The Anatomy of Glenoid Concavity—Bony and Osteochondral Assessment of a Stability-Related Parameter
Abstract
:1. Introduction
2. Materials and Methods
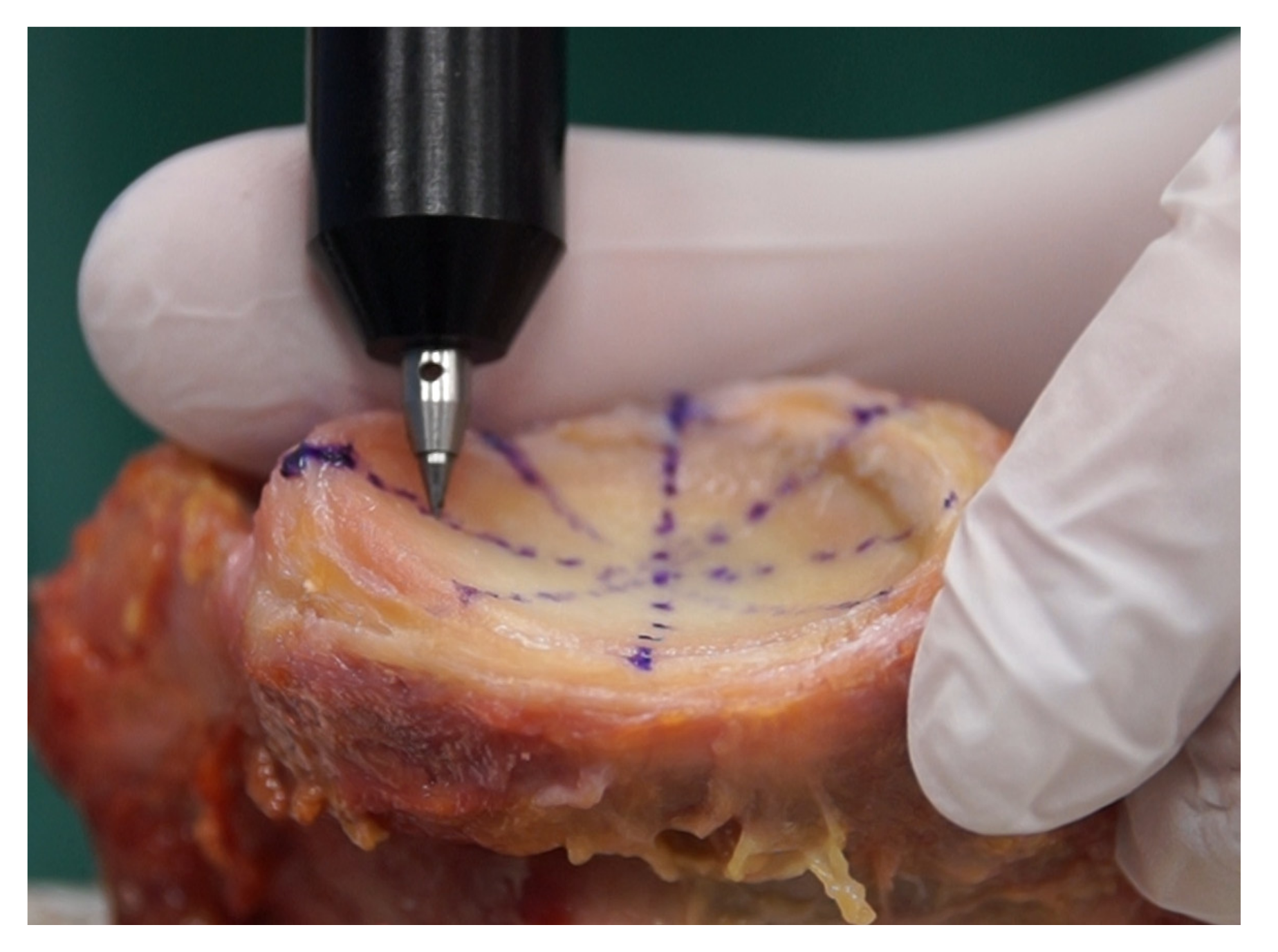
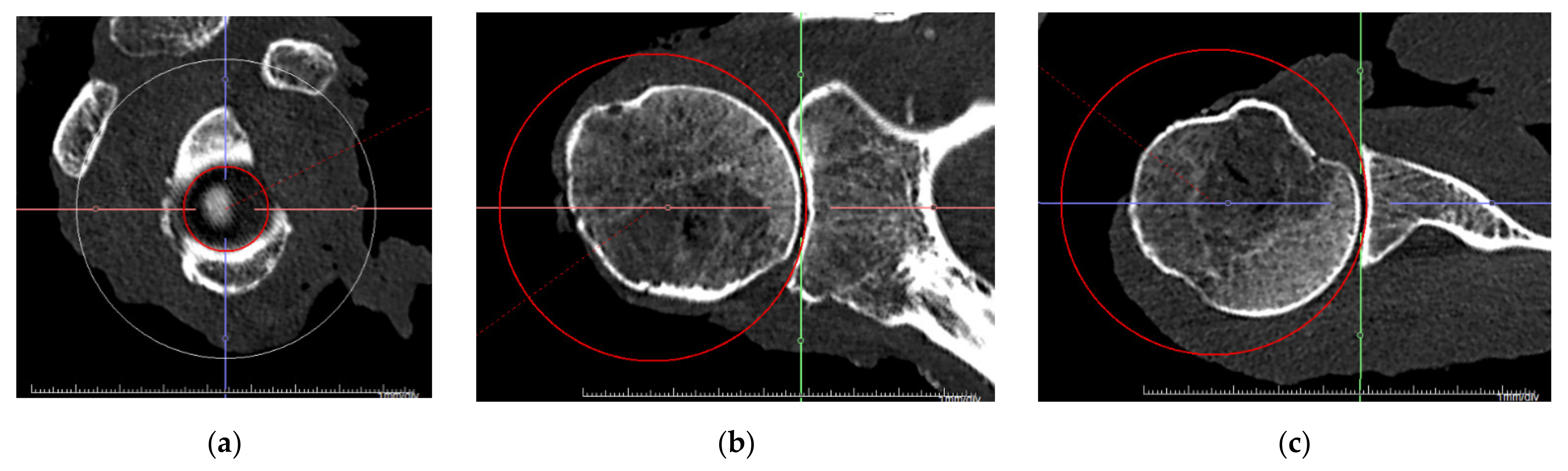
2.1. Specimen Preparation and Data Acquisition
2.2. Definition of Glenoid Axes and Concavity
