The Role of IONM in Reducing the Occurrence of Shoulder Syndrome Following Lateral Neck Dissection for Thyroid Cancer
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Setting and Participants
2.3. Preoperative Work Out
2.4. Surgical Procedure
2.5. IONM System
2.6. Variables
2.7. Statistical Analysis
3. Results
3.1. Demographic and Surgical Results
3.2. Lymph Node Retrieval
3.3. Thyroid Cancer Subtypes
3.4. IONM Use
3.5. Functional Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- Lindfors, H.; Ihre Lundgren, C.; Zedenius, J.; Juhlin, C.C.; Shabo, I. The Clinical Significance of Lymph Node Ratio and Ki-67 Expression in Papillary Thyroid Cancer. World J. Surg. 2021, 45, 2155–2164. [Google Scholar] [CrossRef] [PubMed]
- Polistena, A.; Monacelli, M.; Lucchini, R.; Triola, R.; Conti, C.; Avenia, S.; Barillaro, I.; Sanguinetti, A.; Avenia, N. Surgical morbidity of cervical lymphadenectomy for thyroid cancer: A retrospective cohort study over 25 years. Int. J. Surg. 2015, 21, 128–134. [Google Scholar] [CrossRef] [PubMed]
- Wells, S.A., Jr.; Asa, S.L.; Dralle, H.; Elisei, R.; Evans, D.B.; Gagel, R.F.; Lee, N.; Machens, A.; Moley, J.F.; Pacini, F.; et al. American Thyroid Association Guidelines Task Force on Medullary Thyroid Carcinoma. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 2015, 25, 567–610. [Google Scholar] [CrossRef] [PubMed]
- Bible, K.C.; Kebebew, E.; Brierley, J.; Brito, J.P.; Cabanillas, M.E.; Clark, T.J., Jr.; Di Cristofano, A.; Foote, R.; Giordano, T.; Kasperbauer, J.; et al. 2021 American Thyroid Association Guidelines for Management of Patients with Anaplastic Thyroid Cancer. Thyroid 2021, 31, 337–386. [Google Scholar] [CrossRef]
- Polistena, A.; Sanguinetti, A.; Lucchini, R.; Galasse, S.; Monacelli, M.; Avenia, S.; Boccolini, A.; Johnson, L.B.; Avenia, N. Timing and extension of lymphadenectomy in medullary thyroid carcinoma: A case series from a single institution. Int. J. Surg. 2017, 41 (Suppl. 1), S70–S74. [Google Scholar] [CrossRef] [PubMed]
- Polistena, A.; Monacelli, M.; Lucchini, R.; Triola, R.; Conti, C.; Avenia, S.; Barillaro, I.; Sanguinetti, A.; Avenia, N. Approach to lymph node metastases in sporadic medullary thyroid carcinoma An istitutional experience. Ann. Ital. Chir. 2015, 86, 390–395. [Google Scholar]
- Polistena, A.; Monacelli, M.; Lucchini, R.; Triola, R.; Conti, C.; Avenia, S.; Rondelli, F.; Bugiantella, W.; Barillaro, I.; Sanguinetti, A.; et al. The role of surgery in the treatment of thyroid anaplastic carcinoma in the elderly. Int. J. Surg. 2014, 12, S170–S176. [Google Scholar] [CrossRef][Green Version]
