Diabetes Mellitus and Heart Failure
Abstract
:1. Introduction
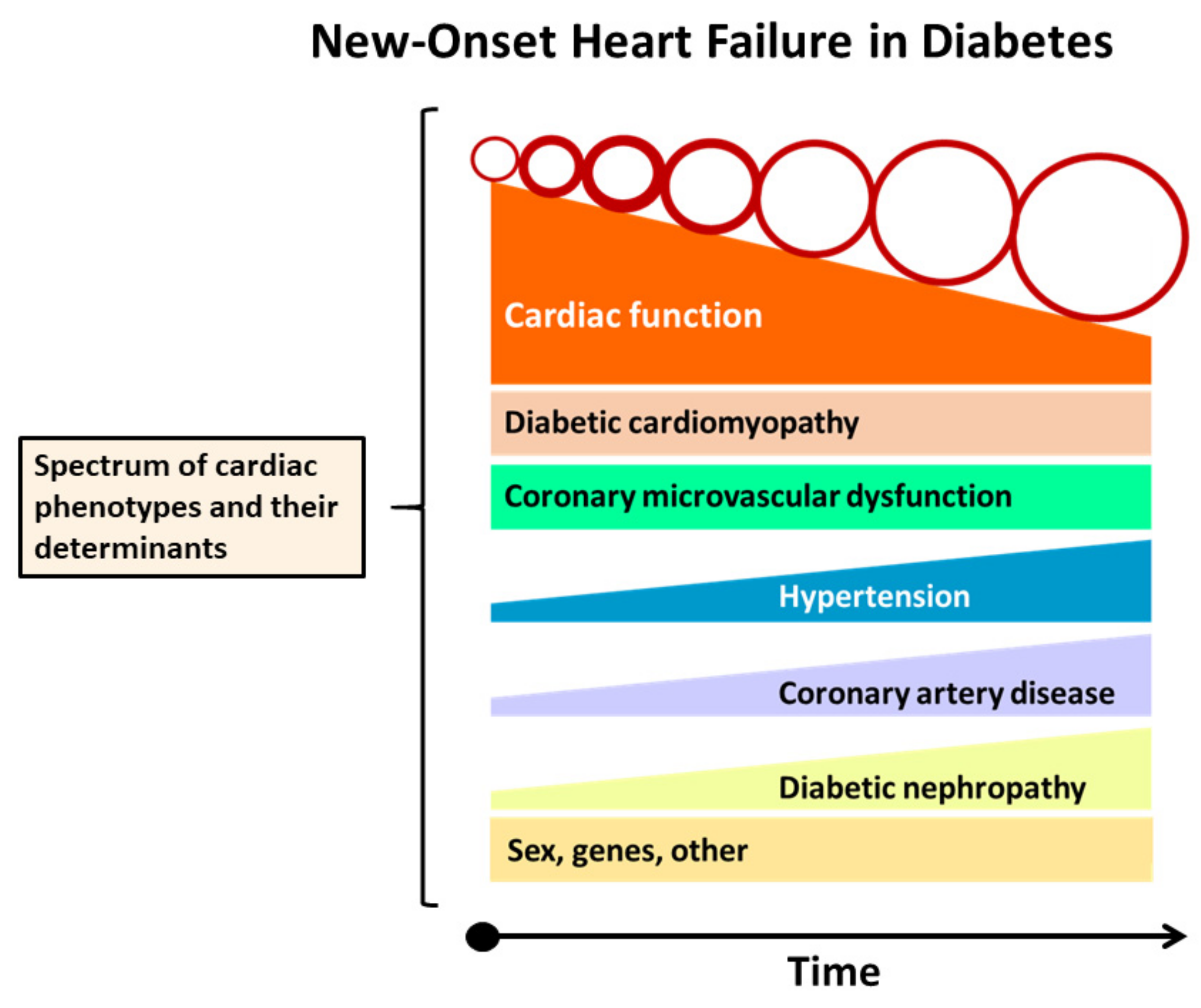
1.1. New-Onset Heart Failure in Diabetes
1.1.1. Epidemiology
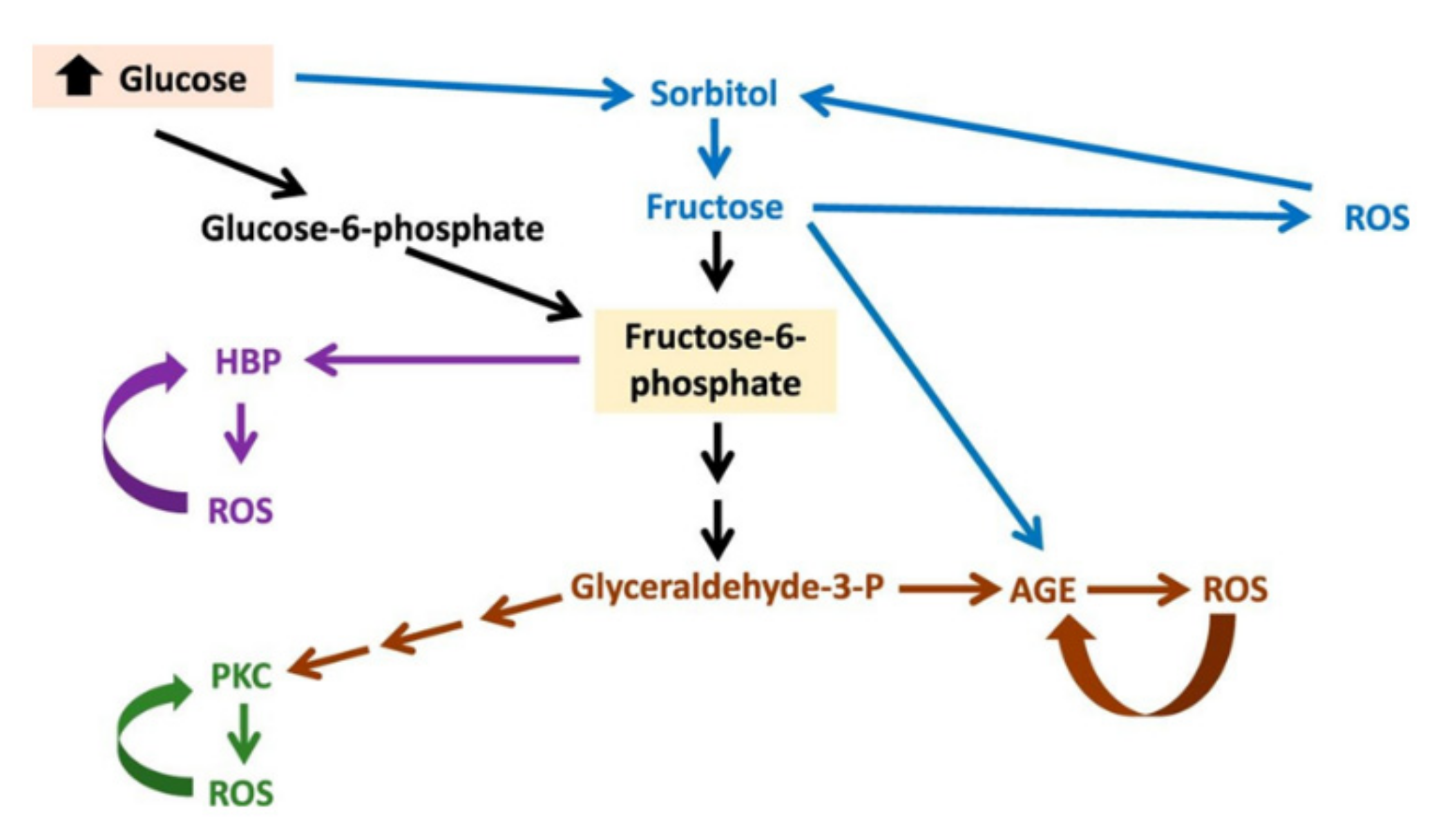
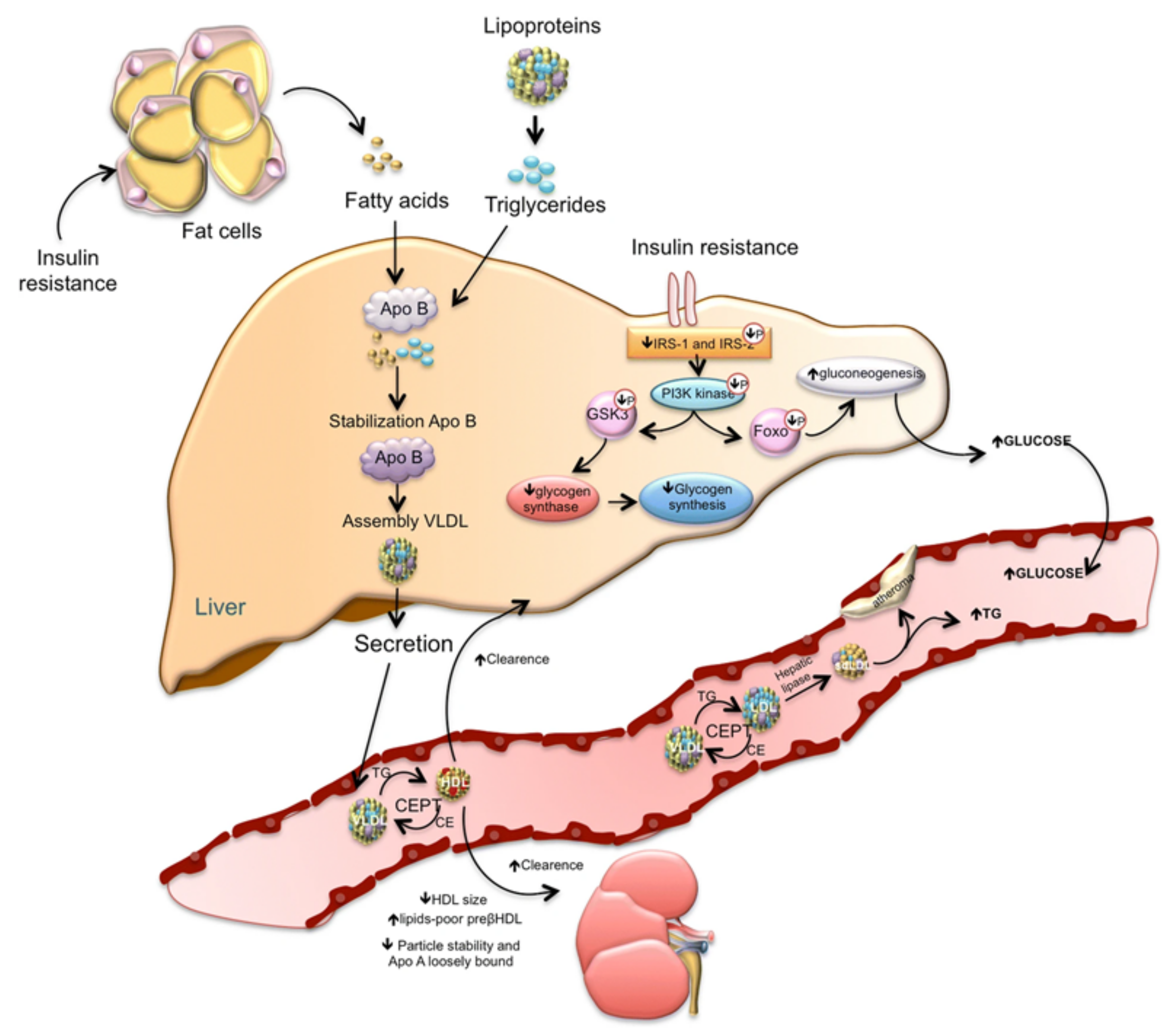
1.1.2. Pathogenesis
- Immune dysregulation. T1DM results from the body’s immune system, which targets insulin-producing β-cells within the pancreatic islets. Patients with T1DM are also at increased risk of developing other autoimmune disorders, including cardiac autoimmunity [12]. Immune-mediated destruction of β-cells in pancreatic islets results in diminished or absent release of insulin and consequent hyperglycemia. Both in patients with T1DM and those with T2DM, chronic hyperglycemia causes subclinical myocardial injury, leading to leakage and exposure of heart muscle proteins, including α-myosin, to the immune system. However, in T1DM patients with poor glycemic control, the dysregulated adaptive immune system is overreactive to myocardial injury, leading to a build-up of proinflammatory CD4+ T cells specific to α-myosin and the development of autoantibodies to MYH6 and other cardiac antigens (Figure 2) [13]. This proinflammatory state leads to myocarditis resembling that seen in Chagas disease, and potentially a more generalized state of low-grade vascular inflammation, facilitating the development of atherosclerotic lesions and HF [14].
- Obesity. Obesity is a major risk factor for the development of T2DM, HTN, CAD, and HF. Obesity alters the function of natriuretic peptides (NPs), which act as a defense mechanism against ventricular stress and the deleterious effects of cardiac volume and pressure overload. NPs act on the kidney promoting diuresis and natriuresis, inducing vasodilation, and protecting the heart from high preload and afterload, which can cause hypertrophy and fibrosis through activation of antifibrotic and antihypertrophic pathways [15]. In addition, NPs reduce the sympathetic tone and suppress renin and aldosterone secretion. Less recognized is the fact that NPs, by promoting adipocyte browning, lipolysis, lipid oxidation, and modulation of adipokine secretion, have emerged as key regulators of energy consumption and metabolism. NPR (NP receptor)-A signaling in skeletal muscles and adipocytes seems to be pivotal to the maintenance of long-term insulin sensitivity, which is disturbed in obesity and decreased glucose-tolerance states [16].
