Portomesenteric Vein Thrombosis after Bariatric Surgery: An Online Survey
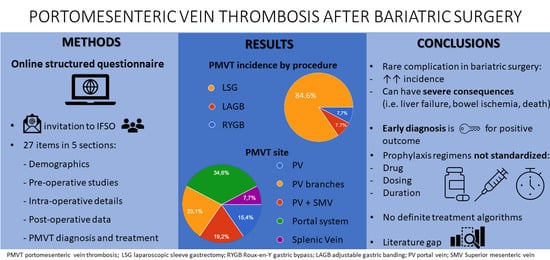
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sampling Plan and Invitation
2.2. Statistical Analysis
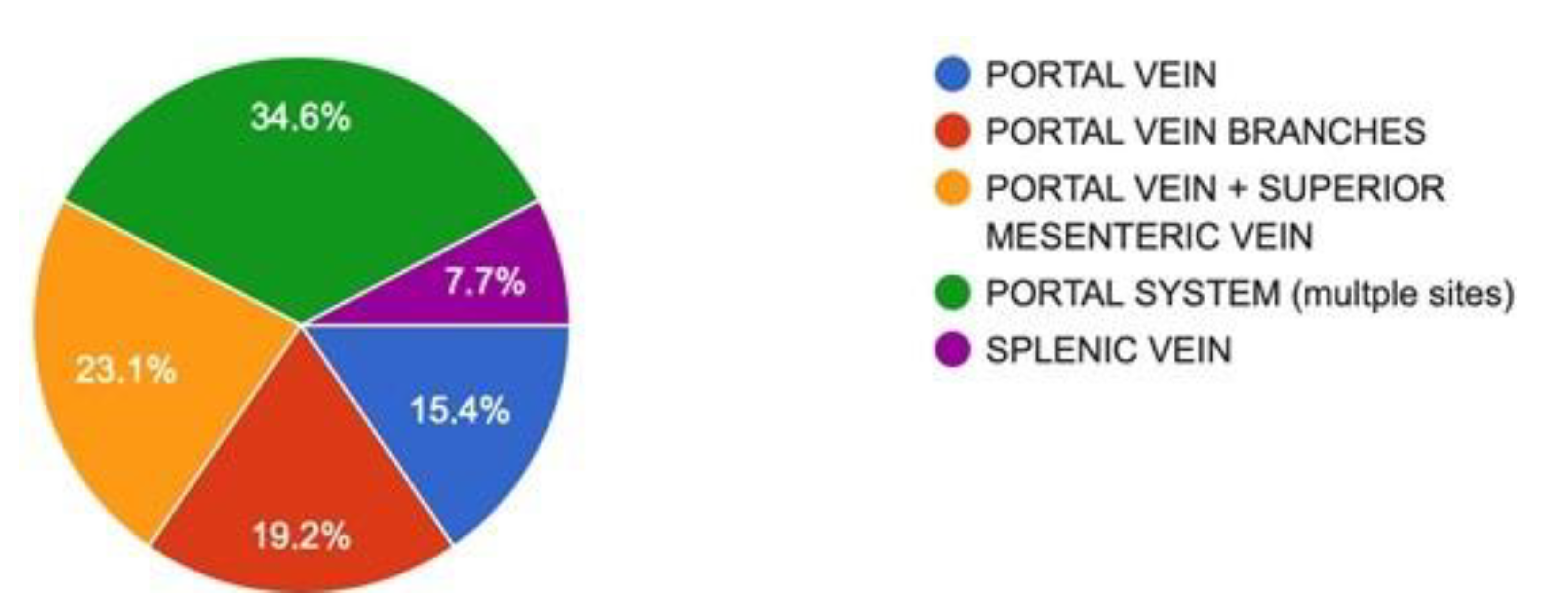
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
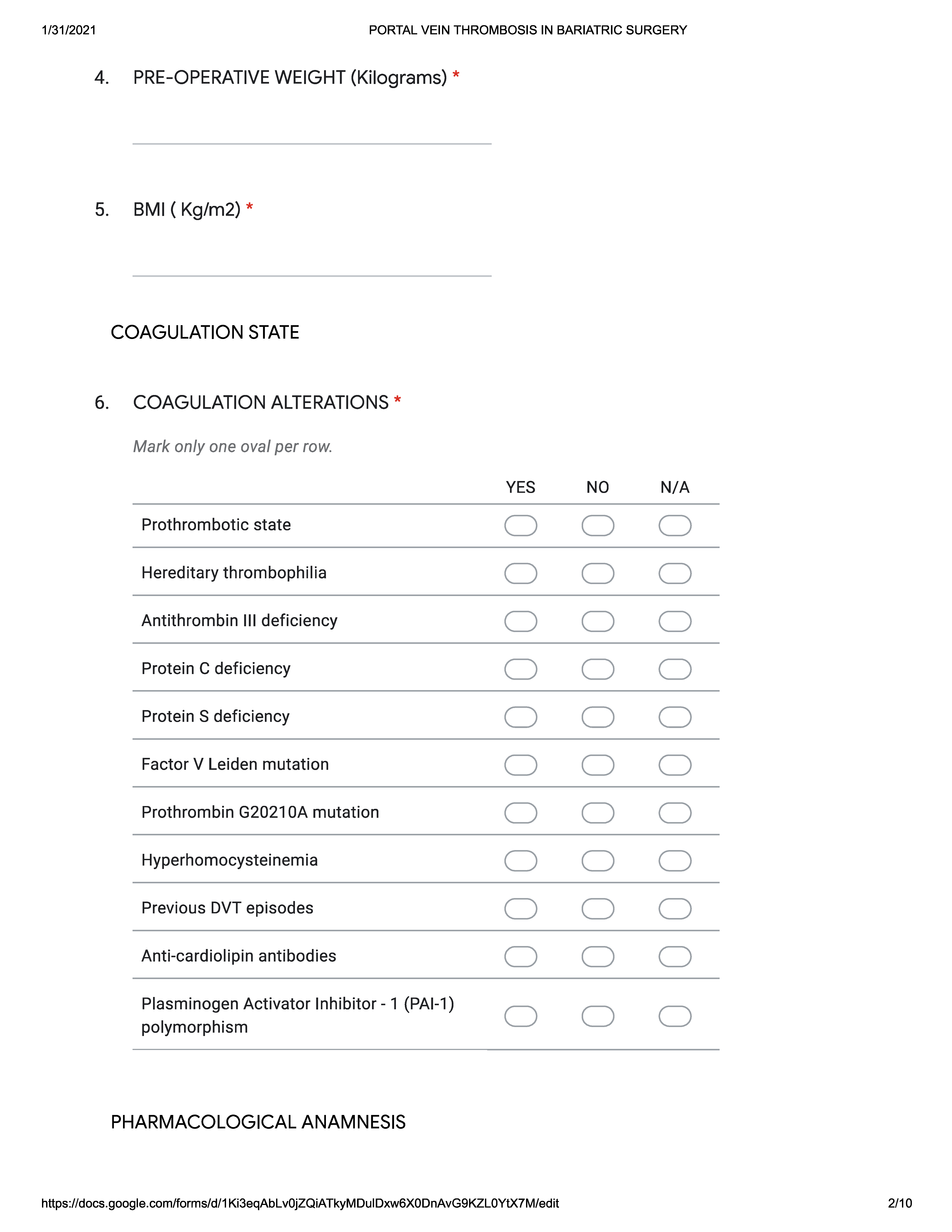
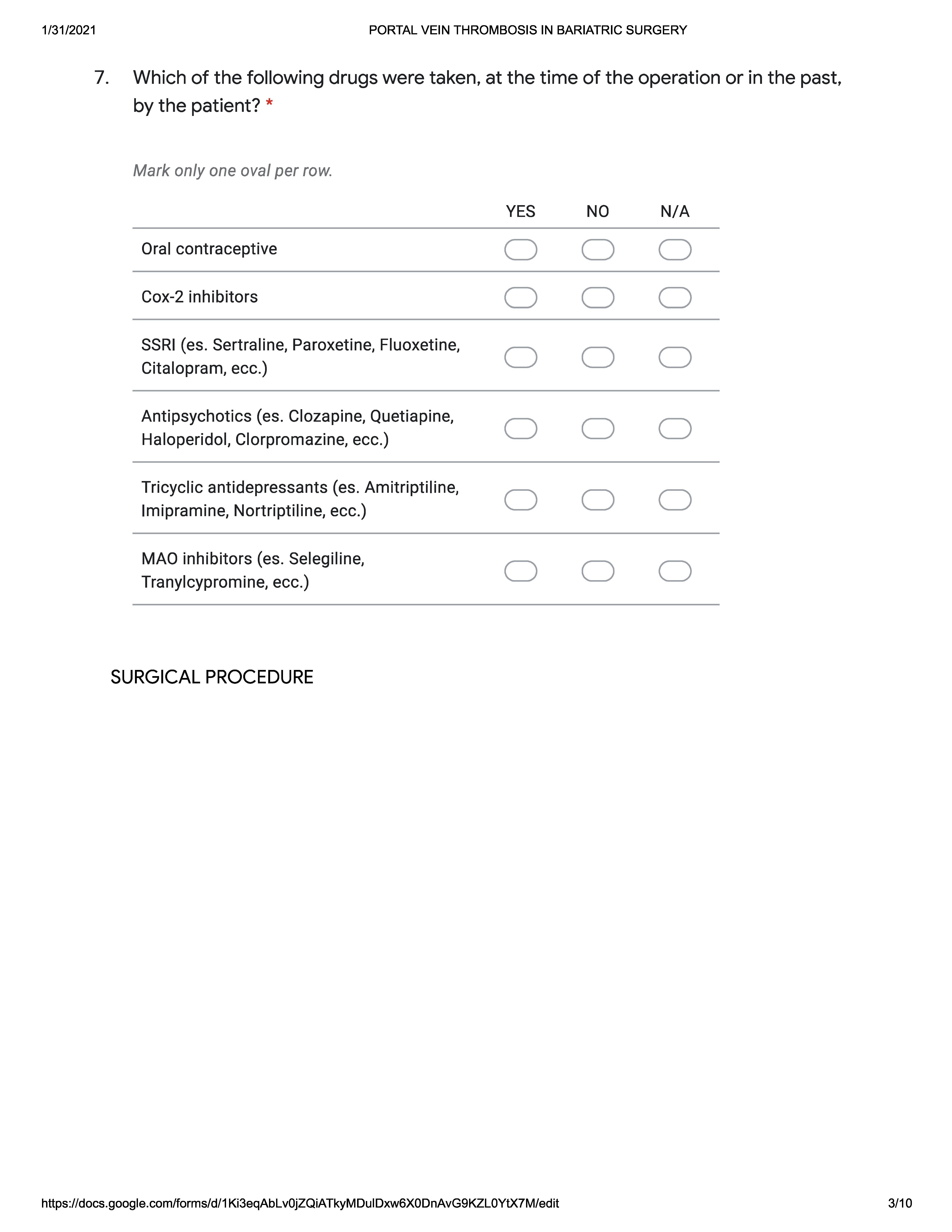
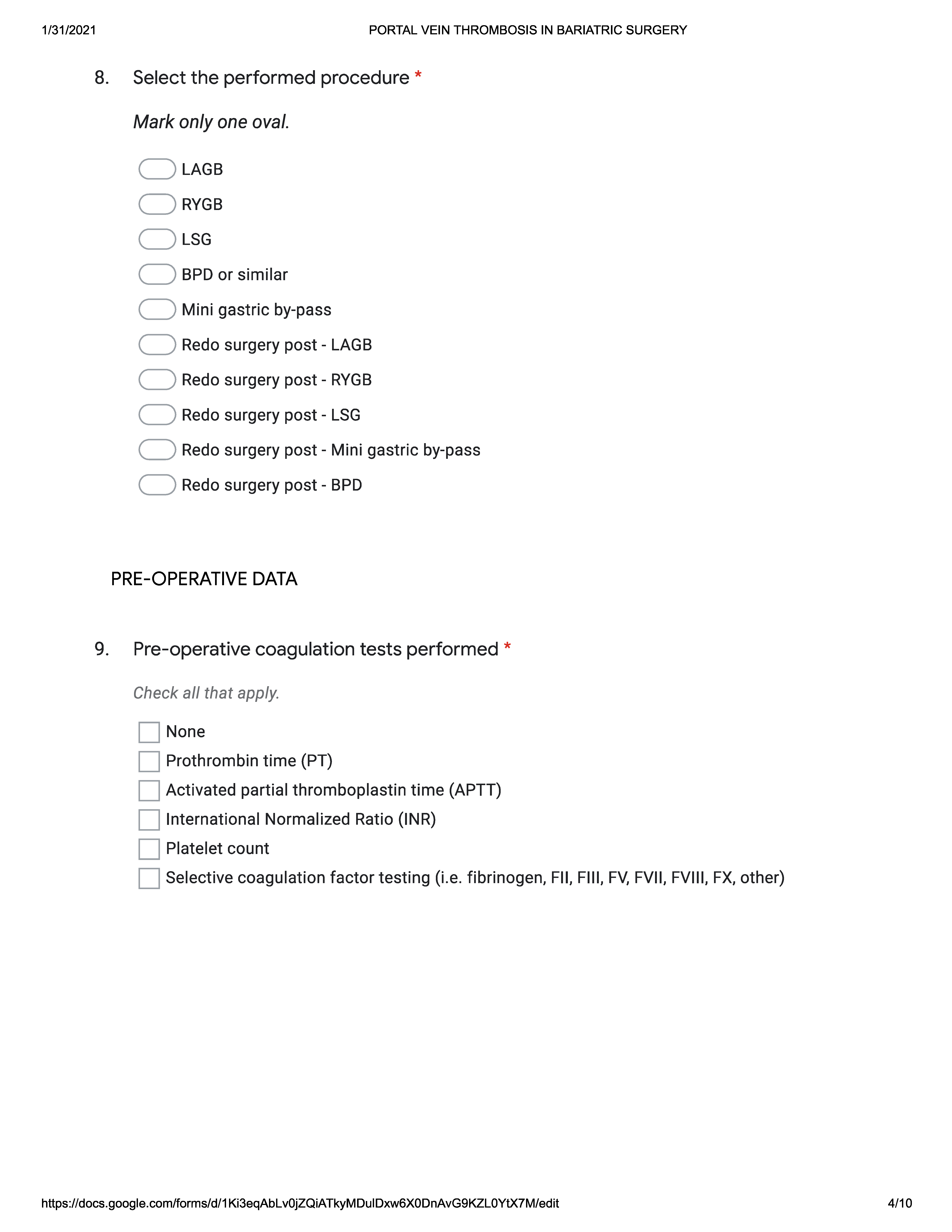
Appendix A




References
- Welbourn, R.; Pournaras, D.J.; Dixon, J.; Higa, K.; Kinsman, R.; Ottosson, J.; Ramos, A.; van Wagensveld, B.; Walton, P.; Weiner, R.; et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Second IFSO Global Registry Report 2013–2015. Obes. Surg. 2018, 28, 313–322. [Google Scholar] [CrossRef]
- Phillips, B.T.; Shikora, S.A. The history of metabolic and bariatric surgery: Development of standards for patient safety and efficacy. Metabolism 2018, 79, 97–107. [Google Scholar] [CrossRef]
- Ramos, A.; Kow, L.; Brown, W.; Welbourn, R.; Dixon, J.; Kinsman, R.; Walton, P. Fifth IFSO Global Registry Report-2019. Obes. Surg. 2019, 29, 782–793. [Google Scholar]
