Criterion-Related Validity of Field-Based Fitness Tests in Adults: A Systematic Review
Abstract
:1. Introduction
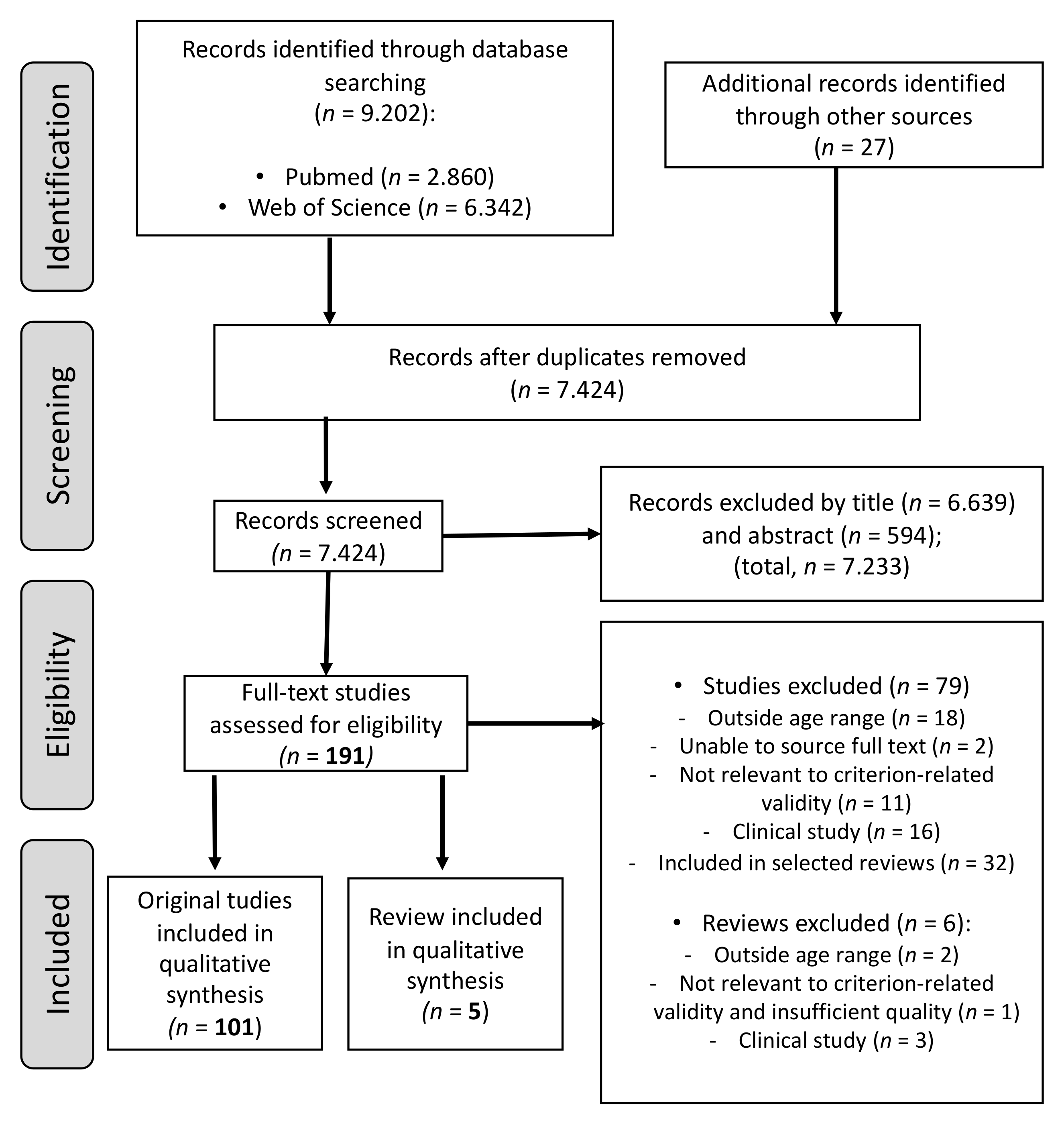
2. Materials and Methods
2.1. Literature Search
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Criteria for Risk of Bias Assessment
2.5. Levels of Evidence
3. Results
3.1. Quality Assessment
3.2. Criterion-Related Validity
3.2.1. Cardiorespiratory Fitness
Distance and Time-Based Run/Walk Tests
Twenty-Metre Shuttle Run Test
Step Tests
3.2.2. Muscular Strength
Maximal Isometric Strength
Endurance Strength
Explosive Strength
3.2.3. Flexibility
3.2.4. Motor Fitness
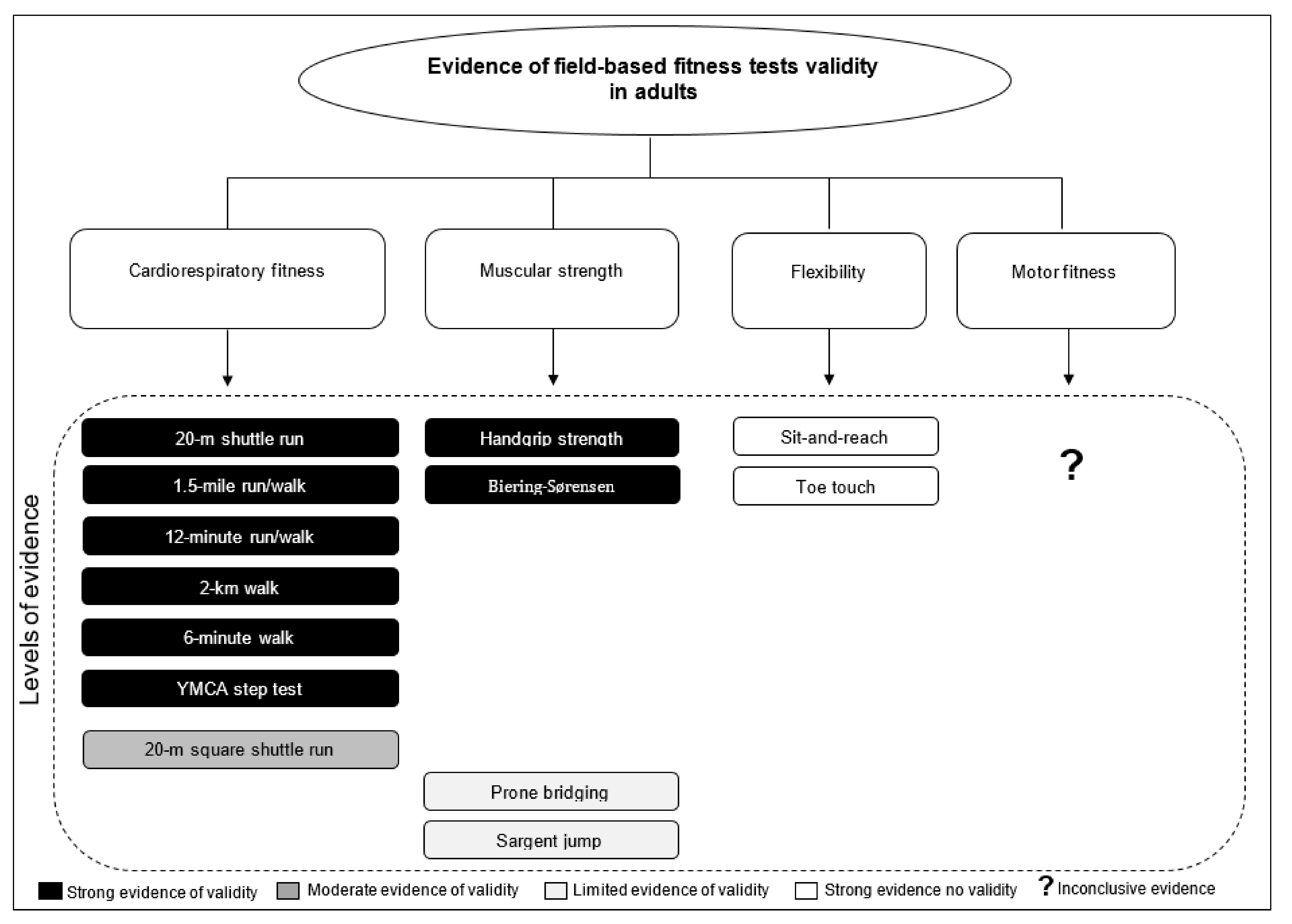
4. Discussion
4.1. Cardiorespiratory Fitness
4.1.1. Distance and Time-Based Run/Walk Tests
4.1.2. Twenty-Metre Shuttle Run Test
4.1.3. Step Tests
4.1.4. Levels of Evidence
4.2. Muscular Strength
4.2.1. Maximal Isometric Strength
4.2.2. Endurance Strength
4.2.3. Explosive Strength
4.2.4. Levels of Evidence
4.3. Flexibility
Levels of Evidence
4.4. Motor Fitness
Levels of Evidence
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Castillo Garzon, M.J.; Ortega Porcel, F.B.; Ruiz Ruiz, J. Improvement of physical fitness as anti-aging intervention. Med. Clin. 2005, 124, 146–155. [Google Scholar]
- LaMonte, M.J.; Barlow, C.E.; Jurca, R.; Kampert, J.B.; Church, T.S.; Blair, S.N. Cardiorespiratory fitness is inversely associated with the incidence of metabolic syndrome: A prospective study of men and women. Circulation 2005, 112, 505–512. [Google Scholar] [CrossRef] [Green Version]
- Fung, M.D.; Canning, K.L.; Mirdamadi, P.; Ardern, C.I.; Kuk, J.L. Lifestyle and weight predictors of a healthy overweight profile over a 20-year follow-up. Obesity 2015, 23, 1320–1325. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Howe, T.E.; Rochester, L.; Neil, F.; Skelton, D.A.; Ballinger, C. Exercise for improving balance in older people. Cochrane Database Syst. Rev. 2011, 11, Cd004963. [Google Scholar] [CrossRef] [PubMed]
- Balducci, S.; Cardelli, P.; Pugliese, L.; D’Errico, V.; Haxhi, J.; Alessi, E.; Iacobini, C.; Menini, S.; Bollanti, L.; Conti, F.G.; et al. Volume-dependent effect of supervised exercise training on fatty liver and visceral adiposity index in subjects with type 2 diabetes The Italian Diabetes Exercise Study (IDES). Diabetes Res. Clin. Pract. 2015, 109, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Pletnikoff, P.P.; Laukkanen, J.A.; Tuomainen, T.P.; Kauhanen, J.; Rauramaa, R.; Ronkainen, K.; Kurl, S. Cardiorespiratory fitness, C-reactive protein and lung cancer risk: A prospective population-based cohort study. Eur. J. Cancer 2015, 51, 1365–1370. [Google Scholar] [CrossRef] [PubMed]
- Sui, X.; Lee, D.C.; Matthews, C.E.; Adams, S.A.; Hebert, J.R.; Church, T.S.; Lee, C.D.; Blair, S.N. Influence of cardiorespiratory fitness on lung cancer mortality. Med. Sci. Sports Exerc. 2010, 42, 872–878. [Google Scholar] [CrossRef] [Green Version]
- Blair, S.N.; Kohl, H.W., 3rd; Paffenbarger, R.S., Jr.; Clark, D.G.; Cooper, K.H.; Gibbons, L.W. Physical fitness and all-cause mortality. A prospective study of healthy men and women. JAMA 1989, 262, 2395–2401. [Google Scholar] [CrossRef]
- Farrell, S.W.; Fitzgerald, S.J.; McAuley, P.A.; Barlow, C.E. Cardiorespiratory fitness, adiposity, and all-cause mortality in women. Med. Sci. Sports Exerc. 2010, 42, 2006–2012. [Google Scholar] [CrossRef]
- Barry, V.W.; Baruth, M.; Beets, M.W.; Durstine, J.L.; Liu, J.; Blair, S.N. Fitness vs. fatness on all-cause mortality: A meta-analysis. Prog. Cardiovasc. Dis. 2014, 56, 382–390. [Google Scholar] [CrossRef]
- Ortega, F.B.; Lavie, C.J.; Blair, S.N. Obesity and Cardiovascular Disease. Circ. Res. 2016, 118, 1752–1770. [Google Scholar] [CrossRef] [Green Version]
- McAuley, P.A.; Beavers, K.M. Contribution of cardiorespiratory fitness to the obesity paradox. Prog. Cardiovasc. Dis. 2014, 56, 434–440. [Google Scholar] [CrossRef]
