“Lessons Learned” Preventing Recurrent Ischemic Strokes through Secondary Prevention Programs: A Systematic Review
Abstract
:1. Introduction
2. Methods
3. Results
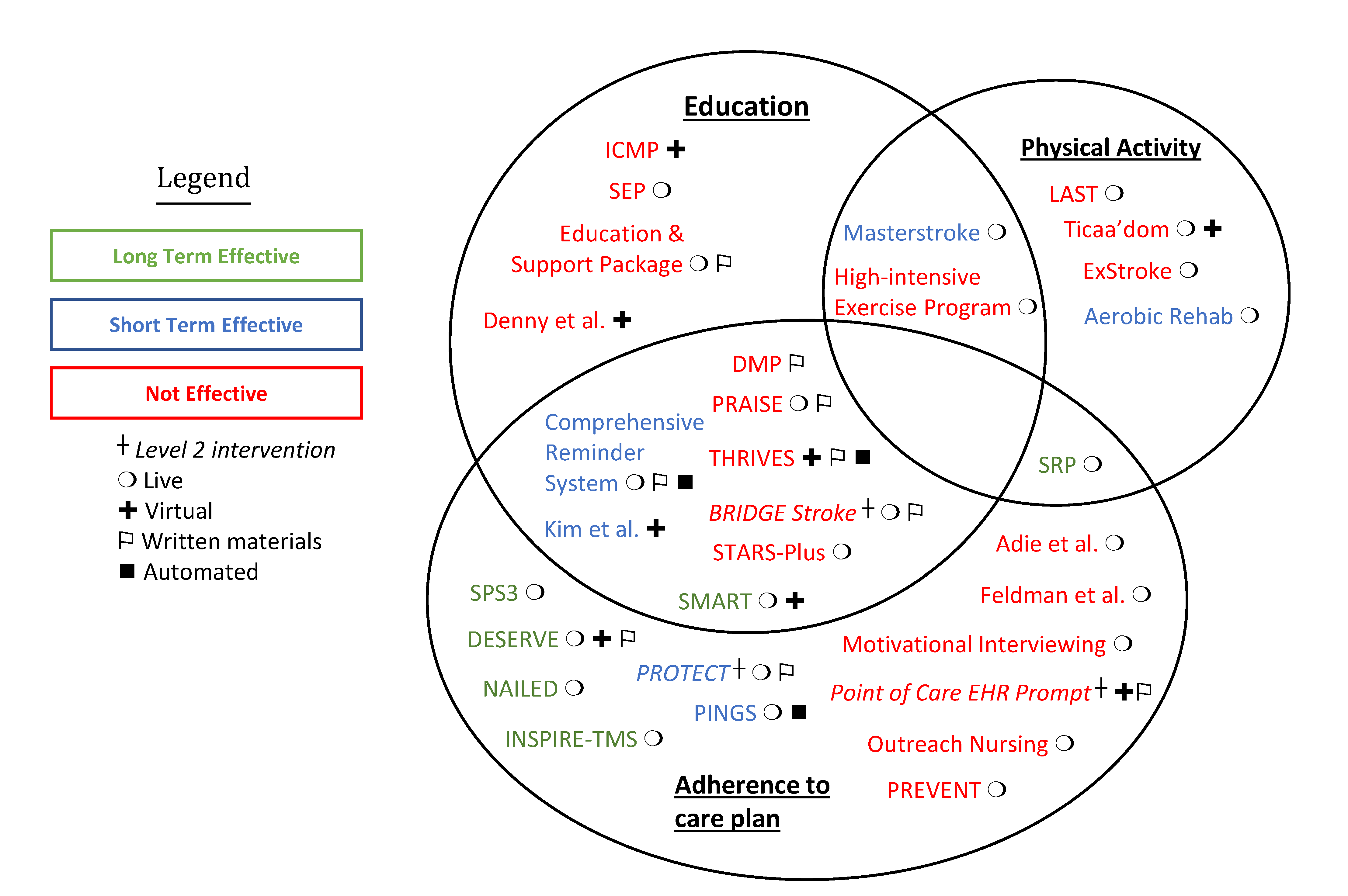
3.1. Long-Term Effective Studies (>6 Months)
3.2. Short-Term Effective Studies
3.3. Studies That Were Not Effective
4. Discussion
| Lesson | Evidence |
|---|---|
| Boden-Albala et al. [17] |
| Irewall et al. [18] | |
| Sanders et al. [46] | |
| Rolls et al. [47] | |
| Ravenell et al. [51] | |
| Ovbiagele et al. [10] |
| SPS3 Investigators [19] | |
| Bangalore et al. [53] | |
| Boden-Albala et al. [17] |
| Irewall et al. [18] | |
| Ahmadi et al. [20] | |
| Adie et al. [22] | |
| Feldman et al. [24] | |
| Barker-Collo et al. [25] | |
| Hornnes et al. [28] | |
| Owolabi et al. [31] | |
| Sarfo et al. [40] | |
| Toledano-Zarhl et al. [42] | |
| Kronish et al. [60] | |
| Ovbiagele et al. [10] |
| Denny et al. [32] | |
| Wan et al. [41,43] | |
| Kim et al. [45] | |
| Benoit et al. [61] | |
| Cuccurullo et al. [21] |
| Wan et al. [41,43] | |
| Toledano-Zarhl et al. [42] | |
| White et al. [50] | |
| Benoit et al. [61] | |
| Sarfo et al. [40] |
| Machline-Carrion et al. [56] | |
| Smith et al. [68] | |
| Urimubenshi et al. [69] | |
| Pandian et al. [70] | |
| Cameron et al. [73] |
| Broderick et al. [74] | |
| Rattray et al. [76] | |
| Blum et al. [77] | |
| Bettger et al. [79] | |
| Nathans et al. [80] |
| Intervention | Short Term (<6 Months) | Long Term (≥6 Months) |
|---|---|---|
| Comprehensive Reminder System [41] | Effective at 3-months post-randomization
| No assessment after 6 months |
| PROTECT [52] | Effective immediately/at the time of discharge
| No assessment after 6 months |
| SRP [21] | Effective at 120-days post-randomization
| Effective at 1-year post-randomization in terms of 1-year mortality
|
| Masterstroke [15] | Effective immediately and at 3-months post-program conclusion
|
|
| NAILED [18] | No assessment before 6 months | Effective at 12-months post-randomization or discharge
|
| Kim et al. [45] | Effective at 3-months post-randomization
| No assessment after 6 months |
| Aerobic Rehab [42] | Effective at 6-weeks post-randomization
| No assessment after 6 months |
| PINGS [40] | Effective at 3-months post-randomization
| No assessment after 6 months |
| DESERVE [17] | No assessment before 6 months | Effective at 12-months post-randomization (in Hispanic patients only)
|
| SMART [16] | Effective at 6-months post-randomization
| Effective at 12-months post-randomization
|
| INSPiRE-TMS [20] | No assessment before 6 months | Effective at 3-years post-randomization
|
| SPS3 [19] | No assessment before 6 months | Effective at 1-year post-randomization
|
| Denny et al. [32] | Not Effective at 30-days post-discharge
| No assessment after 6 months |
| SEP [33] | Not Effective at 6-months post-randomization
| No assessment after 6 months |
| THRIVES [31] | Not Effective at 1-,3- and 6-months post-randomization
| Not Effective at 9- and 12-months post-randomization
|
| PRAISE [60] | No assessment before 6 months | Not Effective at 6-months post-randomization
|
| LAST [39] | No assessment before 6 months | Not Effective at 18-months post-randomization
|
| Adie et al. [22] | Not Effective at 6-months post-randomization
| No assessment after 6 months |
| ExStroke [38] | No assessment before 6 months | Not Effective at 24-months post-randomization
|
| Feldman et al. [24]. | Not Effective at 3-months post-randomization
| Not Effective at 12-months post-randomization
|
| Ticaa’dom [37] | Not Effective at discharge and 6-months post-randomization
| Not Effective at 12-months post-randomization
|
| Point of Care EHR Prompt [26] | No assessment before 6 months | Not Effective at 15-months post-randomization
