Flecainide in Ventricular Arrhythmias: From Old Myths to New Perspectives
Abstract
:1. Introduction
2. Epidemiology of Ventricular Arrhythmia
3. Mechanisms and Clinical Evaluation of Ventricular Arrhythmia
3.1. Pathogenesis
3.2. Clinical Presentation and Electrocardiographic Morphology
4. Flecainide Pharmacology
4.1. Pharmacodynamics
4.2. Pharmacokinetics
4.3. Controlled Release Flecainide
5. Guidelines
5.1. Ventricular Tachycardias in Structurally Normal Hearts
5.2. CPVT
5.3. Long QT Syndrome Type 3
5.4. Andersen-Tawil Syndrome (ATS)–LQTS 7
6. Flecainide: Evidence Gap and Future Perspective
6.1. Ischaemic Heart Disease
6.2. Non-Ischemic Structural Heart Disease
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AAD | Antiarrhythmic Drug |
| ACC | American College of Cardiology |
| AF | Atrial Fibrillation |
| AHA | American Heart Association |
| ARVC | Arrhythmogenic Right Ventricular Cardiomyopathy |
| BBRT | Bundle Branch Reentry Tachycardia |
| CAD | Coronary Artery Disease |
| CMR | Cardiac Magnetic Resonance |
| CPVT | Catecholaminergic Polymorphic Ventricular Tachycardia |
| ESC | European Society of Cardiology |
| ECG | Electrocardiogram |
| HRS | Heart Rhythm Society |
| IVA | Idiopathic Ventricular Arrhythmia |
| LBBB | Left Bundle Branch Block |
| LQTS | Long QT Syndrome |
| LV | Left Ventricle |
| LVOT | Left Ventricular Outflow Tract |
| MI | Myocardial Infarction |
| PCI | Percutaneous Coronary Intervention |
| PVC | Premature Ventricular Complex |
| RBBB | Right Bundle Branch Block |
| RVOT | Right Ventricular Outflow Tract |
| SCD | Sudden Cardiac Death |
| VT | Ventricular Tachycardia |
References
- Hudak, J.M.; Banitt, E.H.; Schmid, J.R. Discovery and Development of Flecainide. Am. J. Cardiol. 1984, 53, 17–20. [Google Scholar] [CrossRef]
- Hodges, M.; Haugland, J.M.; Granrud, G.; Conard, G.J.; Asinger, R.W.; Mikell, F.L.; Krejci, J. Suppression of Ventricular Ectopic Depolarizations by Flecainide Acetate, a New Antiarrhythmic Agent. Circulation 1982, 65, 879–885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nieuwlaat, R.; Capucci, A.; Camm, A.J.; Olsson, S.B.; Andresen, D.; Davies, D.W.; Cobbe, S.; Breithardt, G.; Le Heuzey, J.-Y.; Prins, M.H.; et al. Atrial Fibrillation Management: A Prospective Survey in ESC Member Countries: The Euro Heart Survey on Atrial Fibrillation. Eur. Heart J. 2005, 26, 2422–2434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lavalle, C.; Magnocavallo, M.; Straito, M.; Santini, L.; Forleo, G.B.; Grimaldi, M.; Badagliacca, R.; Lanata, L.; Ricci, R.P. Flecainide How and When: A Practical Guide in Supraventricular Arrhythmias. J. Clin. Med. 2021, 10, 1456. [Google Scholar] [CrossRef] [PubMed]
- Echt, D.S.; Liebson, P.R.; Mitchell, L.B.; Peters, R.W.; Obias-Manno, D.; Barker, A.H.; Arensberg, D.; Baker, A.; Friedman, L.; Greene, H.L. Mortality and Morbidity in Patients Receiving Encainide, Flecainide, or Placebo. The Cardiac Arrhythmia Suppression Trial. N. Engl. J. Med. 1991, 324, 781–788. [Google Scholar] [CrossRef]
