Following Pediatric and Adult IBD Patients through the COVID-19 Pandemic: Changes in Psychosocial Burden and Perception of Infection Risk and Harm over Time
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Questionnaires
- Baseline characteristics including age, sex, country of birth, height and weight, area of living (urban or rural);
- Vaccination status for vaccinations against measles, mumps, rubella, varicella, zoster, pneumococcus and COVID-19 (2nd survey only). At both time points we also asked for influenza vaccinations in the last winter season (prior and during pandemic) and whether participants and healthy household members would choose to be vaccinated against COVID-19, if offered;
- Socio-economic status relating to the living situation, size of flat/house and room number, number and age range of household members, employment status, educational level and household income [9];
- IBD-related questions including IBD phenotype, age at diagnosis, complications, current disease activity and disease flares during the pandemic and detailed information on medication and non-drug supportive therapy for IBD and non-IBD related comorbidities;
- COVID-19 related questions regarding symptoms suggestive for COVID-19 within the last two weeks and since the beginning of the pandemic as well as all previous PCR tests from nasopharyngeal swabs and serology for SARS-CoV-2 antibodies in patients and household members [9]. Furthermore, this section included questions on employment situation, jobs with high number of in-person contacts (teacher, nursing home, health care professionals, grocery, pharmacy, police etc.) and therefore with potentially higher risk of COVID-19 infection, and any conditions or comorbidity with known increased risk for severe COVID-19 outcome;
- Impact on health care utilization for IBD, changes in medication, missed or cancelled clinic visits and diagnostic procedures due to the pandemic and experience with telemedicine;
- Effects on daily life relating to the situation at home, at work or at school, in the family, use of public transport, physical activity, sleeping and eating behavior, alcohol and tobacco habits, involuntary or voluntary weight change, general well-being and loneliness;
- Effects on psychological stress and quality of life were assessed with validated instruments. We used the German version of the Perceived Stress Questionnaire (PSQ) [11,12], which assesses subjectively experienced stress during the last 4 weeks in four domains (“worries”, “tension”, “joy”, demands”) with five items each and a total score ranging from 0 to 100. The domain “joy”, which is positively coded, is transformed into “lack of joy” to calculate the total PSQ score. A high PSQ score reflects a high level of perceived stress. Adult IBD patients and both pIBD parents reflecting their own situation answered the PSQ. To assess IBD-related quality of life, the Short Inflammatory Bowel Disease Questionnaire (SIBDQ) was used for adults [13,14] and the IMPACT III for pediatric patients [15,16]. Results are shown as mean with 95% CI for PSQ, and as mean with SD for SIBDQ and IMPACT III, in agreement with published references [13,15,17].
- Patients’ self-perceived risk and harm of COVID-19: On a scale from 1 (low) to 7 (high), adult patients estimated their risk to acquire COVID-19 infection (perceived risk) and their risk for a severe disease course if they get infected (perceived harm). Parents judged perceived risk and harm for their IBD affected child. Values of <3 and >3 were considered low and high perceived risk/harm, respectively.