- Lavie, C.J.; McAuley, P.A.; Church, T.S.; Milani, R.V.; Blair, S.N. Obesity and cardiovascular diseases: Implications regarding fitness, fatness, and severity in the obesity paradox. J. Am. Coll. Cardiol. 2014, 63, 1345–1354. [Google Scholar] [CrossRef] [Green Version]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Barry, V.W.; Caputo, J.L.; Kang, M. The Joint Association of Fitness and Fatness on Cardiovascular Disease Mortality: A Meta-Analysis. Prog. Cardiovasc. Dis. 2018, 61, 136–141. [Google Scholar] [CrossRef]
- Oktay, A.A.; Lavie, C.J.; Kokkinos, P.F.; Parto, P.; Pandey, A.; Ventura, H.O. The Interaction of Cardiorespiratory Fitness With Obesity and the Obesity Paradox in Cardiovascular Disease. Prog. Cardiovasc. Dis. 2017, 60, 30–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Delextrat, A.A.; Warner, S.; Graham, S.; Neupert, E. An 8-Week Exercise Intervention Based on Zumba Improves Aerobic Fitness and Psychological Well-Being in Healthy Women. J. Phys. Act. Health 2016, 13, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Lee, D.C.; Sui, X.; Kubzansky, L.D.; Ruiz, J.R.; Baruth, M.; Castillo, M.J.; Blair, S.N. Psychological well-being, cardiorespiratory fitness, and long-term survival. Am. J. Prev. Med. 2010, 39, 440–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boots, E.A.; Schultz, S.A.; Oh, J.M.; Larson, J.; Edwards, D.; Cook, D.; Koscik, R.L.; Dowling, M.N.; Gallagher, C.L.; Carlsson, C.M.; et al. Cardiorespiratory fitness is associated with brain structure, cognition, and mood in a middle-aged cohort at risk for Alzheimer's disease. Brain Imaging Behav. 2015, 9, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Willis, B.L.; Gao, A.; Leonard, D.; Defina, L.F.; Berry, J.D. Midlife fitness and the development of chronic conditions in later life. Arch. Intern. Med. 2012, 172, 1333–1340. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Jacobs, D.R., Jr.; Schreiner, P.J.; Launer, L.J.; Whitmer, R.A.; Sidney, S.; Demerath, E.; Thomas, W.; Bouchard, C.; He, K.; et al. Cardiorespiratory fitness and brain volume and white matter integrity: The CARDIA Study. Neurology 2015, 84, 2347–2353. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia-Hermoso, A.; Cavero-Redondo, I.; Ramirez-Velez, R.; Ruiz, J.R.; Ortega, F.B.; Lee, D.C.; Martinez-Vizcaino, V. Muscular Strength as a Predictor of All-Cause Mortality in an Apparently Healthy Population: A Systematic Review and Meta-Analysis of Data From Approximately 2 Million Men and Women. Arch. Phys. Med. Rehabil. 2018, 99, 2100–2113.e5. [Google Scholar] [CrossRef]
- Garcia-Hermoso, A.; Ramirez-Velez, R.; Peterson, M.D.; Lobelo, F.; Cavero-Redondo, I.; Correa-Bautista, J.E.; Martinez-Vizcaino, V. Handgrip and knee extension strength as predictors of cancer mortality: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2018, 28, 1852–1858. [Google Scholar] [CrossRef] [PubMed]
- Kettunen, O.; Kyrolainen, H.; Santtila, M.; Vasankari, T. Physical fitness and volume of leisure time physical activity relate with low stress and high mental resources in young men. J. Sports Med. Phys. Fit. 2014, 54, 545–551. [Google Scholar]
- Currell, K.; Jeukendrup, A.E. Validity, reliability and sensitivity of measures of sporting performance. Sports Med. 2008, 38, 297–316. [Google Scholar] [CrossRef] [PubMed]
- Docherty, D. Field tests and test batteries. In Measurement in Pediatric Exercise Science; Docherty, D., Ed.; Human Kinetics: Champaign, IL, USA, 1996; pp. 285–334. [Google Scholar]
- Castro-Pinero, J.; Artero, E.G.; Espana-Romero, V.; Ortega, F.B.; Sjostrom, M.; Suni, J.; Ruiz, J.R. Criterion-related validity of field-based fitness tests in youth: A systematic review. Br. J. Sports Med. 2009, 44, 934–943. [Google Scholar] [CrossRef]
- Mayorga-Vega, D.; Aguilar-Soto, P.; Viciana, J. Criterion-related validity of the 20-m shuttle run test for estimating cardiorespiratory fitness: A meta-analysis. J. Sports Sci. Med. 2015, 14, 536–547. [Google Scholar]
- Mayorga-Vega, D.; Viciana, J.; Cocca, A.; Merino-Marban, R. Criterion-related validity of toe-touch test for estimating hamstring extensibility: A metaanalysis. J. Hum. Sport Exerc. 2014, 9, 188–200. [Google Scholar] [CrossRef] [Green Version]
- Mayorga-Vega, D.; Bocanegra-Parrilla, R.; Ornelas, M.; Viciana, J. Criterion-related validity of the distance- and time-based walk/run field tests for estimating cardiorespiratory fitness: A systematic review and Meta-analysis. PLoS ONE 2016, 11, e0151671. [Google Scholar] [CrossRef] [Green Version]
