The Impact of Suture Button Removal in Syndesmosis Fixation
Abstract
:1. Introduction
2. Methods
2.1. Subjects
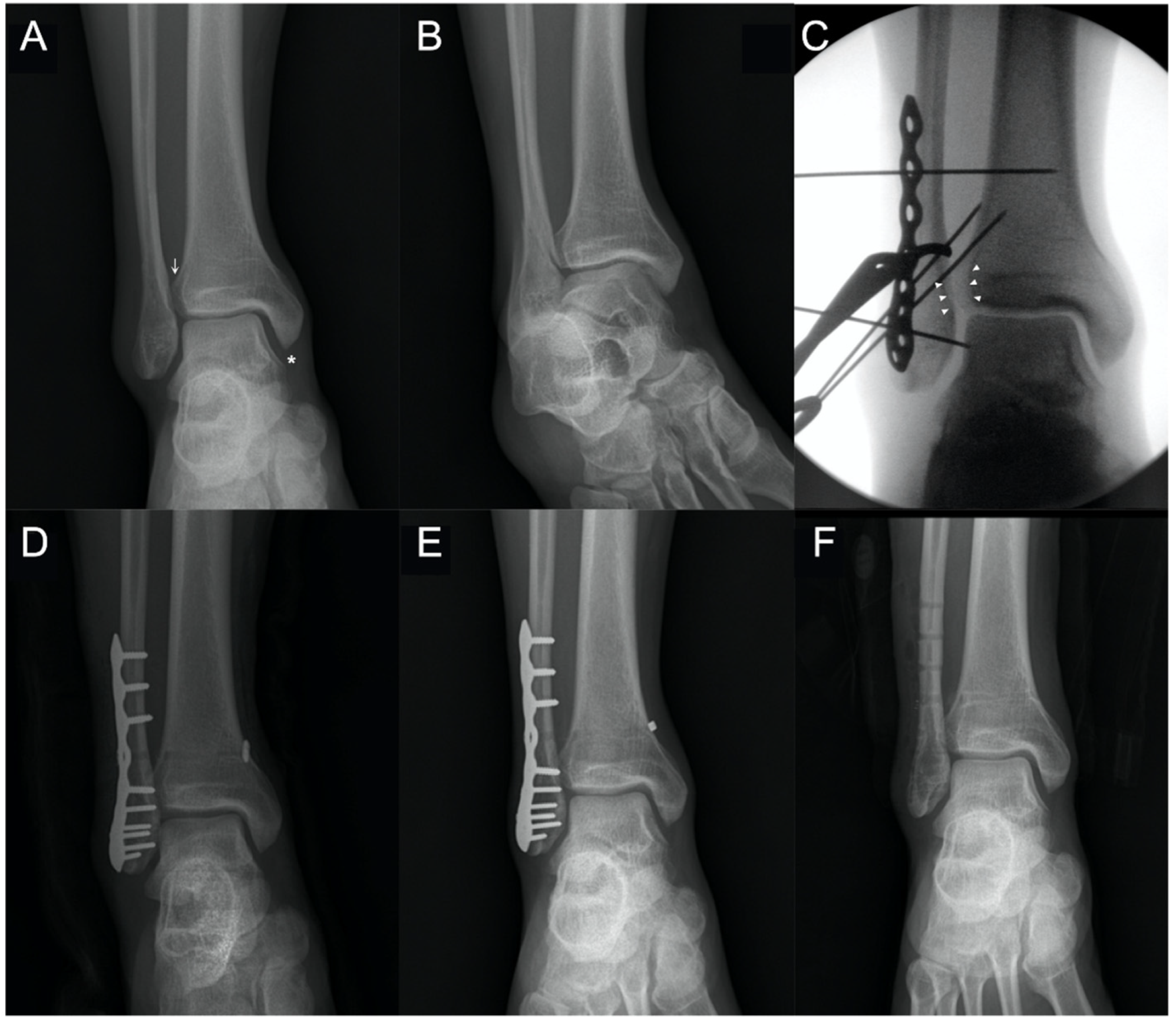
2.2. Surgical Technique
2.3. Postoperative Management
2.4. Removal of Suture Button
2.5. Radiographic Analysis
2.6. Computed Tomography (CT) Analysis
2.7. Clinical Analysis
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dattani, R.; Patnaik, S.; Kantak, A.; Srikanth, B.; Selvan, T. Injuries to the tibiofibular syndesmosis. J. Bone Jt. Surgery. Br. Vol. 2008, 90, 405–410. [Google Scholar] [CrossRef] [Green Version]
- Schepers, T. Acute distal tibiofibular syndesmosis injury: A systematic review of suture-button versus syndesmotic screw repair. Int Orthop. 2012, 36, 1199–1206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schepers, T.; Van Lieshout, E.M.; de Vries, M.R.; Van der Elst, M. Complications of syndesmotic screw removal. Foot Ankle Int. 2011, 32, 1040–1044. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hsu, Y.-T.; Wu, C.-C.; Lee, W.-C.; Fan, K.-F.; Tseng, I.-C.; Lee, P.-C. Surgical treatment of syndesmotic diastasis: Emphasis on effect of syndesmotic screw on ankle function. Int. Orthop. 2011, 35, 359–364. [Google Scholar] [CrossRef] [Green Version]
- Lalli, T.A.; Matthews, L.J.; Hanselman, A.E.; Hubbard, D.F.; Bramer, M.A.; Santrock, R.D. Economic impact of syndesmosis hardware removal. Foot 2015, 25, 131–133. [Google Scholar] [CrossRef] [PubMed]
- Song, D.J.; Lanzi, J.T.; Groth, A.T.; Drake, M.; Orchowski, J.R.; Shaha, S.H.; Lindell, K.K. The Effect of Syndesmosis Screw Removal on the Reduction of the Distal Tibiofibular Joint: A Prospective Radiographic Study. Foot Ankle Int. 2014, 35, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Baek, J.H.; Kim, T.Y.; Kwon, Y.B.; Jeong, B.O. Radiographic change of the distal tibiofibular joint following removal of transfixing screw fixation. Foot Ankle Int. 2018, 39, 318–325. [Google Scholar] [CrossRef]
- Thornes, B.; Shannon, F.; Guiney, A.-M.; Hession, P.; Masterson, E. Suture-button syndesmosis fixation: Accelerated rehabilitation and improved outcomes. Clin. Orthop. Relat. Res. 2005, 431, 207–212. [Google Scholar] [CrossRef]
- Clanton, T.O.; Whitlow, S.R.; Williams, B.T.; Liechti, D.J.; Backus, J.D.; Dornan, G.J.; Saroki, A.J.; Turnbull, T.L.; LaPrade, R.F. Biomechanical comparison of 3 current ankle syndesmosis repair techniques. Foot Ankle Int. 2017, 38, 200–207. [Google Scholar] [CrossRef]
- Lee, J.S.; Curnutte, B.; Pan, K.; Liu, J.; Ebraheim, N.A. Biomechanical Comparison of Suture-Button, Bioabsorbable Screw, and Metal Screw for Ankle Syndesmotic Repair: A Meta-Analysis. Foot Ankle Surg. 2020, 27, 117–122. [Google Scholar] [CrossRef]
