The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course
Abstract
:1. Introduction
2. Materials and Methods
Statistical Analysis
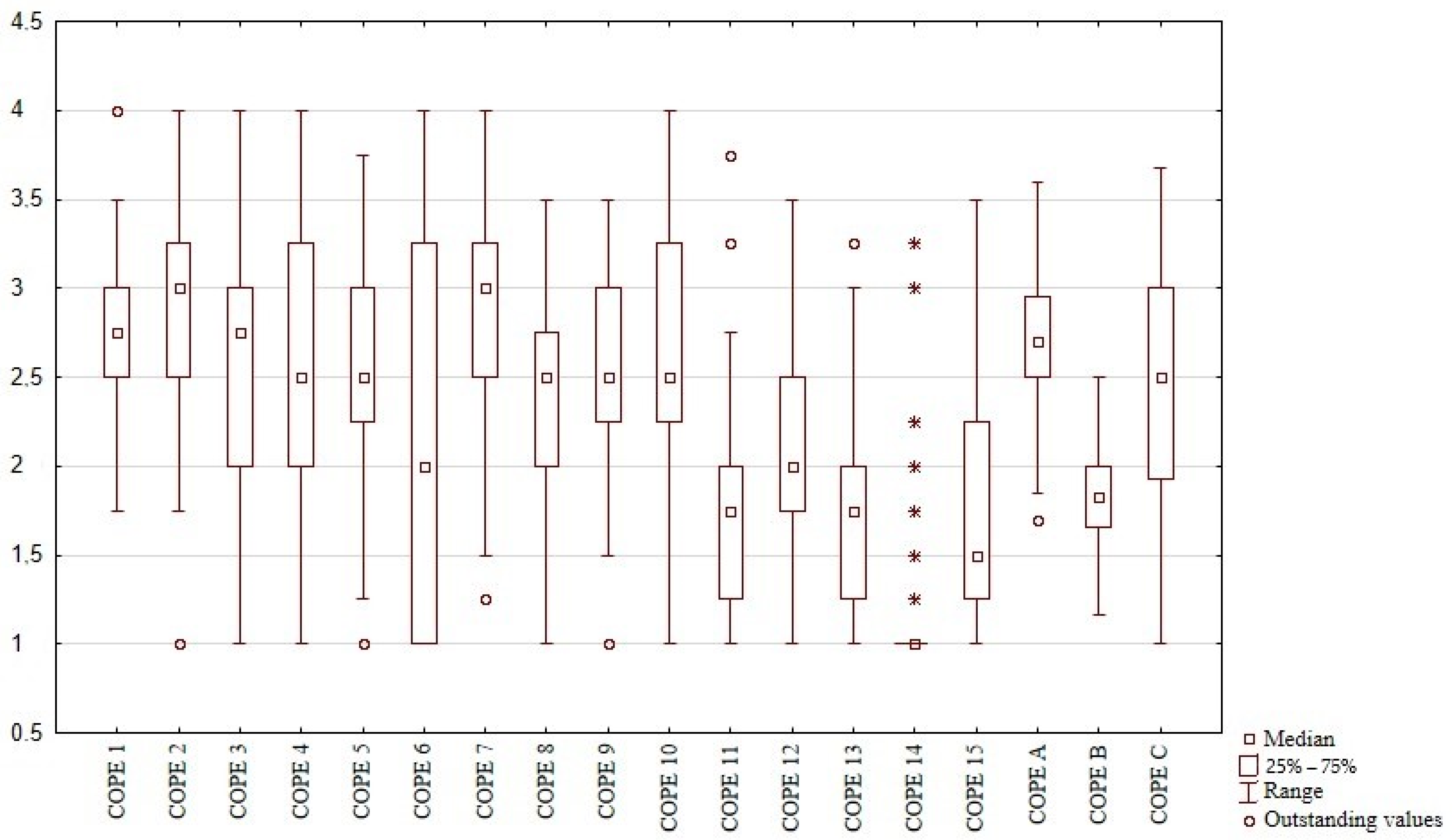
3. Results
3.1. Initial Assessment
3.1.1. Measures of Stress and MS-Related Variables
3.1.2. Measures of Stress and Other Factors
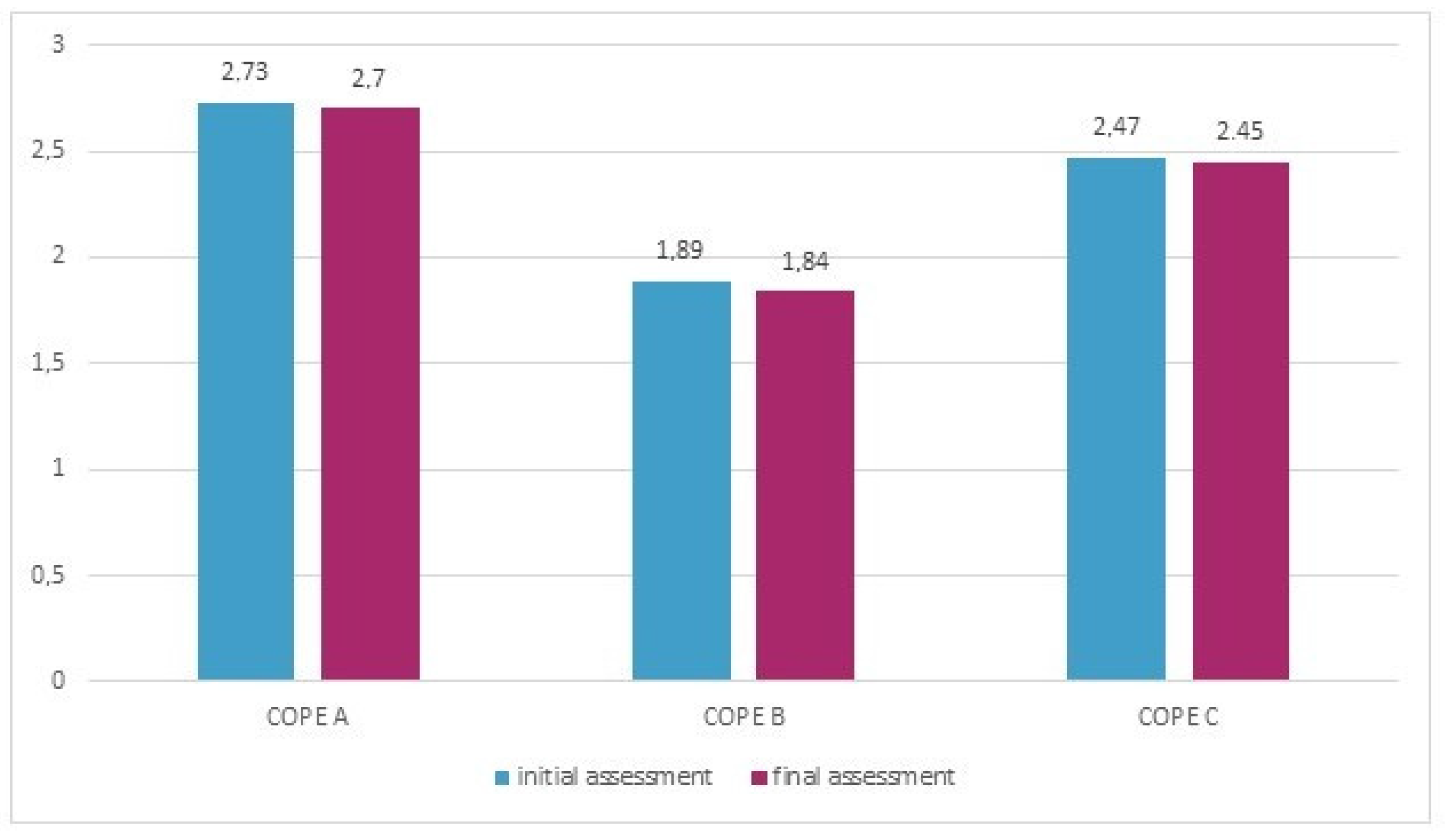
3.2. Assessment after a Year of Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- The Perceived Stress Scale (PSS-10) [15] consists of 10 items concerning the subjective perception of problems, situations and behaviors over the preceding four weeks. The score for each item ranges from 0 (never) to 4 (very often). The total score is the sum of responses to particular items, with a range of 0–40. The higher the score, the greater the level of perceived stress. The interpretation of the results is based on a 10-degree sten scale: scores within stens from 1–4 correspond with a low level of stress, within 5–6 to moderate and within 7–10 to a high level of stress [17]. The internal consistency of the Polish version of the PSS-10 reached a Cronbach’s alpha of 0.86 [17].