- Mayorga-Vega, D.; Merino-Marban, R.; Viciana, J. Criterion-related validity of sit-and-reach tests for estimating hamstring and lumbar extensibility: A meta-analysis. J. Sports Sci. Med. 2014, 13, 1–14. [Google Scholar] [PubMed]
- Bennett, H.; Parfitt, G.; Davison, K.; Eston, R. Validity of submaximal step tests to estimate maximal oxygen uptake in healthy adults. Sports Med. 2016, 46, 737–750. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Shea, B.J.; Hamel, C.; Wells, G.A.; Bouter, L.M.; Kristjansson, E.; Grimshaw, J.; Henry, D.A.; Boers, M. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J. Clin. Epidemiol. 2009, 62, 1013–1020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biddle, S.J.; García Bengoechea, E.; Wiesner, G. Sedentary behaviour and adiposity in youth: A systematic review of reviews and analysis of causality. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 43. [Google Scholar] [CrossRef] [PubMed]
- Oja, P.; Laukkanen, R.; Pasanen, M.; Tyry, T.; Vuori, I. A 2-km walking test for assessing the cardiorespiratory fitness of healthy adults. Int. J. Sports Med. 1991, 12, 356–362. [Google Scholar] [CrossRef]
- Laukkanen, R.; Oja, P.; Pasanen, M.; Vuori, I. Validity of a two kilometre walking test for estimating maximal aerobic power in overweight adults. Int. J. Obes. Relat. Metab. Disord. 1992, 16, 263–268. [Google Scholar]
- Laukkanen, R.M.T.; Oja, P.; Pasanen, M.E.; Vuori, I.M. Criterion validitv of a two-kilometer walking test for predicting the maximal oxygen uptake of moderately to highly active middle-aged adults. Scand. J. Med. Sci. Sports 1993, 3, 267–272. [Google Scholar] [CrossRef]
- Laukkanen, R.M.T.; Kukkonen-Harjula, T.K.; Oja, P.; Pasanen, M.E.; Vuori, I.M. Prediction of change in maximal aerobic power by the 2-km walk test after walking training in middle-aged adults. Int. J. Sports Med. 2000, 21, 113–116. [Google Scholar] [CrossRef]
- Larsen, G.E.; George, J.D.; Alexander, J.L.; Fellingham, G.W.; Aldana, S.G.; Parcell, A.C. Prediction of maximum oxygen consumption from walking, jogging, or running. Res. Q. Exerc. Sport 2002, 73, 66–72. [Google Scholar] [CrossRef]
- McNaughton, L.; Hall, P.; Cooley, D. Validation of several methods of estimating maximal oxygen uptake in young men. Percept. Mot. Ski. 1998, 87, 575–584. [Google Scholar] [CrossRef]
- Kline, C.; Porcari, J.P.; Hintermeister, R.; Freedson, P.S.; Ward, A.; McCarron, R.F.; Ross, J.; Rippe, J. Estimation of from a one-mile track walk, gender, age and body weight. Med. Sports Exerc. 1987, 19, 253–259. [Google Scholar]
- George, J.D.; Fellingham, G.W.; Fisher, A.G. A modified version of the Rockport Fitness Walking Test for college men and women. Res. Q. Exerc. Sport 1998, 69, 205–209. [Google Scholar] [CrossRef]
- Lunt, H.; Roiz De Sa, D.; Roiz De Sa, J.; Allsopp, A. Validation of one-mile walk equations for the estimation of aerobic fitness in British military personnel under the age of 40 years. Mil. Med. 2013, 178, 753–759. [Google Scholar] [CrossRef] [Green Version]
- Greenhalgh, H.A.; George, J.D.; Hager, R.L. Cross-validation of a quarter-mile walk test using two VO2 max regression models. Meas. Phys. Educ. Exerc. Sci. 2001, 5, 139–151. [Google Scholar] [CrossRef]
- Dolgener, F.A.; Hensley, L.D.; Marsh, J.J.; Fjelstul, J.K. Validation of the Rockport Fitness Walking Test in college males and females. Res. Q. Exerc. Sport 1994, 65, 152–158. [Google Scholar] [CrossRef]
- Seneli, R.M.; Ebersole, K.T.; O’Connor, K.M.; Snyder, A.C. Estimated VO2max from the Rockport Walk Test on a Nonmotorized Curved Treadmill. J. Strength Cond. Res. 2013, 27, 3495–3505. [Google Scholar] [CrossRef] [PubMed]
- George, J.D.; Vehrs, P.R.; Allsen, P.E.; Fellingham, G.W.; Fisher, A.G. Development of a submaximal treadmill jogging test for fit college-aged individuals. Med. Sci. Sports Exerc. 1993, 25, 643–647. [Google Scholar] [CrossRef]
- Cao, Z.-B.; Miyatake, N.; Aoyama, T.; Higuchi, M.; Tabata, I. Prediction of maximal oxygen uptake from a 3-minute walk based on gender, age, and body composition. J. Phys. Act. Health 2013, 10, 280–287. [Google Scholar] [CrossRef]