- Andersen, M.R.; Frihagen, F.; Hellund, J.C.; Madsen, J.E.; Figved, W. Randomized trial comparing suture button with single syndesmotic screw for syndesmosis injury. JBJS 2018, 100, 2–12. [Google Scholar] [CrossRef]
- Willmott, H.; Singh, B.; David, L. Outcome and complications of treatment of ankle diastasis with tightrope fixation. Injury 2009, 40, 1204–1206. [Google Scholar] [CrossRef]
- Seyhan, M.; Donmez, F.; Mahirogullari, M.; Cakmak, S.; Mutlu, S.; Guler, O. Comparison of screw fixation with elastic fixation methods in the treatment of syndesmosis injuries in ankle fractures. Injury 2015, 46, S19–S23. [Google Scholar] [CrossRef]
- Gadd, R.; Storey, P.; Davies, M.; Blundell, C. Ankle Tightrope Syndesmosis Fixation: A Review of 38 Cases. In Orthopaedic Proceedings; The British Editorial Society of Bone & Joint Surgery: London, UK, 2011; Volume 93-B, p. 480. [Google Scholar]
- McMurray, D.; Hornung, B.; Venkateswaran, B.; Ali, Z. Walking on a tightrope: Our experience in the treatment of traumatic ankle syndesmosis rupture. Inj. Extra 2008, 5, 182. [Google Scholar] [CrossRef]
- Stoffel, K.; Wysocki, D.; Baddour, E.; Nicholls, R.; Yates, P. Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis: A cadaveric study. JBJS 2009, 91, 2646–2652. [Google Scholar] [CrossRef]
- Brage, M.E.; Bennett, C.R.; Whitehurst, J.B.; Getty, P.J.; Toledano, A. Observer reliability in ankle radiographic measurements. Foot Ankle Int. 1997, 18, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Sclafani, S. Ligamentous injury of the lower tibiofibular syndesmosis: Radiographic evidence. Radiology 1985, 156, 21–27. [Google Scholar] [CrossRef]
- Beumer, A.; Van Hemert, W.; Niesing, R.; Entius, C.; Ginai, A.; Mulder, P.; Swierstra, B. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clin. Orthop. Relat. Res. 2004, 423, 227–234. [Google Scholar] [CrossRef]
- Laflamme, M.; Belzile, E.L.; Bédard, L.; van den Bekerom, M.P.; Glazebrook, M.; Pelet, S. A prospective randomized multicenter trial comparing clinical outcomes of patients treated surgically with a static or dynamic implant for acute ankle syndesmosis rupture. J. Orthop. Trauma 2015, 29, 216–223. [Google Scholar] [CrossRef]
- Jordan, T.H.; Talarico, R.H.; Schuberth, J.M. The radiographic fate of the syndesmosis after trans-syndesmotic screw removal in displaced ankle fractures. J. Foot Ankle Surg. 2011, 50, 407–412. [Google Scholar] [CrossRef]
- Elgafy, H.; Semaan, H.B.; Blessinger, B.; Wassef, A.; Ebraheim, N.A. Computed tomography of normal distal tibiofibular syndesmosis. Skelet. Radiol. 2010, 39, 559–564. [Google Scholar] [CrossRef]