- The DS14 questionnaire [16] includes 14 items divided into two subscales (7 items each): negative affectivity (NEG) and social inhibition (SI). The score for each item ranges from 0 (false) to 4 (true). A result ≥10 in both subscales is used to categorize individuals as having a Type-D personality [17]. The internal consistency of the Polish version of the DS14 reached a Cronbach’s alpha of 0.86 for negative affectivity (NA) and 0.84 for social inhibition (SI) [17].
- 1. Active coping;2. Planning;3. Seeking social support for instrumental reasons4. Seeking social support for emotional reasons;5. Suppression of competing activities;6. Turning to religion;7. Positive reinterpretation and growth;8. Restraint coping;9. Acceptance;10. Focus on and venting of emotions;11. Denial;12. Mental disengagement;13. Behavioral disengagement;14. Alcohol–drug disengagement;15. Humor.General categories of coping strategies:
- -
- COPE A—active coping—this category consists of strategies 1, 2, 5, 7 and 8;
- -
- COPE B—avoidant behavior—this category consists of strategies 9, 11, 12, 13, 14 and 15;
- -
- COPE C—emotion-focused and seeking support—this category consists of strategies 3, 4, 6 and 10.
References
- Lublin, F.D.; Reingold, S.C.; Cohen, J.A.; Cutter, G.R.; Thompson, A.J.; Wolinsky, J.S.; Banwell, B.; Barkhof, F.; Bebo, B.; Calabresi, P.A.; et al. Defining the clinical course of multiple sclerosis. Neurology 2014, 83, 278–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Artemiadis, A.K.; Anagnostouli, M.C.; Alexopoulos, E.C. Stress as a risk factor for multiple sclerosis onset or relapse: A systematic review. Neuroepidemiology 2011, 36, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Benito-León, J. Stress and multiple sclerosis: What’s new? Neuroepidemiology 2011, 36, 121–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zänkert, S.; Bellingrath, S.; Wüst, S.; Kudielka, B.M. HPA axis responses to psychological challenge linking stress and disease: What do we know on sources of intra- and interindividual variability? Psychoneuroendocrinology 2019, 105, 86–97. [Google Scholar] [CrossRef]
- Kern, S.; Ziemssen, T. Brain–immune communication psychoneuroimmunology of multiple sclerosis. Mult. Scler. J. 2008, 14, 6–21. [Google Scholar] [CrossRef]
- Heesen, C.; Mohr, D.C.; Huitinga, I.; Then Bergh, F.; Gaab, J.; Otte, C.; Gold, S.M. Stress regulation in multiple sclerosis-Current issues and concepts. Mult. Scler. J. 2007, 13, 143–148. [Google Scholar] [CrossRef]
- Neustein, J.; Rymaszewska, J. Psychological consequences of multiple sclerosis and assistance possibilities. Physiother. Q. 2017, 25, 8–12. [Google Scholar] [CrossRef] [Green Version]
- Fisher, P.L.; Salmon, P.; Heffer-Rahn, P.; Huntley, C.; Reilly, J.; Cherry, M.G. Predictors of emotional distress in people with multiple sclerosis: A systematic review of prospective studies. J. Affect. Disord. 2020, 276, 752–764. [Google Scholar] [CrossRef]
- Briones-Buixassa, L.; Milà, R.; Ma Aragonès, J.; Bufill, E.; Olaya, B.; Arrufat, F.X. Stress and multiple sclerosis: A systematic review considering potential moderating and mediating factors and methods of assessing stress. Health Psychol. Open 2015, 2, 2055102915612271. [Google Scholar] [CrossRef] [Green Version]
- Carver, C.; Scheier, M.; Weintraub, J. Assessing coping strategies: A theoretically based approach. J. Personal. Soc. Psychol. 1989, 56, 267–283. [Google Scholar] [CrossRef]
- Lazarus, R.; Folkman, S. Stress, Appraisal and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Polman, C.; Reingold, S.; Banwell, B.; Clanet, M.; Cohen, J.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann. Neurol. 2011, 69, 292–302. [Google Scholar] [CrossRef] [Green Version]