2.3. Scoring for Increased Risk for Severe COVID-19 Outcomes (SIRSCO)
2.4. SARS-CoV2 Serology
2.5. Statistical Analysis
3. Results
3.1. Participants and Cohort Description by Age Groups
3.2. Socioeconomic Factors
3.3. COVID-19 Related Symptoms and Testing for Infection
3.4. Impact of the Pandemic on IBD-Related Health Care
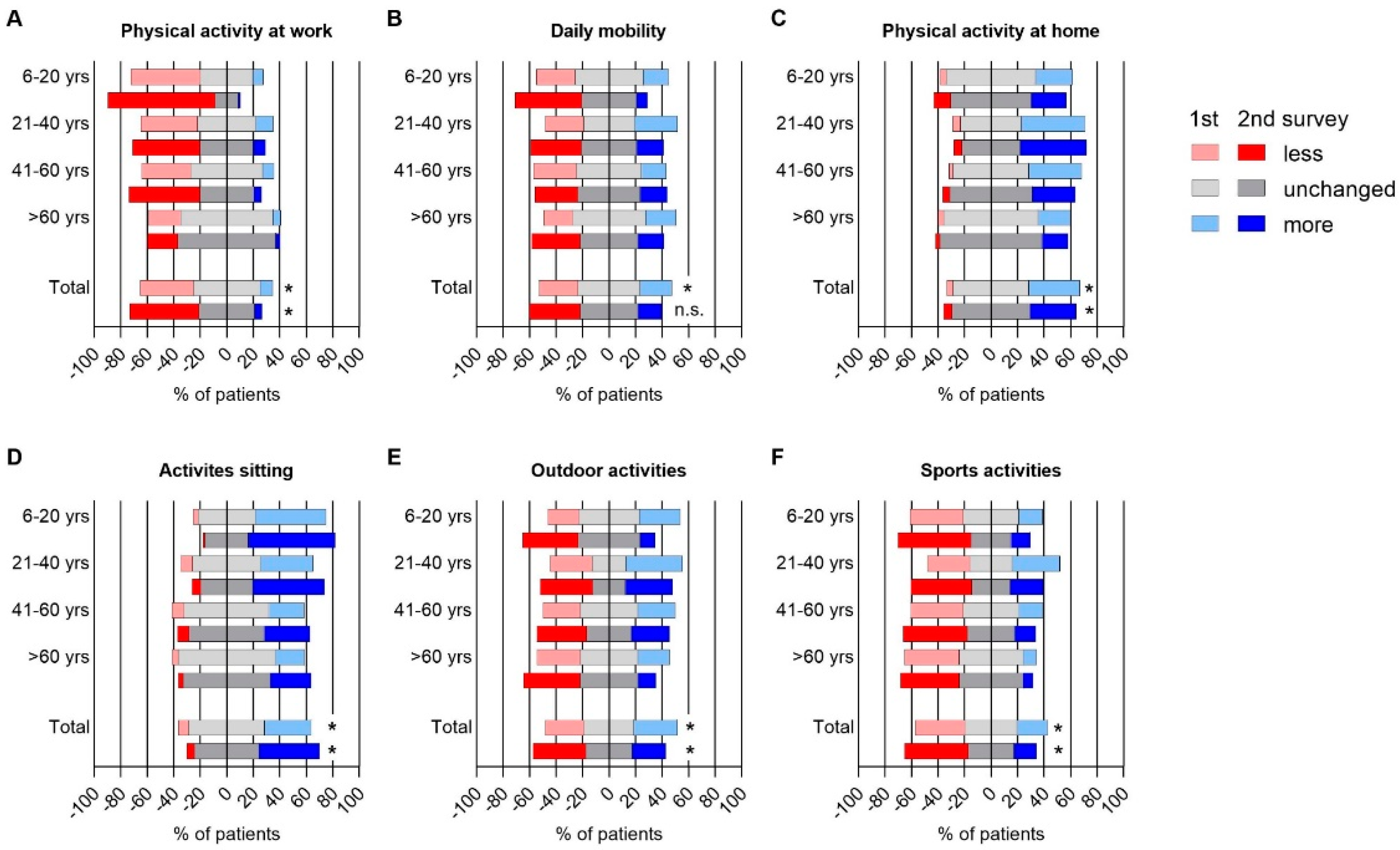
3.5. Impact of the Pandemic on Daily Life
3.6. Impact of the Pandemic on Self-Perceived Stress and Quality of Life
3.7. Perceived Risk to Acquire COVID-19 and Perceived Harm for Severe Outcome in Case of Infection
3.7.1. Univariate Regression Analysis
3.7.2. Multivariable Regression Analysis
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W.; et al. Transmission of 2019-nCoV Infection from an Asymptomatic Contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef] [Green Version]
- Turner, D.; Huang, Y.; Martin-de-Carpi, J.; Aloi, M.; Focht, G.; Kang, B.; Zhou, Y.; Sanchez, C.; Kappelman, M.D.; Uhlig, H.H.; et al. Corona Virus Disease 2019 and Paediatric Inflammatory Bowel Diseases: Global Experience and Provisional Guidance (March 2020) from the Paediatric IBD Porto Group of European Society of Paediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Allocca, M.; Fiorino, G.; Zallot, C.; Furfaro, F.; Gilardi, D.; Radice, S.; Danese, S.; Peyrin-Biroulet, L. Incidence and Patterns of COVID-19 Among Inflammatory Bowel Disease Patients from the Nancy and Milan Cohorts. Clin. Gastroenterol. Hepatol. 2020, 18, 2134–2135. [Google Scholar] [CrossRef] [PubMed]
- Ungaro, R.C.; Brenner, E.J.; Gearry, R.B.; Kaplan, G.G.; Kissous-Hunt, M.; Lewis, J.D.; Ng, S.C.; Rahier, J.F.; Reinisch, W.; Steinwurz, F.; et al. Effect of IBD medications on COVID-19 outcomes: Results from an international registry. Gut 2020, 70, 725–732. [Google Scholar] [CrossRef]
- Khan, N.; Mahmud, N.; Trivedi, C.; Reinisch, W.; Lewis, J.D. Risk factors for SARS-CoV-2 infection and course of COVID-19 disease in patients with IBD in the Veterans Affair Healthcare System. Gut 2021, 70, 1657–1664. [Google Scholar] [CrossRef] [PubMed]
- Brenner, E.J.; Ungaro, R.C.; Gearry, R.B.; Kaplan, G.G.; Kissous-Hunt, M.; Lewis, J.D.; Ng, S.C.; Rahier, J.F.; Reinisch, W.; Ruemmele, F.M.; et al. Corticosteroids, But Not TNF Antagonists, Are Associated with Adverse COVID-19 Outcomes in Patients With Inflamm. Bowel Dis.: Results from an International Registry. Gastroenterology 2020, 159, 481–491. [Google Scholar] [CrossRef]
- Akiyama, S.; Hamdeh, S.; Micic, D.; Sakuraba, A. Prevalence and clinical outcomes of COVID-19 in patients with autoimmune diseases: A systematic review and meta-analysis. Ann. Rheum. Dis. 2020, 80, 384–391. [Google Scholar] [CrossRef]