|
| High-Intensive Exercise Program [36] | Not Effective at 3- and 6-months post-randomization
| No assessment after 6 months |
| PREVENT [28] | No assessment before 6 months | Not Effective at 12-months post-randomization
|
| STARS-Plus [6] | No assessment before 6 months | Not Effective at 12-months post-randomization
|
| DMP [29] | No assessment before 6 months | Not Effective at 30-months post-randomization
|
| ICMP [34] | Not Effective at 1- and 12-weeks post-intervention completion
| No assessment after 6 months |
| Education and Support Package [35] | Not Effective at 3-months post-randomization
| No assessment after 6 months |
| BRIDGE Stroke [56] | Not Effective at 90-days post-randomization
| No assessment after 6 months |
| Outreach Nursing [27] | Not Effective at 6-months post-discharge
| No assessment after 6 months |
| Motivational Interviewing [25] | Not Effective at 3- and 6-months post-randomization
| Not Effective at 9- and 12-months post-randomization
|
| Intervention | Author | Yr 1 | N 1 | Design | Location | Target | Level | Delivery | Leader | Strategy |
|---|---|---|---|---|---|---|---|---|---|---|
| Comprehensive Reminder System | Wan et al. [41] | 2018 | 174 | RCT 1 | China | Patient | 1 | Live Written materials Automated | Nurse | Education Adherence |
| PROTECT | Ovbiagele et al. [52] | 2004 | 130 | Non-RCT | USA | Provider | 2 | Live Written materials | HCW 1 | Adherence |
| Masterstroke | White et al. [15] | 2013 | 22 | Mixed methods | Australia | Patient | 1 | Live | MDT 1 | Education PA |
| NAILED | Irewall et al. [18] | 2019 | 771 | RCT | Sweden | Patient | 1 | Live | Nurse | Adherence |
| n/a | Kim et al. [45] | 2013 | 102 | RCT | South Korea | Patient Caregiver | 1 | Virtual | Researcher | Education Adherence |
| Aerobic Rehab | Toledano-Zarhl et al. [42] | 2011 | 28 | RCT | Middle East | Patient | 1 | Live | AHP 1 | PA |
| PINGS | Sarfo et al. [40] | 2019 | 60 | RCT | Ghana | Patient | 1 | Live Automated | Nurse | Adherence |
| DESERVE | Boden-Albala et al. [17] | 2019 | 552 | RCT | USA | Patient | 1 | Virtual Written materials Live | Care Coordinator | Adherence |
| SMART | Peng et al. [16] | 2014 | 3821 | Cluster RCT | China | Patient | 1 | Live Virtual | HCW | Adherence Education |
| INSPiRE-TMS | Ahmadi et al. [20] | 2020 | 2098 | RCT | Germany | Patient | 1 | Live | HCW | Adherence |
| SPS3 | SPS3 Investigator Group [19] | 2013 | 3020 | RCT | USA | Patient | 1 | Live | Physician | Adherence |
| n/a | Denny et al. [32] | 2017 | 93 | Pre- and post-test | USA | Patient | 1 | Virtual | HCW | Education |
| SEP | Rodgers et al. [33] | 1999 | 204 | RCT | UK | Patient Caregiver | 1 | Live | MDT | Education |
| THRIVES | Owolabi et al. [31] | 2019 | 400 | RCT | Nigeria | Patient | 1 | Automated Virtual Written materials | Physician | Adherence Education |
| PRAISE | Kronish et al. [60] | 2013 | 600 | RCT | USA | Patient | 1 | Live Written materials | Peer group leader | Adherence Education |
| LAST | Askim et al. [39] | 2018 | 380 | RCT | Norway | Patient | 1 | Live | AHP | PA |
| n/a | Adie et al. [22] | 2010 | 56 | RCT | UK | Patient | 1 | Live | Researcher | Adherence |
| ExStroke | Boysen et al. [38] | 2009 | 314 | RCT | Denmark China Poland Estonia | Patient | 1 | Live | HCW | PA |
| n/a | Feldman et al. [24] | 2020 | 495 | 3 arm RCT | USA | Patient | 1 | Live | Nurse practitioner | Adherence |
| Ticaa’dom | Mandigout et al. [37] | 2020 | 83 | RCT | France | Patient | 1 | Live Virtual | AHP | PA |
| Point of Care EHR Prompt | Dregan et al. [26] | 2014 | 106 sites, 11391 pt | Cluster RCT | UK | Provider | 2 | Virtual Written materials | Computer-led | Adherence |
| High-Intensive Exercise Program | Holmgren et al. [36] | 2010 | 34 | RCT | Sweden | Patient | 1 | Live | MDT | PA Education |