- Conzo, G.; Polistena, A.; Calò, P.G.; Bononi, P.; Gambardella, C.; Mauriello, C.; Tartaglia, E.; Avenia, S.; Sanguinetti, A.; Medas, F.; et al. Efficacy of combined treatment for anaplastic thyroid carcinoma: Results of a multinstitutional retrospective analysis. Int. J. Surg. 2014, 12 (Suppl. 1), S178–S182. [Google Scholar] [CrossRef] [PubMed]
- Gane, E.M.; McPhail, S.M.; Hatton, A.L.; Panizza, B.J.; O’Leary, S.P. Neck and Shoulder Motor Function following Neck Dissection: A Comparison with Healthy Control Subjects. Otolaryngol. Head Neck Surg. 2019, 160, 1009–1018. [Google Scholar] [CrossRef]
- McGarvey, A.C.; Chiarelli, P.E.; Osmotherly, P.G.; Hoffman, G.R. Physiotherapy for accessory nerve shoulder dysfunction following neck dissection surgery: A literature review. Head Neck 2011, 33, 274–280. [Google Scholar] [CrossRef]
- Eickmeyer, S.M.; Walczak, C.K.; Myers, K.B.; Lindstrom, D.R.; Layde, P.; Campbell, B.H. Quality of life, shoulder range of motion, and spinal accessory nerve status in 5-year survivors of head and neck cancer. PM R 2014, 12, 1073–1080. [Google Scholar] [CrossRef]
- Bradley, P.J.; Ferlito, A.; Silver, C.E.; Takes, R.P.; Woolgar, J.A.; Strojan, P.; Suárez, C.; Coskun, H.; Zbären, P.; Rinaldo, A. Neck treatment and shoulder morbidity: Still a challenge. Head Neck 2011, 33, 1060–1067. [Google Scholar] [CrossRef] [PubMed]
- Lanisnik, B.; Zargi, M.; Rodi, Z. Electrophysiologic analysis of injury to cranial nerve XI during neck dissection. Head Neck 2016, 38 (Suppl. 1), E372–E376. [Google Scholar] [CrossRef] [PubMed]
- Gane, E.M.; Michaleff, Z.A.; Cottrell, M.A.; McPhail, S.M.; Hatton, A.L.; Panizza, B.J.; O’Leary, S.P. Prevalence, incidence, and risk factors for shoulder and neck dysfunction after neck dissection: A systematic review. Eur. J. Surg. Oncol. 2017, 43, 1199–1218. [Google Scholar] [CrossRef] [PubMed]
- Larsen, M.H.; Lorenzen, M.M.; Bakholdt, V.; Sørensen, J.A. The prevalence of nerve injuries following neck dissections—A systematic review and meta-analysis. Dan. Med. J. 2020, 67, A08190464. [Google Scholar]
- McGarvey, A.C.; Hoffman, G.R.; Osmotherly, P.G.; Chiarelli, P.E. Intra-operative monitoring of the spinal accessory nerve: A systematic review. J. Laryngol. Otol. 2014, 128, 746–751. [Google Scholar] [CrossRef]
- Birinci, Y.; Genc, A.; Ecevit, M.C.; Erdag, T.K.; Guneri, E.A.; Oztura, I.; Evlice, A.; Ikiz, A.O. Spinal Accessory Nerve Monitoring and Clinical Outcome Results of Nerve-Sparing Neck Dissections. Otolaryngol. Head Neck Surg. 2014, 151, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Witt, R.L.; Rejto, L. Spinal accessory nerve monitoring in selective and modified neck dissection. Laryngoscope 2007, 117, 776–780. [Google Scholar] [CrossRef] [PubMed]