- Beck, A.T.; Ward, C.H.; Medelson, M.; Mock, J.; Erbaugh, J. An inventory for measuring depression. Arch. Gen. Psychiatry 1961, 4, 561–571. [Google Scholar] [CrossRef] [Green Version]
- Folstein, M.; Folstein, S.; McHugh, P. “Mini-mental state”: A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 1975, 12, 189–198. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermrlstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Denollet, J. Type D personality: A potential risk factor refined. J. Psychosom. Res. 2000, 49, 255–266. [Google Scholar] [CrossRef] [Green Version]
- Juczynski, Z.; Oginska-Bulik, N. Narzędzia Pomiaru Stresu i Radzenia Sobie Ze Stresem; Pracownia Testów Psychologicznych: Warsaw, Poland, 2009. [Google Scholar]
- Kurtzke, J. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983, 33, 1444–1452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roxburgh, R.; Seaman, S.; Masterman, T.; Hensiek, A.; Sawcer, S.; Vukusic, S.; Achiti, I.; Confavreux, C.; Coustans, M.; le Page, E.; et al. Multiple Sclerosis Severity Score. Using disability and disease duration to rate disease severity. Neurology 2005, 64, 1144–1151. [Google Scholar] [CrossRef] [PubMed]
- Giovannoni, G.; Turner, B.; Gnanapavan, S.; Offiah, C.; Schmierer, K.; Marta, M. Is it time to target no evident disease activity (NEDA) in multiple sclerosis? Mult. Scler. Relat. Disord. 2015, 4, 329–333. [Google Scholar] [CrossRef] [Green Version]
- Scheffer, M.; Becker, J.; de Azeredo, L.A.; Grassi-Oliveira, R.; de Almeida, R.M.M. Subjective and physiological stress measurement in a multiple sclerosis sample and the relation with executive functions performance. J. Neural Transm. 2019, 126, 613–622. [Google Scholar] [CrossRef]
- Pritchard, M.; Elison-Bowers, P.; Birdsall, B. Impact of integrative restoration (iRest) meditation on perceived stress levels in multiple sclerosis and cancer outpatients. Stress Health 2010, 26, 233–237. [Google Scholar] [CrossRef]
- Sanaeinasab, H.; Saffari, M.; Hashempour, M.; Karimi Zarchi, A.A.; Alghamdi, W.A.; Koenig, H.G. Effect of a transactional model education program on coping effectiveness in women with multiple sclerosis. Brain Behav. 2017, 7, e00810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lamis, D.A.; Hirsch, J.K.; Pugh, K.C.; Topciu, R.; Nsamenang, S.A.; Goodman, A.; Duberstein, P.R. Perceived cognitive deficits and depressive symptoms in patients with multiple sclerosis: Perceived stress and sleep quality as mediators. Mult. Scler. Relat. Disord. 2018, 25, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Artemiadis, A.K.; Vervainioti, A.A.; Alexopoulos, E.C.; Rombos, A.; Anagnostouli, M.C.; Darviri, C. Stress management and multiple sclerosis: A randomized controlled trial. Arch. Clin. Neuropsychol. 2012, 27, 406–416. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Senders, A.; Bourdette, D.; Hanes, D.; Yadav, V.; Shinto, L. Perceived Stress in Multiple Sclerosis: The Potential Role of Mindfulness in Health and Well-Being. J. Evid.-Based Complement. Altern. Med. 2014, 19, 104–111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gallo, L.C.; Roesch, S.; Fortmann, A.; Carnethon, M.R.; Penedo, F.J.; Perreira, K.; Birnbaum-Weitzman, O.; Wassertheil-Smoller, D.; Castaneda, S.; Talavera, G.; et al. Associations of chronic stress burden, perceived stress, and traumatic stress with cardiovascular disease prevalence and risk factors in the HCHS/SOL Sociocultural Ancillary Study Linda. Psychosom. Med. 2014, 76, 468–475. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.M.; Wong, J.G.W.S.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, N.M.; Wong, P.C.; Tsang, K.W.T.; Chua, S.E. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can. J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cavallo, P.; Carpinelli, L.; Savarese, G. Perceived stress and bruxism in university students. BMC Res. Notes 2016, 9, 514. [Google Scholar] [CrossRef] [Green Version]