- 3.
- Diabetic cardiomyopathy. There are several definitions of diabetic cardiomyopathy. The 2013 European Society of Cardiology (ESC) Guidelines on diabetes, pre-diabetes, and CV diseases, developed in collaboration with the European Association for the Study of Diabetes (EASD), define diabetic cardiomyopathy as “a clinical condition diagnosed when ventricular dysfunction occurs in the setting of diabetes and in the absence of coronary atherosclerosis and hypertension” [26]. This definition was adopted by the 2018 position statement from the Heart Failure Association of the ESC [27].
1.2. Pathogenesis
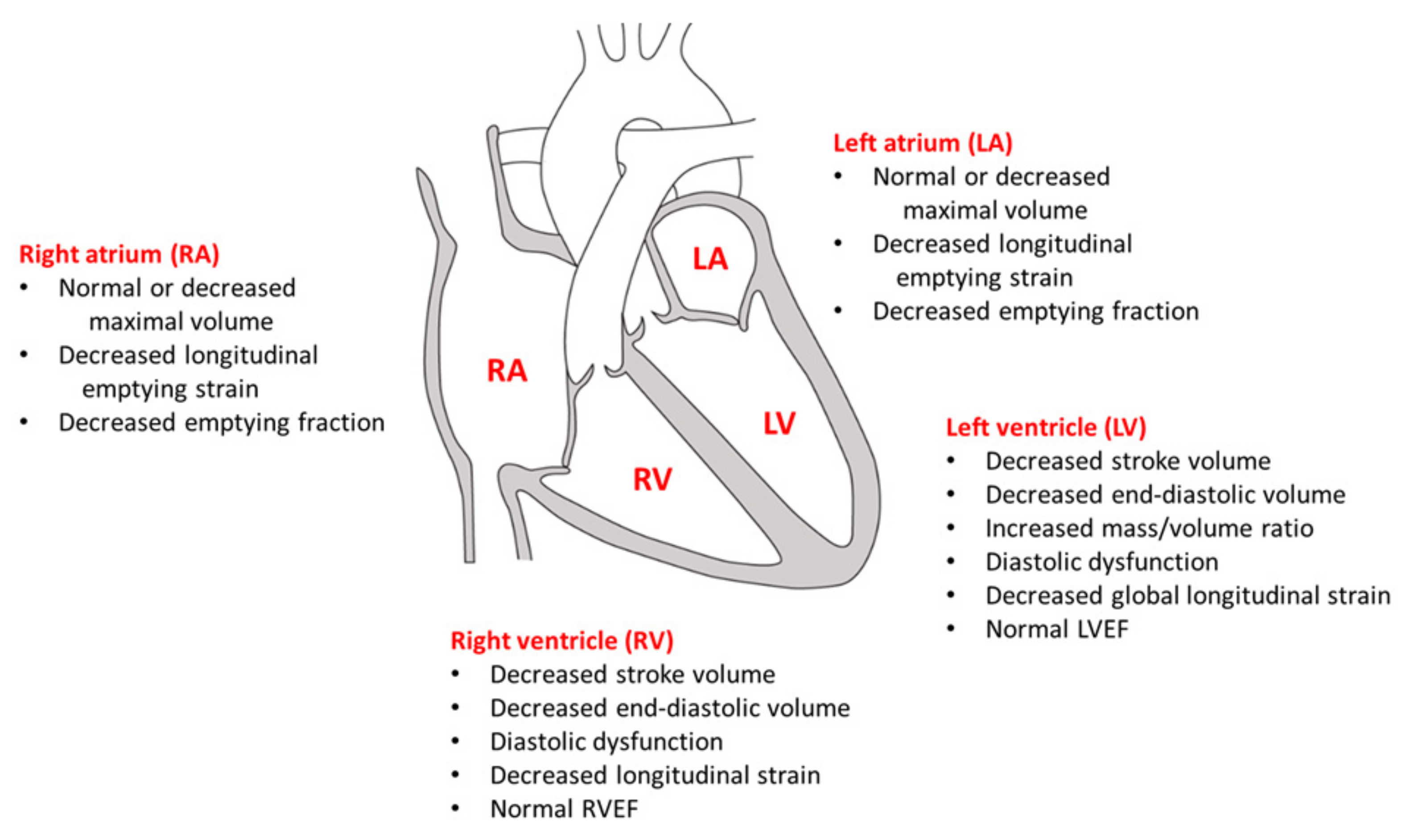
1.3. Cardiac Structural and Functional Abnormalities
- 4.
- Hypertension. HTN is present in many patients with DM. A recent analysis of US national surveys demonstrated that the prevalence of HTN in adults with DM was 76.3% or 66.0% according to the definitions of guidelines from the American College of Cardiology (ACC)/American Heart Association (AHA) and the American Diabetes Association (ADA), respectively [51]. An observational study, which included a cohort of teenagers and young adults who had been diagnosed with DM as a child or adolescent (n = 2018, follow-up period = 7.9 years), reported that patients with T2DM had a higher prevalence of HTN and increased arterial stiffness than those with T1DM [52]. Nevertheless, it is estimated that HTN affects around a third of patients with T1DM and that blood pressure control rates are disappointingly low [53]. Various common pathophysiological mechanisms contribute to the coexistence of HTN and DM, including, but not limited to IR, hyperinsulinemia, abnormal renal sodium handling, overactivation of RAAS, dysautonomia, inflammation, oxidative stress, and endothelial cell dysfunction [53,54].
- 5.