| PREVENT | Hornnes et al. [28] | 2011 | 344 | RCT | Denmark | Patient | 1 | Live | Nurse | Adherence |
| STARS-Plus | Bretz et al. [6] | 2014 | 193 | Pre- and post-test | USA | Patient | 1 | Live | HCW | Education Adherence |
| DMP | Fukuoka et al. [29] | 2019 | 321 | RCT | Japan | Patient | 1 | Written materials | Nurse | Education Adherence |
| ICMP | Maasland et al. [34] | 2007 | 65 | RCT | Netherlands | Patient | 1 | Virtual | Physician | Education |
| Education and Support Package | Eames et al. [35] | 2012 | 119 | RCT | Australia | Patient Caregiver | 1 | Live Written materials | AHP | Education |
| BRIDGE Stroke | Machline-Carrion et al. [56] | 2019 | 36 sites, 1642 pt | Cluster RCT | Latin America | Provider | 1 | Live Written materials | Care coordinator | Education Adherence |
| Outreach Nursing | Boter et al. [27] | 2004 | 536 | RCT | Netherlands | Patient Caregiver | 1 | Live | Nurse | Adherence |
| Motivational Interviewing | Barker-Collo et al. [25] | 2015 | 386 | RCT | New Zealand | Patient | 1 | Live | Researcher | Adherence |
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gorelick, P.B. The global burden of stroke: Persistent and disabling. Lancet Neurol. 2019, 18, 417–418. [Google Scholar] [CrossRef] [Green Version]
- Roger, V.L.; Go, A.S.; Lloyd-Jones, D.M.; Adams, R.J.; Berry, J.D.; Brown, T.M.; Carnethon, M.R.; Dai, S.; de Simone, G.; Ford, E.S.; et al. Heart Disease and Stroke Statistics—2011 Update. Circulation 2011, 123, e18–e209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oza, R.; Rundell, K.; Garcellano, M. Recurrent Ischemic Stroke: Strategies for Prevention. Am. Fam. Physician 2017, 96, 436–440. [Google Scholar] [PubMed]
- Avan, A.; Digaleh, H.; Di Napoli, M.; Stranges, S.; Behrouz, R.; Shojaeianbabaei, G.; Amiri, A.; Tabrizi, R.; Mokhber, N.; Spence, J.D.; et al. Socioeconomic status and stroke incidence, prevalence, mortality, and worldwide burden: An ecological analysis from the Global Burden of Disease Study 2017. BMC Med. 2019, 17, 191. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.O.; Nguyen, M.; Roth, G.A.; Nichols, E.; Alam, T.; Abate, D.; Abd-Allah, F.; Abdelalim, A.; Abraha, H.N.; Abu-Rmeileh, N.M.; et al. Global, regional, and national burden of stroke, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019, 18, 439–458. [Google Scholar] [CrossRef] [Green Version]
- Bretz, M.N.; Graves, A.; West, A.; Kiesz, K.C.; Toth, L.; Welch, M. Steps against Recurrent Stroke Plus. J. Neurosci. Nurs. 2014, 46, E3–E13. [Google Scholar] [CrossRef]
- Lambert, C.; Chaudhary, D.; Olulana, O.; Shahjouei, S.; Avula, V.; Li, J.; Abedi, V.; Zand, R. Sex disparity in long-term stroke recurrence and mortality in a rural population in the United States. Ther. Adv. Neurol. Disord. 2020, 13, 1756286420971895. [Google Scholar] [CrossRef]
- Chaudhary, D.; Abedi, V.; Li, J.; Schirmer, C.M.; Griessenauer, C.J.; Zand, R. Clinical Risk Score for Predicting Recurrence Following a Cerebral Ischemic Event. Front. Neurol. 2019, 10, 1106. [Google Scholar] [CrossRef] [Green Version]
- Burn, J.; Dennis, M.; Bamford, J.; Sandercock, P.; Wade, D.; Warlow, C. Erratum: Long-term risk of recurrent stroke after a first-ever stroke: The Oxfordshire Community Stroke Project. Stroke 1994, 25, 333–337. [Google Scholar] [CrossRef] [Green Version]
- Ovbiagele, B.; Nguyen-Huynh, M.N. Stroke Epidemiology: Advancing Our Understanding of Disease Mechanism and Therapy. Neurotherapeutics 2011, 8, 319–329. [Google Scholar] [CrossRef] [Green Version]
- Groves, T. Enhancing the Quality and Transparency of Health Research. University of Oxford. 2019. Available online: https://gtr.ukri.org/projects?ref=MR%2FJ00488X%2F1#/tabOverview (accessed on 10 September 2021).