- Pelton, K.; Thordarson, D.B.; Barnwell, J. Open versus closed treatment of the fibula in Maissoneuve injuries. Foot Ankle Int. 2010, 31, 604–608. [Google Scholar] [CrossRef]
- Nimick, C.J.; Collman, D.R.; Lagaay, P. Fixation orientation in ankle fractures with syndesmosis injury. J. Foot Ankle Surg. 2013, 52, 315–318. [Google Scholar] [CrossRef]
- Colcuc, C.; Blank, M.; Stein, T.; Raimann, F.; Weber-Spickschen, S.; Fischer, S.; Hoffmann, R. Lower complication rate and faster return to sports in patients with acute syndesmotic rupture treated with a new knotless suture button device. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3156–3164. [Google Scholar] [CrossRef]
- Anand, A.; Wei, R.; Patel, A.; Vedi, V.; Allardice, G.; Anand, B.S. Tightrope fixation of syndesmotic injuries in Weber C ankle fractures: A multicentre case series. Eur. J. Orthop. Surg. Traumatol. 2017, 27, 461–467. [Google Scholar] [CrossRef]
- Bondi, M.; Rossi, N.; Pizzoli, A.; Brivio, L.R. The use of TightRope fixation for ankle syndesmosis injuries: Our experience. Musculoskelet. Surg. 2016, 100, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Coetzee, J.C.; Ebeling, P. Treatment of syndesmosis disruptions with TightRope fixation. Tech. Foot Ankle Surg. 2008, 7, 196–202. [Google Scholar] [CrossRef] [Green Version]
- DeGroot, H.; Al-Omari, A.A.; Ghazaly, S.A.E. Outcomes of suture button repair of the distal tibiofibular syndesmosis. Foot Ankle Int. 2011, 32, 250–256. [Google Scholar] [CrossRef]
- Qamar, F.; Kadakia, A.; Venkateswaran, B. An anatomical way of treating ankle syndesmotic injuries. J. Foot Ankle Surg. 2011, 50, 762–765. [Google Scholar] [CrossRef]
- Treon, K.; Beastall, J.; Kumar, K.; Hope, M. Complications of ankle syndesmosis stabilisation using a tightrope. In Orthopaedic Proceedings; The British Editorial Society of Bone & Joint Surgery: London, UK, 2011; Volume 93-B, p. 62. [Google Scholar]
- Naqvi, G.A.; Cunningham, P.; Lynch, B.; Galvin, R.; Awan, N. Fixation of ankle syndesmotic injuries: Comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am. J. Sports Med. 2012, 40, 2828–2835. [Google Scholar] [CrossRef]
- Kocadal, O.; Yucel, M.; Pepe, M.; Aksahin, E.; Aktekin, C.N. Evaluation of Reduction Accuracy of Suture-Button and Screw Fixation Techniques for Syndesmotic Injuries. Foot Ankle Int. 2016, 37, 1317–1325. [Google Scholar] [CrossRef] [PubMed]
- Rigby, R.B.; Cottom, J.M. Does the Arthrex TightRope(R) provide maintenance of the distal tibiofibular syndesmosis? A 2-year follow-up of 64 TightRopes(R) in 37 patients. J. Foot Ankle Surg. 2013, 52, 563–567. [Google Scholar] [CrossRef]