- Siegel, C.A.; Christensen, B.; Kornbluth, A.; Rosh, J.R.; Kappelman, M.D.; Ungaro, R.C.; Johnson, D.F.; Chapman, S.; Wohl, D.A.; Mantzaris, G.J. Guidance for Restarting Inflammatory Bowel Disease Therapy in Patients Who Withheld Immunosuppressant Medications during COVID-19. J. Crohn Colitis 2020, 14, S769–S773. [Google Scholar] [CrossRef]
- Radon, K.; Saathoff, E.; Pritsch, M.; Guggenbuhl Noller, J.M.; Kroidl, I.; Olbrich, L.; Thiel, V.; Diefenbach, M.; Riess, F.; Forster, F.; et al. Protocol of a population-based prospective COVID-19 cohort study Munich, Germany (KoCo19). BMC Public Health 2020, 20, 1036. [Google Scholar] [CrossRef]
- Pritsch, M.; Radon, K.; Bakuli, A.; Le Gleut, R.; Olbrich, L.; Guggenbuehl Noller, J.M.; Saathoff, E.; Castelletti, N.; Gari, M.; Putz, P.; et al. Prevalence and Risk Factors of Infection in the Representative COVID-19 Cohort Munich. Int. J. Environ. Res. Public Health 2021, 18, 3572. [Google Scholar] [CrossRef]
- Levenstein, S.; Prantera, C.; Varvo, V.; Scribano, M.L.; Berto, E.; Luzi, C.; Andreoli, A. Development of the Perceived Stress Questionnaire: A new tool for psychosomatic research. J. Psychosom. Res. 1993, 37, 19–32. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Walter, O.B.; Kocalevent, R.D.; Weber, C.; Klapp, B.F. The Perceived Stress Questionnaire (PSQ) reconsidered: Validation and reference values from different clinical and healthy adult samples. Psychosom. Med. 2005, 67, 78–88. [Google Scholar] [CrossRef]
- Irvine, E.J.; Zhou, Q.; Thompson, A.K. The Short Inflammatory Bowel Disease Questionnaire: A quality of life instrument for community physicians managing inflammatory bowel disease. CCRPT Investigators. Canadian Crohn’s Relapse Prevention Trial. Am. J. Gastroenterol. 1996, 91, 1571–1578. [Google Scholar]
- Rose, M.; Fliege, H.; Hildebrandt, M.; Korber, J.; Arck, P.; Dignass, A.; Klapp, B. Validation of the new German translation version of the “Short Inflammatory Bowel Disease Questionnaire” (SIBDQ). Z. für Gastroenterol. 2000, 38, 277–286. [Google Scholar] [CrossRef]
- Grant, A.; MacIntyre, B.; Kappelman, M.D.; Otley, A.R. A New Domain Structure for the IMPACT-III Health-related Quality of life Tool for Pediatric Inflammatory Bowel Disease. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 494–500. [Google Scholar] [CrossRef]
- Otley, A.; Smith, C.; Nicholas, D.; Munk, M.; Avolio, J.; Sherman, P.M.; Griffiths, A.M. The IMPACT questionnaire: A valid measure of health-related quality of life in pediatric inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 2002, 35, 557–563. [Google Scholar] [CrossRef]
- Peters, A.; Rospleszcz, S.; Greiser, K.H.; Dallavalle, M.; Berger, K. Complete list of authors available under, C. The Impact of the COVID-19 Pandemic on Self-Reported Health. Deutsches Ärzteblatt Int. 2020, 117, 861–867. [Google Scholar] [CrossRef]