- Priori, S.G.; Blomström-Lundqvist, C.; Mazzanti, A.; Blom, N.; Borggrefe, M.; Camm, J.; Elliott, P.M.; Fitzsimons, D.; Hatala, R.; Hindricks, G.; et al. 2015 ESC Guidelines for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur. Heart J. 2015, 36, 2793–2867. [Google Scholar] [CrossRef] [Green Version]
- Anderson, J.L.; Pratt, C.M.; Waldo, A.L.; Karagounis, L.A. Impact of the Food and Drug Administration Approval of Flecainide and Encainide on Coronary Artery Disease Mortality: Putting “Deadly Medicine” to the Test. Am. J. Cardiol. 1997, 79, 43–47. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; LaPointe, N.M.A.; Curtis, L.H.; Kramer, J.M.; Swann, J.; Honig, P.; Califf, R.M. Outpatient Prescribing of Antiarrhythmic Drugs from 1995 to 2000. Am. J. Cardiol. 2003, 91, 91–94. [Google Scholar] [CrossRef]
- Ruzieh, M.; Moroi, M.K.; Aboujamous, N.M.; Ghahramani, M.; Naccarelli, G.V.; Mandrola, J.; Foy, A.J. Meta-Analysis Comparing the Relative Risk of Adverse Events for Amiodarone Versus Placebo. Am. J. Cardiol. 2019, 124, 1889–1893. [Google Scholar] [CrossRef]
- Di Biase, L.; Romero, J.; Du, X.; Mohanty, S.; Trivedi, C.; Della Rocca, D.G.; Patel, K.; Sanchez, J.; Yang, R.; Alviz, I.; et al. Catheter Ablation of Ventricular Tachycardia in Ischemic Cardiomyopathy: Impact of Concomitant Amiodarone Therapy on Short- and Long-Term Clinical Outcomes. Heart Rhythm 2021, 18, 885–893. [Google Scholar] [CrossRef]
- Hyman, M.C.; Mustin, D.; Supple, G.; Schaller, R.D.; Santangeli, P.; Arkles, J.; Lin, D.; Muser, D.; Dixit, S.; Nazarian, S.; et al. Class IC Antiarrhythmic Drugs for Suspected Premature Ventricular Contraction–Induced Cardiomyopathy. Heart Rhythm 2018, 15, 159–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ermakov, S.; Gerstenfeld, E.P.; Svetlichnaya, Y.; Scheinman, M.M. Use of Flecainide in Combination Antiarrhythmic Therapy in Patients with Arrhythmogenic Right Ventricular Cardiomyopathy. Heart Rhythm 2017, 14, 564–569. [Google Scholar] [CrossRef]
- Ermakov, S.; Hoffmayer, K.S.; Gerstenfeld, E.P.; Scheinman, M.M. Combination Drug Therapy for Patients with Intractable Ventricular Tachycardia Associated with Right Ventricular Cardiomyopathy. Pacing Clin. Electrophysiol. 2014, 37, 90–94. [Google Scholar] [CrossRef]
- Della Rocca, D.G.; Santini, L.; Forleo, G.B.; Sanniti, A.; Del Prete, A.; Lavalle, C.; Di Biase, L.; Natale, A.; Romeo, F. Novel Perspectives on Arrhythmia-Induced Cardiomyopathy: Pathophysiology, Clinical Manifestations and an Update on Invasive Management Strategies. Cardiol. Rev. 2015, 23, 135–141. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Stevenson, W.G.; Ackerman, M.J.; Bryant, W.J.; Callans, D.J.; Curtis, A.B.; Deal, B.J.; Dickfeld, T.; Field, M.E.; Fonarow, G.C.; et al. 2017 AHA/ACC/HRS Guideline for Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation 2018, 138, e272–e391. [Google Scholar] [CrossRef] [Green Version]