- Witt, R.L.; Gillis, T.; Pratt, R., Jr. Spinal accessory nerve monitoring with clinical outcome measures. Ear Nose Throat J. 2006, 85, 540–544. [Google Scholar] [CrossRef] [PubMed]
- Cirocchi, R.; Arezzo, A.; D’Andrea, V.; Abraha, I.; Popivanov, G.I.; Avenia, N.; Gerardi, C.; Henry, B.M.; Randolph, J.; Barczyñski, M. Intraoperative neuromonitoring versus visual nerve identification for prevention of recurrent laryngeal nerve injury in adults undergoing thyroid surgery. Cochrane Database Syst. Rev. 2019, 1, CD012483. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Graves, M.J.; Vikse, J.; Sanna, B.; Pękala, P.A.; Walocha, J.A.; Barczyński, M.; Tomaszewski, K.A. The current state of intermittent intraoperative neural monitoring for prevention of recurrent laryngeal nerve injury during thyroidectomy: A PRISMA-compliant systematic review of overlapping meta-analyses. Langenbecks Arch. Surg. 2017, 402, 663–673. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef] [PubMed]
- Smallridge, R.C.; Ain, K.B.; Asa, S.L.; Bible, K.C.; Brierley, J.D.; Burman, K.D.; Kebebew, E.; Lee, N.Y.; Nikiforov, Y.E.; Rosenthal, M.S.; et al. American Thyroid Association Anaplastic Thyroid Cancer Guidelines Taskforce. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid 2012, 22, 1104–1139. [Google Scholar] [CrossRef] [PubMed]
- Rosato, L.; De Crea, C.; Bellantone, R.; Brandi, M.L.; De Toma, G.; Filetti, S.; Miccoli, P.; Pacini, F.; Pelizzo, M.R.; Pontecorvi, A.; et al. Diagnostic, therapeutic and health-care management protocol in thyroid surgery: A position statement of the Italian Association of Endocrine Surgery Units (U.E.C. CLUB). J. Endocrinol. Investig. 2016, 39, 939–953. [Google Scholar] [CrossRef] [PubMed]
- Breckenridge, J.D.; McAuley, J.H. Shoulder Pain and Disability Index (SPADI). J. Physiother. 2011, 57, 197. [Google Scholar] [CrossRef]
- Kang, S.W.; Lee, S.H.; Park, J.H.; Jeong, J.S.; Park, S.; Lee, C.R.; Jeong, J.J.; Nam, K.H.; Chung, W.Y.; Park, C.S. A comparative study of the surgical outcomes of robotic and conventional open modified radical neck dissection for papillary thyroid carcinoma with lateral neck node metastasis. Surg. Endosc. 2012, 26, 3251–3257. [Google Scholar] [CrossRef]
- Ngo, D.Q.; Tran, T.D.; Le, D.T.; Ngo, Q.X.; Van Le, Q. Transoral Endoscopic Modified Radical Neck Dissection for Papillary Thyroid Carcinoma. Ann. Surg. Oncol. 2021, 28, 2766. [Google Scholar] [CrossRef]