- Garber, M.C.; Huston, S.A.; Breese, C.R. Sources of stress in a pharmacy student population. Curr. Pharm. Teach. Learn. 2019, 11, 329–337. [Google Scholar] [CrossRef]
- Mills, S.D.; Azizoddin, D.; Racaza, G.Z.; Wallace, D.J.; Weisman, M.H.; Nicassio, P.M. The psychometric properties of the Perceived Stress Scale-10 among patients with systemic lupus erythematosus. Lupus 2017, 26, 1218–1223. [Google Scholar] [CrossRef]
- Trojan, D.; Arnold, D.; Shapiro, S.; Bar-Or, A.; Robinson, A.; Le Cruguel, J.; Narayanan, S.; Tartaglia, M.; Caramanos, Z.; Da Costa, D. Fatigue in post-poliomyelitis syndrome: Association with disease-related, behavioral, and psychosocial factors. PM&R 2009, 1, 442–449. [Google Scholar]
- Denollet, J.; Schiffer, A.A.; Spek, V. A general propensity to psychological distress affects cardiovascular outcomes: Evidence from research on the type D (distressed) personality profile. Circ. Cardiovasc. Qual. Outcomes 2010, 3, 546–557. [Google Scholar] [CrossRef] [Green Version]
- Beutel, M.E.; Wiltink, J.; Till, Y.; Wild, P.S.; Münzel, T.; Ojeda, F.M.; Zeller, T.; Schnabel, R.B.; Lackner, K.; Blettner, M.; et al. Type D personality as a cardiovascular risk marker in the general population: Results from the gutenberg health study. Psychother. Psychosom. 2012, 81, 108–117. [Google Scholar] [CrossRef] [PubMed]
- Jandackova, V.K.; Koenig, J.; Jarczok, M.N.; Fischer, J.E.; Thayer, J.F. Potential biological pathways linking Type-D personality and poor health: A cross-sectional investigation. PLoS ONE 2017, 12, e0176014. [Google Scholar] [CrossRef] [Green Version]
- Oginska-Bulik, N. Czy osobowość sprzyja etiopatogenezie chorób? Nowe kierunki badań-osobowość typu D. Now Psychol. 2006, 11, 69–79. [Google Scholar]
- Strober, L.B. Personality in multiple sclerosis (MS): Impact on health, psychological well-being, coping, and overall quality of life. Psychol. Health Med. 2017, 22, 152–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Demirci, S.; Demirci, K.; Demirci, S. The effect of type D personality on quality of life in patients with multiple sclerosis. Noropsikiyatri Ars. 2017, 54, 272–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lorefice, L.; Fenu, G.; Frau, J.; Coghe, G.; Marrosu, M.G.; Cocco, E. The burden of multiple sclerosis and patients’ coping strategies. BMJ Support. Palliat. Care 2018, 8, 38–40. [Google Scholar] [CrossRef] [PubMed]
- Gazioglu, S.; Cakmak, V.A.; Ozkorumak, E.; Usta, N.C.; Ates, C.; Boz, C. Personality traits of patients with multiple sclerosis and their relationship with clinical characteristics. J. Nerv. Ment. Dis. 2014, 202, 408–411. [Google Scholar] [CrossRef]
- Goretti, B.; Portaccio, E.; Zipoli, V.; Razzolini, L.; Amato, M.P. Coping strategies, cognitive impairment, psychological variables and their relationship with quality of life in multiple sclerosis. Neurol. Sci. 2010, 31, 227–230. [Google Scholar] [CrossRef]
- Nielsen-Prohl, J.; Saliger, J.; Güldenberg, V.; Breier, G.; Karbe, H. Stress-stimulated volitional coping competencies and depression in multiple sclerosis. J. Psychosom. Res. 2013, 74, 221–226. [Google Scholar] [CrossRef]
- Kroencke, D.C.; Denney, D.R. Stress and coping in multiple sclerosis: Exacerbation, remission and chronic subgroups. Mult. Scler. J. 1999, 5, 89–93. [Google Scholar] [CrossRef]
- Rätsep, T.; Kallasmaa, T.; Pulver, A.; Gross-Paju, K. Personality as a predictor of coping efforts in patients with multiple sclerosis. Mult. Scler. J. 2000, 6, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Gioia, M.C.; Cerasa, A.; Valentino, P.; Fera, F.; Nisticò, R.; Liguori, M.; Lanza, P.; Quattrone, A. Neurofunctional correlates of personality traits in relapsing-remitting multiple sclerosis: An fMRI study. Brain Cogn. 2009, 71, 320–327. [Google Scholar] [CrossRef]