- Lo, R.; Chia, K.K.M.; Hsia, H.H. Ventricular Tachycardia in Ischemic Heart Disease. Card. Electrophysiol. Clin. 2017, 9, 25–46. [Google Scholar] [CrossRef] [PubMed]
- Markman, T.M.; Nazarian, S. Treatment of Ventricular Arrhythmias: What’s New? Trends Cardiovasc. Med. 2019, 29, 249–261. [Google Scholar] [CrossRef]
- Hingorani, P.; Karnad, D.R.; Rohekar, P.; Kerkar, V.; Lokhandwala, Y.Y.; Kothari, S. Arrhythmias Seen in Baseline 24-Hour Holter ECG Recordings in Healthy Normal Volunteers During Phase 1 Clinical Trials. J. Clin. Pharm. 2016, 56, 885–893. [Google Scholar] [CrossRef] [Green Version]
- Latchamsetty, R.; Yokokawa, M.; Morady, F.; Kim, H.M.; Mathew, S.; Tilz, R.; Kuck, K.-H.; Nagashima, K.; Tedrow, U.; Stevenson, W.G.; et al. Multicenter Outcomes for Catheter Ablation of Idiopathic Premature Ventricular Complexes. JACC Clin. Electrophysiol. 2015, 1, 116–123. [Google Scholar] [CrossRef] [PubMed]
- Caceres, J.; Jazayeri, M.; McKinnie, J.; Avitall, B.; Denker, S.T.; Tchou, P.; Akhtar, M. Sustained Bundle Branch Reentry as a Mechanism of Clinical Tachycardia. Circulation 1989, 79, 256–270. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhatt, A.G.; Mittal, S. Ventricular Tachycardia in Structurally Normal Hearts. In Encyclopedia of Cardiovascular Research and Medicine; Elsevier: Cham, Switzerland, 2018; pp. 700–724. ISBN 978-0-12-805154-2. [Google Scholar]
- Wit, A.L. Cellular Electrophysiologic Mechanisms of Cardiac Arrhythmias. Cardiol. Clin. 1990, 8, 393–409. [Google Scholar] [CrossRef]
- Cabo, C.; Wit, A.L. Cellular Electrophysiologic Mechanisms of Cardiac Arrhythmias. Cardiol. Clin. 1997, 15, 517–538. [Google Scholar] [CrossRef]
- Flinders, D.C.; Roberts, S.D. Ventricular Arrhythmias. Prim. Care 2000, 27, 709–724;vii. [Google Scholar] [CrossRef]
- AlMahameed, S.T.; Ziv, O. Ventricular Arrhythmias. Med. Clin. N. Am. 2019, 103, 881–895. [Google Scholar] [CrossRef] [PubMed]
- Lerman, B.B.; Ip, J.E.; Shah, B.K.; Thomas, G.; Liu, C.F.; Ciaccio, E.J.; Wit, A.L.; Cheung, J.W.; Markowitz, S.M. Mechanism-Specific Effects of Adenosine on Ventricular Tachycardia. J. Cardiovasc. Electrophysiol. 2014, 25, 1350–1358. [Google Scholar] [CrossRef] [PubMed]
- Tschabrunn, C.M.; Roujol, S.; Nezafat, R.; Faulkner-Jones, B.; Buxton, A.E.; Josephson, M.E.; Anter, E. A Swine Model of Infarct-Related Reentrant Ventricular Tachycardia: Electroanatomic, Magnetic Resonance, and Histopathological Characterization. Heart Rhythm 2016, 13, 262–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhaskaran, A.; De Silva, K.; Rao, K.; Campbell, T.; Trivic, I.; Bennett, R.G.; Kizana, E.; Kumar, S. Ventricular Tachycardia Ablation in Non-Ischemic Cardiomyopathy. Korean Circ. J. 2020, 50, 203–219. [Google Scholar] [CrossRef]
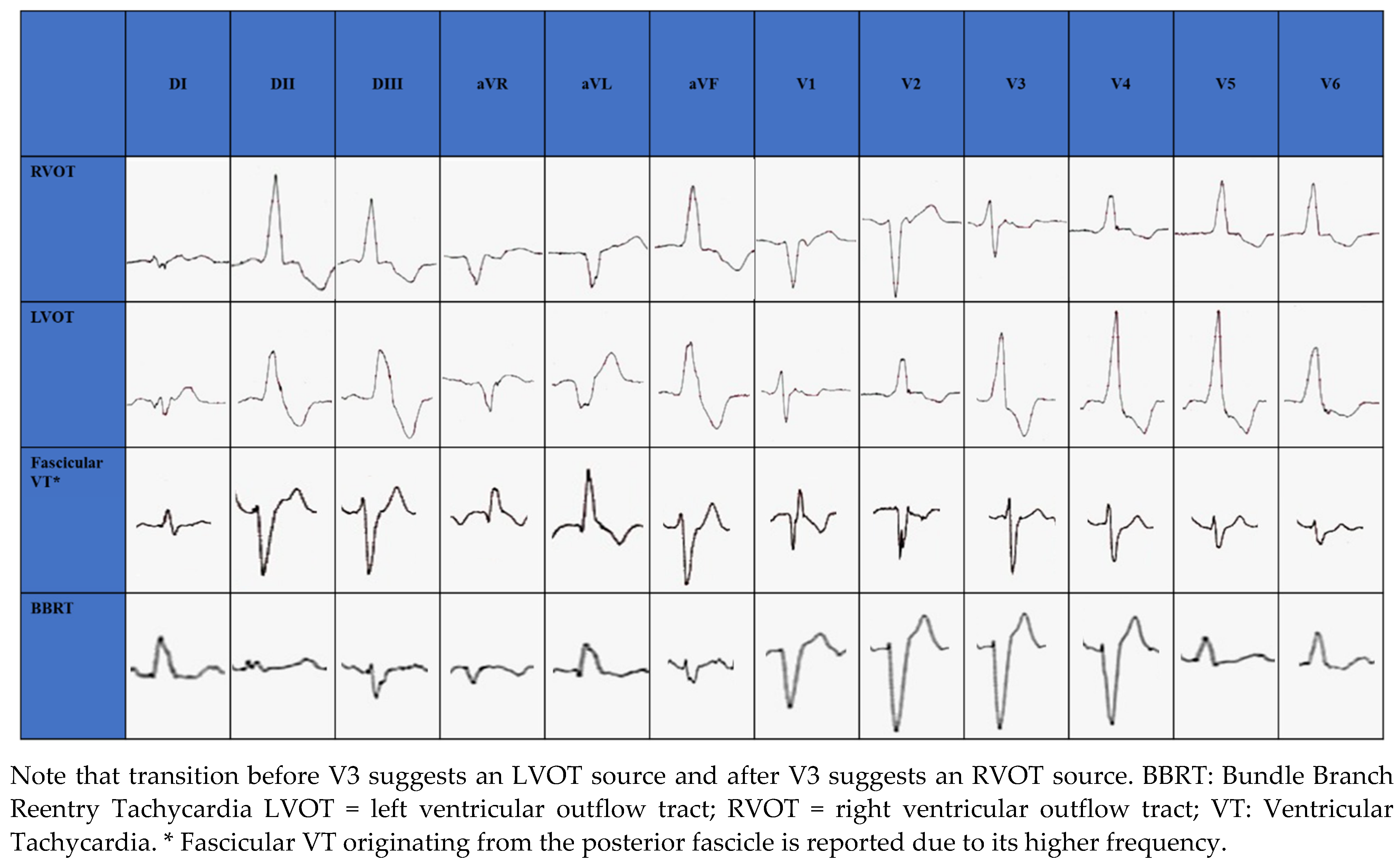
- Lavalle, C.; Mariani, M.V.; Piro, A.; Straito, M.; Severino, P.; Della Rocca, D.G.; Forleo, G.B.; Romero, J.; Di Biase, L.; Fedele, F. Electrocardiographic Features, Mapping and Ablation of Idiopathic Outflow Tract Ventricular Arrhythmias. J. Interv. Card. Electrophysiol. 2020, 57, 207–218. [Google Scholar] [CrossRef]