- Moher, D.; PRISMA-P Group; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Cleary, P.D.; Gross, C.P.; Zaslavsky, A.M.; Taplin, S.H. Multilevel Interventions: Study Design and Analysis Issues. J. Natl. Cancer Inst. Monogr. 2012, 2012, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Ovbiagele, B.; Saver, J.L.; Fredieu, A.; Suzuki, S.; McNair, N.; Dandekar, A.; Razinia, T.; Kidwell, C.S. PROTECT: A coordinated stroke treatment program to prevent recurrent thromboembolic events. Neurology 2004, 63, 1217–1222. [Google Scholar] [CrossRef] [PubMed]
- White, J.H.; Bynon, B.L.; Marquez, J.; Sweetapple, A.; Pollack, M. Masterstroke: A pilot group stroke prevention program for community dwelling stroke survivors. Disabil. Rehabil. 2012, 35, 931–938. [Google Scholar] [CrossRef]
- Peng, B.; Ni, J.; Anderson, C.S.; Zhu, Y.; Wang, Y.; Pu, C.; Wu, J.; Wang, J.; Zhou, L.; Yao, M.; et al. Implementation of a Structured Guideline–Based Program for the Secondary Prevention of Ischemic Stroke in China. Stroke 2014, 45, 515–519. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boden-Albala, B.; Goldmann, E.; Parikh, N.S.; Carman, H.; Roberts, E.T.; Lord, A.S.; Torrico, V.; Appleton, N.; Birkemeier, J.; Parides, M.; et al. Efficacy of a Discharge Educational Strategy vs Standard Discharge Care on Reduction of Vascular Risk in Patients with Stroke and Transient Ischemic Attack: The DESERVE Randomized Clinical Trial. JAMA Neurol. 2019, 76, 20–27. [Google Scholar] [CrossRef]
- Irewall, A.-L.; Ögren, J.; Bergström, L.; Laurell, K.; Söderström, L.; Mooe, T. Nurse-led, telephone-based secondary preventive follow-up benefits stroke/TIA patients with low education: A randomized controlled trial sub-study. Trials 2019, 20, 1–10. [Google Scholar] [CrossRef]
- Benavente, O.R.; Coffey, C.S.; Conwit, R.; Hart, R.G.; McClure, L.A.; Pearce, L.; Pergola, P.E.; Szychowski, J. Blood-pressure targets in patients with recent lacunar stroke: The SPS3 randomised trial. Lancet 2013, 382, 507–515. [Google Scholar] [CrossRef] [Green Version]
- Ahmadi, M.; Laumeier, I.; Ihl, T.; Steinicke, M.; Ferse, C.; Endres, M.; Grau, A.; Hastrup, S.; Poppert, H.; Palm, F.; et al. A support programme for secondary prevention in patients with transient ischaemic attack and minor stroke (INSPiRE-TMS): An open-label, randomised controlled trial. Lancet Neurol. 2019, 19, 49–60. [Google Scholar] [CrossRef]
- Cuccurullo, S.J.; Fleming, T.K.; Kostis, W.J.; Greiss, C.; Gizzi, M.S.; Eckert, A.; Ray, A.R.; Scarpati, R.; Cosgrove, N.M.; Beavers, T.; et al. Impact of a Stroke Recovery Program Integrating Modified Cardiac Rehabilitation on All-Cause Mortality, Cardiovascular Performance and Functional Performance. Am. J. Phys. Med. Rehabil. 2019, 98, 953–963. [Google Scholar] [CrossRef]
- Adie, K.; James, M.A. Does telephone follow-up improve blood pressure after minor stroke or TIA? Age Ageing 2010, 39, 598–603. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machline-Carrion, M.J.; Santucci, E.V.; Damiani, L.P.; Bahit, C.; Málaga, G.; Pontes-Neto, O.M.; Martins, S.C.O.; Zétola, V.F.; Normilio-Silva, K.; De Freitas, G.R.; et al. An international cluster-randomized quality improvement trial to increase the adherence to evidence-based therapies for acute ischemic stroke and transient ischemic attack patients: Rationale and design of the BRIDGE STROKE Trial. Am. Hear. J. 2018, 207, 49–57. [Google Scholar] [CrossRef] [PubMed]
- Feldman, P.H.; McDonald, M.V.; Trachtenberg, M.; Trifilio, M.; Onorato, N.; Sridharan, S.; Silver, S.; Eimicke, J.; Teresi, J. Reducing Hypertension in a Poststroke Black and Hispanic Home Care Population: Results of a Pragmatic Randomized Controlled Trial. Am. J. Hypertens. 2019, 33, 362–370. [Google Scholar] [CrossRef]
- Barker-Collo, S.; Krishnamurthi, R.; Witt, E.; Feigin, V.L.; Jones, A.; McPherson, K.; Starkey, N.; Parag, V.; Jiang, Y.; Barber, P.A.; et al. Improving Adherence to Secondary Stroke Prevention Strategies Through Motivational Interviewing. Stroke 2015, 46, 3451–3458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dregan, A.; van Staa, T.; McDermott, L.; McCann, G.; Ashworth, M.; Charlton, J.; Wolfe, C.; Rudd, A.; Yardley, L.; Gulliford, M.C.; et al. Point-of-Care Cluster Randomized Trial in Stroke Secondary Prevention Using Electronic Health Records. Stroke 2014, 45, 2066–2071. [Google Scholar] [CrossRef]
- Boter, H. Multicenter Randomized Controlled Trial of an Outreach Nursing Support Program for Recently Discharged Stroke Patients. Stroke 2004, 35, 2867–2872. [Google Scholar] [CrossRef]