- Coronary artery disease. DM is a risk factor for CAD, independent of other major risk factors such as HTN, hyperlipidemia, and tobacco smoking. Baseline DM is associated with 2- to 3-fold increased rates of incident CAD, myocardial infarction (MI), and fatal CAD [55,56]. The Finnish study found that the seven-year incidence of MI in diabetic subjects with no history of prior MI was the same as that in nondiabetic subjects with a history of prior MI, giving rise to the concept of DM as a cardiovascular risk equivalent [57]. It is noteworthy that investigation of the relationship between T2DM and CAD has identified shared genes between T2DM and CAD with noticeable examples being the 9p21 locus, the IRS1 locus, and the LPL and ANGPTL4 genes, which are involved in triglyceride metabolism [58].
- 6.
- Coronary microvascular dysfunction. The coronary microcirculation is a firmly regulated network with several associated physiological processes acting to match myocardial perfusion to metabolic demands [63]. Derangement of this mechanism, defined as CMD, is present in many DM patients and carries an increased risk of adverse CV clinical outcomes [64].
- 7.
- Diabetic nephropathy. Diabetic nephropathy is the most frequent cause of chronic kidney disease (CKD), representing a large and dire public health problem [68]. Diabetic nephropathy develops in the setting of a systemic, chronic proinflammatory state that contributes to vascular and myocardial remodeling, resulting in atherosclerotic lesions, vascular calcification, and vascular senescence as well as myocardial fibrosis and calcification of cardiac valves which mimic accelerated aging of the CV system [69,70]. Some studies suggest that the excess CV risk both in T1DM and T2DM is confined in patients with diabetic nephropathy [71,72]. Intensive glucose regulation decreases the risk of diabetic nephropathy and also suppresses the renin–angiotensin system (RAS) and is a significant treatment target both for the prevention and management of diabetic nephropathy [73]. However, hyperglycemia is often difficult to control in the CKD population, as several antihyperglycemic agents are contraindicated in CKD patients, and the pharmacokinetics of others, including insulin, change with declining glomerular filtration rate [74,75].
1.3.1. Stages of Heart Failure Development in Diabetes
1.3.2. Prevention of New-Onset Heart Failure in Diabetes
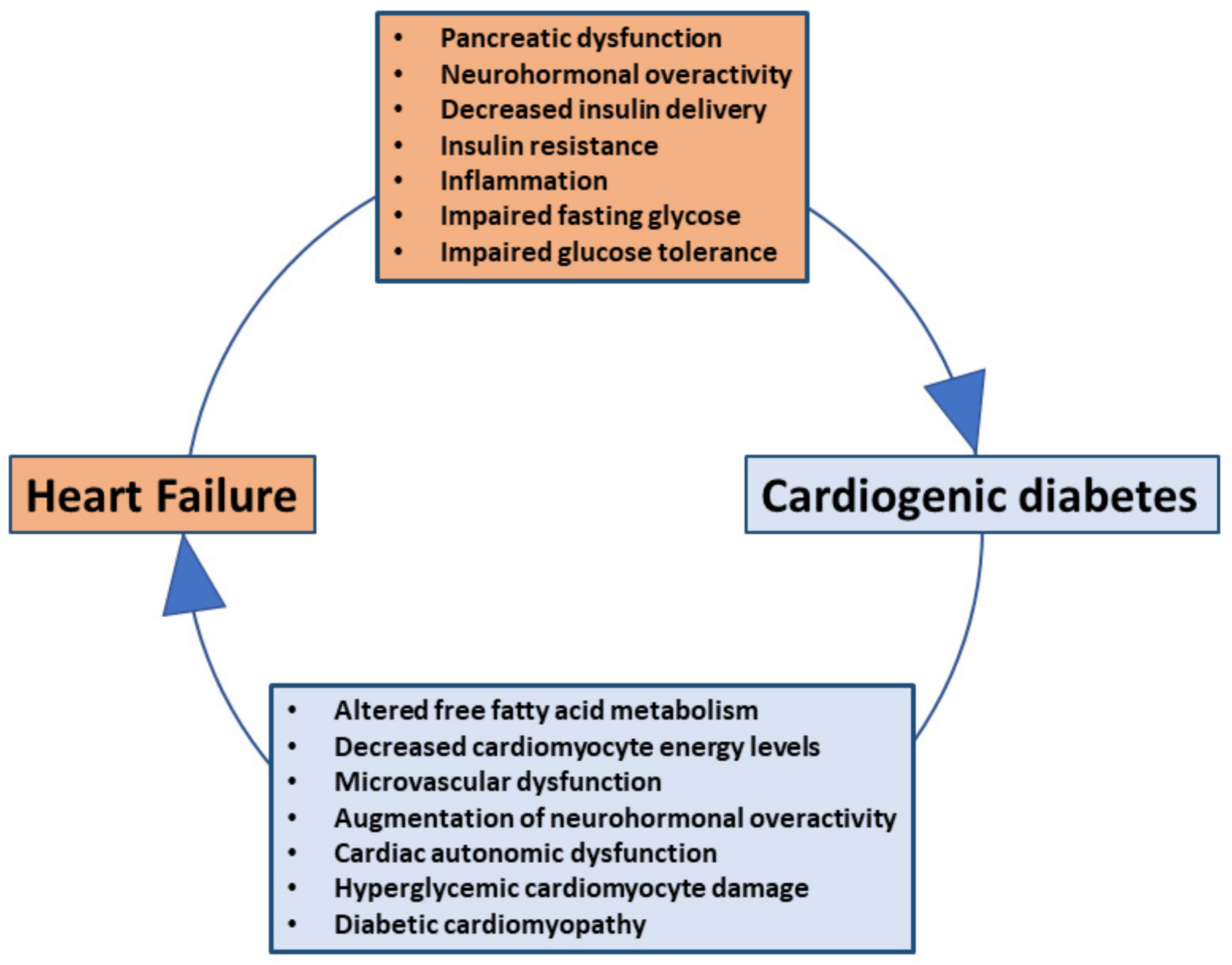
1.4. New-Onset Diabetes (Cardiogenic Diabetes) in Patients with Heart Failure
1.4.1. Epidemiology
1.4.2. Pathogenesis
1.4.3. Prevention of New-Onset Diabetes in Patients with Heart Failure
1.4.4. Gaps in Knowledge and Future Perspectives
2. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gulsin, G.S.; Athithan, L.; McCann, G.P. Diabetic cardiomyopathy: Prevalence, determinants and potential treatments. Ther. Adv. Endocrinol. Metab. 2019, 10. [Google Scholar] [CrossRef] [PubMed]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef] [Green Version]
- Lind, M.; Bounias, I.; Olsson, M.; Gudbjornsdottir, S.; Svensson, A.M.; Rosengren, A. Glycaemic control and incidence of heart failure in 20,985 patients with type 1 diabetes: An observational study. Lancet 2011, 378, 140–146. [Google Scholar] [CrossRef]
- Stratton, I.M.; Adler, A.I.; Neil, H.A.; Matthews, D.R.; Manley, S.E.; Cull, C.A.; Hadden, D.; Turner, R.C.; Holman, R.R. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): Prospective observational study. Br. Med. J. 2000, 321, 405–412. [Google Scholar] [CrossRef] [Green Version]
- Bouthoorn, S.; Valstar, G.B.; Gohar, A.; den Ruijter, H.M.; Reitsma, H.B.; Hoes, A.W.; Rutten, F.H. The prevalence of left ventricular diastolic dysfunction and heart failure with preserved ejection fraction in men and women with type 2 diabetes: A systematic review and meta-analysis. Diab. Vasc. Dis. Res. 2018, 15, 477–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konduracka, E.; Gackowski, A.; Rostoff, P.; Galicka-Latala, D.; Frasik, W.; Piwowarska, W. Diabetes-specific cardiomyopathy in type 1 diabetes mellitus: No evidence for its occurrence in the era of intensive insulin therapy. Eur. Heart J. 2007, 28, 2465–2471. [Google Scholar] [CrossRef] [Green Version]
- Zareini, B.; Rorth, R.; Holt, A.; Mogensen, U.M.; Selmer, C.; Gislason, G.; Schou, M.; Kober, L.; Torp-Pedersen, C.; Lamberts, M.; et al. Heart failure and the prognostic impact and incidence of new-onset of diabetes mellitus: A nationwide cohort study. Cardiovasc. Diabetol. 2019, 18, 79. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kannel, W.B.; Hjortland, M.; Castelli, W.P. Role of diabetes in congestive heart failure: The Framingham study. Am. J. Cardiol. 1974, 34, 29–34. [Google Scholar] [CrossRef]
- Kodama, S.; Fujihara, K.; Horikawa, C.; Sato, T.; Iwanaga, M.; Yamada, T.; Kato, K.; Watanabe, K.; Shimano, H.; Izumi, T.; et al. Diabetes mellitus and risk of new-onset and recurrent heart failure: A systematic review and meta-analysis. ESC Heart Fail. 2020, 7, 2146–2174. [Google Scholar] [CrossRef] [PubMed]
- Triposkiadis, F.; Giamouzis, G.; Parissis, J.; Starling, R.C.; Boudoulas, H.; Skoularigis, J.; Butler, J.; Filippatos, G. Reframing the association and significance of co-morbidities in heart failure. Eur. J. Heart Fail. 2016, 18, 744–758. [Google Scholar] [CrossRef] [PubMed]
- Bell, D.S. Heart failure: The frequent, forgotten, and often fatal complication of diabetes. Diabetes Care 2003, 26, 2433–2441. [Google Scholar] [CrossRef] [Green Version]
- Hughes, J.W.; Riddlesworth, T.D.; DiMeglio, L.A.; Miller, K.M.; Rickels, M.R.; McGill, J.B. Network TDEC: Autoimmune Diseases in Children and Adults With Type 1 Diabetes From the T1D Exchange Clinic Registry. J. Clin. Endocrinol. Metab. 2016, 101, 4931–4937. [Google Scholar] [CrossRef] [PubMed]
- Sousa, G.R.; Pober, D.; Galderisi, A.; Lv, H.; Yu, L.; Pereira, A.C.; Doria, A.; Kosiborod, M.; Lipes, M.A. Glycemic Control, Cardiac Autoimmunity, and Long-Term Risk of Cardiovascular Disease in Type 1 Diabetes Mellitus. Circulation 2019, 139, 730–743. [Google Scholar] [CrossRef] [PubMed]
- Petrie, J.R.; Sattar, N. Excess Cardiovascular Risk in Type 1 Diabetes Mellitus. Circulation 2019, 139, 744–747. [Google Scholar] [CrossRef] [PubMed]
- Rubattu, S.; Triposkiadis, F. Resetting the neurohormonal balance in heart failure (HF): The relevance of the natriuretic peptide (NP) system to the clinical management of patients with HF. Heart Fail. Rev. 2017, 22, 279–288. [Google Scholar] [CrossRef] [Green Version]