- Kortekangas, T.; Savola, O.; Flinkkila, T.; Lepojarvi, S.; Nortunen, S.; Ohtonen, P.; Katisko, J.; Pakarinen, H. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury 2015, 46, 1119–1126. [Google Scholar] [CrossRef] [PubMed]
- Maempel, J.; Ward, A.; Chesser, T.; Kelly, M. Use of tightrope fixation in ankle syndesmotic injuries. Chin. J. Traumatol. 2014, 17, 8–11. [Google Scholar] [PubMed]
- Westermann, R.W.; Rungprai, C.; Goetz, J.E.; Femino, J.; Amendola, A.; Phisitkul, P. The effect of suture-button fixation on simulated syndesmotic malreduction: A cadaveric study. J. Bone Jt. Surg. Am. 2014, 96, 1732–1738. [Google Scholar] [CrossRef] [PubMed]
- Peterson, K.S.; Chapman, W.D.; Hyer, C.F.; Berlet, G.C. Maintenance of reduction with suture button fixation devices for ankle syndesmosis repair. Foot Ankle Int. 2015, 36, 679–684. [Google Scholar] [CrossRef]
- Shimozono, Y.; Hurley, E.T.; Myerson, C.L.; Murawski, C.D.; Kennedy, J.G. Suture button versus syndesmotic screw for syndesmosis injuries: A meta-analysis of randomized controlled trials. Am. J. Sports Med. 2019, 47, 2764–2771. [Google Scholar] [CrossRef]
- Storey, P.; Gadd, R.J.; Blundell, C.; Davies, M.B. Complications of suture button ankle syndesmosis stabilization with modifications of surgical technique. Foot Ankle Int. 2012, 33, 717–721. [Google Scholar] [CrossRef]





| Patient No. | Age (Years) | Sex | Fracture Pattern | SB Removal (Months) | FU (Months) |
|---|---|---|---|---|---|
| 1 | 25 | M | SER (LM, PM) | 12 | 15 |
| 2 | 26 | M | Isolated | 13 | 16 |
| 3 | 24 | M | SER (LM) | 8 | 12 |
| 4 | 25 | M | Maisonneuve | 12 | 15 |
| 5 | 25 | M | SER (LM) | 12 | 15 |
| 6 | 24 | M | Maisonneuve (MM) | 12 | 15 |
| 7 | 27 | M | PER (LM) | 12 | 18 |
| 8 | 22 | M | PER (LM, MM, PM) | 12 | 15 |
| 9 | 24 | M | PER (LM) | 12 | 15 |
| 10 | 22 | M | SER (LM) | 12 | 15 |
| 11 | 24 | M | Maisonneuve (MM) | 14 | 18 |
| 12 | 28 | M | PER (LM) | 12 | 15 |
| 13 | 22 | M | SER (LM) | 12 | 15 |
| 14 | 25 | M | SER (LM) | 12 | 24 |
| 15 | 24 | M | PER (LM) | 12 | 15 |
| 16 | 33 | M | Maisonneuve | 19 | 36 |
| 17 | 25 | M | SER (LM) | 12 | 15 |
| 18 | 26 | M | SER (LM) | 13 | 20 |
| 19 | 23 | M | PER PM | 12 | 15 |
| 20 | 26 | M | SER (LM) | 10 | 16 |
| 21 | 21 | M | SER (LM) | 12 | 25 |
| 22 | 26 | M | SER (LM) | 12 | 24 |
| 23 | 22 | M | PER (LM, MM, PM) | 12 | 24 |
| 24 | 21 | M | SER (LM) | 13 | 16 |
| 25 | 22 | M | SER (LM) | 14 | 18 |
| 26 | 23 | M | SER (LM) | 14 | 18 |
| 27 | 21 | M | SER (LM) | 10 | 19 |
| 28 | 20 | M | Isolated | 13 | 22 |
| 29 | 23 | M | SER (LM) | 16 | 19 |
| 30 | 21 | M | SER (LM, PM) | 11 | 20 |
| 31 | 22 | M | PER (LM, MM, PM) | 13 | 18 |