- Di Thommazo-Luporini, L.; Pinheiro Carvalho, L.; Luporini, R.; Trimer, R.; Falasco Pantoni, C.B.; Catai, A.M.; Arena, R.; Borghi-Silva, A. The six-minute step test as a predictor of cardiorespiratory fitness in obese women. Eur. J. Phys. Rehabil. Med. 2015, 51, 793–802. [Google Scholar] [PubMed]
- Di Thommazo-Luporini, L.; Carvalho, L.P.; Luporini, R.L.; Trimer, R.; Falasco Pantoni, C.B.; Martinez, A.F.; Catai, A.M.; Arena, R.; Borghi-Silva, A. Are cardiovascular and metabolic responses to field walking tests interchangeable and obesity-dependent? Disabil. Rehabil. 2016, 38, 1820–1829. [Google Scholar] [CrossRef]
- Manttari, A.; Suni, J.; Sievanen, H.; Husu, P.; Vaha-Ypya, H.; Valkeinen, H.; Tokola, K.; Vasankari, T. Six-minute walk test: A tool for predicting maximal aerobic power (VO2 max) in healthy adults. Clin. Physiol. Funct. Imaging 2018. [Google Scholar] [CrossRef] [PubMed]
- Bonet, J.B.; Magalhaes, J.; Viscor, G.; Pages, T.; Javierre, C.F.; Torrella, J.R. A field tool for the aerobic power evaluation of middle-aged female recreational runners. Women Health 2020, 60, 839–848. [Google Scholar] [CrossRef] [PubMed]
- Cooper, S.M.; Baker, J.S.; Tong, R.J.; Roberts, E.; Hanford, M. The repeatability and criterion related validity of the 20 m multistage fitness test as a predictor of maximal oxygen uptake in active young men. Br. J. Sports Med. 2005, 39, e19. [Google Scholar] [CrossRef] [PubMed]
- Flouris, A.D.; Koutedakis, Y.; Nevill, A.; Metsios, G.S.; Tsiotra, G.; Parasiris, Y. Enhancing specificity in proxy-design for the assessment of bioenergetics. J. Sci. Med. Sport 2004, 7, 197–204. [Google Scholar] [CrossRef] [Green Version]
- Metsios, G.S.; Flouris, A.D.; Koutedakis, Y.; Nevill, A. Criterion-related validity and test-retest reliability of the 20m square shuttle test. J. Sci. Med. Sport 2008, 11, 214–217. [Google Scholar] [CrossRef]
- Flouris, A.D.; Metsios, G.S.; Koutedakis, Y. Enhancing the efficacy of the 20 m multistage shuttle run test. Br. J. Sports Med. 2005, 39, 166–170. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Jung, S.H.; Cho, H.C. Validity and Reliability of Shuttle-Run Test in Korean Adults. Int. J. Sports Med. 2011, 32, 580–585. [Google Scholar] [CrossRef]
- Jurio-Iriarte, B.; Gorostegi-Anduaga, I.; Rodrigo Aispuru, G.; Perez-Asenjo, J.; Brubaker, P.H.; Maldonado-Martin, S. Association between Modified Shuttle Walk Test and cardiorespiratory fitness in overweight/obese adults with primary hypertension: EXERDIET-HTA study. J. Am. Soc. Hypertens. 2017, 11, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Jurio-Iriarte, B.; Brubaker, P.H.; Gorostegi-Anduaga, I.; Corres, P.; Martinez Aguirre-Betolaza, A.; Maldonado-Martin, S. Validity of the modified shuttle walk test to assess cardiorespiratory fitness after exercise intervention in overweight/obese adults with primary hypertension. Clin. Exp. Hypertens. 2018, 41, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Lima, L.P.; Leite, H.R.; Matos, M.A.; Neves, C.D.C.; Lage, V.; Silva, G.P.D.; Lopes, G.S.; Chaves, M.G.A.; Santos, J.N.V.; Camargos, A.C.R.; et al. Cardiorespiratory fitness assessment and prediction of peak oxygen consumption by Incremental Shuttle Walking Test in healthy women. PLoS ONE 2019, 14, e0211327. [Google Scholar] [CrossRef]
- Aadahl, M.; Zacho, M.; Linneberg, A.; Thuesen, B.H.; Jorgensen, T. Comparison of the Danish step test and the watt-max test for estimation of maximal oxygen uptake: The Health2008 study. Eur. J. Prev. Cardiol. 2013, 20, 1088–1094. [Google Scholar] [CrossRef]
- Kumar, S.K.; Khare, P.; Jaryal, A.K.; Talwar, A. Validity of heart rate based nomogram fors estimation of maximum oxygen uptake in Indian population. Indian J. Physiol. Pharmacol. 2012, 56, 279–283. [Google Scholar] [PubMed]
- Ricci, P.A.; Cabiddu, R.; Jürgensen, S.P.; André, L.D.; Oliveira, C.R.; Di Thommazo-Luporini, L.; Ortega, F.P.; Borghi-Silva, A. Validation of the two-minute step test in obese with comorbibities and morbidly obese patients. Braz. J. Med Biol. Res. 2019, 52, e8402. [Google Scholar] [CrossRef] [PubMed]