- Vinnakota, S.; Chen, H.H. The Importance of Natriuretic Peptides in Cardiometabolic Diseases. J. Endocr. Soc. 2020, 4, bvaa052. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.J. Natriuretic Peptide Deficiency-When There Is Too Little of a Good Thing. JAMA Cardiol. 2018, 3, 7–9. [Google Scholar] [CrossRef]
- Jordan, J.; Birkenfeld, A.L.; Melander, O.; Moro, C. Natriuretic Peptides in Cardiovascular and Metabolic Crosstalk: Implications for Hypertension Management. Hypertension 2018, 72, 270–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khouri, M.G.; Peshock, R.M.; Ayers, C.R.; de Lemos, J.A.; Drazner, M.H. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: The Dallas heart study. Circ. Cardiovasc. Imaging 2010, 3, 164–171. [Google Scholar] [CrossRef] [PubMed]
- Aurigemma, G.P.; de Simone, G.; Fitzgibbons, T.P. Cardiac remodeling in obesity. Circ. Cardiovasc. Imaging 2013, 6, 142–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Turkbey, E.B.; McClelland, R.L.; Kronmal, R.A.; Burke, G.L.; Bild, D.E.; Tracy, R.P.; Arai, A.E.; Lima, J.A.; Bluemke, D.A. The impact of obesity on the left ventricle: The Multi-Ethnic Study of Atherosclerosis (MESA). JACC Cardiovasc. Imaging 2010, 3, 266–274. [Google Scholar] [CrossRef] [Green Version]
- Woodiwiss, A.J.; Libhaber, C.D.; Majane, O.H.; Libhaber, E.; Maseko, M.; Norton, G.R. Obesity promotes left ventricular concentric rather than eccentric geometric remodeling and hypertrophy independent of blood pressure. Am. J. Hypertens. 2008, 21, 1144–1151. [Google Scholar] [CrossRef]
- Lee, T.C.; Jin, Z.; Homma, S.; Nakanishi, K.; Elkind, M.S.V.; Rundek, T.; Tugcu, A.; Matsumoto, K.; Sacco, R.L.; Di Tullio, M.R. Changes in Left Ventricular Mass and Geometry in the Older Adults: Role of Body Mass and Central Obesity. J. Am. Soc. Echocardiogr. 2019, 32, 1318–1325. [Google Scholar] [CrossRef] [PubMed]
- Cuspidi, C.; Rescaldani, M.; Sala, C.; Grassi, G. Left-ventricular hypertrophy and obesity: A systematic review and meta-analysis of echocardiographic studies. J. Hypertens. 2014, 32, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Corbin, K.D.; Driscoll, K.A.; Pratley, R.E.; Smith, S.R.; Maahs, D.M.; Mayer-Davis, E.J. Advancing Care for Type 1 Diabetes and Obesity Network (ACT1ON): Obesity in Type 1 Diabetes: Pathophysiology, Clinical Impact, and Mechanisms. Endocr. Rev. 2018, 39, 629–663. [Google Scholar] [CrossRef] [Green Version]
- Task Force, M.; Ryden, L.; Grant, P.J.; Anker, S.D.; Berne, C.; Cosentino, F.; Danchin, N.; Deaton, C.; Escaned, J.; Hammes, H.P.; et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur. Heart J. 2013, 34, 3035–3087. [Google Scholar]
- Seferovic, P.M.; Petrie, M.C.; Filippatos, G.S.; Anker, S.D.; Rosano, G.; Bauersachs, J.; Paulus, W.J.; Komajda, M.; Cosentino, F.; de Boer, R.A.; et al. Type 2 diabetes mellitus and heart failure: A position statement from the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 853–872. [Google Scholar] [CrossRef] [PubMed]
- Dandamudi, S.; Slusser, J.; Mahoney, D.W.; Redfield, M.M.; Rodeheffer, R.J.; Chen, H.H. The prevalence of diabetic cardiomyopathy: A population-based study in Olmsted County, Minnesota. J. Card. Fail. 2014, 20, 304–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klajda, M.D.; Scott, C.G.; Rodeheffer, R.J.; Chen, H.H. Diabetes Mellitus Is an Independent Predictor for the Development of Heart Failure: A Population Study. Mayo. Clin. Proc. 2020, 95, 124–133. [Google Scholar] [CrossRef] [Green Version]
- Tsimihodimos, V.; Gonzalez-Villalpando, C.; Meigs, J.B.; Ferrannini, E. Hypertension and Diabetes Mellitus: Coprediction and Time Trajectories. Hypertension 2018, 71, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Reaven, G.M. Banting Lecture 1988. Role of insulin resistance in human disease 1988. Nutrition 1997, 13, 65. [Google Scholar] [PubMed]
- Moreno, P.R.; Murcia, A.M.; Palacios, I.F.; Leon, M.N.; Bernardi, V.H.; Fuster, V.; Fallon, J.T. Coronary composition and macrophage infiltration in atherectomy specimens from patients with diabetes mellitus. Circulation 2000, 102, 2180–2184. [Google Scholar] [CrossRef] [Green Version]
- Schramm, T.K.; Gislason, G.H.; Kober, L.; Rasmussen, S.; Rasmussen, J.N.; Abildstrom, S.Z.; Hansen, M.L.; Folke, F.; Buch, P.; Madsen, M.; et al. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: A population study of 3.3 million people. Circulation 2008, 117, 1945–1954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jia, G.; DeMarco, V.G.; Sowers, J.R. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat. Rev. Endocrinol. 2016, 12, 144–153. [Google Scholar] [CrossRef]
- Jia, G.; Whaley-Connell, A.; Sowers, J.R. Diabetic cardiomyopathy: A hyperglycaemia—and insulin-resistance-induced heart disease. Diabetologia 2018, 61, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.; Zhang, Z.; Zheng, C.; Wintergerst, K.A.; Keller, B.B.; Cai, L. Mechanisms of diabetic cardiomyopathy and potential therapeutic strategies: Preclinical and clinical evidence. Nat. Rev. Cardiol. 2020, 17, 585–607. [Google Scholar] [CrossRef] [PubMed]
- Kahkoska, A.R.; Nguyen, C.T.; Adair, L.A.; Aiello, A.E.; Burger, K.S.; Buse, J.B.; Dabelea, D.; Dolan, L.M.; Malik, F.S.; Mottl, A.K.; et al. Longitudinal Phenotypes of Type 1 Diabetes in Youth Based on Weight and Glycemia and Their Association with Complications. J. Clin. Endocrinol. Metab. 2019, 104, 6003–6016. [Google Scholar] [CrossRef]
- Mapanga, R.F.; Essop, M.F. Damaging effects of hyperglycemia on cardiovascular function: Spotlight on glucose metabolic pathways. Am. J Physiol. Heart Circ. Physiol. 2016, 310, H153–H173. [Google Scholar] [CrossRef] [Green Version]
- Ormazabal, V.; Nair, S.; Elfeky, O.; Aguayo, C.; Salomon, C.; Zuniga, F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018, 17, 122. [Google Scholar] [CrossRef] [PubMed]
- Jia, G.; Hill, M.A.; Sowers, J.R. Diabetic Cardiomyopathy: An Update of Mechanisms Contributing to This Clinical Entity. Circ. Res. 2018, 122, 624–638. [Google Scholar] [CrossRef]
- Karwi, Q.G.; Uddin, G.M.; Ho, K.L.; Lopaschuk, G.D. Loss of Metabolic Flexibility in the Failing Heart. Front. Cardiovasc. Med. 2018, 5, 68. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tuleta, I.; Frangogiannis, N.G. Diabetic fibrosis. Biochim. Biophys. Acta Mol Basis Dis. 2021, 1867, 166044. [Google Scholar] [CrossRef]