- Paek, S.H.; Lee, H.A.; Kwon, H.; Kang, K.H.; Park, S.J. Comparison of robot-assisted modified radical neck dissection using a bilateral axillary breast approach with a conventional open procedure after propensity score matching. Surg. Endosc. 2020, 34, 622–627. [Google Scholar] [CrossRef]
- Dziegielewski, P.T.; McNeely, M.L.; Ashworth, N.; O’Connell, D.A.; Barber, B.; Courneya, K.S.; Debenham, B.J.; Seikaly, H. 2b or not 2b? Shoulder function after level 2b neck dissection: A double-blind randomized controlled clinical trial. Cancer 2020, 126, 1492–1501. [Google Scholar] [CrossRef]
- Sharma, R.K.; Lee, J.; Liou, R.; McManus, C.; Lee, J.A.; Kuo, J.H. Optimal surgeon-volume threshold for neck dissections in the setting of primary thyroid malignancies. Surgery 2021, 12. [Google Scholar] [CrossRef]
- Godballe, C.; Madsen, A.R.; Sørensen, C.H.; Schytte, S.; Trolle, W.; Helweg-Larsen, J.; Barfoed, L.; Kristiansen, L.; Sørensen, V.Z.; Samuelsen, G.; et al. Risk factors for recurrent nerve palsy after thyroid surgery: A national study of patients treated at Danish departments of ENT Head and Neck Surgery. Eur. Arch. Otorhinolaryngol. 2014, 271, 2267–2276. [Google Scholar] [CrossRef]
- Loyo, M.; Tufano, R.P.; Gourin, C.G. National trends in thyroid surgery and the effect of volume on short-term outcomes. Laryngoscope 2013, 123, 2056–2063. [Google Scholar] [CrossRef] [PubMed]
- Prete, F.P.; Sgaramella, L.I.; Di Meo, G.; Pasculli, A.; Calculli, G.; Protopapa, G.; Gurrado, A.; Testini, M. Introducing routine intraoperative nerve monitoring in a high-volume endocrine surgery centre: A health technology assessment. Updates Surg. 2021, 1–11, Epub ahead of print. [Google Scholar] [CrossRef]
- Ferlito, A.; Robbins, K.T.; Silver, C.E.; Hasegawa, Y.; Rinaldo, A. Classification of neck dissections: An evolving system. Auris Nasus Larynx 2009, 36, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Ferlito, A.; Robbins, K.T.; Shah, J.P.; Medina, J.E.; Silver, C.E.; Al-Tamimi, S.; Fagan, J.J.; Paleri, V.; Takes, R.P.; Bradford, C.R.; et al. Proposal for a rational classification of neck dissections. Head Neck 2011, 33, 445–450. [Google Scholar] [CrossRef] [PubMed]
- Popovski, V.; Benedetti, A.; Popovic-Monevska, D.; Grcev, A.; Stamatoski, A.; Zhivadinovik, J. Spinal accessory nerve preservation in modified neck dissections: Surgical and functional outcomes. Acta Otorhinolaryngol. Ital. 2017, 37, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Svenberg Lind, C.; Lundberg, B.; Hammarstedt Nordenvall, L.; Heiwe, S.; Persson, J.K.; Hydman, J. Quantification of Trapezius Muscle Innervation During Neck Dissections: Cervical Plexus Versus the Spinal Accessory Nerve. Ann. Otol. Rhinol. Laryngol. 2015, 124, 881–885. [Google Scholar] [CrossRef]