- Park, K.-M.; Kim, Y.-H.; Marchlinski, F.E. Using the Surface Electrocardiogram to Localize the Origin of Idiopathic Ventricular Tachycardia. Pacing Clin. Electrophysiol. 2012, 35, 1516–1527. [Google Scholar] [CrossRef]
- Della Rocca, D.G.; Gianni, C.; Mohanty, S.; Trivedi, C.; Di Biase, L.; Natale, A. Localization of Ventricular Arrhythmias for Catheter Ablation: The Role of Surface Electrocardiogram. Card. Electrophysiol. Clin. 2018, 10, 333–354. [Google Scholar] [CrossRef]
- Di Biase, L.; Romero, J.; Zado, E.S.; Diaz, J.C.; Gianni, C.; Hranitzki, P.M.; Sanchez, J.E.; Mohanty, S.; Al-Ahmad, A.; Mohanty, P.; et al. Variant of Ventricular Outflow Tract Ventricular Arrhythmias Requiring Ablation from Multiple Sites: Intramural Origin. Heart Rhythm 2019, 16, 724–732. [Google Scholar] [CrossRef] [PubMed]
- Betensky, B.P.; Park, R.E.; Marchlinski, F.E.; Hutchinson, M.D.; Garcia, F.C.; Dixit, S.; Callans, D.J.; Cooper, J.M.; Bala, R.; Lin, D.; et al. The V(2) Transition Ratio: A New Electrocardiographic Criterion for Distinguishing Left from Right Ventricular Outflow Tract Tachycardia Origin. J. Am. Coll. Cardiol. 2011, 57, 2255–2262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Q.; Xu, J.; Gianni, C.; Trivedi, C.; Della Rocca, D.G.; Bassiouny, M.; Canpolat, U.; Tapia, A.C.; Burkhardt, J.D.; Sanchez, J.E.; et al. Simple Electrocardiographic Criteria for Rapid Identification of Wide QRS Complex Tachycardia: The New Limb Lead Algorithm. Heart Rhythm 2020, 17, 431–438. [Google Scholar] [CrossRef]
- Dukkipati, S.R.; Koruth, J.S.; Choudry, S.; Miller, M.A.; Whang, W.; Reddy, V.Y. Catheter Ablation of Ventricular Tachycardia in Structural Heart Disease: Indications, Strategies, and Outcomes-Part II. J. Am. Coll. Cardiol. 2017, 70, 2924–2941. [Google Scholar] [CrossRef]
- Sung, R.K.; Boyden, P.A.; Scheinman, M. Cellular Physiology and Clinical Manifestations of Fascicular Arrhythmias in Normal Hearts. JACC Clin. Electrophysiol. 2017, 3, 1343–1355. [Google Scholar] [CrossRef]
- Sung, R.K.; Kim, A.M.; Tseng, Z.H.; Han, F.; Inada, K.; Tedrow, U.B.; Viswanathan, M.N.; Badhwar, N.; Varosy, P.D.; Tanel, R.; et al. Diagnosis and Ablation of Multiform Fascicular Tachycardia. J. Cardiovasc. Electrophysiol. 2013, 24, 297–304. [Google Scholar] [CrossRef]
- Josephson, M.A.; Ikeda, N.; Singh, B.N. Effects of Flecainide on Ventricular Function: Clinical and Experimental Correlations. Am. J. Cardiol. 1984, 53, 95–100. [Google Scholar] [CrossRef]
- Anno, T.; Hondeghem, L.M. Interactions of Flecainide with Guinea Pig Cardiac Sodium Channels. Importance of Activation Unblocking to the Voltage Dependence of Recovery. Circ. Res. 1990, 66, 789–803. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Follmer, C.H.; Colatsky, T.J. Block of Delayed Rectifier Potassium Current, IK, by Flecainide and E-4031 in Cat Ventricular Myocytes. Circulation 1990, 82, 289–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Padfield, G.J.; AlAhmari, L.; Lieve, K.V.V.; AlAhmari, T.; Roston, T.M.; Wilde, A.A.; Krahn, A.D.; Sanatani, S. Flecainide Monotherapy Is an Option for Selected Patients with Catecholaminergic Polymorphic Ventricular Tachycardia Intolerant of β-Blockade. Heart Rhythm 2016, 13, 609–613. [Google Scholar] [CrossRef]