- Ernande, L.; Bergerot, C.; Rietzschel, E.R.; De Buyzere, M.L.; Thibault, H.; Pignonblanc, P.G.; Croisille, P.; Ovize, M.; Groisne, L.; Moulin, P.; et al. Diastolic dysfunction in patients with type 2 diabetes mellitus: Is it really the first marker of diabetic cardiomyopathy? J. Am. Soc. Echocardiogr. 2011, 24, 1268–1275.e1. [Google Scholar] [CrossRef] [PubMed]
- Minciuna, I.A.; Hilda Orasan, O.; Minciuna, I.; Lazar, A.L.; Sitar-Taut, A.V.; Oltean, M.; Tomoaia, R.; Puiu, M.; Sitar-Taut, D.A.; Pop, D.; et al. Assessment of subclinical diabetic cardiomyopathy by speckle-tracking imaging. Eur. J. Clin. Investig. 2021, 51, e13475. [Google Scholar] [CrossRef]
- Chen, Q.; Gan, Y.; Li, Z.Y. Left ventricular diastolic dysfunction in type 2 diabetes patients: A novel 2D strain analysis based on cardiac magnetic resonance imaging. Comput. Methods Biomech. Biomed. Engin. 2016, 19, 1330–1338. [Google Scholar] [CrossRef]
- Tadic, M.; Cuspidi, C. Left atrial function in diabetes: Does it help? Acta Diabetol. 2021, 58, 131–137. [Google Scholar] [CrossRef]
- Steele, J.M.; Urbina, E.M.; Mazur, W.M.; Khoury, P.R.; Nagueh, S.F.; Tretter, J.T.; Alsaied, T. Left atrial strain and diastolic function abnormalities in obese and type 2 diabetic adolescents and young adults. Cardiovasc. Diabetol. 2020, 19, 163. [Google Scholar] [CrossRef] [PubMed]
- Linssen, P.B.C.; Veugen, M.G.J.; Henry, R.M.A.; van der Kallen, C.J.H.; Kroon, A.A.; Schram, M.T.; Brunner-La Rocca, H.P.; Stehouwer, C.D.A. Associations of (pre)diabetes with right ventricular and atrial structure and function: The Maastricht Study. Cardiovasc. Diabetol. 2020, 19, 88. [Google Scholar] [CrossRef]
- Jensen, M.T.; Fung, K.; Aung, N.; Sanghvi, M.M.; Chadalavada, S.; Paiva, J.M.; Khanji, M.Y.; de Knegt, M.C.; Lukaschuk, E.; Lee, A.M.; et al. Changes in Cardiac Morphology and Function in Individuals With Diabetes Mellitus: The UK Biobank Cardiovascular Magnetic Resonance Substudy. Circ. Cardiovasc. Imaging 2019, 12, e009476. [Google Scholar] [CrossRef] [Green Version]
- Kumric, M.; Ticinovic Kurir, T.; Borovac, J.A.; Bozic, J. Role of novel biomarkers in diabetic cardiomyopathy. World J. Diabetes 2021, 12, 685–705. [Google Scholar] [CrossRef]
- Shin, D.; Bohra, C.; Kongpakpaisarn, K. Impact of the Discordance Between the American College of Cardiology/American Heart Association and American Diabetes Association Recommendations on Hypertension in Patients with Diabetes Mellitus in the United States. Hypertension 2018, 72, 256–259. [Google Scholar] [CrossRef]
- Dabelea, D.; Stafford, J.M.; Mayer-Davis, E.J.; D’Agostino, R., Jr.; Dolan, L.; Imperatore, G.; Linder, B.; Lawrence, J.M.; Marcovina, S.M.; Mottl, A.K.; et al. Association of Type 1 Diabetes vs Type 2 Diabetes Diagnosed During Childhood and Adolescence With Complications During Teenage Years and Young Adulthood. JAMA 2017, 317, 825–835. [Google Scholar] [CrossRef] [Green Version]
- Katsimardou, A.; Imprialos, K.; Stavropoulos, K.; Sachinidis, A.; Doumas, M.; Athyros, V.G. Treatment strategies for hypertension in patients with type 1 diabetes. Expert Opin. Pharmacother. 2020, 21, 1241–1252. [Google Scholar] [CrossRef]
- Yildiz, M.; Esenboga, K.; Oktay, A.A. Hypertension and diabetes mellitus: Highlights of a complex relationship. Curr. Opin. Cardiol. 2020, 35, 397–404. [Google Scholar] [CrossRef]
- Fraser, G.E.; Strahan, T.M.; Sabate, J.; Beeson, W.L.; Kissinger, D. Effects of traditional coronary risk factors on rates of incident coronary events in a low-risk population. The Adventist Health Study. Circulation 1992, 86, 406–413. [Google Scholar] [CrossRef] [Green Version]
- Folsom, A.R.; Szklo, M.; Stevens, J.; Liao, F.; Smith, R.; Eckfeldt, J.H. A prospective study of coronary heart disease in relation to fasting insulin, glucose, and diabetes. The Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care 1997, 20, 935–942. [Google Scholar] [CrossRef]
- Haffner, S.M.; Lehto, S.; Ronnemaa, T.; Pyorala, K.; Laakso, M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N. Engl. J. Med. 1998, 339, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Goodarzi, M.O.; Rotter, J.I. Genetics Insights in the Relationship Between Type 2 Diabetes and Coronary Heart Disease. Circ. Res. 2020, 126, 1526–1548. [Google Scholar] [CrossRef] [PubMed]
- Secrest, A.M.; Becker, D.J.; Kelsey, S.F.; LaPorte, R.E.; Orchard, T.J. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: The Allegheny County type 1 diabetes registry. Diabetes Care 2010, 33, 2573–2579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huxley, R.R.; Peters, S.A.; Mishra, G.D.; Woodward, M. Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015, 3, 198–206. [Google Scholar] [CrossRef]
- Costacou, T.; Edmundowicz, D.; Prince, C.; Conway, B.; Orchard, T.J. Progression of coronary artery calcium in type 1 diabetes mellitus. Am. J. Cardiol. 2007, 100, 1543–1547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, P.J.; Cosentino, F.; Marx, N. Diabetes and coronary artery disease: Not just a risk factor. Heart 2020, 106, 1357–1364. [Google Scholar] [CrossRef] [PubMed]
- Kibel, A.; Selthofer-Relatic, K.; Drenjancevic, I.; Bacun, T.; Bosnjak, I.; Kibel, D.; Gros, M. Coronary microvascular dysfunction in diabetes mellitus. J. Int. Med. Res. 2017, 45, 1901–1929. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konst, R.E.; Guzik, T.J.; Kaski, J.C.; Maas, A.; Elias-Smale, S.E. The pathogenic role of coronary microvascular dysfunction in the setting of other cardiac or systemic conditions. Cardiovasc. Res. 2020, 116, 817–828. [Google Scholar] [CrossRef] [Green Version]
- Li, X.M.; Jiang, L.; Guo, Y.K.; Ren, Y.; Han, P.L.; Peng, L.Q.; Shi, R.; Yan, W.F.; Yang, Z.G. The additive effects of type 2 diabetes mellitus on left ventricular deformation and myocardial perfusion in essential hypertension: A 3.0 T cardiac magnetic resonance study. Cardiovasc. Diabetol. 2020, 19, 161. [Google Scholar] [CrossRef]
- Liu, X.; Yang, Z.G.; Gao, Y.; Xie, L.J.; Jiang, L.; Hu, B.Y.; Diao, K.Y.; Shi, K.; Xu, H.Y.; Shen, M.T.; et al. Left ventricular subclinical myocardial dysfunction in uncomplicated type 2 diabetes mellitus is associated with impaired myocardial perfusion: A contrast-enhanced cardiovascular magnetic resonance study. Cardiovasc. Diabetol. 2018, 17, 139. [Google Scholar] [CrossRef] [Green Version]
- Vancheri, F.; Longo, G.; Vancheri, S.; Henein, M. Coronary Microvascular Dysfunction. J. Clin. Med. 2020, 9, 2880. [Google Scholar] [CrossRef]
