Body Image in Borderline Personality Disorder: A Systematic Review of the Emerging Empirical Literature
Abstract
:1. Introduction
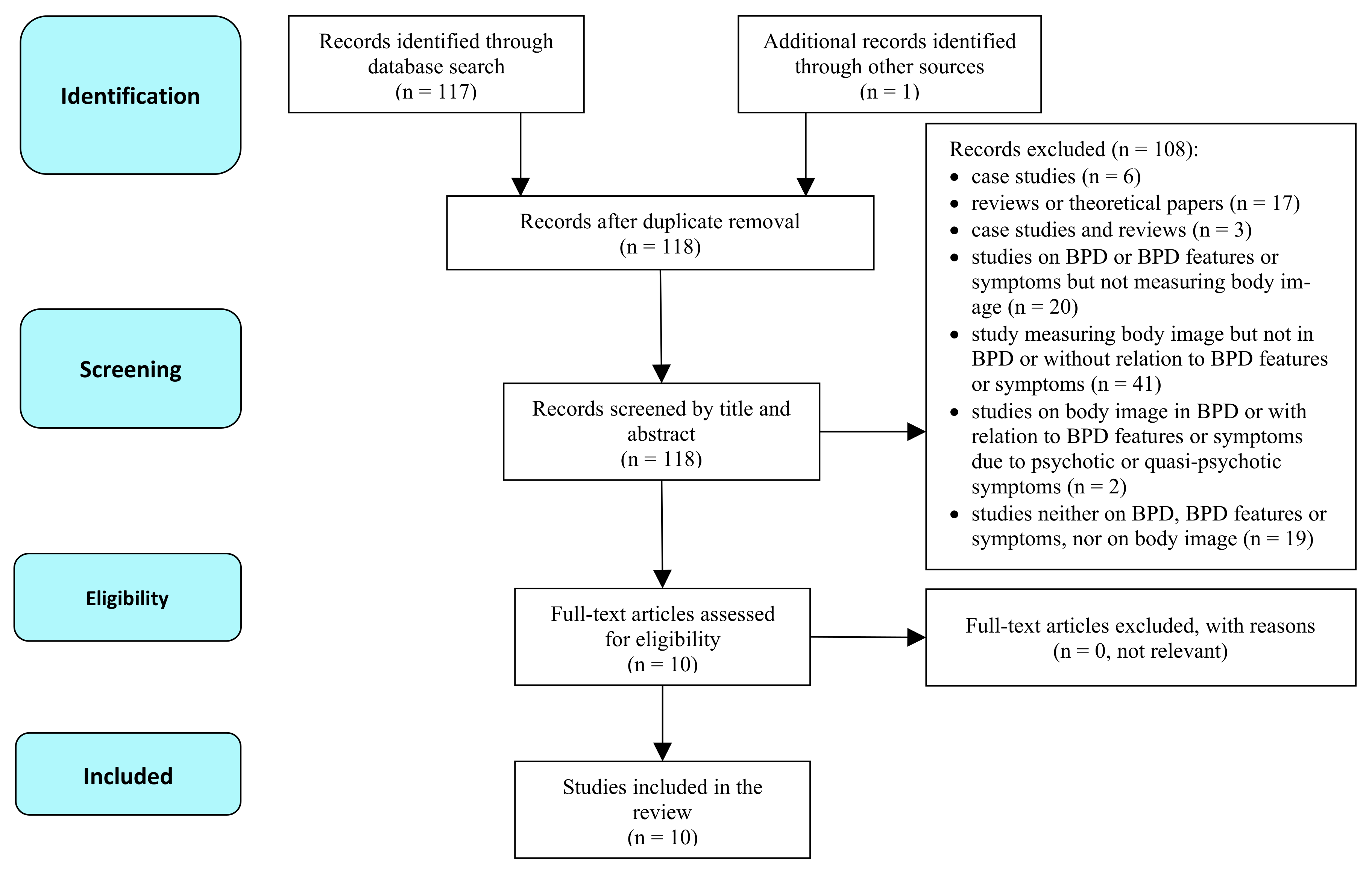
2. Methods
2.1. Search Strategy
2.2. Inclusion Criteria
3. Results
3.1. Characteristics of the Studies
3.2. Results by Body Image Components
3.2.1. Body Perception (Body Regard, Body Attitude)
3.2.2. Affect and Cognition
3.2.3. General Body Dissatisfaction
4. Discussion
4.1. Limitations
4.2. Future Directions and Practical Clinical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Sansone, R.A.; Chu, J.W.; Wiederman, M.W. Body image and borderline personality disorder among psychiatric inpatients. Compr. Psychiatry 2010, 51, 579–584. [Google Scholar] [CrossRef]
- Levy, K.N.; Edell, W.S.; McGlashan, T.H. Depressive experiences in inpatients with borderline personality disorder. Psychiatr. Quart 2007, 78, 129–143. [Google Scholar] [CrossRef]
- Cash, T.F. Cognitive-behavioral perspectives on body image. In Body Image: A handbook of Theory, Research and Clinical Practice; Cash, T.F., Pruzinsky, T., Eds.; The Guilford Press: New York, NY, USA, 2004. [Google Scholar]
- Griffen, T.C.; Naumann, E.; Hildebrandt, T. Mirror exposure therapy for body image disturbances and eating disorders: A review. Clin. Psychol. Rev. 2018, 65, 163–174. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases, 10th ed.; WHO Press: Geneva, Switzerland, 1998. [Google Scholar]
- Farstad, S.M.; McGeown, L.; von Ranson, K.M. Eating disorders and personality, 2004–2016: A systematic review and meta-analysis. Clin. Psychol. Rev. 2016, 46, 91–105. [Google Scholar] [CrossRef]
- Coon, D. Essentials of Psychology, 6th ed.; West Publishing Company: Eagan, MN, USA, 1994. [Google Scholar]
- Bailey, J.A. Self-image, self-concept, and self-identity revisited. J. Natl. Med. Assoc. 2003, 95, 383–386. [Google Scholar] [PubMed]
- Kernberg, O. The diagnosis of borderline conditions in adolescence. Adolesc. Psychiatry 1978, 6, 298–319. [Google Scholar] [PubMed]
- Rüsch, N.; Lieb, K.; Göttler, I.; Hermann, C.; Schramm, E.; Richter, H.; Jacob, G.A.; Corrigan, P.W.; Bohus, M. Shame and implicit self-concept in women with borderline personality disorder. Am. J. Psychiatry 2007, 194, 766–773. [Google Scholar] [CrossRef] [PubMed]
- Dyer, A.; Borgmann, E.; Feldmann, R.E.; Kleindienst, N.; Priebe, K.; Bohus, M.; Vocks, S. Body image disturbance in patients with borderline personality disorder: Impact of eating disorders and perceived childhood sexual abuse. Body Image 2013, 10, 220–225. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Dyer, A.S.; Feldmann, R.E., Jr.; Borgmann, E. Body-related emotions in posttraumatic stress disorder following childhood sexual abuse. J. Child. Sex. Abus. 2015, 24, 627–640. [Google Scholar] [CrossRef]
- Kleindienst, N.; Priebe, K.; Borgmann, E.; Cornelisse, S.; Krüger, A.; Ebner-Priemer, U.; Dyer, A. Body self-evaluation and physical scars in patients with borderline personality disorder. Bord. Pers. Disord. Emot. Dysregulation 2014, 1, 2. [Google Scholar] [CrossRef]
- Kleindienst, N.; Löffler, A.; Herzig, M.; Bertsch, K.; Bekrater-Bodmann, R. Evaluation of the own body in women with current and remitted borderline personality disorder: Evidence for long-lasting effects of childhood sexual abuse. Eur. J. Psychotraumatol. 2020, 11, 1764707. [Google Scholar] [CrossRef] [PubMed]