- Hornnes, N.; Larsen, K.; Boysen, G. Blood Pressure 1 Year after Stroke: The Need to Optimize Secondary Prevention. J. Stroke Cerebrovasc. Dis. 2011, 20, 16–23. [Google Scholar] [CrossRef]
- Fukuoka, Y.; Hosomi, N.; Hyakuta, T.; Omori, T.; Ito, Y.; Uemura, J.; Yagita, Y.; Kimura, K.; Matsumoto, M.; Moriyama, M.; et al. Effects of a Disease Management Program for Preventing Recurrent Ischemic Stroke. Stroke 2019, 50, 705–712. [Google Scholar] [CrossRef]
- Kronish, I.M.; Goldfinger, J.Z.; Negron, R.; Fei, K.; Tuhrim, S.; Arniella, G.; Horowitz, C.R. Effect of Peer Education on Stroke Prevention. Stroke 2014, 45, 3330–3336. [Google Scholar] [CrossRef] [Green Version]
- Owolabi, M.O.; Gebregziabher, M.; Akinyemi, R.; Akinyemi, J.O.; Akpa, O.; Olaniyan, O.; Salako, B.L.; Arulogun, O.; Tagge, R.; Uvere, E.; et al. Randomized Trial of an Intervention to Improve Blood Pressure Control in Stroke Survivors. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005904. [Google Scholar] [CrossRef]
- Denny, M.C.; Vahidy, F.; Vu, K.Y.T.; Sharrief, A.Z.; Savitz, S.I. Video-based educational intervention associated with improved stroke literacy, self-efficacy, and patient satisfaction. PLoS ONE 2017, 12, e0171952. [Google Scholar] [CrossRef] [Green Version]
- Rodgers, H.; Atkinson, C.; Bond, S.; Suddes, M.; Dobson, R.; Curless, R. Randomized Controlled Trial of a Comprehensive Stroke Education Program for Patients and Caregivers. Stroke 1999, 30, 2585–2591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maasland, E.; Koudstaal, P.J.; Habbema, J.D.F.; Dippel, D.W.J. Effects of an individualized multimedia computer program for health education in patients with a recent minor stroke or transient ischemic attack? A randomized controlled trial. Acta Neurol. Scand. 2007, 115, 41–48. [Google Scholar] [CrossRef]
- Eames, S.; Hoffmann, T.; Worrall, L.; Read, S.; Wong, A. Randomised controlled trial of an education and support package for stroke patients and their carers. BMJ Open 2013, 3, e002538. [Google Scholar] [CrossRef] [PubMed]
- Holmgren, E.; Gosman-Hedström, G.; Lindström, B.; Wester, P. What is the benefit of a high-intensive exercise program on health-related quality of life and depression after stroke? A randomized controlled trial. Adv. Physiother. 2010, 12, 125–133. [Google Scholar] [CrossRef] [Green Version]
- Mandigout, S.; Chaparro, D.; Borel, B.; Kammoun, B.; Salle, J.-Y.; Compagnat, M.; Daviet, J.-C. Effect of individualized coaching at home on walking capacity in subacute stroke patients: A randomized controlled trial (Ticaa’dom). Ann. Phys. Rehabil. Med. 2020, 64, 101453. [Google Scholar] [CrossRef]
- Boysen, G.; Krarup, L.-H.; Zeng, X.; Oskedra, A.; Kõrv, J.; Andersen, G.; Gluud, C.; Pedersen, A.; Lindahl, M.; Hansen, L.; et al. ExStroke Pilot Trial of the effect of repeated instructions to improve physical activity after ischaemic stroke: A multinational randomised controlled clinical trial. BMJ 2009, 339, b2810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Askim, T.; Langhammer, B.; Ihle-Hansen, H.; Gunnes, M.; Lydersen, S.; Indredavik, B.; Engstad, T.; Magnussen, J.; Hansen, A.; Schjørlien, R.; et al. Efficacy and safety of individualized coaching after stroke: The LAST study (life after stroke) a pragmatic randomized controlled trial. Stroke 2018, 49, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Sarfo, F.S.; Treiber, F.; Jenkins, C.; Patel, S.; Gebregziabher, M.; Singh, A.; Sarfo-Kantanka, O.; Saulson, R.; Appiah, L.; Oparebea, E.; et al. Phone-based Intervention under Nurse Guidance after Stroke (PINGS): Study protocol for a randomized controlled trial. Trials 2016, 17, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wan, L.-H.; Zhang, X.-P.; You, L.-M.; Ruan, H.-F.; Chen, S.-X. The Efficacy of a Comprehensive Reminder System to Improve Health Behaviors and Blood Pressure Control in Hypertensive Ischemic Stroke Patients. J. Cardiovasc. Nurs. 2018, 33, 509–517. [Google Scholar] [CrossRef]
- Toledano-Zarhi, A.; Tanne, D.; Carmeli, E.; Katz-Leurer, M. Feasibility, safety and efficacy of an early aerobic rehabilitation program for patients after minor ischemic stroke: A pilot randomized controlled trial. NeuroRehabilitation 2011, 28, 85–90. [Google Scholar] [CrossRef]