- Sangiorgi, G.M.; Cereda, A.; Porchetta, N.; Benedetto, D.; Matteucci, A.; Bonanni, M.; Chiricolo, G.; De Lorenzo, A. Endovascular Bariatric Surgery as Novel Minimally Invasive Technique for Weight Management in the Morbidly Obese: Review of the Literature. Nutrients 2021, 13, 2541. [Google Scholar] [CrossRef]
- Tan, S.B.M.; Greenslade, J.; Martin, D.; Talbot, M.; Loi, K.; Hopkins, G. Portomesenteric vein thrombosis in sleeve gastrectomy: A 10-year review. Surg. Obes. Relat. Dis. 2018, 14, 271–275. [Google Scholar] [CrossRef]
- Minoda, A.M.; Cadete, R.B.F.; Teixeira, S.R.; Muglia, V.F.; Elias Junior, J.; de Melo-Leite, A.F. The ABCD of portal vein thrombosis: A systematic approach. Radiol. Bras. 2020, 53, 424–429. [Google Scholar] [CrossRef]
- Karaman, K.; Aziret, M.; Bal, A.; Öter, V.; Ercan, M.; Bostancı, E.B. Porto-mesenteric venous thrombosis after laparoscopic sleeve gastrectomy: A case report and systematic review of the 104 cases. Obes. Res. Clin. Pract. 2018, 12, 317–325. [Google Scholar] [CrossRef]
- Parikh, M.; Somoza, E.; Chopra, A.; Friedman, D.; Chui, P.; Park, J.; Ude-Welcome, A.; Saunders, J.K. Thrombophilia prevalence in patients seeking laparoscopic sleeve gastrectomy: Extended chemoprophylaxis may decrease portal vein thrombosis rate. Surg. Obes. Relat. Dis. 2020, 16, 839–843. [Google Scholar] [CrossRef]