- Gao, Y.D.; Ding, M.; Dong, X.; Zhang, J.J.; Kursat Azkur, A.; Azkur, D.; Gan, H.; Sun, Y.L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Romero Starke, K.; Petereit-Haack, G.; Schubert, M.; Kämpf, D.; Schliebner, A.; Hegewald, J.; Seidler, A. The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression. Int. J. Environ. Res. Public Health 2020, 17, 5974. [Google Scholar] [CrossRef] [PubMed]
- Michelena, X.; Borrell, H.; López-Corbeto, M.; López-Lasanta, M.; Moreno, E.; Pascual-Pastor, M.; Erra, A.; Serrat, M.; Espartal, E.; Antón, S.; et al. Incidence of COVID-19 in a cohort of adult and paediatric patients with rheumatic diseases treated with targeted biologic and synthetic disease-modifying anti-rheumatic drugs. Semin. Arthritis Rheum. 2020, 50, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, A.; Nicastro, E.; Speziani, C.; De Giorgio, M.; Pasulo, L.; Magro, B.; Fagiuoli, S.; Antiga, L.D. Health status of patients with autoimmune liver disease during SARS-CoV-2 outbreak in northern Italy. J. Hepatol. 2020, 73, 702–705. [Google Scholar] [CrossRef]
- Ssentongo, P.; Ssentongo, A.E.; Heilbrunn, E.S.; Ba, D.M.; Chinchilli, V.M. Association of cardiovascular disease and 10 other pre-existing comorbidities with COVID-19 mortality: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0238215. [Google Scholar] [CrossRef]
- Yang, J.; Hu, J.; Zhu, C. Obesity aggravates COVID-19: A systematic review and meta-analysis. J. Med. Virol. 2021, 93, 257–261. [Google Scholar] [CrossRef]
- Földi, M.; Farkas, N.; Kiss, S.; Zádori, N.; Váncsa, S.; Szakó, L.; Dembrovszky, F.; Solymár, M.; Bartalis, E.; Szakács, Z.; et al. Obesity is a risk factor for developing critical condition in COVID-19 patients: A systematic review and meta-analysis. Obes. Rev. 2020, 21, e13095. [Google Scholar] [CrossRef] [PubMed]
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef]
- Pranata, R.; Huang, I.; Lim, M.A.; Wahjoepramono, E.J.; July, J. Impact of cerebrovascular and cardiovascular diseases on mortality and severity of COVID-19-systematic review, meta-analysis, and meta-regression. J. Stroke Cerebrovasc. Dis. 2020, 29, 104949. [Google Scholar] [CrossRef] [PubMed]
- Matsushita, K.; Ding, N.; Kou, M.; Hu, X.; Chen, M.; Gao, Y.; Honda, Y.; Zhao, D.; Dowdy, D.; Mok, Y.; et al. The Relationship of COVID-19 Severity with Cardiovascular Disease and Its Traditional Risk Factors: A Systematic Review and Meta-Analysis. Glob. Heart 2020, 15, 64. [Google Scholar] [CrossRef] [PubMed]
- Martins-Filho, P.R.; Tavares, C.S.S.; Santos, V.S. Factors associated with mortality in patients with COVID-19. A quantitative evidence synthesis of clinical and laboratory data. Eur. J. Intern. Med. 2020, 76, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Karagiannidis, C.; Mostert, C.; Hentschker, C.; Voshaar, T.; Malzahn, J.; Schillinger, G.; Klauber, J.; Janssens, U.; Marx, G.; Weber-Carstens, S.; et al. Case characteristics, resource use, and outcomes of 10,021 patients with COVID-19 admitted to 920 German hospitals: An observational study. Lancet 2020, 8, 853–862. [Google Scholar] [CrossRef]