- McGarvey, A.C.; Hoffman, G.R.; Osmotherly, P.G.; Chiarelli, P.E. Maximizing shoulder function after accessory nerve injury and neck dissection surgery: A multicenter randomized controlled trial. Head Neck 2015, 37, 1022–1031. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.S. Do patients benefit from physiotherapy for shoulder dysfunction following neck dissection? A systematic review. J. Laryngol. Otol. 2020, 134, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Do, J.H.; Yoon, I.J.; Cho, Y.K.; Ahn, J.S.; Kim, J.K.; Jeon, J. Comparison of hospital based and home based exercise on quality of life, and neck and shoulder function in patients with spinal accessary nerve injury after head and neck cancer surgery. Oral Oncol. 2018, 86, 100–104. [Google Scholar] [CrossRef]
- Barber, B.; McNeely, M.; Chan, K.M.; Beaudry, R.; Olson, J.; Harris, J.; Seikaly, H.; O’Connell, D. Intraoperative brief electrical stimulation (BES) for prevention of shoulder dysfunction after oncologic neck dissection: Study protocol for a randomized controlled trial. Trials 2015, 16, 240. [Google Scholar] [CrossRef]
- Al-Qurayshi, Z.; Sullivan, C.B.; Pagedar, N.; Randolph, G.; Kandil, E. Prevalence of major structures injury in thyroid and neck surgeries: A national perspective. Gland Surg. 2020, 9, 1924–1932. [Google Scholar] [CrossRef]
- Sahli, Z.T.; Zhou, S.; Sharma, A.K.; Segev, D.L.; Massie, A.; Zeiger, M.A.; Mathur, A. Rising Cost of Thyroid Surgery in Adult Patients. J. Surg. Res. 2021, 260, 28–37. [Google Scholar] [CrossRef]
- Polistena, A.; Di Lorenzo, P.; Sanguinetti, A.; Buccelli, C.; Conzo, G.; Conti, A.; Niola, M.; Avenia, N. Medicolegal implications of surgical errors and complications in neck surgery: A review based on the Italian current legislation. Open Med. 2016, 11, 298–306. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Sun, H. The application of intraoperative neuromonitoring in lateral neck dissections for thyroid cancers. Ann. Thyroid 2019, 4, 15. [Google Scholar] [CrossRef]
- Lee, C.H.; Huang, N.C.; Chen, H.C.; Chen, M.K. Minimizing shoulder syndrome with intra-operative spinal accessory nerve monitoring for neck dissection. Acta Otorhinolaryngol. Ital. 2013, 33, 93–96. [Google Scholar] [PubMed]
- Parmeggiani, D.; Gambardella, C.; Patrone, R.; Polistena, A.; De Falco, M.; Ruggiero, R.; Cirocchi, R.; Sanguinetti, A.; Cuccurullo, V.; Accardo, M.; et al. Radioguided thyroidectomy for follicular tumors: Multicentric experience. Int. J. Surg. 2017, 41, S75–S81. [Google Scholar] [CrossRef] [PubMed]