- Lynch, S.G.; Kroencke, D.C.; Denney, D.R. The relationship between disability and depression in multiple sclerosis: The role of uncertainty, coping, and hope. Mult. Scler. J. 2001, 7, 411–416. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.F.; Tennant, C.C.; Sharrock, M.; Hodgkinson, S.; Dunn, S.M.; Pollard, J.M. Relationship between stress and relapse in multiple sclerosis: Part II. Direct and indirect relationships. Mult. Scler. J. 2006, 12, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, C.E.; Foley, F.W.; Rao, S.M.; Bernardin, L.J.; Lee, H.; Genderson, M.W. Stress and course of disease in multiple sclerosis. Behav. Med. 1999, 25, 110–116. [Google Scholar] [CrossRef]
- Nowaczyk, N.; Cierpialkowska, L. Psychological profiles of patients with multiple sclerosis based on Hobfoll’s conservation of resources theory. Health Psychol. Rep. 2016, 4, 332–339. [Google Scholar] [CrossRef]
- Lode, K.; Bru, E.; Klevan, G.; Myhr, K.M.; Nyland, H.; Larsen, J.P. Coping with multiple sclerosis: A 5-year follow-up study. Acta Neurol. Scand. 2010, 122, 336–342. [Google Scholar] [CrossRef]
- Buljevac, D.; Hop, W.C.J.; Reedeker, W.; Janssens, A.C.J.W.; Van Doorn, P.A.; Hintzen, R.Q. Self reported stressful life events and exacerbations in multiple sclerosis: Prospective study. BMJ 2003, 327, 646. [Google Scholar] [CrossRef] [Green Version]
- Abdollahpour, I.; Nedjat, S.; Mansournia, M.A.; Eckert, S.; Weinstock-Guttman, B. Stress-full life events and multiple sclerosis: A population-based incident case-control study. Mult. Scler. Relat. Disord. 2018, 26, 168–172. [Google Scholar] [CrossRef]
- Mohr, D.C.; Hart, S.L.; Julian, L.; Cox, D.; Pelletier, D. Association between stressful life events and exacerbation in multiple sclerosis: A meta-analysis. Br. Med. J. 2004, 328, 731–733. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitsonis, C.I.; Zervas, I.M.; Mitropoulos, P.A.; Dimopoulos, N.P.; Soldatos, C.R.; Potagas, C.M.; Sfagos, C.A. The impact of stressful life events on risk of relapse in women with multiple sclerosis: A prospective study. Eur. Psychiatry 2008, 23, 497–504. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.F.; Tennant, C.C.; Sharrock, M.; Hodgkinson, S.; Dunn, S.M.; Pollard, J.D. Relationship between stress and relapse in multiple sclerosis: Part I. Important features. Mult. Scler. J. 2006, 12, 453–464. [Google Scholar] [CrossRef] [PubMed]
- Palumbo, R.; Fontanillas, L.; Salmaggi, A.; La Mantia, L.; Milanese, C. Stressful life events and multiple sclerosis: A retrospective study. Ital. J. Neurol. Sci. 1998, 19, 259–260. [Google Scholar] [CrossRef]
- Liu, X.J.; Ye, H.X.; Li, W.P.; Dai, R.; Chen, D.; Jin, M. Relationship between psychosocial factors and onset of multiple sclerosis. Eur. Neurol. 2009, 62, 130–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kern, S.; Schrempf, W.; Schneider, H.; Schultheiß, T.; Reichmann, H.; Ziemssen, T. Neurological disability, psychological distress, and health-related quality of life in MS patients within the first three years after diagnosis. Mult. Scler. J. 2009, 15, 752–758. [Google Scholar] [CrossRef] [PubMed]
- Riise, T.; Mohr, D.C.; Munger, K.L.; Rich-Edwards, J.W.; Kawachi, I.; Ascherio, A. Stress and the risk of multiple sclerosis. Neurology 2011, 76, 1866–1871. [Google Scholar] [CrossRef] [Green Version]
- Gasperini, C.; Grasso, M.G.; Fiorelli, M.; Millefiorini, E.; Morino, S.; Anzini, A.; Colleluori, A.; Salvetti, M.; Buttinelli, C.; Pozzilli, C. A controlled study of potential risk factors preceding exacerbation in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 1995, 59, 303–305. [Google Scholar] [CrossRef] [Green Version]
- Oveisgharan, S.; Hosseini, S.; Arbabi, M.; Nafissi, S. Stress differentially predicts multiple sclerosis relapses. Neurol. Asia 2014, 19, 53–58. [Google Scholar]