- Aziz, F.; Mandelbrot, D.; Singh, T.; Parajuli, S.; Garg, N.; Mohamed, M.; Astor, B.C.; Djamali, A. Early Report on Published Outcomes in Kidney Transplant Recipients Compared to Nontransplant Patients Infected with Coronavirus Disease 2019. Transplant. Proc. 2020, 52, 2659–2662. [Google Scholar] [CrossRef] [PubMed]
- Duricova, D.; Burisch, J.; Jess, T.; Gower-Rousseau, C.; Lakatos, P.L. Age-related differences in presentation and course of inflammatory bowel disease: An update on the population-based literature. J. Crohn’s Colitis 2014, 8, 1351–1361. [Google Scholar] [CrossRef]
- Loftus, C.G.; Loftus, E.V., Jr.; Harmsen, W.S.; Zinsmeister, A.R.; Tremaine, W.J.; Melton, L.J., 3rd; Sandborn, W.J. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940–2000. Inflamm. Bowel Dis. 2007, 13, 254–261. [Google Scholar] [CrossRef]
- Ott, C.; Obermeier, F.; Thieler, S.; Kemptner, D.; Bauer, A.; Schölmerich, J.; Rogler, G.; Timmer, A. The incidence of inflammatory bowel disease in a rural region of Southern Germany: A prospective population-based study. Eur. J. Gastroenterol. Hepatol. 2008, 20, 917–923. [Google Scholar] [CrossRef] [Green Version]
- Kennedy, N.A.; Goodhand, J.R.; Bewshea, C.; Nice, R.; Chee, D.; Lin, S.; Chanchlani, N.; Butterworth, J.; Cooney, R.; Croft, N.M.; et al. Anti-SARS-CoV-2 antibody responses are attenuated in patients with IBD treated with infliximab. Gut 2021, 70, 865–875. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, E.W.; Beyl, R.A.; Fearnbach, S.N.; Altazan, A.D.; Martin, C.K.; Redman, L.M. The Impact of COVID-19 Stay-At-Home Orders on Health Behaviors in Adults. Obesity 2021, 29, 438–445. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.E.M.; Brady, E.M.; Robertson, N. Associations between social jetlag and mental health in young people: A systematic review. Chronobiol. Int. 2019, 36, 1316–1333. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.; Bahammam, A.S.; Bragazzi, N.L.; Saif, Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef] [PubMed]
- Koletzko, B.; Holzapfel, C.; Schneider, U.; Hauner, H. Lifestyle and Body Weight Consequences of the COVID-19 Pandemic in Children: Increasing Disparity. Ann. Nutr. Metab. 2021, 77, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef] [PubMed]
- Rozich, J.J.; Holmer, A.; Singh, S. Effect of Lifestyle Factors on Outcomes in Patients with Inflammatory Bowel Diseases. Am. J. Gastroenterol. 2020, 115, 832–840. [Google Scholar] [CrossRef]
