S.-B. Concomitant ankle osteoarthritis is related to increased ankle pain and a worse clinical outcome following total knee arthroplasty. J. Bone Jt. Surg. Am. 2018, 100, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Xie, K.; Jiang, X.; Han, X.; Ai, S.; Qu, X.; Yan, M. Association between knee malalignment and ankle degeneration in patients with end-stage knee osteoarthritis. J. Arthroplast. 2018, 33, 3694–3698.e1. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-W.; Gwak, H.-C.; Kim, J.-H.; Lee, C.-R.; Kim, J.-G.; Oh, M.; Park, J.-H. Radiologic factors affecting ankle pain before and after total knee arthroplasty for the varus osteoarthritic knee. J. Foot Ankle Surg. 2018, 57, 865–869. [Google Scholar] [CrossRef]
- Gursu, S.; Sofu, H.; Verdonk, P.; Sahin, V. Effects of total knee arthroplasty on ankle alignment in patients with varusgonarthrosis: Do we sacrifice ankle to the knee? Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2470–2475. [Google Scholar] [CrossRef]
- Gao, F.; Ma, J.; Sun, W.; Guo, W.; Li, Z.; Wang, W. Radiographic assessment of knee–ankle alignment after total knee arthroplasty for varus and valgus knee osteoarthritis. Knee 2017, 24, 107–115. [Google Scholar] [CrossRef]
- Kim, J.G.; Suh, D.H.; Choi, G.W.; Koo, B.M.; Kim, S.-G. Change in the weight-bearing line ratio of the ankle joint and ankle joint line orientation after knee arthroplasty and high tibial osteotomy in patients with genu varum deformity. Int. Orthop. 2021, 45, 117–124. [Google Scholar] [CrossRef]
- Jeong, B.O.; Kim, T.Y.; Baek, J.H.; Jung, H.; Song, S.H. Following the correction of varus deformity of the knee through total knee arthroplasty, significant compensatory changes occur not only at the ankle and subtalar joint, but also at the foot. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3230–3237. [Google Scholar] [CrossRef]
- Tonogai, I.; Hamada, D.; Sairyo, K. Radiographic changes in coronal alignment of the ankle joint immediately after primary total knee arthroplasty for varus knee osteoarthritis. Foot Ankle Online J. 2017, 10, 2. [Google Scholar] [CrossRef]
- Burssens, A.B.; Buedts, K.; Barg, A.; Vluggen, E.; Demey, P.; Saltzman, C.L.; Victor, J.M. Is lower-limb alignment associated with hindfoot deformity in the coronal plane? A weightbearing CT analysis. Clin. Orthop. Relat. Res. 2020, 478, 154–168. [Google Scholar] [CrossRef] [Green Version]
- Norton, A.A.; Callaghan, J.J.; Amendola, A.; Phisitkul, P.; Wongsak, S.; Liu, S.S.; Fruehling-Wall, C. Correlation of knee and hindfoot deformities in advanced knee OA: Compensatory hindfoot alignment and where it occurs. Clin. Orthop. Relat. Res. 2015, 473, 166–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, B.; Saltzman, C.L.; Chalayon, O.; Barg, A. Does the subtalar joint compensate for ankle malalignment in end-stage ankle arthritis? Clin. Orthop. Relat. Res. 2015, 473, 318–325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshimoto, K.; Noguchi, M.; Yamada, A.; Nasu, Y. Compensatory Function of the Subtalar Joint for Lower Extremity Malalignment. Adv. Orthop. 2019, 2019, 7656878. [Google Scholar] [CrossRef] [PubMed]