| Years, Mean ± SD | |
|---|---|
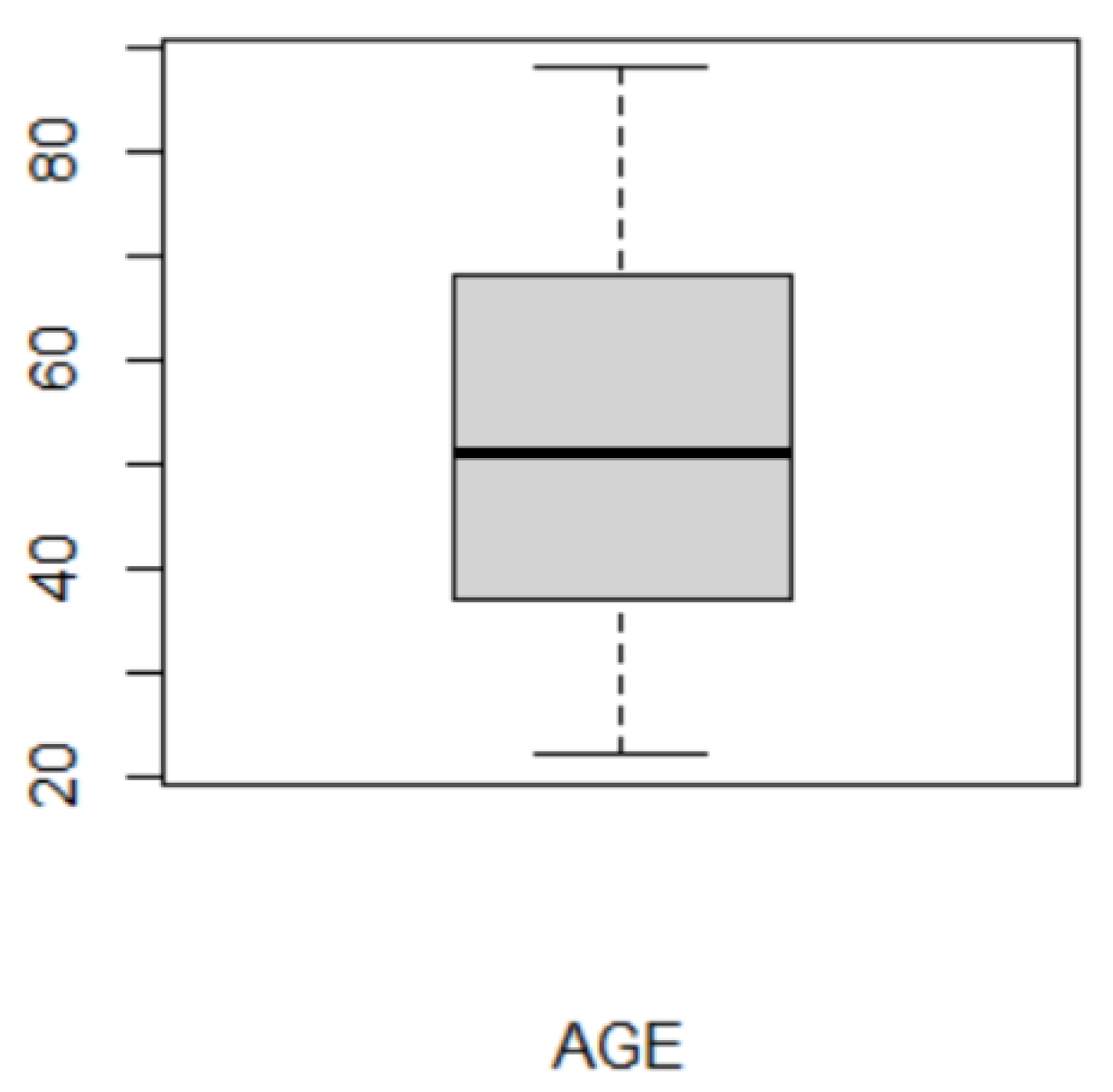
| Age | 51.20 ± 17.59 |
| n (%) | |
| Gender | |
| Female | 30 (53.57) |
| Male | 26 (46.43) |
| Surgical procedure | |
| MRND + TT | 19 (33.93) |
| MRND + TT + CND | 19 (33.93) |
| MRND + CND | 3 (5.36) |
| MRND | 15 (26.79) |
| Side of the procedure | |
| Right | 28 (50) |
| Left | 28 (50) |
| Thyroid cancer subtype | |
| PTC | 40 (71.43) |
| FTC | 7 (12.50) |
| MTC | 6 (10.71) |
| PDTC | 3 (5.36) |
| SPDI | SPDI | |
|---|---|---|
| p.o. day 3 | 6 Months | Type of Nerve Lesion |
| IONM+ visualization (n = 2) | ||
| 57% | 4% | transient |
| 60% | 5% | transient |
| Visualization only (n = 4) | ||
| 60% | 10% | transient |
| 38% | 0% | transient |
| 55% | 6% | transient |
| 75% | 60% | permanent |
| Nerve Identification and Monitoring | No Lesion (n) | Temporary Lesion (n) | Permanent Lesion (n) |
|---|---|---|---|
| IONM+visualization | 91.3% (21) | 8.7% (2) | 0% (0) |
| Visualization only | 87.88% (29) | 9.09% (3) | 3.03% (1) |
| Overall | 89.29% (50) | 8.93% (5) | 1.79% (1) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polistena, A.; Ranalli, M.; Avenia, S.; Lucchini, R.; Sanguinetti, A.; Galasse, S.; Rondelli, F.; Vannucci, J.; Patrone, R.; Velotti, N.; et al. The Role of IONM in Reducing the Occurrence of Shoulder Syndrome Following Lateral Neck Dissection for Thyroid Cancer. J. Clin. Med. 2021, 10, 4246. https://doi.org/10.3390/jcm10184246
Polistena A, Ranalli M, Avenia S, Lucchini R, Sanguinetti A, Galasse S, Rondelli F, Vannucci J, Patrone R, Velotti N, et al. The Role of IONM in Reducing the Occurrence of Shoulder Syndrome Following Lateral Neck Dissection for Thyroid Cancer. Journal of Clinical Medicine. 2021; 10(18):4246. https://doi.org/10.3390/jcm10184246
Chicago/Turabian StylePolistena, Andrea, Monia Ranalli, Stefano Avenia, Roberta Lucchini, Alessandro Sanguinetti, Sergio Galasse, Fabio Rondelli, Jacopo Vannucci, Renato Patrone, Nunzio Velotti, and et al. 2021. "The Role of IONM in Reducing the Occurrence of Shoulder Syndrome Following Lateral Neck Dissection for Thyroid Cancer" Journal of Clinical Medicine 10, no. 18: 4246. https://doi.org/10.3390/jcm10184246
APA StylePolistena, A., Ranalli, M., Avenia, S., Lucchini, R., Sanguinetti, A., Galasse, S., Rondelli, F., Vannucci, J., Patrone, R., Velotti, N., Conzo, G., & Avenia, N. (2021). The Role of IONM in Reducing the Occurrence of Shoulder Syndrome Following Lateral Neck Dissection for Thyroid Cancer. Journal of Clinical Medicine, 10(18), 4246. https://doi.org/10.3390/jcm10184246