- Braunwald, E. Diabetes, heart failure, and renal dysfunction: The vicious circles. Prog. Cardiovasc. Dis. 2019, 62, 298–302. [Google Scholar] [CrossRef]
- De Boer, I.H.; Bakris, G.L. Diabetic Kidney Disease: A Determinant of Cardiovascular Risk in Type 1 Diabetes. Diabetes Care 2018, 41, 662–663. [Google Scholar] [CrossRef] [Green Version]
- Jankowski, J.; Floege, J.; Fliser, D.; Bohm, M.; Marx, N. Cardiovascular Disease in Chronic Kidney Disease: Pathophysiological Insights and Therapeutic Options. Circulation 2021, 143, 1157–1172. [Google Scholar] [CrossRef]
- Groop, P.H.; Thomas, M.C.; Moran, J.L.; Waden, J.; Thorn, L.M.; Makinen, V.P.; Rosengard-Barlund, M.; Saraheimo, M.; Hietala, K.; Heikkila, O.; et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 2009, 58, 1651–1658. [Google Scholar] [CrossRef] [Green Version]
- Afkarian, M.; Sachs, M.C.; Kestenbaum, B.; Hirsch, I.B.; Tuttle, K.R.; Himmelfarb, J.; de Boer, I.H. Kidney disease and increased mortality risk in type 2 diabetes. J. Am. Soc. Nephrol. 2013, 24, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Dagar, N.; Das, P.; Bisht, P.; Taraphdar, A.K.; Velayutham, R.; Arumugam, S. Diabetic nephropathy: A twisted thread to unravel. Life Sci. 2021, 278, 119635. [Google Scholar] [CrossRef] [PubMed]
- Aguilar, D. Heart Failure, Diabetes Mellitus, and Chronic Kidney Disease: A Clinical Conundrum. Circ. Heart Fail. 2016, 9, e003316. [Google Scholar] [CrossRef] [Green Version]
- Lovre, D.; Shah, S.; Sihota, A.; Fonseca, V.A. Managing Diabetes and Cardiovascular Risk in Chronic Kidney Disease Patients. Endocrinol. Metab. Clin. N. Am. 2018, 47, 237–257. [Google Scholar] [CrossRef]
- Kang, Y.; Wang, S.; Huang, J.; Cai, L.; Keller, B.B. Right ventricular dysfunction and remodeling in diabetic cardiomyopathy. Am. J. Physiol. Heart Circ. Physiol. 2019, 316, H113–H122. [Google Scholar] [CrossRef] [PubMed]
- Maisch, B.; Alter, P.; Pankuweit, S. Diabetic cardiomyopathy—Fact or fiction? Herz 2011, 36, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, R.H.; Abel, E.D. Basic Mechanisms of Diabetic Heart Disease. Circ. Res. 2020, 126, 1501–1525. [Google Scholar] [CrossRef]
- Seferovic, P.M.; Paulus, W.J. Clinical diabetic cardiomyopathy: A two-faced disease with restrictive and dilated phenotypes. Eur. Heart J. 2015, 36, 1718–1727. [Google Scholar] [CrossRef] [PubMed]
- Klein, H.U. Diabetes Mellitus: Merely “Comorbidity” or an Important Risk Factor? JACC Clin. Electrophysiol. 2020, 6, 559–561. [Google Scholar] [CrossRef]
- Butler, J.; Anker, S.D.; Packer, M. Redefining Heart Failure with a Reduced Ejection Fraction. JAMA 2019, 322, 1761–1762. [Google Scholar] [CrossRef]
- Gu, J.; Yin, Z.F.; Zhang, H.L.; Fan, Y.Q.; Zhang, J.F.; Wang, C.Q. Characteristics and outcomes of transitions among heart failure categories: A prospective observational cohort study. ESC Heart Fail. 2020, 7, 616–625. [Google Scholar] [CrossRef] [Green Version]
- Bayes-Genis, A.; Lupon, J. Heart failure is ejection fraction in motion. Eur. J. Heart Fail. 2021, 23, 564–566. [Google Scholar] [CrossRef]
- Triposkiadis, F.; Butler, J.; Abboud, F.M.; Armstrong, P.W.; Adamopoulos, S.; Atherton, J.J.; Backs, J.; Bauersachs, J.; Burkhoff, D.; Bonow, R.O.; et al. The continuous heart failure spectrum: Moving beyond an ejection fraction classification. Eur. Heart J. 2019, 40, 2155–2163. [Google Scholar] [CrossRef]
- Bruemmer, D.; Nissen, S.E. Prevention and management of cardiovascular disease in patients with diabetes: Current challenges and opportunities. Cardiovasc. Endocrinol. Metab. 2020, 9, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Pandey, A.; Garg, S.; Khunger, M.; Darden, D.; Ayers, C.; Kumbhani, D.J.; Mayo, H.G.; de Lemos, J.A.; Berry, J.D. Dose-Response Relationship Between Physical Activity and Risk of Heart Failure: A Meta-Analysis. Circulation 2015, 132, 1786–1794. [Google Scholar] [CrossRef] [Green Version]
- Pandey, A.; Cornwell, W.K., 3rd; Willis, B.; Neeland, I.J.; Gao, A.; Leonard, D.; DeFina, L.; Berry, J.D. Body Mass Index and Cardiorespiratory Fitness in Mid-Life and Risk of Heart Failure Hospitalization in Older Age: Findings From the Cooper Center Longitudinal Study. JACC Hearth Fail. 2017, 5, 367–374. [Google Scholar] [CrossRef]
- Sundstrom, J.; Bruze, G.; Ottosson, J.; Marcus, C.; Naslund, I.; Neovius, M. Weight Loss and Heart Failure: A Nationwide Study of Gastric Bypass Surgery Versus Intensive Lifestyle Treatment. Circulation 2017, 135, 1577–1585. [Google Scholar] [CrossRef]
- Aminian, A.; Zajichek, A.; Arterburn, D.E.; Wolski, K.E.; Brethauer, S.A.; Schauer, P.R.; Kattan, M.W.; Nissen, S.E. Association of Metabolic Surgery with Major Adverse Cardiovascular Outcomes in Patients With Type 2 Diabetes and Obesity. JAMA 2019, 322, 1271–1282. [Google Scholar] [CrossRef]
- Gilbert, R.E.; Krum, H. Heart failure in diabetes: Effects of anti-hyperglycaemic drug therapy. Lancet 2015, 385, 2107–2117. [Google Scholar] [CrossRef]
- Abraira, C.; Duckworth, W.C.; Moritz, T. Group V: Glycaemic separation and risk factor control in the Veterans Affairs Diabetes Trial: An interim report. Diabetes Obes. Metab. 2009, 11, 150–156. [Google Scholar] [CrossRef]
- Zelniker, T.A.; Wiviott, S.D.; Raz, I.; Im, K.; Goodrich, E.L.; Furtado, R.H.M.; Bonaca, M.P.; Mosenzon, O.; Kato, E.T.; Cahn, A.; et al. Comparison of the Effects of Glucagon-Like Peptide Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors for Prevention of Major Adverse Cardiovascular and Renal Outcomes in Type 2 Diabetes Mellitus. Circulation 2019, 139, 2022–2031. [Google Scholar] [CrossRef]
- Pernicova, I.; Korbonits, M. Metformin—Mode of action and clinical implications for diabetes and cancer. Nat. Rev. Endocrinol. 2014, 10, 143–156. [Google Scholar] [CrossRef]
- UK Prospective Diabetes Study (UKPDS) Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 1998, 352, 854–865. [Google Scholar] [CrossRef]
- Petrie, J.R.; Rossing, P.R.; Campbell, I.W. Metformin and cardiorenal outcomes in diabetes: A reappraisal. Diabetes Obes. Metab. 2020, 22, 904–915. [Google Scholar] [CrossRef]
- Sheahan, K.H.; Wahlberg, E.A.; Gilbert, M.P. An overview of GLP-1 agonists and recent cardiovascular outcomes trials. Postgrad. Med. J. 2020, 96, 156–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
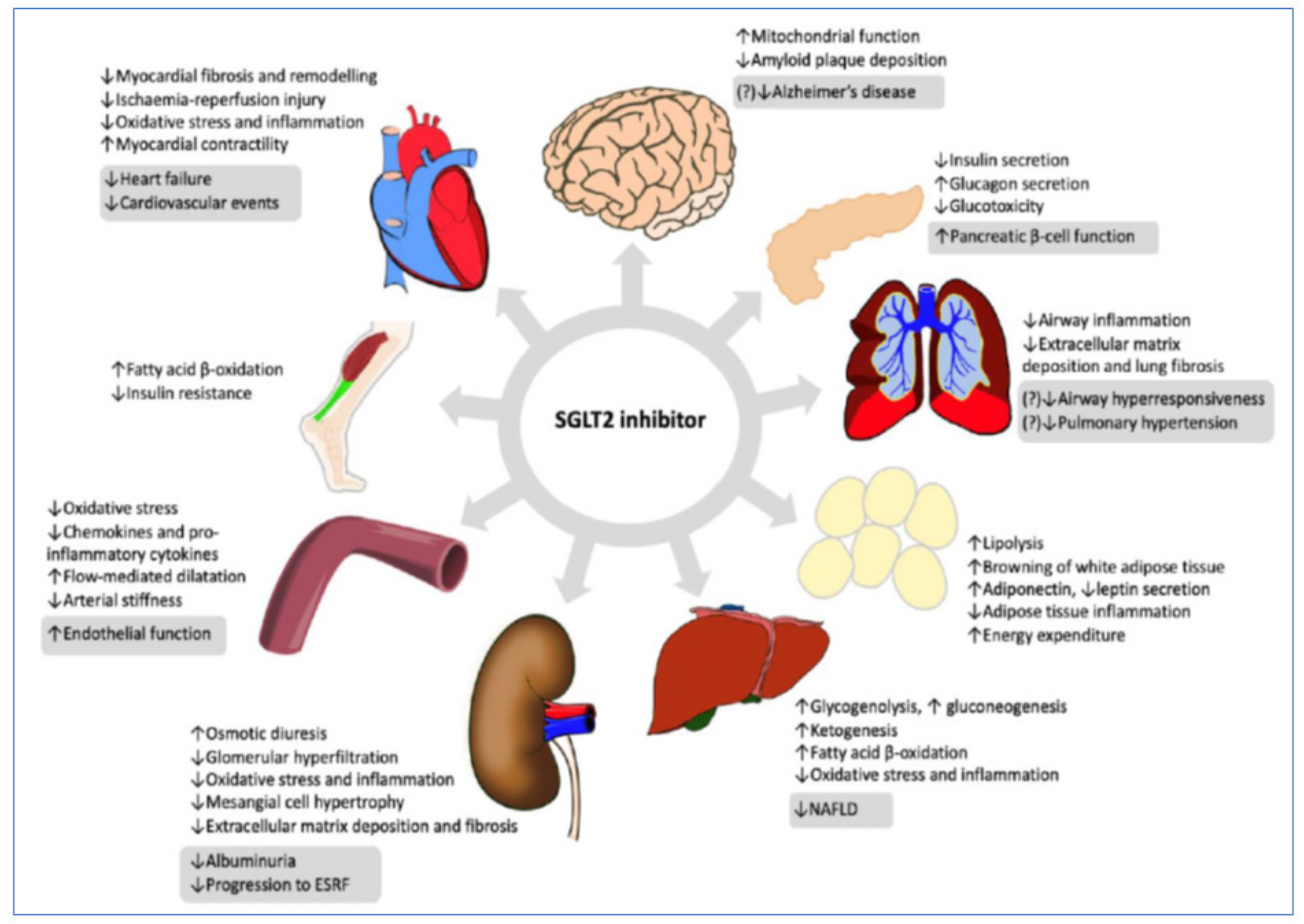
- Hoong, C.W.S.; Chua, M.W.J. SGLT2 inhibitors as calorie restriction-mimetics: Insights on longevity pathways and age-related diseases. Endocrinology 2021, 162, bqab079. [Google Scholar] [CrossRef]