- Krähenbühl, N.; Siegler, L.; Deforth, M.; Zwicky, L.; Hintermann, B.; Knupp, M. Subtalar joint alignment in ankle osteoarthritis. Foot Ankle Surg. 2019, 25, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Colin, F.; Horn Lang, T.; Zwicky, L.; Hintermann, B.; Knupp, M. Subtalar joint configuration on weightbearing CT scan. Foot Ankle Int. 2014, 35, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Cooke, T.D.V.; Sled, E.A.; Scudamore, R.A. Frontal plane knee alignment: A call for standardized measurement. J. Rheumatol. 2007, 34, 1796–1801. [Google Scholar]
- Paley, D.; Tetsworth, K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin. Orthop. Relat. Res. 1992, 280, 48–64. [Google Scholar]
- Cox, J.; Hewes, T.F. “Normal” talar tilt angle. Clin. Orthop. Relat. Res. 1979, 140, 37–41. [Google Scholar] [CrossRef]
- Saltzman, C.L.; Salamon, M.L.; Blanchard, G.M.; Huff, T.; Hayes, A.; Buckwalter, J.A.; Amendola, A. Epidemiology of ankle arthritis: Report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop. J. 2005, 25, 44–46. [Google Scholar]
- Valderrabano, V.; Horisberger, M.; Russell, I.; Dougall, H.; Hintermann, B. Etiology of ankle osteoarthritis. Clin. Orthop. Relat. Res. 2009, 467, 1800–1806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gao, F.; Ma, J.; Sun, W.; Guo, W.; Li, Z.; Wang, W. The influence of knee malalignment on the ankle alignment in varus and valgus gonarthrosis based on radiographic measurement. Eur. J. Radiol. 2016, 85, 228–232. [Google Scholar] [CrossRef] [PubMed]
- Hashimoto, T.; Inokuchi, S. A kinematic study of ankle joint instability due to rupture of the lateral ligaments. Foot Ankle Int. 1997, 18, 729–734. [Google Scholar] [CrossRef]
- Tarr, R.R.; Resnick, C.T.; Wagner, K.S.; Sarmiento, A. Changes in tibiotalar joint contact areas following experimentally induced tibial angular deformities. Clin. Orthop. Relat. Res. 1985, 199, 72–80. [Google Scholar] [CrossRef]
- Usuelli, F.G.; Di Silvestri, C.A.; D’Ambrosi, R.; Orenti, A.; Randelli, F. Total ankle replacement: Is pre-operative varus deformity a predictor of poor survival rate and clinical and radiological outcomes? Int. Orthop. 2019, 43, 243–249. [Google Scholar] [CrossRef]
- Nakada, I.; Nakamura, I.; Juji, T.; Ito, K.; Matsumoto, T. Correlation between knee and hindfoot alignment in patients with rheumatoid arthritis: The effects of subtalar joint destruction. Mod. Rheumatol. 2015, 25, 689–693. [Google Scholar] [CrossRef]