- Witthöft, M.; Borgmann, E.; White, A.; Dyer, A. Body-related attentional biases in patients with posttraumatic stress disorder resulting from childhood sexual abuse with and without co-occurring borderline personality disorder. J. Behav. Ther. Exp. Psychiatry 2015, 46, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Sansone, R.A.; Wiederman, M.W.; Monteith, D. Obesity, borderline personalitysymptomatology, and body image among women in a psychiatric outpatient setting. Int. J. Eat. Disord. 2001, 29, 76–79. [Google Scholar] [CrossRef]
- Dyer, A.; Hennrich, L.; Borgmann, E.; White, A.J.; Alpers, G.W. Body image and noticeable self-inflicted scars. J. Nerv. Ment. Dis. 2013, 201, 1080–1084. [Google Scholar] [CrossRef]
- Muehlenkamp, J.J.; Bagge, C.L.; Tull, M.T.; Gratz, K.L. Body regard as a moderator of the relation between emotion dysregulation and non-suicidal self-injury. Suicide Life-Threat. Behav. 2013, 43, 479–493. [Google Scholar]
- Steiger, H.; Leung, F.Y.K.; Houle, L. Relationships among borderline features, body dissatisfaction and bulimic symptoms in nonclinical females. Addict. Behav. 1992, 17, 397–406. [Google Scholar] [CrossRef]
- Walsh, B.W. The Body Attitudes Scale; Unpublished manuscript; 1999. [Google Scholar]
- Rosen, J.C.; Srebnik, D.; Saltzberg, E.; Wendt, S. Development of a Body Image Avoidance Questionnaire. Psychol. Assess. 1991, 3, 32–37. [Google Scholar] [CrossRef]
- Cash, T.F.; Labarge, A.S. Development of the Appearance Schemas Inventory: A new cognitive body-image assessment. Cognit. Ther. Res. 1996, 20, 37–50. [Google Scholar] [CrossRef]
- Garner, D.M.; Olmsted, M.P.; de Polivy, J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int. J. Eat. Disord. 1983, 2, 15–34. [Google Scholar] [CrossRef]
- Kling, J.; Kwakkenbos, L.; Diedrichs, P.C.; Rumsey, N.; Frisén, A.; Brandão, M.P.; Silva, A.G.; Dooley, B.; Rodgers, R.F.; Fitzgerald, A. Systematic review of body image measures. Body Image 2019, 30, 170–211. [Google Scholar] [CrossRef] [PubMed]
- Seehausen, A.; Brenner, C.; Wallis-Simon, H.; Ripper, S.; Otte, M.; Hartmann, B.; Renneberg, B. Body image of people with scars and disfigurement: A questionnaire for the assessment of body image after burn injury. Verhal. Verhal. 2010, 31, 399–414. [Google Scholar]
- Brown, T.; Cash, T.; Mikulka, P. Attitudinal body-image assessment: Factor analysis of the Body-Self Relations Questionnaire. J. Pers. Assess. 1990, 55, 135–144. [Google Scholar] [PubMed]
- Cash, T.F. The Multidimensional Body-Self Relations Questionnaire. User’s Manual. 2000. Available online: http:/www.body-images.com (accessed on 1 July 2021).
- Conte, H.; Plutchik, R.; Karasu, T.B.; Jerret, I. A self-report borderline scale, discriminative validity and preliminary norms. J. Nerv. Ment. Disord. 1980, 168, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Weaver, T.L.; Resnick, H.S.; Kokoska, M.S.; Etzel, J.C. Appearance-related residual injury, posttraumatic stress, and body image: Associations within a sample of female victims of intimate partner violence. J. Trauma Stress 2007, 20, 999–1008. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, H. Body-image dissatisfaction as a predictor of suicidal ideation among Korean boys and girls in different stages of adolescence: A two-year longitudinal study. J. Adolesc. Health 2009, 45, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Cano, T.; Beato-Fernández, L.; Llario, A. Body dissatisfaction as a predictor of self-reported suicide attempts in adolescents: A Spanish community prospective study. J. Adolesc. Health 2006, 38, 684–688. [Google Scholar] [CrossRef] [PubMed]