- Xiao, L.; Nie, X.; Cheng, Y.; Wang, N. Sodium-Glucose Cotransporter-2 Inhibitors in Vascular Biology: Cellular and Molecular Mechanisms. Cardiovasc. Drugs Ther. 2021. [Google Scholar] [CrossRef]
- Vardeny, O. The Sweet Spot: Heart Failure Prevention with SGLT2 Inhibitors. Am. J. Med. 2020, 133, 182–185. [Google Scholar] [CrossRef]
- Lopaschuk, G.D.; Verma, S. Mechanisms of Cardiovascular Benefits of Sodium Glucose Co-Transporter 2 (SGLT2) Inhibitors: A State-of-the-Art Review. JACC Basic Transl. Sci. 2020, 5, 632–644. [Google Scholar] [CrossRef]
- Bhatt, D.L.; Szarek, M.; Steg, P.G.; Cannon, C.P.; Leiter, L.A.; McGuire, D.K.; Lewis, J.B.; Riddle, M.C.; Voors, A.A.; Metra, M.; et al. Sotagliflozin in Patients with Diabetes and Recent Worsening Heart Failure. N. Engl. J. Med. 2021, 384, 117–128. [Google Scholar] [CrossRef]
- Pitt, B.; Bhatt, D.L. Does SGLT1 Inhibition Add Benefit to SGLT2 Inhibition in Type 2 Diabetes Mellitus? Circulation 2021, 144, 4–6. [Google Scholar] [CrossRef]
- Buse, J.B.; Wexler, D.J.; Tsapas, A.; Rossing, P.; Mingrone, G.; Mathieu, C.; D’Alessio, D.A.; Davies, M.J. 2019 Update to: Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2020, 43, 487–493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosentino, F.; Grant, P.J.; Aboyans, V.; Bailey, C.J.; Ceriello, A.; Delgado, V.; Federici, M.; Filippatos, G.; Grobbee, D.E.; Hansen, T.B.; et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur. Heart J. 2020, 41, 255–323. [Google Scholar] [CrossRef] [Green Version]
- Marx, N.; Davies, M.J.; Grant, P.J.; Mathieu, C.; Petrie, J.R.; Cosentino, F.; Buse, J.B. Guideline recommendations and the positioning of newer drugs in type 2 diabetes care. Lancet Diabetes Endocrinol. 2021, 9, 46–52. [Google Scholar] [CrossRef]
- Khan, M.S.; Fonarow, G.C.; McGuire, D.K.; Hernandez, A.F.; Vaduganathan, M.; Rosenstock, J.; Handelsman, Y.; Verma, S.; Anker, S.D.; McMurray, J.J.V.; et al. Glucagon-Like Peptide 1 Receptor Agonists and Heart Failure: The Need for Further Evidence Generation and Practice Guidelines Optimization. Circulation 2020, 142, 1205–1218. [Google Scholar] [CrossRef] [PubMed]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Januzzi, J.L., Jr. Preventing and Treating Heart Failure with Sodium-Glucose Co-Transporter 2 Inhibitors. Am. J. Cardiol. 2019, 124, S20–S27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Vandvik, P.O.; Lytvyn, L.; Guyatt, G.H.; Palmer, S.C.; Rodriguez-Gutierrez, R.; Foroutan, F.; Agoritsas, T.; Siemieniuk, R.A.C.; Walsh, M.; et al. SGLT-2 inhibitors or GLP-1 receptor agonists for adults with type 2 diabetes: A clinical practice guideline. Br. Med. J. 2021, 373, n1091. [Google Scholar] [CrossRef]
- Tenenbaum, A.; Motro, M.; Fisman, E.Z.; Leor, J.; Freimark, D.; Boyko, V.; Mandelzweig, L.; Adler, Y.; Sherer, Y.; Behar, S. Functional class in patients with heart failure is associated with the development of diabetes. Am. J. Med. 2003, 114, 271–275. [Google Scholar] [CrossRef]
- Zareini, B.; Blanche, P.B.; Holt, A.H. New-onset type 2 diabetes in heart failure: Impact of heart failure and death versus ischemic events–a Danish nationwide cohort study. Eur. Heart J. 2020, 41. [Google Scholar] [CrossRef]
- Paolillo, S.; Rengo, G.; Pellegrino, T.; Formisano, R.; Pagano, G.; Gargiulo, P.; Savarese, G.; Carotenuto, R.; Petraglia, L.; Rapacciuolo, A.; et al. Insulin resistance is associated with impaired cardiac sympathetic innervation in patients with heart failure. Eur. Hearth J. Cardiovasc. Imaging 2015, 16, 1148–1153. [Google Scholar] [CrossRef] [Green Version]
- Morisco, C.; Lembo, G.; Trimarco, B. Insulin resistance and cardiovascular risk: New insights from molecular and cellular biology. Trends Cardiovasc. Med. 2006, 16, 183–188. [Google Scholar] [CrossRef]
- Yaribeygi, H.; Farrokhi, F.R.; Butler, A.E.; Sahebkar, A. Insulin resistance: Review of the underlying molecular mechanisms. J. Cell Physiol. 2019, 234, 8152–8161. [Google Scholar] [CrossRef] [PubMed]
- Himanshu, D.; Ali, W.; Wamique, M. Type 2 diabetes mellitus: Pathogenesis and genetic diagnosis. J. Diabetes Metab. Disord. 2020, 19, 1959–1966. [Google Scholar] [CrossRef]
- Buscemi, S.; Nicolucci, A.; Lucisano, G.; Galvano, F.; Grosso, G.; Massenti, F.M.; Amodio, E.; Bonura, A.; Sprini, D.; Rini, G.B. Impact of chronic diuretic treatment on glucose homeostasis. Diabetol. Metab. Syndr. 2013, 5, 80. [Google Scholar] [CrossRef] [Green Version]
- Torp-Pedersen, C.; Metra, M.; Charlesworth, A.; Spark, P.; Lukas, M.A.; Poole-Wilson, P.A.; Swedberg, K.; Cleland, J.G.; Di Lenarda, A.; Remme, W.J.; et al. Effects of metoprolol and carvedilol on pre-existing and new onset diabetes in patients with chronic heart failure: Data from the Carvedilol Or Metoprolol European Trial (COMET). Heart 2007, 93, 968–973. [Google Scholar] [CrossRef]
- Bakris, G.L.; Fonseca, V.; Katholi, R.E.; McGill, J.B.; Messerli, F.H.; Phillips, R.A.; Raskin, P.; Wright, J.T., Jr.; Oakes, R.; Lukas, M.A.; et al. Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: A randomized controlled trial. JAMA 2004, 292, 2227–2236. [Google Scholar] [CrossRef] [Green Version]
- Aguilar, D.; Solomon, S.D. ACE inhibitors and angiotensin receptor antagonists and the incidence of new-onset diabetes mellitus: An emerging theme. Drugs 2006, 66, 1169–1177. [Google Scholar] [CrossRef]
- Preiss, D.; van Veldhuisen, D.J.; Sattar, N.; Krum, H.; Swedberg, K.; Shi, H.; Vincent, J.; Pocock, S.J.; Pitt, B.; Zannad, F.; et al. Eplerenone and new-onset diabetes in patients with mild heart failure: Results from the Eplerenone in Mild Patients Hospitalization and Survival Study in Heart Failure (EMPHASIS-HF). Eur. J. Hearth Fail. 2012, 14, 909–915. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jordan, J.; Stinkens, R.; Jax, T.; Engeli, S.; Blaak, E.E.; May, M.; Havekes, B.; Schindler, C.; Albrecht, D.; Pal, P.; et al. Improved Insulin Sensitivity With Angiotensin Receptor Neprilysin Inhibition in Individuals With Obesity and Hypertension. Clin. Pharmacol. Ther. 2017, 101, 254–263. [Google Scholar] [CrossRef]
- Seferovic, J.P.; Claggett, B.; Seidelmann, S.B.; Seely, E.W.; Packer, M.; Zile, M.R.; Rouleau, J.L.; Swedberg, K.; Lefkowitz, M.; Shi, V.C.; et al. Effect of sacubitril/valsartan versus enalapril on glycaemic control in patients with heart failure and diabetes: A post-hoc analysis from the PARADIGM-HF trial. Lancet Diabetes Endocrinol. 2017, 5, 333–340. [Google Scholar] [CrossRef] [Green Version]