- Sumner, J.A.; Colich, N.L.; Uddin, M.; Armstrong, D.; McLaughlin, K.A. Early Experiences of Threat, but Not Deprivation, Are Associated with Accelerated Biological Aging in Children and Adolescents. Biol. Psychiatry 2019, 85, 268–278. [Google Scholar] [CrossRef]
- Umucu, E.; Lee, B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020, 65, 193–198. [Google Scholar] [CrossRef]
- Kujawa, A.; Green, H.; Compas, B.E.; Dickey, L.; Pegg, S. Exposure to COVID-19 pandemic stress: Associations with depression and anxiety in emerging adults in the United States. Depress. Anxiety 2020, 37, 1280–1288. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef] [PubMed]
- Christian, B.J. Translational Research—Family Management and Parenting Stress Associated with Chronic Conditions in Children. J. Pediatric Nurs. 2019, 45, 73–75. [Google Scholar] [CrossRef] [PubMed]
- Coyne, L.W.; Gould, E.R.; Grimaldi, M.; Wilson, K.G.; Baffuto, G.; Biglan, A. First Things First: Parent Psychological Flexibility and Self-Compassion during COVID-19. Behav. Anal. Pract. 2020. [Google Scholar] [CrossRef] [PubMed]
- Cushman, G.; Shih, S.; Reed, B. Parent and Family Functioning in Pediatric Inflammatory Bowel Disease. Children 2020, 7, 188. [Google Scholar] [CrossRef] [PubMed]
- Engstrom, I. Parental distress and social interaction in families with children with inflammatory bowel disease. J. Am. Acad. Child Adolesc. Psychiatry 1991, 30, 904–912. [Google Scholar] [CrossRef]
- Ingerski, L.M.; Baldassano, R.N.; Denson, L.A.; Hommel, K.A. Barriers to oral medication adherence for adolescents with inflammatory bowel disease. J. Pediatr. Psychol. 2010, 35, 683–691. [Google Scholar] [CrossRef] [Green Version]
- Calvano, C.; Engelke, L.; Di Bella, J.; Kindermann, J.; Renneberg, B.; Winter, S.M. Families in the COVID-19 pandemic: Parental stress, parent mental health and the occurrence of adverse childhood experiences-results of a representative survey in Germany. Eur. Child Adolesc. Psychiatry 2021. [Google Scholar] [CrossRef]
- Yu, M.; Ye, Z.; Chen, Y.; Qin, T.; Kou, J.; Tian, D.; Xiao, F. Questionnaire assessment helps the self-management of patients with inflammatory bowel disease during the outbreak of Coronavirus Disease 2019. Aging 2020, 12, 12468–12478. [Google Scholar] [CrossRef] [PubMed]
- Martinelli, M.; Strisciuglio, C.; Fedele, F.; Miele, E.; Staiano, A. Clinical and Psychological Issues in Children with Inflammatory Bowel Disease during COVID-19 Pandemic. Inflamm. Bowel Dis. 2020, 26, e95–e96. [Google Scholar] [CrossRef]