- Hilliard, F.A.; Steele, D.S.; Laver, D.; Yang, Z.; Le Marchand, S.J.; Chopra, N.; Piston, D.W.; Huke, S.; Knollmann, B.C. Flecainide Inhibits Arrhythmogenic Ca2+ Waves by Open State Block of Ryanodine Receptor Ca2+ Release Channels and Reduction of Ca2+ Spark Mass. J. Mol. Cell. Cardiol. 2010, 48, 293–301. [Google Scholar] [CrossRef] [Green Version]
- Belardinelli, L.; Giles, W.R.; Rajamani, S.; Karagueuzian, H.S.; Shryock, J.C. Cardiac Late Na+ Current: Proarrhythmic Effects, Roles in Long QT Syndromes, and Pathological Relationship to CaMKII and Oxidative Stress. Heart Rhythm 2015, 12, 440–448. [Google Scholar] [CrossRef]
- Holmes, B.; Heel, R.C. A Preliminary Review of Its Pharmacodynamic Properties and Therapeutic efficiancy. Drugs 1985, 29, 1–33. [Google Scholar] [CrossRef] [PubMed]
- Roden, D.M.; Woosley, R.L. Drug Therapy. Flecainide. N. Engl. J. Med. 1986, 315, 36–41. [Google Scholar] [CrossRef]
- Crijns, H.J.; van Gelder, I.C.; Lie, K.I. Supraventricular Tachycardia Mimicking Ventricular Tachycardia during Flecainide Treatment. Am. J. Cardiol. 1988, 62, 1303–1306. [Google Scholar] [CrossRef]
- Boriani, G.; Diemberger, I.; Biffi, M.; Martignani, C.; Branzi, A. Pharmacological Cardioversion of Atrial Fibrillation: Current Management and Treatment Options. Drugs 2004, 64, 2741–2762. [Google Scholar] [CrossRef] [PubMed]
- Gentzkow, G.D.; Sullivan, J.Y. Extracardiac Adverse Effects of Flecainide. Am. J. Cardiol. 1984, 53, 101–105. [Google Scholar] [CrossRef]
- Conard, G.J.; Ober, R.E. Metabolism of Flecainide. Am. J. Cardiol. 1984, 53, 41–51. [Google Scholar] [CrossRef]
- Tjandra-Maga, T.; Verbesselt, R.; Hecken, A.; Mullie, A.; Schepper, P. Flecainide: Single and Multiple Oral Dose Kinetics, Absolute Bioavailability and Effect of Food and Antacid in Man. Br. J. Clin. Pharmacol. 1986, 22, 309–316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, S.-F. Polymorphism of Human Cytochrome P450 2D6 and Its Clinical Significance: Part I. Clin. Pharmacokinet. 2009, 48, 689–723. [Google Scholar] [CrossRef] [PubMed]
- Doki, K.; Homma, M.; Kuga, K.; Aonuma, K.; Kohda, Y. SCN5A Promoter Haplotype Affects the Therapeutic Range for Serum Flecainide Concentration in Asian Patients. Pharm. Genom. 2013, 23, 349–354. [Google Scholar] [CrossRef] [Green Version]
- Aliot, E.; Capucci, A.; Crijns, H.J.; Goette, A.; Tamargo, J. Twenty-Five Years in the Making: Flecainide Is Safe and Effective for the Management of Atrial Fibrillation. Europace 2011, 13, 161–173. [Google Scholar] [CrossRef]
- Tamargo, J.; Capucci, A.; Mabo, P. Safety of Flecainide. Drug Saf. 2012, 35, 273–289. [Google Scholar] [CrossRef]
- Shea, P.; Lal, R.; Kim, S.S.; Schechtman, K.; Ruffy, R. Flecainide and Amiodarone Interaction. J. Am. Coll. Cardiol. 1986, 7, 1127–1130. [Google Scholar] [CrossRef] [Green Version]