- Wan, L.-H.; You, L.-M.; Chen, S.-X.; Zhang, X.-P.; Mo, M.-M.; Zhang, Y.-M.; Ou, C.-L.; Ao, Y.-A.; Xiong, X.-N.; Zhang, M.; et al. The effectiveness of a comprehensive reminder system in the secondary prevention of hypertensive ischaemic stroke: Randomized controlled trial protocol. J. Adv. Nurs. 2016, 72, 3195–3206. [Google Scholar] [CrossRef]
- Hamm, L.F.; Sanderson, B.K.; Ades, P.A.; Berra, K.; Kaminsky, L.A.; Roitman, J.L.; Williams, M.A. Core Competencies for Cardiac Rehabilitation/Secondary Prevention Professionals. J. Cardiopulm. Rehabil. Prev. 2011, 31, 2–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.-I.; Lee, S.; Kim, J.-H. Effects of a web-based stroke education program on recurrence prevention behaviors among stroke patients: A pilot study. Health Educ. Res. 2013, 28, 488–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sanders, K.; Schnepel, L.; Smotherman, C.; Livingood, W.; Dodani, S.; Antonios, N.; Lukens-Bull, K.; Balls-Berry, J.; Johnson, Y.; Miller, T.; et al. Assessing the Impact of Health Literacy on Education Retention of Stroke Patients. Prev. Chronic Dis. 2014, 11, E55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rolls, C.A.; Obamiro, K.O.; Chalmers, L.; Bereznicki, L.R.E. The relationship between knowledge, health literacy, and adherence among patients taking oral anticoagulants for stroke thromboprophylaxis in atrial fibrillation. Cardiovasc. Ther. 2017, 35, e12304. [Google Scholar] [CrossRef]
- Qian, F.; Fonarow, G.C.; Smith, E.E.; Xian, Y.; Pan, W.; Hannan, E.L.; Shaw, B.; Glance, L.G.; Peterson, E.D.; Eapen, Z.J.; et al. Racial and Ethnic Differences in Outcomes in Older Patients with Acute Ischemic Stroke. Circ. Cardiovasc. Qual. Outcomes 2013, 6, 284–292. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flores, L.; Verduzco-Gutierrez, M.; Molinares, D.; Silver, J.K. Disparities in Health Care for Hispanic Patients in Physical Medicine and Rehabilitation in the United States. Am. J. Phys. Med. Rehabil. 2019, 99, 338–347. [Google Scholar] [CrossRef] [PubMed]
- White, H.; Boden-Albala, B.; Wang, C.; Elkind, M.S.; Rundek, T.; Wright, C.B.; Sacco, R.L. Ischemic Stroke Subtype Incidence Among Whites, Blacks, and Hispanics. Circulation 2005, 111, 1327–1331. [Google Scholar] [CrossRef] [Green Version]
- Ravenell, J.; Leighton-Herrmann, E.; Abel-Bey, A.; DeSorbo, A.; Teresi, J.; Valdez, L.; Gordillo, M.; Gerin, W.; Hecht, M.; Ramirez, M.; et al. Tailored approaches to stroke health education (TASHE): Study protocol for a randomized controlled trial. Trials 2015, 16, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Ovbiagele, B.; Diener, H.-C.; Yusuf, S.; Martin, R.H.; Cotton, D.; Vinisko, R.; Donnan, G.; Bath, P.; PROFESS Investigators. Level of Systolic Blood Pressure Within the Normal Range and Risk of Recurrent Stroke. JAMA 2011, 306, 2137–2144. [Google Scholar] [CrossRef] [Green Version]
- Bangalore, S.; Toklu, B.; Gianos, E.; Schwartzbard, A.; Weintraub, H.; Ogedegbe, G.; Messerli, F.H. Optimal Systolic Blood Pressure Target After SPRINT: Insights from a Network Meta-Analysis of Randomized Trials. Am. J. Med. 2017, 130, 707–719.e8. [Google Scholar] [CrossRef] [Green Version]
- Mant, J.; McManus, R.J.; Roalfe, A.; Fletcher, K.; Taylor, C.J.; Martin, U.; Virdee, S.; Greenfield, S.; Hobbs, R. Different systolic blood pressure targets for people with history of stroke or transient ischaemic attack: PAST-BP (Prevention After Stroke—Blood Pressure) randomised controlled trial. BMJ 2016, 352, i708. [Google Scholar] [CrossRef] [Green Version]
- Altmann, M.; Thommessen, B.; Rønning, O.M.; Reichenbach, A.S.; Fure, B. Blood pressure differences between patients with lacunar and nonlacunar infarcts. Brain Behav. 2015, 5, e00353. [Google Scholar] [CrossRef] [Green Version]
- Machline-Carrion, M.J.; Santucci, E.V.; Damiani, L.P.; Bahit, M.C.; Málaga, G.; Pontes-Neto, O.M.; Martins, S.C.O.; Zétola, V.F.; Normilio-Silva, K.; De Freitas, G.R.; et al. Effect of a Quality Improvement Intervention on Adherence to Therapies for Patients with Acute Ischemic Stroke and Transient Ischemic Attack. JAMA Neurol. 2019, 76, 932–941. [Google Scholar] [CrossRef]
- Wein, T.; Lindsay, M.P.; Côté, R.; Foley, N.; Berlingieri, J.; Bhogal, S.; Bourgoin, A.; Buck, B.; Cox, J.; Davidson, D.; et al. Canadian stroke best practice recommendations: Secondary prevention of stroke, sixth edition practice guidelines, update 2017. Int. J. Stroke 2017, 13, 420–443. [Google Scholar] [CrossRef] [PubMed]