- Weller, I.M.; Thomas, S.G.; Cox, M.H.; Corey, P.N. A study to validate the Canadian Aerobic Fitness Test. Can. J. Public Health 1992, 83, 120–124. [Google Scholar] [CrossRef]
- Carvalho, L.P.; Di Thommazo-Luporini, L.; Aubertin-Leheudre, M.; Bonjorno Junior, J.C.; de Oliveira, C.R.; Luporini, R.L.; Mendes, R.G.; Lopes Zangrando, K.T.; Trimer, R.; Arena, R.; et al. Prediction of cardiorespiratory fitness by the six-minute step test and its association with muscle strength and power in sedentary obese and lean young women: A cross-sectional study. PLoS ONE 2015, 10, e0145960. [Google Scholar] [CrossRef] [PubMed]
- Teren, A.; Zachariae, S.; Beutner, F.; Ubrich, R.; Sandri, M.; Engel, C.; Loeffler, M.; Gielen, S. Incremental value of veterans specific activity questionnaire and the ymca-step test for the assessment of cardiorespiratory fitness in population-based studies. Eur. J. Prev. Cardiol. 2016, 23, 1221–1227. [Google Scholar] [CrossRef] [PubMed]
- Beutner, F.; Ubrich, R.; Zachariae, S.; Engel, C.; Sandri, M.; Teren, A.; Gielen, S. Validation of a brief step-test protocol for estimation of peak oxygen uptake. Eur. J. Prev. Cardiol. 2015, 22, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Lee, O.; Lee, S.; Kang, M.; Mun, J.; Chung, J. Prediction of maximal oxygen consumption using the Young Men’s Christian Association-step test in Korean adults. Eur. J. Appl. Physiol. 2019, 119, 1245–1252. [Google Scholar] [CrossRef] [PubMed]
- Kieu, N.T.V.; Jung, S.J.; Shin, S.W.; Jung, H.W.; Jung, E.S.; Won, Y.H.; Kim, Y.G.; Chae, S.W. The validity of the YMCA 3-minute step test for estimating maximal oxygen uptake in healthy Korean and Vietnamese adults. J. Lifestyle Med. 2020, 10, 21–29. [Google Scholar] [CrossRef]
- Hong, S.H.; Yang, H.I.; Kim, D.I.; Gonzales, T.I.; Brage, S.; Jeon, J.Y. Validation of submaximal step tests and the 6-min walk test for predicting maximal oxygen consumption in young and healthy participants. Int. J. Environ. Res. Public Health 2019, 16, 4858. [Google Scholar] [CrossRef] [Green Version]
- Hansen, D.; Jacobs, N.; Thijs, H.; Dendale, P.; Claes, N. Validation of a single-stage fixed-rate step test for the prediction of maximal oxygen uptake in healthy adults. Clin. Physiol. Funct. Imaging 2016, 36, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Espana-Romero, V.; Artero, E.G.; Santaliestra-Pasias, A.M.; Gutierrez, A.; Castillo, M.J.; Ruiz, J.R. Hand span influences optimal grip span in boys and girls aged 6 to 12 years. J. Hand Surg. 2008, 33, 378–384. [Google Scholar] [CrossRef] [PubMed]
- Cadenas-Sanchez, C.; Sanchez-Delgado, G.; Martinez-Tellez, B.; Mora-Gonzalez, J.; Löf, M.; España-Romero, V.; Ruiz, J.R.; Ortega, F.B. Reliability and validity of different models of TKK hand dynamometers. Am. J. Occup. Ther. 2016, 70, 7004300010. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolimechkov, S.; Castro-Piñero, J.; Petrov, A.; Alexandrova, A. The effect of elbow position on the handgrip strength test in children: Validity and reliability of TKK 5101 and DynX dynamometers. Pedagog. Phys Cult Sports 2020, 24, 240–247. [Google Scholar] [CrossRef]
- Shechtman, O.; Gestewitz, L.; Kimble, C. Reliability and validity of the DynEx dynamometer. J. Hand Ther. 2005, 18, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F.; Dolan, P. Electromyographic median frequency changes during isometric contraction of the back extensors to fatigue. Spine 1994, 19, 1223–1229. [Google Scholar] [CrossRef]
- Coorevits, P.; Danneels, L.; Cambier, D.; Ramon, H.; Vanderstraeten, G. Assessment of the validity of the Biering-Sørensen test for measuring back muscle fatigue based on EMG median frequency characteristics of back and hip muscles. J. Electromyogr. Kinesiol. 2008, 18, 997–1005. [Google Scholar] [CrossRef]
- Kankaanpää, M.; Laaksonen, D.; Taimela, S.; Kokko, S.M.; Airaksinen, O.; Hänninen, O. Age, sex, and body mass index as determinants of back and hip extensor fatigue in the isometric Sørensen back endurance test. Arch. Phys. Med. Rehabil. 1998, 79, 1069–1075. [Google Scholar] [CrossRef]