- Peckham, H.; de Gruijter, N.M.; Raine, C.; Radziszewska, A.; Ciurtin, C.; Wedderburn, L.R.; Rosser, E.C.; Webb, K.; Deakin, C.T. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020, 11, 6317. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, L.L.; Shavit, Y.Z.; Barnes, J.T. Age Advantages in Emotional Experience Persist Even Under Threat from the COVID-19 Pandemic. Psychol. Sci. 2020, 31, 1374–1385. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, T.J.; Fields, E.C.; Garcia, S.M.; Kensinger, E.A. The relation between age and experienced stress, worry, affect, and depression during the spring 2020 phase of the COVID-19 pandemic in the United States. Emotion 2021. [Google Scholar] [CrossRef]
- Klaiber, P.; Wen, J.H.; DeLongis, A.; Sin, N.L. The Ups and Downs of Daily Life during COVID-19: Age Differences in Affect, Stress, and Positive Events. J. Gerontol. Ser. B 2021, 76, e30–e37. [Google Scholar] [CrossRef] [PubMed]




| Factors, n (%) | All Patients | 6–20 Years | >20–40 Years | >40–60 Years | >60 Years | p-Value f |
|---|---|---|---|---|---|---|
| N = 504 (100%) | 90 (18%) | 167 (33%) | 175 (35%) | 72 (14%) | ||
| Male sex | 272 (54.0) | 51 (56.7) | 88 (52.7) | 95 (54.3) | 38 (52.8) | 0.94 |
| Age at inclusion in y, median (IQR) | 40 (27–54) | 15 (12–17) | 33 (28–36) | 50 (45–55) | 68 (63–74) | <0.001 |
| Age at diagnosis in y, median (IQR), N = 491 | 23 (15–33) | 10 (7–13) | 21 (16–27) | 30 (21–39) | 48 (28–57) | <0.001 |
| Disease duration in y, median (IQR), N = 491 | 12 (5–21) | 4 (1–7) | 10 (6–15) | 18.5 (11.5–27.5) | 23 (12–36) | <0.001 |
| Influenza vaccination season 2019/20 | 204 (40.5) | 33 (36.7) | 60 (35.9) | 59 (33.7) | 41 (56.9) | 0.008 |
| BMI categories a | <0.001 | |||||
| Underweight | 40 (8.0) | 26 (29.2) | 10 (6.0) | 3 (1.7) | 1 (1.4) | |
| Normal weight | 275 (54.7) | 54 (60.7) | 109 (65.3) | 82 (46.9) | 30 (41.7) | |
| Overweight | 130 (25.8) | 8 (9.0) | 34 (20.4) | 57 (32.6) | 31 (43.1) | |
| Obesity | 58 (11.5) | 1 (1.1) | 14 (8.4) | 33 (18.9) | 10 (13.9) | |
| IBD type | 0.005 | |||||
| Crohn’s Disease | 296 (58.7) | 44 (48.9) | 100 (59.9) | 110 (62.9) | 42 (58.3) | |
| Ulcerative colitis | 180 (35.7) | 34 (37.8) | 55 (32.9) | 61 (34.9) | 30 (41.7) | |
| IBD-u | 20 (4.0) | 10 (11.1) | 8 (4.8) | 2 (1.1) | 0 (0.0) | |
| Disease activity | 0.020 | |||||
| Remission | 230 (45.7) | 40 (44.9) | 92 (55.1) | 71 (40.6) | 27 (37.5) | |
| Mild | 198 (39.4) | 39 (43.8) | 54 (32.3) | 80 (45.7) | 25 (34.7) | |
| Moderate | 59 (11.7) | 8 (9.0) | 16 (9.6) | 19 (10.9) | 16 (22.2) | |
| Severe | 16 (3.2) | 2 (2.2) | 5 (3.0) | 5 (2.9) | 4 (5.6) | |
| Any surgery due to IBD | 185 (36.7) | 16 (17.8) | 51 (30.5) | 80 (45.7) | 38 (52.8) | <0.001 |
| Any bowel resection | 116 (23.0) | 6 (6.7) | 26 (15.6) | 57 (32.6) | 27 (37.5) | <0.001 |
| SIRSCObIndex, N = 504 | <0.0001 | |||||
| 0 = no increased risk | 58 (11.5) | 15 (16.7) | 22 (13.2) | 18 (10.3) | 3 (4.2) | |
| 1 = mild | 249 (49.4) | 59 (65.6) | 104 (62.3) | 73 (41.7) | 13 (18.1) | |
| 2 = moderate | 116 (23.0) | 16 (17.8) | 32 (19.2) | 49 (28.0) | 19 (26.4) | |
| 3–4 = severe | 66 (13.1) | 0 (0.0) | 9 (5.4) | 32 (18.3) | 25 (34.7) | |