- Meda Pharmaceuticals Ltd. Flecainide Acetate—Summary of Product Characteristics (UK). 2013. Available online: www.Medicines.Org.Uk/Emc/Medicine/3905 (accessed on 17 August 2014).
- Lim, K.S.; Cho, J.-Y.; Jang, I.-J.; Kim, B.-H.; Kim, J.; Jeon, J.-Y.; Tae, Y.-M.; Yi, S.; Eum, S.; Shin, S.-G.; et al. Pharmacokinetic Interaction of Flecainide and Paroxetine in Relation to the CYP2D6*10 Allele in Healthy Korean Subjects. Br. J. Clin. Pharm. 2008, 66, 660–666. [Google Scholar] [CrossRef] [Green Version]
- Nemeroff, C.B.; DeVane, C.L.; Pollock, B.G. Newer Antidepressants and the Cytochrome P450 System. Am. J. Psychiatry 1996, 153, 311–320. [Google Scholar] [CrossRef] [PubMed]
- Coumel, P.; Maison-Blanche, P.; Tarral, E.; Périer, A.; Milliez, P.; Leenhardt, A. Pharmacodynamic Equivalence of Two Flecainide Acetate Formulations in Patients with Paroxysmal Atrial Fibrillation by QRS Analysis of Ambulatory Electrocardiogram. J. Cardiovasc. Pharmacol. 2003, 41, 771–779. [Google Scholar] [CrossRef]
- Tarantino, N.; Della Rocca, D.; De Leon De La Cruz, N.; Manheimer, E.; Magnocavallo, M.; Lavalle, C.; Gianni, C.; Mohanty, S.; Trivedi, C.; Al-Ahmad, A.; et al. Catheter Ablation of Life-Threatening Ventricular Arrhythmias in Athletes. Medicina 2021, 57, 205. [Google Scholar] [CrossRef] [PubMed]
- Kannankeril, P.J.; Moore, J.P.; Cerrone, M.; Priori, S.G.; Kertesz, N.J.; Ro, P.S.; Batra, A.S.; Kaufman, E.S.; Fairbrother, D.L.; Saarel, E.V.; et al. Efficacy of Flecainide in the Treatment of Catecholaminergic Polymorphic Ventricular Tachycardia: A Randomized Clinical Trial. JAMA Cardiol. 2017, 2, 759–766. [Google Scholar] [CrossRef] [Green Version]
- Khoury, A.; Marai, I.; Suleiman, M.; Blich, M.; Lorber, A.; Gepstein, L.; Boulos, M. Flecainide Therapy Suppresses Exercise-Induced Ventricular Arrhythmias in Patients with CASQ2-Associated Catecholaminergic Polymorphic Ventricular Tachycardia. Heart Rhythm 2013, 10, 1671–1675. [Google Scholar] [CrossRef]
- Watanabe, H.; van der Werf, C.; Roses-Noguer, F.; Adler, A.; Sumitomo, N.; Veltmann, C.; Rosso, R.; Bhuiyan, Z.A.; Bikker, H.; Kannankeril, P.J.; et al. Effects of Flecainide on Exercise-Induced Ventricular Arrhythmias and Recurrences in Genotype-Negative Patients with Catecholaminergic Polymorphic Ventricular Tachycardia. Heart Rhythm 2013, 10, 542–547. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wangüemert Pérez, F.; Hernández Afonso, J.S.; Groba Marco, M.D.V.; Caballero Dorta, E.; Álvarez Acosta, L.; Campuzano Larrea, O.; Pérez, G.; Brugada Terradellas, J.; Brugada Terradellas, R. Flecainide Reduces Ventricular Arrhythmias in Patients With Genotype RyR2-Positive Catecholaminergic Polymorphic Ventricular Tachycardia. Rev. Esp. Cardiol. 2018, 71, 185–191. [Google Scholar] [CrossRef]
- Hwang, H.S.; Baldo, M.P.; Rodriguez, J.P.; Faggioni, M.; Knollmann, B.C. Efficacy of Flecainide in Catecholaminergic Polymorphic Ventricular Tachycardia Is Mutation-Independent but Reduced by Calcium Overload. Front. Physiol. 2019, 10, 992. [Google Scholar] [CrossRef] [Green Version]