- De Blaiser, C.; De Ridder, R.; Willems, T.; Danneels, L.; Roosen, P. Reliability and validity of trunk flexor and trunk extensor strength measurements using handheld dynamometry in a healthy athletic population. Phys. Ther. Sport 2018, 34, 180–186. [Google Scholar] [CrossRef]
- Bui, H.T.; Farinas, M.-I.; Fortin, A.-M.; Comtois, A.-S.; Leone, M. Comparison and analysis of three different methods to evaluate vertical jump height. Clin. Physiol. Funct. Imaging 2015, 35, 203–209. [Google Scholar] [CrossRef]
- Kawano, M.M.; Ambar, G.; Oliveira, B.I.R.; Boer, M.C.; Cardoso, A.P.R.G.; Cardoso, J.R. Influence of the gastrocnemius muscle on the sit-and-reach test assessed by angular kinematic analysis. Braz. J. Phys. Ther. 2010, 14, 10–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bassett, D.R., Jr.; Howley, E.T.; Thompson, D.L.; King, G.A.; Strath, S.J.; McLaughlin, J.E.; Parr, B.B. Validity of inspiratory and expiratory methods of measuring gas exchange with a computerized system. J. Appl. Physiol. 2001, 91, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Meredith, M.D.; Welk, G.J. Fitnessgram & Activitygram Test Administration Manual, 4th ed.; Human Kinetics: Champaign, IL, USA, 2010. [Google Scholar]
- Ruiz, J.R.; Ortega, F.B.; Castro-Piñero, J. Validity and reliability of the 1/4 mile run-walk test in physically active children and adolescents. Nutr. Hosp. 2014, 31, 875–882. [Google Scholar]
- Krahenbuhl, G.S.; Pangrazi, R.P.; Burkett, L.N.; Schneider, M.J.; Petersen, G. Field estimation of VO2 max in children eight years of age. Med. Sci. Sports 1977, 9, 37–40. [Google Scholar] [CrossRef] [PubMed]
- McCormack, W.P.; Cureton, K.J.; Bullock, T.A.; Weyand, P.G. Metabolic determinants of 1-mile run/walk performance in children. Med. Sci. Sports Exerc. 1991, 23, 611–617. [Google Scholar] [CrossRef]
- Shephard, R.J. Tests of maximum oxygen intake. A critical review. Sports Med. 1984, 1, 99–124. [Google Scholar] [CrossRef]
- Duncan, M.J.; Mota, J.; Carvalho, J.; Nevill, A.M. An Evaluation of Prediction Equations for the 6 Minute Walk Test in Healthy European Adults Aged 50–85 Years. PLoS ONE 2015, 10, e0139629. [Google Scholar]
- Burr, J.F.; Bredin, S.S.; Faktor, M.D.; Warburton, D.E. The 6-minute walk test as a predictor of objectively measured aerobic fitness in healthy working-aged adults. Physician Sportsmed. 2011, 39, 133–139. [Google Scholar] [CrossRef]
- Leger, L.A.; Mercier, D.; Gadoury, C.; Lambert, J. The multistage 20 m shuttle run test for aerobic fitness. J. Sports Sci. 1988, 6, 93–101. [Google Scholar] [CrossRef]
- Santo, A.; Golding, L.A. Predicting maximum oxygen uptake from a modified 3-minute step test. Res. Q. Exer. Sport 2003, 74, 110–115. [Google Scholar] [CrossRef]
- Mayhew, J.L.; Ball, T.E.; Ward, T.E.; Hart, C.L.; Arnold, M.D. Relationships of structural dimensions to bench press strength in college males. J. Sports Med. Phys. Fit. 1991, 31, 135–141. [Google Scholar]
- Stark, T.; Walker, B.; Phillips, J.K.; Fejer, R.; Beck, R. Hand-held dynamometry correlation with the gold standard isokinetic dynamometry: A systematic review. PM R. 2011, 3, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Paul, D.J.; Nassis, G.P. Testing strength and power in soccer players: The application of conventional and traditional methods of assessment. J. Strength Cond. Res. 2015, 29, 1748–1758. [Google Scholar] [CrossRef] [PubMed]
- De Ste Croix, M.; Deighan, M.; Armstrong, N. Assessment and interpretation of isokinetic muscle strength during growth and maturation. Sports Med. 2003, 33, 727–743. [Google Scholar] [CrossRef] [PubMed]
- España-Romero, V.; Ortega, F.B.; Vicente-Rodríguez, G.; Artero, E.G.; Rey, J.P.; Ruiz, J.R. Elbow position affects handgrip strength in adolescents: Validity and reliability of Jamar, DynEx, and TKK dynamometers. J. Strength Cond. Res. 2010, 24, 272–277. [Google Scholar] [CrossRef] [PubMed]
- Balogun, J.A.; Akomolafe, C.T.; Amusa, L.O. Grip strength: Effects of testing posture and elbow position. Arch. Phys. Med. Rehabil. 1991, 72, 280–283. [Google Scholar] [PubMed]
- NHANES, Muscle Strength Procedures Manual; National Health and Nutrition Examination Survey (NHANES); CDC: Druid Hills, GA, USA, 2013.