- Zannad, F.; Ferreira, J.P.; Pocock, S.J.; Anker, S.D.; Butler, J.; Filippatos, G.; Brueckmann, M.; Ofstad, A.P.; Pfarr, E.; Jamal, W.; et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: A meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet 2020, 396, 819–829. [Google Scholar] [CrossRef]
- Anker, S.D.; Butler, J.; Filippatos, G.; Shahzeb Khan, M.; Ferreira, J.P.; Bocchi, E.; Bohm, M.; Brunner-La Rocca, H.P.; Choi, D.J.; Chopra, V.; et al. Baseline characteristics of patients with heart failure with preserved ejection fraction in the EMPEROR-Preserved trial. Eur. J. Hearth Fail. 2020, 22, 2383–2392. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
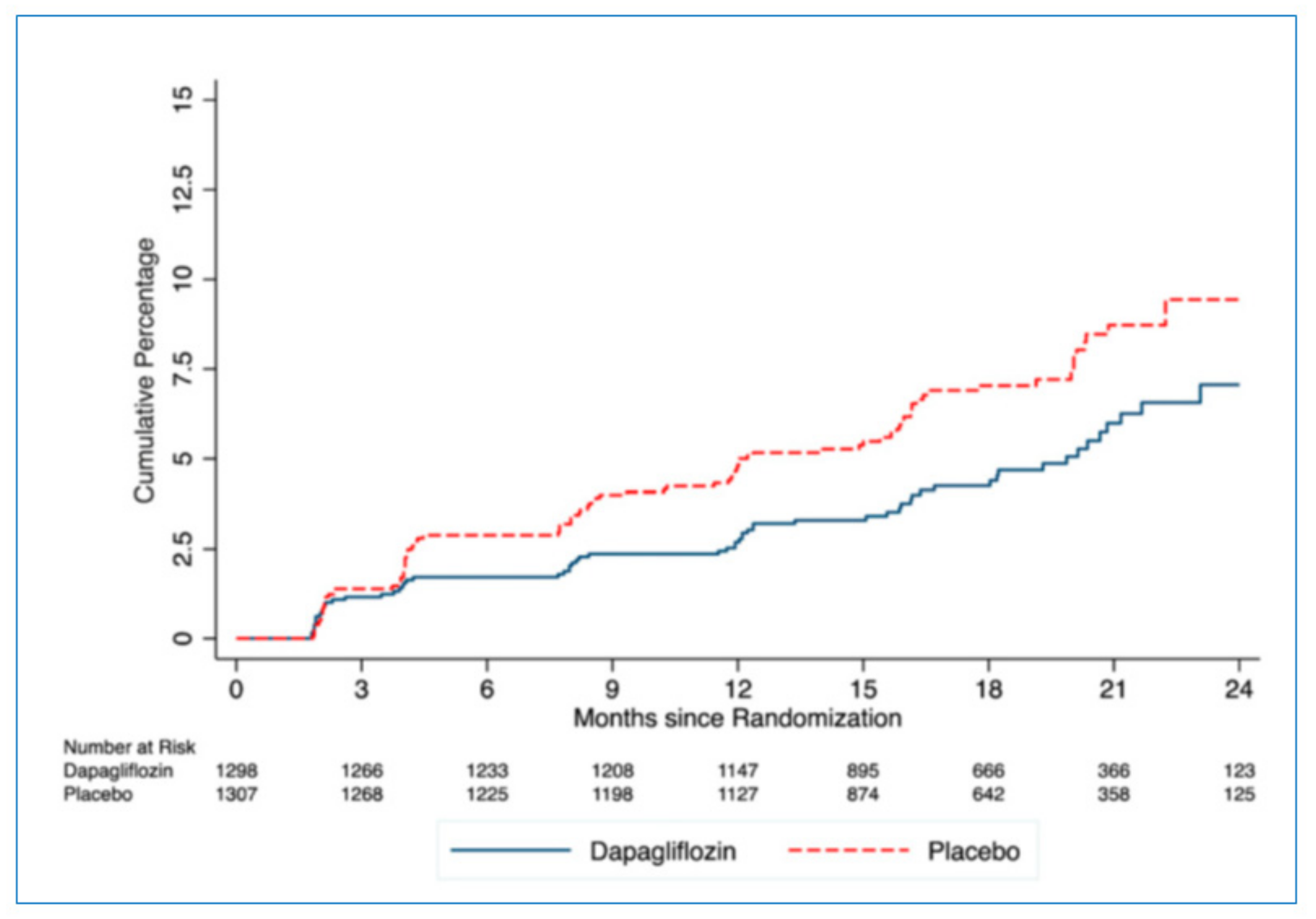
- Inzucchi, S.E.; Docherty, K.F.; Kober, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Solomon, S.D.; Verma, S.; Belohlavek, J.; et al. Dapagliflozin and the Incidence of Type 2 Diabetes in Patients With Heart Failure and Reduced Ejection Fraction: An Exploratory Analysis From DAPA-HF. Diabetes Care 2021, 44, 586–594. [Google Scholar] [CrossRef]
- Yaribeygi, H.; Sathyapalan, T.; Maleki, M.; Jamialahmadi, T.; Sahebkar, A. Molecular mechanisms by which SGLT2 inhibitors can induce insulin sensitivity in diabetic milieu: A mechanistic review. Life Sci. 2020, 240, 117090. [Google Scholar] [CrossRef]
- Alpert, M.A. Obesity cardiomyopathy: Pathophysiology and evolution of the clinical syndrome. Am. J. Med. Sci. 2001, 321, 225–236. [Google Scholar] [CrossRef]
- Tousoulis, D.; Oikonomou, E.; Siasos, G.; Stefanadis, C. Diabetes Mellitus and Heart Failure. Eur. Cardiol. 2014, 9, 37–42. [Google Scholar] [CrossRef]
- Shah, A.D.; Langenberg, C.; Rapsomaniki, E.; Denaxas, S.; Pujades-Rodriguez, M.; Gale, C.P.; Deanfield, J.; Smeeth, L.; Timmis, A.; Hemingway, H. Type 2 diabetes and incidence of cardiovascular diseases: A cohort study in 1.9 million people. Lancet Diabetes Endocrinol. 2015, 3, 105–113. [Google Scholar] [CrossRef] [Green Version]
- Nicholsm, G.A.; Moler, E.J. Cardiovascular disease, heart failure, chronic kidney disease and depression independently increase the risk of incident diabetes. Diabetologia 2011, 54, 523–526. [Google Scholar] [CrossRef] [Green Version]
- Bahrami, H.; Bluemke, D.A.; Kronmal, R.; Bertoni, A.G.; Lloyd-Jones, D.M.; Shahar, E.; Szklo, M.; Lima, J.A. Novel metabolic risk factors for incident heart failure and their relationship with obesity: The MESA (Multi-Ethnic Study of Atherosclerosis) study. J. Am. Coll. Cardiol. 2008, 51, 1775–1783. [Google Scholar] [CrossRef] [Green Version]
- Xanthopoulos, A.; Giamouzis, G.; Melidonis, A.; Kitai, T.; Paraskevopoulou, E.; Paraskevopoulou, P.; Patsilinakos, S.; Triposkiadis, F.; Skoularigis, J. Red blood cell distribution width as a prognostic marker in patients with heart failure and diabetes mellitus. Cardiovasc. Diabetol. 2017, 16, 81. [Google Scholar] [CrossRef] [PubMed]
- Peterson, L.R.; Gropler, R.J. Metabolic and Molecular Imaging of the Diabetic Cardiomyopathy. Circ. Res. 2020, 126, 1628–1645. [Google Scholar] [CrossRef] [PubMed]
- Badawi, R.D.; Shi, H.; Hu, P.; Chen, S.; Xu, T.; Price, P.M.; Ding, Y.; Spencer, B.A.; Nardo, L.; Liu, W.; et al. First Human Imaging Studies with the EXPLORER Total-Body PET Scanner. J. Nucl. Med. 2019, 60, 299–303. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.M.; Laforest, R.; Nensa, F.; Zheng, J.; Gropler, R.J.; Woodard, P.K. Cardiac Applications of PET/MR Imaging. Magn. Reason. Imaging Clin. N. Am. 2017, 25, 325–333. [Google Scholar] [CrossRef] [PubMed]


| Features | Stage | |||
|---|---|---|---|---|
| A | B | C | D | |
| Diabetic cardiomyopathy | Present | Present | Present | Present |
| Coexisting morbidities (hypertension, coronary artery disease (CAD), chronic kidney disease (CKD)) | Absent | Absent | Present | Present |
| Mechanisms | Metabolic disturbances (hyperglycemia, insulin resistance, hyperinsulinemia) leading to cardiac steatosis, microvascular dysfunction, increased ROS, and inflammation | Stage A plus myocardial necrosis, interstitial fibrosis, capillary microaneurysms, coronary microvascular rarefaction, and loss of cardiac metabolic flexibility | Stage B plus cardiovascular impairment due to coexisting morbidities | Stage C plus increased severity of coexisting morbidities (e.g., diffuse CAD and/or severe CKD) |
| Left ventricular remodeling | Absent Occasionally concentric remodeling or hypertrophy | Concentric remodeling or hypertrophy | Concentric hypertrophy or indeterminate hypertrophy (magnification) or eccentric hypertrophy | Eccentric hypertrophy |
| Cardiac function | Normal or mild diastolic dysfunction and mild decrease in systolic strain of both atria and ventricles | Diastolic dysfunction, decreased systolic strain Right and left atrial and ventricular involvement | Severe diastolic dysfunction Decreased LVEF Pulmonary hypertension | Biventricular refractory heart failure |
| NYHA functional class | Asymptomatic, no limitation of physical activity (NYHA I) | Symptoms occurring during ordinary physical activity Slight/moderate limitation of physical activity (NYHA II) | Symptoms occurring during minimal physical activity. Marked limitation of physical activity (NYHA III) | Symptoms occurring at rest. Unable to carry out any physical activity without discomfort (NYHA IV) Death |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Triposkiadis, F.; Xanthopoulos, A.; Bargiota, A.; Kitai, T.; Katsiki, N.; Farmakis, D.; Skoularigis, J.; Starling, R.C.; Iliodromitis, E. Diabetes Mellitus and Heart Failure. J. Clin. Med. 2021, 10, 3682. https://doi.org/10.3390/jcm10163682
Triposkiadis F, Xanthopoulos A, Bargiota A, Kitai T, Katsiki N, Farmakis D, Skoularigis J, Starling RC, Iliodromitis E. Diabetes Mellitus and Heart Failure. Journal of Clinical Medicine. 2021; 10(16):3682. https://doi.org/10.3390/jcm10163682
Chicago/Turabian StyleTriposkiadis, Filippos, Andrew Xanthopoulos, Alexandra Bargiota, Takeshi Kitai, Niki Katsiki, Dimitrios Farmakis, John Skoularigis, Randall C. Starling, and Efstathios Iliodromitis. 2021. "Diabetes Mellitus and Heart Failure" Journal of Clinical Medicine 10, no. 16: 3682. https://doi.org/10.3390/jcm10163682
APA StyleTriposkiadis, F., Xanthopoulos, A., Bargiota, A., Kitai, T., Katsiki, N., Farmakis, D., Skoularigis, J., Starling, R. C., & Iliodromitis, E. (2021). Diabetes Mellitus and Heart Failure. Journal of Clinical Medicine, 10(16), 3682. https://doi.org/10.3390/jcm10163682