- Fonarow, G.C.; Smith, E.; Reeves, M.J.; Pan, W.; Olson, D.; Hernandez, A.F.; Peterson, E.D.; Schwamm, L.; Get with the Guidelines Steering Committee and Hospitals. Hospital-Level Variation in Mortality and Rehospitalization for Medicare Beneficiaries with Acute Ischemic Stroke. Stroke 2011, 42, 159–166. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mampuya, W.M. Cardiac rehabilitation past, present and future: An overview. Cardiovasc. Diagn. Ther. 2012, 2, 38–49. [Google Scholar] [CrossRef] [PubMed]
- Kronish, I.M.; Edmondson, D.; Goldfinger, J.Z.; Fei, K.; Horowitz, C.R. Posttraumatic Stress Disorder and Adherence to Medications in Survivors of Strokes and Transient Ischemic Attacks. Stroke 2012, 43, 2192–2197. [Google Scholar] [CrossRef] [Green Version]
- Benoit, C.; Lopez, D.; Loiseau, M.; Labreuche, J.; Kyheng, M.; Bourdain, F.; Lapergue, B. Impact of a Pre-Discharge Education Session on Stroke Knowledge: A Randomized Trial. J. Stroke Cerebrovasc. Dis. 2020, 29, 105272. [Google Scholar] [CrossRef] [PubMed]
- Jhaveri, M.M.; Benjamin-Garner, R.; Rianon, N.; Sherer, M.; Francisco, G.; Vahidy, F.; Kobayashi, K.; Gaber, M.; Shoemake, P.; Vu, K.; et al. Telemedicine-guided education on secondary stroke and fall prevention following inpatient rehabilitation for Texas patients with stroke and their caregivers: A feasibility pilot study. BMJ Open 2017, 7, e017340. [Google Scholar] [CrossRef] [Green Version]
- Sakakibara, B.M.; Lear, S.A.; Barr, S.I.; Benavente, O.; Goldsmith, C.H.; Silverberg, N.D.; Yao, J.; Eng, J.J. CIHR Author Manuscript A telehealth intervention to promote healthy lifestyles after stroke: The Stroke Coach protocol. Int. J. Stroke 2018, 13, 217–222. [Google Scholar] [CrossRef]
- Mendyk, A.-M.; Network, O.T.B.O.S.; Duhamel, A.; Bejot, Y.; Leys, D.; Derex, L.; Dereeper, O.; Detante, O.; Garcia, P.-Y.; Godefroy, O.; et al. Controlled Education of patients after Stroke (CEOPS)- nurse-led multimodal and long-term interventional program involving a patient’s caregiver to optimize secondary prevention of stroke: Study protocol for a randomized controlled trial. Trials 2018, 19, 137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coombes, J.; Rowett, D.; Whitty, J.A.; Cottrell, N.W. Using a structured, patient-centred, educational exchange to facilitate a shared conversation about stroke prevention medications. J. Eval. Clin. Pract. 2019, 26, 635–644. [Google Scholar] [CrossRef]
- Glass, T.A.; McAtee, M.J. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Soc. Sci. Med. 2006, 62, 1650–1671. [Google Scholar] [CrossRef] [PubMed]
- McKinlay, J.B.; Marceau, L.D. Upstream healthy public policy: Lessons from the battle of tobacco. Int. J. Health Serv. 2000, 30, 49–69. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.A.; Risser, J.M.; Lisabeth, L.D.; Moyé, L.A.; Morgenstern, L.B. Access to Care, Acculturation, and Risk Factors for Stroke in Mexican Americans. Stroke 2003, 34, 2671–2675. [Google Scholar] [CrossRef] [Green Version]
- Urimubenshi, G.; Cadilhac, D.A.; Kagwiza, J.N.; Wu, O.; Langhorne, P. Stroke care in Africa: A systematic review of the literature. Int. J. Stroke 2018, 13, 797–805. [Google Scholar] [CrossRef]
- Pandian, J.D.; Kalkonde, Y.; Sebastian, I.A.; Felix, C.; Urimubenshi, G.; Bosch, J. Stroke systems of care in low-income and middle-income countries: Challenges and opportunities. Lancet 2020, 396, 1443–1451. [Google Scholar] [CrossRef]
- Lear, S.A.; Singer, J.; Banner-Lukaris, D.; Horvat, D.; Park, J.E.; Bates, J.; Ignaszewski, A. Improving access to cardiac rehabilitation using the internet: A randomized trial. Stud. Health Technol. Inform. 2015, 209, 58. [Google Scholar]
- Mandic, S.; Body, D.; Barclay, L.; Walker, R.; Nye, E.R.; Grace, S.; Williams, M. Community-Based Cardiac Rehabilitation Maintenance Programs: Use and Effects. Hear. Lung Circ. 2015, 24, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Cameron, J.I.; Tsoi, C.; Marsella, A. Optimizing Stroke Systems of Care by Enhancing Transitions Across Care Environments. Stroke 2008, 39, 2637–2643. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Broderick, J.P.; Abir, M. Transitions of Care for Stroke Patients. Circ. Cardiovasc. Qual. Outcomes 2015, 8, S190–S192. [Google Scholar] [CrossRef] [PubMed]
- Transitional Care Services Cost-Effective after Hospitalization for Heart Failure, Study Finds|News Center|Stanford Medicine. Available online: https://med.stanford.edu/news/all-news/2020/01/transitional-services-after-heart-failure-worth-cost.html (accessed on 15 May 2021).