- He, J.; Sun, S.; Zickgraf, H.F.; Lin, Z.; Fan, X. Meta-analysis of gender differences in body appreciation. Body Image 2020, 33, 90–100. [Google Scholar] [CrossRef]
- Sattler, F.A.; Eickmeyer, S.; Eisenkolb, J. Body image disturbance in children andadolescents with anorexia nervosa and bulimia nervosa: A systematic review. Eat. Weight Disord.—St. 2019, 25, 857–865. [Google Scholar] [CrossRef]
- Fuller-Tyszkiewicz, M. Body image states in everyday life: Evidence from ecological momentary assessment methodology. Body Image 2019, 31, 245–272. [Google Scholar] [CrossRef]
- Gaudio, S.; Quattrocchi, C.C. Neural basis of a multidimensional model of body image distortion in anorexia nervosa. Neurosci. Biobehav. Rev. 2012, 36, 1839–1847. [Google Scholar] [CrossRef]
- Mohr, H.M.; Zimmermann, J.; Roder, C.; Lenz, C.; Overbeck, G.; Grabhorn, R. Separating two components of body image in anorexia nervosa using fMRI. Psychol. Med. 2010, 40, 1519–1529. [Google Scholar] [CrossRef] [PubMed]
- Vizgaitis, A.L.; Lenzenweger, M.F. Pierced identities: Body modification, borderline personality features, identity, and self-concept disturbances. Pers. Disord. Theory Res. Treat. 2019, 10, 154–162. [Google Scholar] [CrossRef] [PubMed]
- Morioka, D.; Ohkubo, F. Borderline personality disorder and aesthetic plastic surgery. Aesthet. Plast. Surg. 2014, 38, 1169–1176. [Google Scholar] [CrossRef]
- Semiz, U.; Basoglu, C.; Cetin, M.; Ebrinc, S.; Uzun, O.; Ergun, B. Body dysmorphic disorder in patients with borderline personality disorder: Prevalence, clinical characteristics, and role of childhood trauma. Acta Neuropsychiatr. 2008, 20, 33–40. [Google Scholar] [CrossRef]
- Mattei, V.D.; Bagliacca, E.P.; Lavezzari, L.; Pierro, R.D.; Carnelli, L.; Zucchi, P. Body Image and Personality in Aesthetic Plastic Surgery: A Case-Control Study. Open J. Med. Psychol. 2015, 4, 35–44. [Google Scholar] [CrossRef] [Green Version]
- Stasik-O’Brien, S.M.; Schmidt, J. The role of disgust in body image disturbance: Incremental predictive power of self-disgust. Body Image 2018, 27, 128–137. [Google Scholar] [CrossRef]
- Von Spreckelsen, P.; Glashouwer, K.A.; Bennik, E.C.; Wessel, I.; de Jong, P.J. Negative body image: Relationships with heightened disgust propensity, disgust sensitivity, and self-directed disgust. PLoS ONE 2018, 13, e0198532. [Google Scholar] [CrossRef]
- Onden-Lim, M.; Wu, R.; Grisham, J.R. Body image concern and selective attention to disgusting and non-self-appearance-related stimuli. Body Image 2012, 9, 535–538. [Google Scholar] [CrossRef]
- Stoffers, J.M.; Völlm, B.A.; Rücker, G.; Timmer, A.; Huband, N.; Lieb, K. Psychol.ogical therapies for people with borderline personality disorder. Cochrane Database Syst. Rev. 2012, 8, CD005652. [Google Scholar]