| 32 | 35 | M | Isolated | 7 | 17 |
| 33 | 35 | M | isolated | 12 | 16 |
| Authors | No. of Patients with Removal/Total | Cause of Removal | Time at Implant Removal | Radiographic Outcome |
|---|---|---|---|---|
| McMurray et al. [15] (2007) | 2/16 (12.5%) | Infection (1) Irritation (1) | NR | NR |
| Willmott et al. [12] (2009) | 2/6 (33.3%) | Irritation | 6 Mo/10 Mo | No diastasis |
| Treon et al. [31] (2009) | 4/18 (22.2%) | Wound breakdown, knot prominence | NR | NR |
| Gadd et al. [14] (2009) | 3/38 (7.9%) | Osteomyelitis (2) postoperative fall (1) | NR | NR |
| Coetzee and Ebeling [28] (2009) | 1/12 (8.3%) | Infection | 6 mon | NR |
| Qamar et al. [30] (2011) | 1/16 (6.3%) | Irritation | NR | NR |
| DeGroot et al. [29] (2011) | 6/24 (25%) | Irritation (4) Pain (1) Open fracture (1) | 12~35 Mo (4) 12 weeks (1) 8 weeks (1) | No diastasis |
| Naqvi et al. [32] (2012) | 3/49 (6.1%) | Infection (1) Infected sinus formation (1) Irritation (1) | NR 6 Mo 5 Mo | No diastasis |
| Rigby et al. [34] (2013) | 4/37 (10.8%) | Irritation | NR | |
| Maemple et al. [36] (2014) | 1/12 (8.3%) | Routine removal | NR | NR |
| Seyhan et al. [13] (2015) | 6/15 (40%) | Irritation (4) Irritation (2) | NR (4) 8 Mo/12 Mo (2) | NR |
| Kortekangas et al. [35] (2015) | 1/21 (4.8%) | Infection | 6 weeks | NR |
| Laflamme et al. [20] (2015) | 2/34 (5.9%) | Infection | 14 weeks | No diastasis |
| Kocadal et al. [33] (2016) | 1/26 (3.8%) | Irritation | NR | NR |
| Bondi et al. [27] (2016) | 1/36 (2.8%) | Irritation | 6 Mo | No diastasis |
| Anand et al. [26] (2017) | 1/36 (2.8%) | Irritation | 6 Mo | NR |
| Anderson et al. [11] (2018) | 11/48 (22.9%) | Local discomfort from SB (6) and plate (5) | NR | No diastasis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Kwon, M.; Day, J.; Seilern und Aspang, J.; Shim, J.; Cho, J. The Impact of Suture Button Removal in Syndesmosis Fixation. J. Clin. Med. 2021, 10, 3726. https://doi.org/10.3390/jcm10163726
Kim J, Kwon M, Day J, Seilern und Aspang J, Shim J, Cho J. The Impact of Suture Button Removal in Syndesmosis Fixation. Journal of Clinical Medicine. 2021; 10(16):3726. https://doi.org/10.3390/jcm10163726
Chicago/Turabian StyleKim, Jaeyoung, Minsoo Kwon, Jonathan Day, Jesse Seilern und Aspang, Jaehoon Shim, and Jaeho Cho. 2021. "The Impact of Suture Button Removal in Syndesmosis Fixation" Journal of Clinical Medicine 10, no. 16: 3726. https://doi.org/10.3390/jcm10163726
APA StyleKim, J., Kwon, M., Day, J., Seilern und Aspang, J., Shim, J., & Cho, J. (2021). The Impact of Suture Button Removal in Syndesmosis Fixation. Journal of Clinical Medicine, 10(16), 3726. https://doi.org/10.3390/jcm10163726