- Chorin, E.; Taub, R.; Medina, A.; Flint, N.; Viskin, S.; Benhorin, J. Long-Term Flecainide Therapy in Type 3 Long QT Syndrome. EP Eur. 2018, 20, 370–376. [Google Scholar] [CrossRef]
- Miyamoto, K.; Aiba, T.; Kimura, H.; Hayashi, H.; Ohno, S.; Yasuoka, C.; Tanioka, Y.; Tsuchiya, T.; Yoshida, Y.; Hayashi, H.; et al. Efficacy and Safety of Flecainide for Ventricular Arrhythmias in Patients with Andersen-Tawil Syndrome with KCNJ2 Mutations. Heart Rhythm 2015, 12, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Baranchuk, A.; Morillo, C.A.; Thoenes, M.; Ventura, R.; Connolly, S.J. Current Role of Medical Therapy for Prevention or Termination of Atrial Fibrillation. In Atrial Fibrillation; Natale, A., Jalife, J., Eds.; Humana Press: Totowa, NJ, USA, 2008; pp. 185–195. ISBN 978-1-58829-856-0. [Google Scholar]
- Akiyama, T.; Pawitan, Y.; Greenberg, H.; Kuo, C.-S.; Reynolds-Haertle, R.A. The CAST Investigators Increased Risk of Death and Cardiac Arrest from Encainide and Flecainide in Patients after Non-Q-Wave Acute Myocardial Infarction in the Cardiac Arrhythmia Suppression Trial. Am. J. Cardiol. 1991, 68, 1551–1555. [Google Scholar] [CrossRef]
- Meinertz, T.; Lip, G.Y.H.; Lombardi, F.; Sadowski, Z.P.; Kalsch, B.; Camez, A.; Hewkin, A.; Eberle, S. Efficacy and Safety of Propafenone Sustained Release in the Prophylaxis of Symptomatic Paroxysmal Atrial Fibrillation (The European Rythmol/Rytmonorm Atrial Fibrillation Trial [ERAFT] Study). Am. J. Cardiol. 2002, 90, 1300–1306. [Google Scholar] [CrossRef]
- Pantlin, P.G.; Bober, R.M.; Bernard, M.L.; Khatib, S.; Polin, G.M.; Rogers, P.A.; Morin, D.P. Class 1C Antiarrhythmic Drugs in Atrial Fibrillation and Coronary Artery Disease. J. Cardiovasc. Electrophysiol. 2020, 31, 607–611. [Google Scholar] [CrossRef] [Green Version]
- Ashraf, H.; Ko, N.K.; Ladia, V.; Agasthi, P.; Prendiville, T.; O’Herlihy, F.; Pujari, S.H.; Mulpuru, S.K.; Scott, L.; Sorajja, D. Use of Flecainide in Stable Coronary Artery Disease: An Analysis of Its Safety in Both Nonobstructive and Obstructive Coronary Artery Disease. Am. J. Cardiovasc. Drugs 2021, 1–10. [Google Scholar] [CrossRef]
- Tilz, R.R.; Lenarczyk, R.; Scherr, D.; Haugaa, K.H.; Iliodromitis, K.; Pürerfellner, H.; Kiliszek, M.; Dagres, N. Management of Ventricular Tachycardia in the Ablation Era: Results of the European Heart Rhythm Association Survey. EP Eur. 2018, 20, 209–213. [Google Scholar] [CrossRef]
- Chung, R.; Houghtaling, P.L.; Tchou, M.; Niebauer, M.J.; Lindsay, B.D.; Tchou, P.J.; Chung, M.K. Left Ventricular Hypertrophy and Antiarrhythmic Drugs in Atrial Fibrillation: Impact on Mortality: LVH, Antiarrhythmic Drugs, and Mortality. Pacing Clin. Electrophysiol. 2014, 37, 1338–1348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haruki, S.; Minami, Y.; Suzuki, A.; Hagiwara, N. Effects of Flecainide on Left Ventricular Pressure Gradient and Symptoms in Obstructive Hypertrophic Cardiomyopathy: A Comparison of Flecainide and Disopyramide. Heart Vessel. 2015, 30, 604–610. [Google Scholar] [CrossRef] [PubMed]