- Somer, E.; Golan, D.; Dishon, S.; Cuzin-Disegni, L.; Lavi, I.; Miller, A. Patients with multiple sclerosis in a war zone: Coping strategies associated with reduced risk for relapse. Mult. Scler. J. 2010, 16, 463–471. [Google Scholar] [CrossRef]
- Nisipeanu, P.; Korczyn, A. Psychological stress as risk factor for exacerbations in multiple sclerosis. Neurology 1993, 43, 1311–1312. [Google Scholar] [CrossRef] [PubMed]
- McCabe, M. A longitudinal study of coping strategies and quality of life among people with multiple sclerosis. J. Clin. Psychol. Med. Settings 2006, 13, 367–377. [Google Scholar] [CrossRef]
- Dennison, L.; Moss-Morris, R.; Chalder, T. A review of psychological correlates of adjustment in patients with multiple sclerosis. Clin. Psychol. Rev. 2009, 29, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Aikens, J.E.; Fischer, J.S.; Namey, M.; Rudick, R.A. A replicated prospective investigation of life stress, coping, and depressive symptoms in multiple sclerosis. J. Behav. Med. 1997, 20, 433–445. [Google Scholar] [CrossRef] [PubMed]
- Barlow, J.; Turner, A.; Edwards, R.; Gilchrist, M. A randomised controlled trial of lay-led self-management for people with multiple sclerosis. Patient Educ. Couns. 2009, 77, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Bombardier, C.; Cunniffe, M.; Wadhwani, R.; Gibbons, L.; Blake, K.; Kraft, G. The Efficacy of Telephone Counseling for Health Promotion in People With Multiple Sclerosis: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2008, 89, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Tesar, N.; Bandion, K.; Baumhackl, U. Efficacy of a neuropsychological training programme for patients with multiple sclerosis -A randomised controlled trial. Wien. Klin. Wochenschr. 2005, 117, 747–754. [Google Scholar] [CrossRef] [PubMed]

| Mean | SD | MIN | MAX | Median | |
|---|---|---|---|---|---|
| Disease duration (years) | 7.25 | 5.34 | 1 | 28 | 6 |
| Duration of treatment | 3.44 | 3.07 | 0.5 | 13 | 2.5 |
| EDSS | 2.05 | 5.4 | 1 | 6 | 2 |
| MSSS | 3.28 | 1.61 | 0.76 | 6.46 | 2.87 |
| Number | % | |
|---|---|---|
| Place of residence | ||
| Rural | 22 | 33.8 |
| Urban | 43 | 66.2 |
| Marital status | ||
| Single | 13 | 20 |
| Married | 40 | 61.5 |
| Divorced | 5 | 7.7 |
| Other | 7 | 10.8 |
| Level of education | ||
| Vocational | 5 | 7.7 |
| Secondary education | 24 | 36.9 |
| Higher education | 36 | 55.4 |
| Occupational status | ||
| Studying | 2 | 3 |
| Working | 52 | 80 |
| Unnemployed | 4 | 6.2 |
| Pension/retiremet | 7 | 10.8 |
| Mean | SD | MIN | MAX | Median | |
|---|---|---|---|---|---|
| PSS-10 | 16.9 | 6.7 | 3.0 | 28 | 17 |
| DS-14 NEG | 12.4 | 7.1 | 0 | 27 | 12 |
| DS-14 SI | 8.97 | 6.38 | 0 | 25 | 8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kotas, R.; Nowakowska-Kotas, M.; Budrewicz, S.; Pokryszko-Dragan, A. The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course. J. Clin. Med. 2021, 10, 3916. https://doi.org/10.3390/jcm10173916
Kotas R, Nowakowska-Kotas M, Budrewicz S, Pokryszko-Dragan A. The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course. Journal of Clinical Medicine. 2021; 10(17):3916. https://doi.org/10.3390/jcm10173916
Chicago/Turabian StyleKotas, Roman, Marta Nowakowska-Kotas, Sławomir Budrewicz, and Anna Pokryszko-Dragan. 2021. "The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course" Journal of Clinical Medicine 10, no. 17: 3916. https://doi.org/10.3390/jcm10173916
APA StyleKotas, R., Nowakowska-Kotas, M., Budrewicz, S., & Pokryszko-Dragan, A. (2021). The Level of Stress and Coping Strategies in Patients with Multiple Sclerosis and Their Relationships with the Disease Course. Journal of Clinical Medicine, 10(17), 3916. https://doi.org/10.3390/jcm10173916