- Ruiz-Ruiz, J.; Mesa, J.L.; Gutiérrez, A.; Castillo, M.J. Hand size influences optimal grip span in women but not in men. J. Hand Surg. 2002, 27, 897–901. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, W.J.; Kim, K.J.; Song, D.G.; Lee, J.S.; Park, K.Y.; Lee, J.W.; Chang, S.H.; Choy, W.S. Sarcopenia and Back Muscle Degeneration as Risk Factors for Back Pain: A Comparative Study. Asian Spine J. 2020, 14, 364–372. [Google Scholar] [CrossRef] [Green Version]
- Abdelraouf, O.R.; Abdel-Aziem, A.A. The relationship between core endurance and back dysfunction in collegiate male athletes with and without nonspecific low back pain. Int. J. Sports Phys. Ther. 2016, 11, 337–344. [Google Scholar]
- Ozcan Kahraman, B.; Salik Sengul, Y.; Kahraman, T.; Kalemci, O. Developing a Reliable Core Stability Assessment Battery for Patients with Nonspecific Low Back Pain. Spine 2016, 41, E844–E850. [Google Scholar] [CrossRef] [Green Version]
- Arab, A.M.; Salavati, M.; Ebrahimi, I.; Ebrahim Mousavi, M. Sensitivity, specificity and predictive value of the clinical trunk muscle endurance tests in low back pain. Clin. Rehabil. 2007, 21, 640–647. [Google Scholar] [CrossRef]
- del Pozo-Cruz, B.; Mocholi, M.H.; del Pozo-Cruz, J.; Parraca, J.A.; Adsuar, J.C.; Gusi, N. Reliability and validity of lumbar and abdominal trunk muscle endurance tests in office workers with nonspecific subacute low back pain. J. Back Musculoskelet. Rehabil. 2014, 27, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Cadenas-Sanchez, C.; Sanchez-Delgado, G.; Mora-Gonzalez, J.; Martinez-Tellez, B.; Artero, E.G.; Castro-Pinero, J.; Labayen, I.; Chillon, P.; Lof, M.; et al. Systematic review and proposal of a field-based physical fitness-test battery in preschool children: The PREFIT battery. Sports Med. 2015, 45, 533–555. [Google Scholar] [CrossRef]
- Ruiz, J.R.; Castro-Piñero, J.; Espana-Romero, V.; Artero, E.G.; Ortega, F.B.; Cuenca, M.M.; Jimenez-Pavon, D.; Chillon, P.; Girela-Rejon, M.J.; Mora, J.; et al. Field-based fitness assessment in young people: The ALPHA health-related fitness test battery for children and adolescents. Br. J. Sports Med. 2011, 45, 518–524. [Google Scholar] [CrossRef]
- Leighton, J.R. An instrument and technic for the measurement of range of joint motion. Arch. Phys. Med. Rehabil. 1955, 36, 571–578. [Google Scholar]
- Kanbur, N.O.; Duzgun, I.; Derman, O.; Baltaci, G. Do sexual maturation stages affect flexibility in adolescent boys aged 14 years? J. Sports Med. Phys. Fit. 2005, 45, 53–57. [Google Scholar]
- Castro-Pinero, J.; Chillon, P.; Ortega, F.B.; Montesinos, J.L.; Sjostrom, M.; Ruiz, J.R. Criterion-related validity of sit-and-reach and modified sit-and-reach test for estimating hamstring flexibility in children and adolescents aged 6-17 years. Int. J. Sports Med. 2009, 30, 658–662. [Google Scholar] [CrossRef] [PubMed]
- Wells, K.F.; Dillon, E.K. The sit-and-reach. A test of back and leg flexibility. Res. Q. Exerc. Sport 1952, 23, 115–118. [Google Scholar] [CrossRef]
- Kraus, H.; Hirschland, R. Minimum muscular fitness of the school children. Res. Q. 1954, 25, 178–188. [Google Scholar] [CrossRef]
- Nuzzo, J.L. The Case for Retiring Flexibility as a Major Component of Physical Fitness. Sports Med. 2020, 50, 853–870. [Google Scholar] [CrossRef] [PubMed]
- Elbaz, A.; Sabia, S.; Brunner, E.; Shipley, M.; Marmot, M.; Kivimaki, M.; Singh-Manoux, A. Association of walking speed in late midlife with mortality: Results from the Whitehall II cohort study. Age 2013, 35, 943–952. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niiranen, T.J.; Enserro, D.M.; Larson, M.G.; Vasan, R.S. Multisystem Trajectories Over the Adult Life Course and Relations to Cardiovascular Disease and Death. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2019, 74, 1778–1785. [Google Scholar] [CrossRef] [PubMed]
- Cooper, R.; Strand, B.H.; Hardy, R.; Patel, K.V.; Kuh, D. Physical capability in mid-life and survival over 13 years of follow-up: British birth cohort study. BMJ 2014, 348, g2219. [Google Scholar] [CrossRef] [Green Version]