- Glashouwer, K.A.; Neimeijer, R.A.M.; de Koning, M.L.; Vestjens, M.; Martijn, C. Evaluative conditioning as a body image intervention for adolescents with eating disorders. J. Consult. Clin. Psychol. 2018, 86, 1046–1055. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Study | Country | Group (Overall Sample Size; no. of Women); Clinical Sample Type | Mean Age (SD), Age Range [Years] | Mean Education Level [Years of Education or Degree] | Mean BMI (SD), BMI Range | Study Design | BPDMeasure | Body Image Measure | Main Results | Results by Components of Body Image Disturbances | Limitations |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dyer, Borgmann, et al. [12] | Germany | BPD (N = 89; 89); HCs (N = 41; 41); inpatients and outpatients | MBPD = 31.09 (9.15), NI; MHCs = 31.57 (11.53), NI | NI | MBPD = 26.97 (7.64), NI; MHCs = 25.99 (5.79), NI | Cross-sectional | IPDE, BSL-23 | BIAQ, MBSRQ-AS | History of CSA and comorbid ED independently related to ↑ negative body image | Affect/Cognition: BPD > HC in mean BIAQ and MBSRQ; BPD > HC in BID; BPD + LDED > BPD -LDED in BID | Only self-reported measures of body image; no mean education level; only women |
| Dyer, Feldmann, et al. [18] | Germany | BPD (N = 25; 25); PTSD (N = 23; 23); PTSD + BPD (N = 22; 22); HCs (N = 27; 27); inpatients and outpatients | MBPD = 31.44 (9.31), NI MBPD + PTSD = 30.57 (9.08), NI; MPTSD = 38.91 (8.59), NI; MHCs = 30.82 (10.33), NI | NI | NI, NI | Cross-sectional | IPDE | Modified SBA | ↑ negative emotions toward the body in patients with BPD than in HCs, but ↓ negative than in patients with BPD + PTSD and those with PTSD | Affect/Cognition: BPD + PTSD > BPD -PTSD in negative feelings related to their body; | Significant age differences between the BPD and PTSD groups; no mean education level; no mean BMI; only women; small sample sizes |
| Dyer, Hennrich, et al. [22] | Germany | NSSI (N = 56; 56); A/S (N = 69; 69); general | MNSSI = 27.39 (8.42); MA/S = 27.23 (10.18); NI for each group separately, but 18–60 for the whole sample | NI | MNSSI = 25.57 (8.29), NI; MA/S = 23.47 (6.06), NI | Cross-sectional | BSL-23 | FKBB (EBIABI), MBSRQ-AS | ↑ negative body image in individuals engaged in NSSI than in individuals with A/S | Perception: NSSI > A/S in BPD symptoms, quantity of self-harming behaviors, perception of appearance of the scar; NSSI > A/S in 3/5 assessed BID components | Only self-reported measures of BPD and body image; no mean education level; only women |
| Kleindienst et al. [20] | Germany | BPD (N = 26; 26); rBPD (N = 22; 22); HCs (N = 20; 20); inpatients and outpatients | MBPD = 31.65 (9.09); MrBPD = 29.77 (5.44); MHCs = 27.05 (7.17) | NI | MBPD = 24.91 (5.56), NI; MrBPD = 24.04 (6.60), NI; MHCs = 23.40 (5.32), NI | Cross-sectional | IPDE, BSL-23 | SBA | Participants with rBPD: ↑ positive evaluation of their own body than cBPD who evaluated their own body significantly negatively | General body dissatisfaction: cBPD > rBPD and HCs in the negative evaluation of their own body; negative body image in the cBPD group but positive in the rBPD group in terms of neutral body areas. In cBPD and rBPD: ↑ negative evaluation of sexually connoted body areas than in HCs | Small sample size; only women; age limit (max. 50 years old); no mean education level |