- Danion, J.; Genser, L.; Scatton, O. Sleeve Gastrectomy: You Might Lose your Liver! Obes. Surg. 2019, 29, 350–352. [Google Scholar] [CrossRef]
- Schmitz, S.M.T.; Kroh, A.; Koch, A.; Brozat, J.F.; Stier, C.; Neumann, U.P.; Ulmer, T.F.; Alizai, P.H. Comparison of Liver Recovery After Sleeve Gastrectomy and Roux-en-Y-Gastric Bypass. Obes. Surg. 2021, 31, 3218–3226. [Google Scholar] [CrossRef]
- Shoar, S.; Saber, A.A.; Rubenstein, R.; Safari, S.; Brethauer, S.A.; Al-Thani, H.; Asarian, A.P.; Aminian, A. Portomesentric and splenic vein thrombosis (PMSVT) after bariatric surgery: A systematic review of 110 patients. Surg. Obes. Relat. Dis. 2018, 14, 47–59. [Google Scholar] [CrossRef] [PubMed]
- Goodfellow, M.; Courtney, M.; Upadhyay, Y.; Marsh, R.; Mahawar, K. Mesenteric Venous Thrombosis Due to Coronavirus in a Post Roux-en-Y Gastric Bypass Patient: A Case Report. Obes. Surg. 2021, 31, 2308–2310. [Google Scholar] [CrossRef] [PubMed]
- Ofosu, A.; Ramai, D.; Novikov, A.; Sushma, V. Portal Vein Thrombosis in a Patient with COVID-19. Am. J. Gastroenterol. 2020, 115, 1545–1546. [Google Scholar] [CrossRef] [PubMed]