- Nitz, J.C.; Stock, L.; Khan, A. Health-related predictors of falls and fractures in women over 40. Osteoporos. Int. 2013, 24, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.X.M.; Yao, J.; Zirek, Y.; Reijnierse, E.M.; Maier, A.B. Muscle mass, strength, and physical performance predicting activities of daily living: A meta-analysis. J. Cachexia Sarcopenia Muscle 2020, 11, 3–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Briggs, R.; Carey, D.; Claffey, P.; McNicholas, T.; Donoghue, O.; Kennelly, S.P.; Kenny, R.A. Do Differences in Spatiotemporal Gait Parameters Predict the Risk of Developing Depression in Later Life? J. Am. Geriatr. Soc. 2019, 67, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
| Field-Based Fitness Test | Strong | Moderate | Limited |
|---|---|---|---|
| Shuttle run tests | |||
| 20 m shuttle run |  | ||
| 20 m square shuttle |  | ||
| Incremental shuttle walk |  | ||
| Distance and time-based run/walk test | |||
| 1.5-mile run/walk |  | ||
| 12 min run/walk |  | ||
| 5000 m run/walk | ◐ | ||
| 3 miles run/walk | ◐ | ||
| 2 miles run/walk | ◐ | ||
| 3.000 m run/walk | ◐ | ||
| 1000 m run/walk | ◐ | ||
| 600 m run/walk | ◐ | ||
| 600 yd run/walk | ◐ | ||
| ½-mile run/walk | ◐ | ||
| ¼-mile run/walk | ◐ | ||
| 9 min run/walk |  | ||
| 2 km walk |  | ||
| 6 min walk |  | ||
| 1-mile walk |  | ||
| ¼-mile walk |  | ||
| 3 min walk |  | ||
| Treadmill jogging |  | ||
| Mankato submaximal exercise |  | ||
| Modified Astrand–Ryhming |  | ||
| University Montreal |  | ||
| Ruffier | ⵔ | ||
| Step tests | |||
| YMCA step |  | ||
| Chester step |  | ||
| Modified Harvard step |  | ||
| 6 min single 15 cm-step |  | ||
| Modified Canadian aerobic fitness step |  | ||
| Tecumseh step |  | ||
| Astrand–Ryhming step |  | ||
| Danish step | ⵔ | ||
| Queen’s College step |  | ||
| 2 min step | ⵔ |
 Indicates high validity; ⵔ moderate validity; ◐ low/null validity;
Indicates high validity; ⵔ moderate validity; ◐ low/null validity;  inconclusive validity.
inconclusive validity.| Field-Based Fitness Test | Strong | Moderate | Limited |
|---|---|---|---|
| Maximal isometric strength | |||
| Handgrip strength (TKK) |  | ||
| Handgrip strength (Jamar) | ◐ | ||
| Handgrip strength (DynEx) |  | ||
| Hip and back endurance strength | |||
| Biering–Sørensen |  | ||
| Abdominal endurance strength | |||
| Prone bridging |  | ||
| Original/modifications curl-up | ⵔ | ||
| Lower body endurance strength | |||
| Sit-to-stand |  | ||
| Lower body explosive strength | |||
| Sargent jump |  | ||
| Upper body endurance strength | |||
| Original/modification flexed-arm hang |  | ||
| Baumgartner modified pull-up |  | ||
| Standard push-up |  | ||
| Hand-release push-up |  | ||
| Bent-knee push-up |  | ||
| Revised push-up |  | ||
| Lower back flexibility | |||
| Original/modifications sit-and-reach | |||
| Hamstring flexibility | ⵔ | ||
| Original/modifications sit-and-reach | ◐ | ||
| Toe-touch | ◐ | ||
| Agility | |||
| Ten-step | ◐ | ||
| Balance | |||
| Romberg test |  |
 Indicates high validity; ⵔ moderate validity; ◐ low/null validity;
Indicates high validity; ⵔ moderate validity; ◐ low/null validity;  inconclusive validity.
inconclusive validity.Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro-Piñero, J.; Marin-Jimenez, N.; Fernandez-Santos, J.R.; Martin-Acosta, F.; Segura-Jimenez, V.; Izquierdo-Gomez, R.; Ruiz, J.R.; Cuenca-Garcia, M. Criterion-Related Validity of Field-Based Fitness Tests in Adults: A Systematic Review. J. Clin. Med. 2021, 10, 3743. https://doi.org/10.3390/jcm10163743
Castro-Piñero J, Marin-Jimenez N, Fernandez-Santos JR, Martin-Acosta F, Segura-Jimenez V, Izquierdo-Gomez R, Ruiz JR, Cuenca-Garcia M. Criterion-Related Validity of Field-Based Fitness Tests in Adults: A Systematic Review. Journal of Clinical Medicine. 2021; 10(16):3743. https://doi.org/10.3390/jcm10163743
Chicago/Turabian StyleCastro-Piñero, Jose, Nuria Marin-Jimenez, Jorge R. Fernandez-Santos, Fatima Martin-Acosta, Victor Segura-Jimenez, Rocio Izquierdo-Gomez, Jonatan R. Ruiz, and Magdalena Cuenca-Garcia. 2021. "Criterion-Related Validity of Field-Based Fitness Tests in Adults: A Systematic Review" Journal of Clinical Medicine 10, no. 16: 3743. https://doi.org/10.3390/jcm10163743
APA StyleCastro-Piñero, J., Marin-Jimenez, N., Fernandez-Santos, J. R., Martin-Acosta, F., Segura-Jimenez, V., Izquierdo-Gomez, R., Ruiz, J. R., & Cuenca-Garcia, M. (2021). Criterion-Related Validity of Field-Based Fitness Tests in Adults: A Systematic Review. Journal of Clinical Medicine, 10(16), 3743. https://doi.org/10.3390/jcm10163743