| Kleindienst et al. [19] | Germany | BPD (N = 80; 80); PTSD (N = 36; 36); AD (N = 37; 37); HCs (N = 47; 47); wait-list patients | MBPD = 32.40 (9.68); MPTSD = 36.75 (9.24); MAD = 35.84 (11.72); MHCs = 31.23 (11.52); NI for each group separately, but 18–59 for the whole sample | NI | MBPD = 28.74 (8.62), NI; MPTSD = 26.33 (8.70), NI; MAD = 25.63 (10.23), NI; MHCs = 24.74 (5.65), NI | Cross-sectional | IPDE, BSL-23 | SBA | BPD: ↑ negative self-evaluation with and without PTSD or reported CSA and in other groups; BPD + CSA and BPD–CSA had similar scores in negative body rati ng | General body dissatisfaction: mean evaluation of body areas differed across the 4 diagnostic groups; HCs > PTSD > BPD in average body rating | Only self-reported measures of body image; no mean education level; only women; small sample size (HCs); a speculative nature of scars |
| Muehlenkamp et al. [23] | USA | N = 398; 297; undergraduate students | M = 20.25 (2.45), NI | NI | NI, NI | Cross-sectional | BEST | BAS (4 subscales) | Negative body image as a moderator of the relation between difficulties in emotion regulation and NSSI | Perception: negative associations in body regard and NA, emotional dysregulation. and BPD symptoms; a positive association between NSSI and emotional dysregulation, BPD symptoms and NA. NSSI frequency significantly associated with emotional dysregulation and low body regard | Only self-reported measures of BPD and body image; only a nonclinical sample; no mean education level; no mean BMI |
| Sansone et al. [24] | USA | N = 48; 48 outpatients | M = 32.98 (9.28), 18–56 | NI, but 85.4% women graduated from high school and 22.9% earned an academic degree | NI, but 17 women had BMI > 27.3 (obesity cut-off), NI | Cross-sectional | PDQ-R (BPD subscale) | BIAQ, EDI (BD subscale), 2 items on attractiveness | Patients with BPD features reported ↓ general body satisfaction, ↓ attractiveness, ↓ facial attractiveness, ↑ social avoidance due to body image concerns | Perception: PDQ-R scores positively corelated with BMI and other body image measures; obese women > nonobese women in PDQ-R. General body dissatisfaction: scores on PDQ-R positively correlated with body dissatisfaction. | Only self-reported measures of BPD and body image; no HCs group; no mean education level; no mean BMI; only women |
| Sansone et al. [2] | USA | N = 126; 126; inpatients | M = 34.84 (12.19), 18–74 | NI, but 15.1% did not graduate from high school, 24.4% earned at least a 4-year college degree, and 5.9% earned a graduate degree | NI, NI | Cross-sectional | PDQ-4 (BPD subscale) | ASI (BIVS subscale) | Patients with BPD features reported ↑ negative evaluation of appearance | Affect/Cognition: ↑ BPD features => body image vulnerability, appearance stereotyping, private self-consciousness, public self-consciousness, and a lack of familiarity with one’s own body. | Only self-reporedt measures of BPD and body image; no mean education level; no mean BMI; only women |