- Andreini, D.; Dello Russo, A.; Pontone, G.; Mushtaq, S.; Conte, E.; Perchinunno, M.; Guglielmo, M.; Coutinho Santos, A.; Magatelli, M.; Baggiano, A.; et al. CMR for Identifying the Substrate of Ventricular Arrhythmia in Patients With Normal Echocardiography. JACC Cardiovasc. Imaging 2020, 13, 410–421. [Google Scholar] [CrossRef] [PubMed]



| Origin of VT/PVC | Treatment Recommended | COR | LEO |
|---|---|---|---|
| RVOT | Primary Catheter Ablation preferred to Class IC | I | B |
| LVOT/Aortic Cusp/Epicardial | Class IC first line | I | C |
| Catheter Ablation after drug failure | IIA | B | |
| Idiopathic Left VT | Catheter Ablation first line | I | B |
| Class IC, beta blockers, verapamil alternative | I | C | |
| Papillary muscle | Class IC, beta blockers, verapamil first line | I | C |
| Catheter Ablation after drug failure | IIA | B | |
| Mitral and Tricuspid anulus | Class IC, beta blockers, verapamil first line | I | C |
| Catheter Ablation after drug failure | IIA | B | |
| Children with RVOT/LVOT | Class IC alternative to beta blockers/verapamil | IIA | C |
| Catheter Ablation after drug failure if >5 years | IIA | B | |
| CPVT | Flecainide should be added to betablockers in case of recurrent syncope or bidirectional VT | IIA * I ** | C B-NR |
| Flecainide should be added to betablockers to reduce ICD appropriate shocks | IIA | C | |
| LQTS type 3 | Sodium channel blockers (flecainide, mexiletine, ranolazine) as add-on to shorten QTc > 500 ms | IIB | C |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lavalle, C.; Trivigno, S.; Vetta, G.; Magnocavallo, M.; Mariani, M.V.; Santini, L.; Forleo, G.B.; Grimaldi, M.; Badagliacca, R.; Lanata, L.; et al. Flecainide in Ventricular Arrhythmias: From Old Myths to New Perspectives. J. Clin. Med. 2021, 10, 3696. https://doi.org/10.3390/jcm10163696
Lavalle C, Trivigno S, Vetta G, Magnocavallo M, Mariani MV, Santini L, Forleo GB, Grimaldi M, Badagliacca R, Lanata L, et al. Flecainide in Ventricular Arrhythmias: From Old Myths to New Perspectives. Journal of Clinical Medicine. 2021; 10(16):3696. https://doi.org/10.3390/jcm10163696
Chicago/Turabian StyleLavalle, Carlo, Sara Trivigno, Giampaolo Vetta, Michele Magnocavallo, Marco Valerio Mariani, Luca Santini, Giovanni Battista Forleo, Massimo Grimaldi, Roberto Badagliacca, Luigi Lanata, and et al. 2021. "Flecainide in Ventricular Arrhythmias: From Old Myths to New Perspectives" Journal of Clinical Medicine 10, no. 16: 3696. https://doi.org/10.3390/jcm10163696
APA StyleLavalle, C., Trivigno, S., Vetta, G., Magnocavallo, M., Mariani, M. V., Santini, L., Forleo, G. B., Grimaldi, M., Badagliacca, R., Lanata, L., & Ricci, R. P. (2021). Flecainide in Ventricular Arrhythmias: From Old Myths to New Perspectives. Journal of Clinical Medicine, 10(16), 3696. https://doi.org/10.3390/jcm10163696