| ≥5 = very severe | 15 (3.0) | 0 (0.0) | 0 (0.0) | 3 (1.7) | 12 (16.7) | |
| Any drug for non-IBD disease | 198 (39.5) | 14 (15.9) | 47 (28.1) | 85 (48.6) | 52 (72.2) | <0.001 |
| IBD associated medication | ||||||
| None | 49 (9.7) | 3 (3.3) | 18 (10.8) | 21 (12.0) | 7 (9.7) | 0.14 |
| Only 5-ASA | 48 (9.5) | 10 (11.1) | 15 (9.0) | 15 (8.6) | 8 (11.1) | 0.87 |
| Any 5-ASA | 164 (32.5) | 42 (46.7) | 48 (28.7) | 47 (26.9) | 27 (37.5) | 0.005 |
| Any Immune modulator c (IM) | 67 (13.3) | 37 (41.1) | 15 (9.0) | 8 (4.6) | 7 (9.7) | <0.001 |
| Any biologic d/Jak-Inhibitor | 350 (69.4) | 60 (66.7) | 120 (71.9) | 127 (72.6) | 43 (59.7) | 0.19 |
| Any current corticosteroids | 64 (12.7) | 8 (8.9) | 16 (9.6) | 22 (12.6) | 18 (25.0) | 0.006 |
| Any immunosuppressive medication incl. biologics, IM, corticosteroids | 401 (79.6) | 74 (82.2) | 133 (79.6) | 138 (78.9) | 56 (77.8) | 0.9 |
| Combo-therapy e +/− 5-ASA | 33 (6.5) | 25 (27.8) | 7 (4.2) | 1 (0.6) | 0 (0.0) | <0.001 |
| Any supplements incl. probiotics, vitamins, over the counter drugs | 383 (76.0) | 76 (84.4) | 121 (72.5) | 131 (74.9) | 55 (76.4) | 0.19 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koletzko, L.; Klucker, E.; Le Thi, T.G.; Breiteneicher, S.; Rubio-Acero, R.; Neuhaus, L.; Stark, R.G.; Standl, M.; Wieser, A.; Török, H.; et al. Following Pediatric and Adult IBD Patients through the COVID-19 Pandemic: Changes in Psychosocial Burden and Perception of Infection Risk and Harm over Time. J. Clin. Med. 2021, 10, 4124. https://doi.org/10.3390/jcm10184124
Koletzko L, Klucker E, Le Thi TG, Breiteneicher S, Rubio-Acero R, Neuhaus L, Stark RG, Standl M, Wieser A, Török H, et al. Following Pediatric and Adult IBD Patients through the COVID-19 Pandemic: Changes in Psychosocial Burden and Perception of Infection Risk and Harm over Time. Journal of Clinical Medicine. 2021; 10(18):4124. https://doi.org/10.3390/jcm10184124
Chicago/Turabian StyleKoletzko, Leandra, Elisabeth Klucker, Thu Giang Le Thi, Simone Breiteneicher, Raquel Rubio-Acero, Lukas Neuhaus, Reneé G. Stark, Marie Standl, Andreas Wieser, Helga Török, and et al. 2021. "Following Pediatric and Adult IBD Patients through the COVID-19 Pandemic: Changes in Psychosocial Burden and Perception of Infection Risk and Harm over Time" Journal of Clinical Medicine 10, no. 18: 4124. https://doi.org/10.3390/jcm10184124
APA StyleKoletzko, L., Klucker, E., Le Thi, T. G., Breiteneicher, S., Rubio-Acero, R., Neuhaus, L., Stark, R. G., Standl, M., Wieser, A., Török, H., Koletzko, S., & Schwerd, T. (2021). Following Pediatric and Adult IBD Patients through the COVID-19 Pandemic: Changes in Psychosocial Burden and Perception of Infection Risk and Harm over Time. Journal of Clinical Medicine, 10(18), 4124. https://doi.org/10.3390/jcm10184124