- Parry, A.H.; Wani, A.H.; Yaseen, M. Acute Mesenteric Ischemia in Severe Coronavirus-19 (COVID-19): Possible Mechanisms and Diagnostic Pathway. Acad. Radiol. 2020, 27, 1190. [Google Scholar] [CrossRef]
- Burkey, C.; Teng, C.; Hussein, K.I.; Sabetta, J. Cytomegalovirus (CMV)-associated portal vein thrombosis in a healthy, immunocompetent man. BMJ Case Rep. 2020, 13, e238645. [Google Scholar] [CrossRef]
- Goitein, D.; Matter, I.; Raziel, A.; Keidar, A.; Hazzan, D.; Rimon, U.; Sakran, N. Portomesenteric thrombosis following laparoscopic bariatric surgery: Incidence, patterns of clinical presentation, and etiology in a bariatric patient population. JAMA Surg. 2013, 148, 340–346. [Google Scholar] [CrossRef]
- Chawla, Y.K.; Bodh, V. Portal vein thrombosis. J. Clin. Exp. Hepatol. 2015, 5, 22–40. [Google Scholar] [CrossRef] [Green Version]
- Osman, A.M.A.; Helmy, A.S.; Mikhail, S.; AlAyat, A.A.; Serour, D.K.; Ibrahim, M.Y. Early Effects of Laparoscopic Sleeve Gastrectomy and Laparoscopic One-Anastomosis Gastric Bypass on Portal Venous Flow: A Prospective Cohort Study. Obes. Surg. 2021, 31, 2410–2418. [Google Scholar] [CrossRef]