- Chandler, J.T.; Moskal, J.T. Evaluation of knee and hindfoot alignment before and after total knee arthroplasty: A prospective analysis. J. Arthroplast. 2004, 19, 211–216. [Google Scholar] [CrossRef]
- Milgrom, C.; Giladi, M.; Simkin, A.; Stein, M.; Kashtan, H.; Margulies, J.; Steinberg, R.; Aharonson, Z. The normal range of subtalar inversion and eversion in young males as measured by three different techniques. Foot Ankle 1985, 6, 143–145. [Google Scholar] [CrossRef]
- Bestwick-Stevenson, T.; Ifesemen, O.S.; Pearson, R.G.; Edwards, K.L. Association of Sports Participation with Osteoarthritis: A Systematic Review and Meta-Analysis. Orthop. J. Sports Med. 2021, 9, 23259671211004554. [Google Scholar] [CrossRef] [PubMed]
- Armenis, E.; Pefanis, N.; Tsiganos, G.; Karagounis, P.; Baltopoulos, P. Osteoarthritis of the ankle and foot complex in former Greek soccer players. Foot Ankle Spec. 2011, 4, 338–343. [Google Scholar] [CrossRef] [PubMed]


| Total | Valgus Group (Preoperative PTA < 0°) | Varus Group (Preoperative PTA ≥ 0°) | p-Value a | |
|---|---|---|---|---|
| Number (%) | 90 | 14 (15.6) | 76 (84.4) | |
| Age (years) | 72.0 [66.0, 79.0] | 72.0 [68.8, 77.0] | 72.0 [65.0, 79.0] | 0.462 |
| Sex Male (%) Female (%) | 28 (31.1) 62 (68.9) | 5 (35.7) 9 (64.3) | 23 (30.3) 53 (69.7) | 0.756 |
| BMI (kg/m2) | 27.7 [25.8, 30.9] | 27.3 [24.5, 32.6] | 27.7 [26.0, 30.8] | 0.609 |
| Side Right (%) Left (%) | 44 (48.9) 46 (51.1) | 6 (42.9) 8 (57.1) | 38 (50.0) 38 (50.0) | 0.623 |
| Preoperative parameters | ||||
| HKA (°) | 10.4 [6.4, 14.2] | 10.5 [3.6, 12.3] | 10.4 [6.9, 14.3] | 0.379 |
| LDTA (°) | 88.1 [84.8, 89.9] | 88.9 [86.0, 92.5] | 88.0 [84.6, 89.5] | 0.130 |
| PGA (°) | −5.4 [−8.8, −1.5] | −6.6 [−8.8, −2.3] | −5.4 [−9.1, −1.2] | 0.494 |
| TGA (°) | −6.7 [−10.3, −3.0] | −5.2 [−7.0, −1.8] | −6.8 [−10.9, −3.1] | 0.208 |
| PTA (°) | 0.9 [0.3, 2.3] | −1.3 [−1.7, −0.6] | 1.2 [0.5, 2.5] | <0.001 |
| Medial space (mm) | 2.3 [1.8, 2.9] | 2.3 [1.8, 2.8] | 2.3 [1.8, 2.9] | 0.978 |
| Superior space (mm) | 2.5 [2.2, 3.0] | 3.0 [2.4, 3.3] | 2.5 [2.2, 2.8] | 0.021 |
| Radiographic Parameters | Preoperative | Postoperative | p-Value a | |
|---|---|---|---|---|
| Valgus group | HKA (°) | 10.5 [3.6, 12.3] | 2.7 [0.5, 5.0] | 0.001 |
| PGA (°) | −6.6 [−8.8, −2.3] | −1.6 [−3.9, 1.8] | 0.017 | |
| TGA (°) | −5.2 [−7.0, −1.8] | −0.1 [−3.1, 2.6] | 0.008 | |
| PTA (°) | −1.3 [−1.7, −0.6] | −0.9 [−1.4, 0.0] | 0.197 | |
| Medial space (mm) | 2.3 [1.8, 2.8] | 2.3 [1.7, 3.7] | 0.937 | |
| Superior space (mm) | 3.0 [2.4, 3.3] | 2.8 [2.4, 3.3] | 0.537 | |
| Varus group | HKA (°) | 10.4 [6.9, 14.3] | 2.3 [0.9, 4.8] | <0.001 |
| PGA (°) | −5.4 [−9.1, −1.2] | −1.1 [−4.5, 3.2] | <0.001 | |
| TGA (°) | −6.8 [−10.9, −3.1] | −1.7 [−5.5, 2.6] | <0.001 | |
| PTA (°) | 1.2 [0.5, 2.5] | 0.3 [−0.2, 1.6] | <0.001 | |
| Medial space (mm) | 2.3 [1.8, 2.9] | 2.5 [1.7, 3.1] | 0.154 | |