| Steiger et al. [25] | Canada | BPD (N = 49; 49); BD/BPD (N = 22; 22); BD (N = 38; 38); BN (N = 22; 22); LR (N = 418; 418); high-school students (BPD, BD/BPD; BD, LR) and inpatients (BN) | MBPD = 15.47 (2.26); MBD/BPD = 16.59 (4.85); MBD = 15.53 (1.80); MBN = 24.50 (4.17); MLR = 15.23 (2.16); NI for the BN group, but 12–18 for the remaining 4 groups | NI | MBPD = 20.61 (2.70), NI; MBD/BPD = 21.45 (2.22), NI; MBN = 22.45 (2.77), NI; MBD = 22.53 (2.44), NI; MLR = 20.50 (2.09), NI | Cross-sectional | BSI | EDI (BDS subscale) | Girls with high body dissatisfaction and severe BPD features showed ↑ eating disorders symptoms, but ↓ than women with BN | General body dissatisfaction: BD/BPD did not significantly differ from BN in the degree of body dissatisfaction | Only self-reported measures of BPD and body image; no mean education level; only women; significant age differences between patients with BN and all other groups; no control for mean BMI; small sample sizes in the BD/BPD and BN groups |
| Witthöft et al. [21] | Germany | BPD + PTSD (N = 29; 29); PTSD (N = 32; 32); HCs (N = 30; 30); inpatients | MBPD + PTSD = 30.72 (8.62), NI; MPTSD = 39.28 (10.15), NI; MHCs = 32.80 (12.01), NI | NI, but ≥10 years was the case for: 73.1% of BPD + PTSD; 58.1% of PTSD; 96.4% of HCs | MBPD + PTSD = 27.69 (7.17), NI; MPTSD = 28.38 (7.49), NI; MHCs = 25.37 (5.52), NI | Experi-mental | IPDE, BSL-23 | EST | Patients with BPD + PTSD reported ↑ attentional bias toward body-related stimuli than those with PTSD and HCs | Affect/cognition : PTSD + BPD > HCs in bias on words related to the body | No self-reported measure of body image; indirect measure of body image; no group with BPD without comorbid PTSD; significant age and education level differences between some of the groups; no mean education level; only women |
| Body Image Measure | Reference | Components of Body Image Measured in the Reviewed Studies |
|---|---|---|
| ASI (BIVS subscale) | Cash, Labarge [24] | Affect and cognition |
| BAS | Walsh [22] | Body perception (body regard) |
| BIAQ | Rosen et al. [23] | Body perception |
| EDI (BDS subscale) | Garner et al. [25] | General body dissatisfaction |
| FKBB (EBIABI) | Seehausen et al. [27] | Body perception (originally designed to specifically measure body perception with regard to burn injuries) |
| MBSRQ-AS | Brown et al. [28]; Cash [29] | Affect and cognition |
| Modified SBA | Dyer et al. [14]; original version: Kleindienst et al. [15] | General body dissatisfaction |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wayda-Zalewska, M.; Kostecka, B.; Kucharska, K. Body Image in Borderline Personality Disorder: A Systematic Review of the Emerging Empirical Literature. J. Clin. Med. 2021, 10, 4264. https://doi.org/10.3390/jcm10184264
Wayda-Zalewska M, Kostecka B, Kucharska K. Body Image in Borderline Personality Disorder: A Systematic Review of the Emerging Empirical Literature. Journal of Clinical Medicine. 2021; 10(18):4264. https://doi.org/10.3390/jcm10184264
Chicago/Turabian StyleWayda-Zalewska, Magdalena, Barbara Kostecka, and Katarzyna Kucharska. 2021. "Body Image in Borderline Personality Disorder: A Systematic Review of the Emerging Empirical Literature" Journal of Clinical Medicine 10, no. 18: 4264. https://doi.org/10.3390/jcm10184264
APA StyleWayda-Zalewska, M., Kostecka, B., & Kucharska, K. (2021). Body Image in Borderline Personality Disorder: A Systematic Review of the Emerging Empirical Literature. Journal of Clinical Medicine, 10(18), 4264. https://doi.org/10.3390/jcm10184264