- Godoroja, D.; Hainarosie, D.; Zaharencu, A.; Copaescu, C. Portal Vein Thrombosis a Rare but Life-threatening Complication after Laparoscopic Sleeve Gastrectomy: A 5 Years Study in a Bariatric Center of Excellence. Chirurgia 2019, 114, 711–724. [Google Scholar] [CrossRef] [PubMed]
- James, A.W.; Rabl, C.; Westphalen, A.C.; Fogarty, P.F.; Posselt, A.M.; Campos, G.M. Portomesenteric venous thrombosis after laparoscopic surgery: A systematic literature review. Arch. Surg. 2009, 144, 520–526. [Google Scholar] [CrossRef]
- Bani Hani, M.N.; Al Manasra, A.R.A.; Obeidat, F.; Al-Omari, M.H.; Bani Hani, F. Portomesenteric Venous Thrombosis Post-Laparoscopic Sleeve Gastrectomy: Do Energy Systems Pose as Instigating Factor to This Infrequent Complication? Clin. Med. Insights Case Rep. 2019, 12. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| N Patients | 26 |
| Surgery | LSG 22/RYGB 2/LAGB 2 |
| Sex | 14 F/12 M |
| Median pre-op weight | 129.26 ± 20.79 kg |
| Median BMI | 44.55 ± 5.32 kg/m2 |
| Coagulation disorder | 3 (12%) |
| Previous DVT | 3 (12%) |
| SSRIs | 4 (16.6%) |
| Symptom | Patients (%) |
|---|---|
| Abdominal pain | 26 (96.15%) |
| Fever | 7 (26.9%) |
| Anorexia | 5 (19.2%) |
| Nausea | 12 (46.15%) |
| Vomit | 7 (26.9%) |
| Diarrhoea | 3 (11.5%) |