| Superior space (mm) | 2.5 [2.2, 2.8] | 2.6 [2.3, 2.9] | 0.013 |
| Ankle Parameters | Correlation between Ankle Parameter Changes and ∆HKA | Correlation between Ankle Parameter Changes and Preoperative HKA | |||
|---|---|---|---|---|---|
| r a | p a | r a | p a | ||
| Valgus group | ∆PGA (°) | −0.499 | 0.069 | 0.484 | 0.079 |
| ∆TGA (°) | −0.526 | 0.053 | 0.543 | 0.045 | |
| ∆PTA (°) | −0.077 | 0.793 | 0.029 | 0.923 | |
| ∆Medial space (mm) | −0.115 | 0.695 | 0.341 | 0.233 | |
| ∆Superior space (mm) | 0.156 | 0.593 | −0.208 | 0.475 | |
| Varus group | ∆PGA (°) | −0.519 | <0.001 | 0.363 | 0.001 |
| ∆TGA (°) | −0.615 | <0.001 | 0.463 | <0.001 | |
| ∆PTA (°) | 0.247 | 0.032 | −0.235 | 0.041 | |
| ∆Medial space (mm) | −0.116 | 0.32 | 0.073 | 0.531 | |
| ∆Superior space (mm) | −0.036 | 0.759 | 0.001 | 0.993 | |
| Ankle Parameters | Valgus Group | Varus Group | p-Value a | |
|---|---|---|---|---|
| Postoperative | HKA (°) | 2.7 [0.5, 5.0] | 2.3 [0.9, 4.8] | 0.824 |
| PGA (°) | −1.6 [−3.9, 1.8] | −1.1 [−4.5, 3.2] | 0.676 | |
| TGA (°) | −0.1 [−3.1, 2.6] | −1.7 [−5.5, 2.6] | 0.439 | |
| PTA (°) | −0.9 [−1.4, 0.0] | 0.3 [−0.2, 1.6] | <0.001 | |
| Medial space (mm) | 2.3 [1.7, 3.7] | 2.5 [1.7, 3.1] | 0.929 | |
| Superior space (mm) | 2.8 [2.4, 3.3] | 2.6 [2.3, 2.9] | 0.145 | |
| Preoperative and Postoperative Differences | ∆HKA (°) | −6.4 [−11.0, −3.8] | −8.1 [−12.2, −4.8] | 0.293 |
| ∆PGA (°) | 4.5 [2.0, 9.1] | 4.9 [1.1, 7.4] | 0.566 | |
| ∆TGA (°) | 3.3 [2.2, 9.1] | 5.4 [1.6, 8.0] | 0.859 | |
| ∆PTA (°) | 0.4 [−0.5, 1.4] | −0.7 [−1.6, −0.2] | <0.001 | |
| ∆Medial space (mm) | −0.1 [−0.2, 0.5] | 0.0 [−0.3, 0.5] | 0.499 | |
| ∆Superior space (mm) | 0.0 [−0.2, 0.1] | 0.1 [−0.1, 0.4] | 0.100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shih, H.-T.; Liao, W.-J.; Tu, K.-C.; Lee, C.-H.; Tang, S.-C.; Wang, S.-P. Poor Correction Capacity of Preexisting Ankle Valgus Deformity after Total Knee Arthroplasty. J. Clin. Med. 2021, 10, 3624. https://doi.org/10.3390/jcm10163624
Shih H-T, Liao W-J, Tu K-C, Lee C-H, Tang S-C, Wang S-P. Poor Correction Capacity of Preexisting Ankle Valgus Deformity after Total Knee Arthroplasty. Journal of Clinical Medicine. 2021; 10(16):3624. https://doi.org/10.3390/jcm10163624
Chicago/Turabian StyleShih, Han-Ting, Wei-Jen Liao, Kao-Chang Tu, Cheng-Hung Lee, Shih-Chieh Tang, and Shun-Ping Wang. 2021. "Poor Correction Capacity of Preexisting Ankle Valgus Deformity after Total Knee Arthroplasty" Journal of Clinical Medicine 10, no. 16: 3624. https://doi.org/10.3390/jcm10163624
APA StyleShih, H.-T., Liao, W.-J., Tu, K.-C., Lee, C.-H., Tang, S.-C., & Wang, S.-P. (2021). Poor Correction Capacity of Preexisting Ankle Valgus Deformity after Total Knee Arthroplasty. Journal of Clinical Medicine, 10(16), 3624. https://doi.org/10.3390/jcm10163624