- Rattray, N.A.; Sico, J.J.; Cox, L.M.; Russ, A.L.; Matthias, M.S.; Frankel, R.M. Crossing the Communication Chasm: Challenges and Opportunities in Transitions of Care from the Hospital to the Primary Care Clinic. Jt. Comm. J. Qual. Patient Saf. 2017, 43, 127–137. [Google Scholar] [CrossRef] [Green Version]
- Blum, M.; Øien, H.; Carmichael, H.L.; Heidenreich, P.; Owens, D.K.; Goldhaber-Fiebert, J.D. Cost-Effectiveness of Transitional Care Services After Hospitalization with Heart Failure. Ann. Intern. Med. 2020, 172, 248. [Google Scholar] [CrossRef]
- Blane, D.N.; Macdonald, S.; O’Donnell, C.A. What works and why in the identification and referral of adults with comorbid obesity in primary care: A realist review. Obes. Rev. 2019, 21, e12979. [Google Scholar] [CrossRef]
- Bettger, J.P.; Alexander, K.P.; Dolor, R.J.; Olson, D.M.; Kendrick, A.S.; Wing, L.; Coeytaux, R.R.; Graffagnino, C.; Duncan, P.W. Transitional Care After Hospitalization for Acute Stroke or Myocardial Infarction. Ann. Intern. Med. 2012, 157, 407–416. [Google Scholar] [CrossRef]
- Nathans, A.M.; Bhole, R.; Finch, C.K.; George, C.M.; Alexandrov, A.V.; March, K.L. Impact of a Pharmacist-Driven Poststroke Transitions of Care Clinic on 30 and 90-Day Hospital Readmission Rates. J. Stroke Cerebrovasc. Dis. 2020, 29, 104648. [Google Scholar] [CrossRef]
- Schölmerich, V.L.N.; Kawachi, I. Translating the Socio-Ecological Perspective into Multilevel Interventions. Health Educ. Behav. 2016, 43, 17–20. [Google Scholar] [CrossRef] [Green Version]
| Study Design | Target Population | Level of Intervention 1 | Delivery Method 1 | Study Leader 1 | Effectiveness | Strategy |
|---|---|---|---|---|---|---|
| What was the outlined design strategy referenced in the “methods” section? | Who was the study defined to benefit? | Where in the healthcare model was the intervention targeted to take effect? | How was the intervention provided to the target group? | Who oversaw the delivery of the intervention to the target group? | Was the study effectively able to accomplish significant change compared to the control group or pre-test levels? | What is the overarching aim of the intervention? |
| RCT 2 Non-RCT 2 Cluster randomized, Prospective cohort, Mixed methods, Pre/post-test | Patients Caregivers Providers | One (individual) Two (provider) | Live Written materials Automated Virtual | Nurse Physician Researcher HCW 2 MDT 2 AHP 2 Care coordinator Peer Leader Computer-led | Long-term Effective Short-term Effective Not Effective | Adherence to Care Plan Education Physical Activity |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lambert, C.M.; Olulana, O.; Bailey-Davis, L.; Abedi, V.; Zand, R. “Lessons Learned” Preventing Recurrent Ischemic Strokes through Secondary Prevention Programs: A Systematic Review. J. Clin. Med. 2021, 10, 4209. https://doi.org/10.3390/jcm10184209
Lambert CM, Olulana O, Bailey-Davis L, Abedi V, Zand R. “Lessons Learned” Preventing Recurrent Ischemic Strokes through Secondary Prevention Programs: A Systematic Review. Journal of Clinical Medicine. 2021; 10(18):4209. https://doi.org/10.3390/jcm10184209
Chicago/Turabian StyleLambert, Clare McGarvey, Oluwaseyi Olulana, Lisa Bailey-Davis, Vida Abedi, and Ramin Zand. 2021. "“Lessons Learned” Preventing Recurrent Ischemic Strokes through Secondary Prevention Programs: A Systematic Review" Journal of Clinical Medicine 10, no. 18: 4209. https://doi.org/10.3390/jcm10184209
APA StyleLambert, C. M., Olulana, O., Bailey-Davis, L., Abedi, V., & Zand, R. (2021). “Lessons Learned” Preventing Recurrent Ischemic Strokes through Secondary Prevention Programs: A Systematic Review. Journal of Clinical Medicine, 10(18), 4209. https://doi.org/10.3390/jcm10184209