| Intestinal bleeding | 1 (3.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carrano, F.M.; Weiner, S.; Elshafei, M.; Ahmed, S.; Talishinskiy, T.; Tognoni, V.; Mahawar, K.; Di Lorenzo, N. Portomesenteric Vein Thrombosis after Bariatric Surgery: An Online Survey. J. Clin. Med. 2021, 10, 4024. https://doi.org/10.3390/jcm10174024
Carrano FM, Weiner S, Elshafei M, Ahmed S, Talishinskiy T, Tognoni V, Mahawar K, Di Lorenzo N. Portomesenteric Vein Thrombosis after Bariatric Surgery: An Online Survey. Journal of Clinical Medicine. 2021; 10(17):4024. https://doi.org/10.3390/jcm10174024
Chicago/Turabian StyleCarrano, Francesco Maria, Sylvia Weiner, Moustafa Elshafei, Saleem Ahmed, Toghrul Talishinskiy, Valeria Tognoni, Kamal Mahawar, and Nicola Di Lorenzo. 2021. "Portomesenteric Vein Thrombosis after Bariatric Surgery: An Online Survey" Journal of Clinical Medicine 10, no. 17: 4024. https://doi.org/10.3390/jcm10174024
APA StyleCarrano, F. M., Weiner, S., Elshafei, M., Ahmed, S., Talishinskiy, T., Tognoni, V., Mahawar, K., & Di Lorenzo, N. (2021). Portomesenteric Vein Thrombosis after Bariatric Surgery: An Online Survey. Journal of Clinical Medicine, 10(17), 4024. https://doi.org/10.3390/jcm10174024