2.3. Measurements and Outcome Parameter
2.4. Statistical Analysis
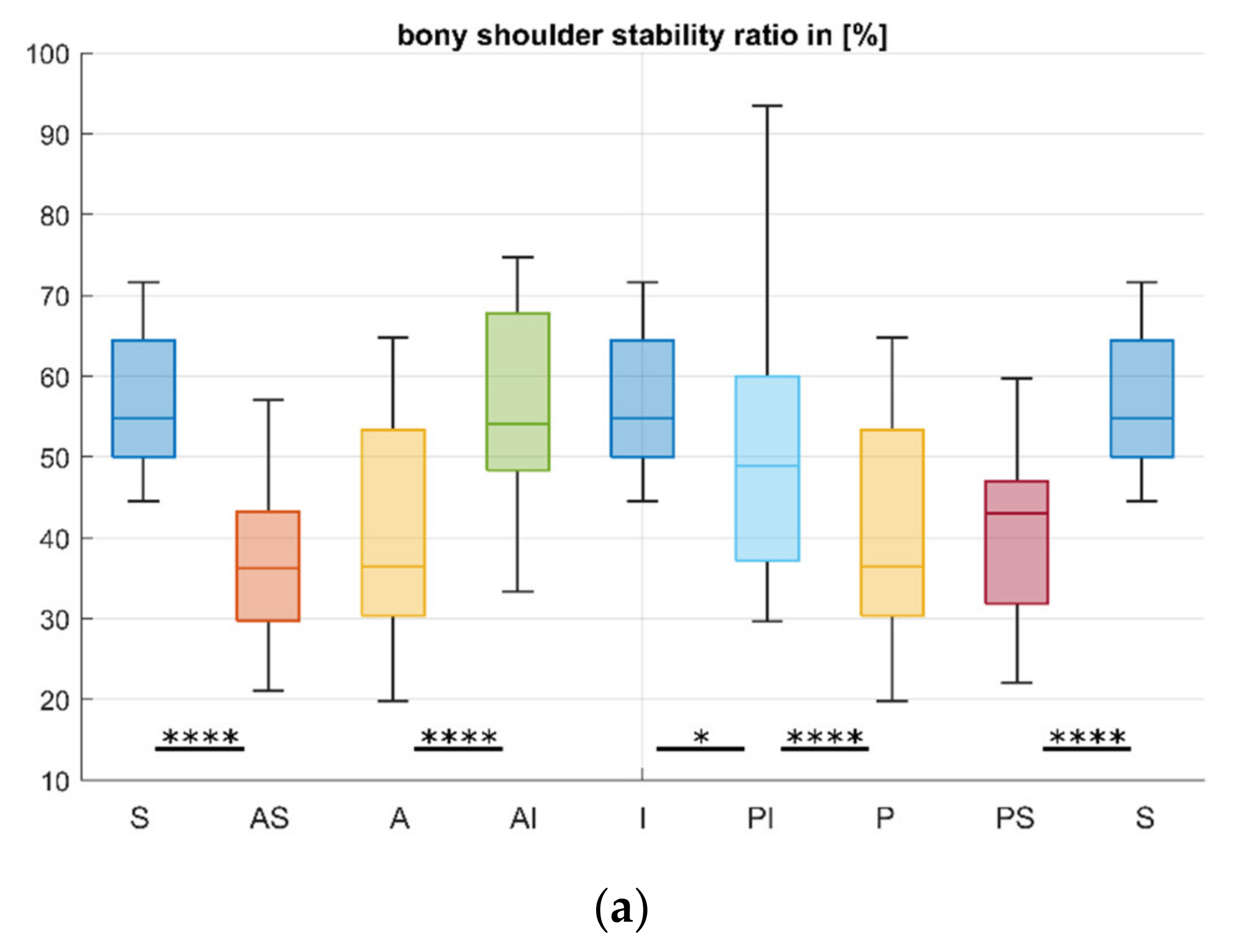
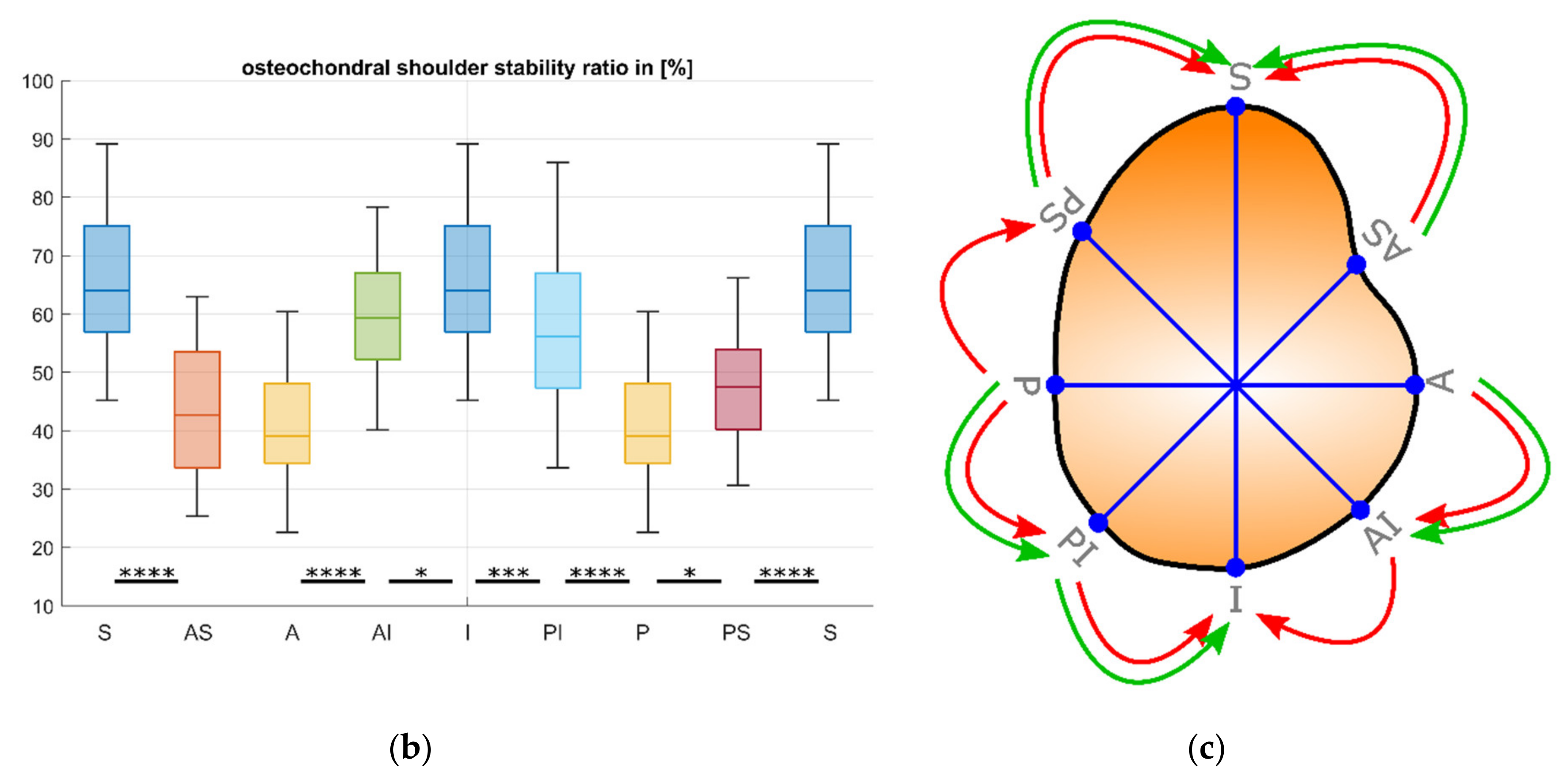
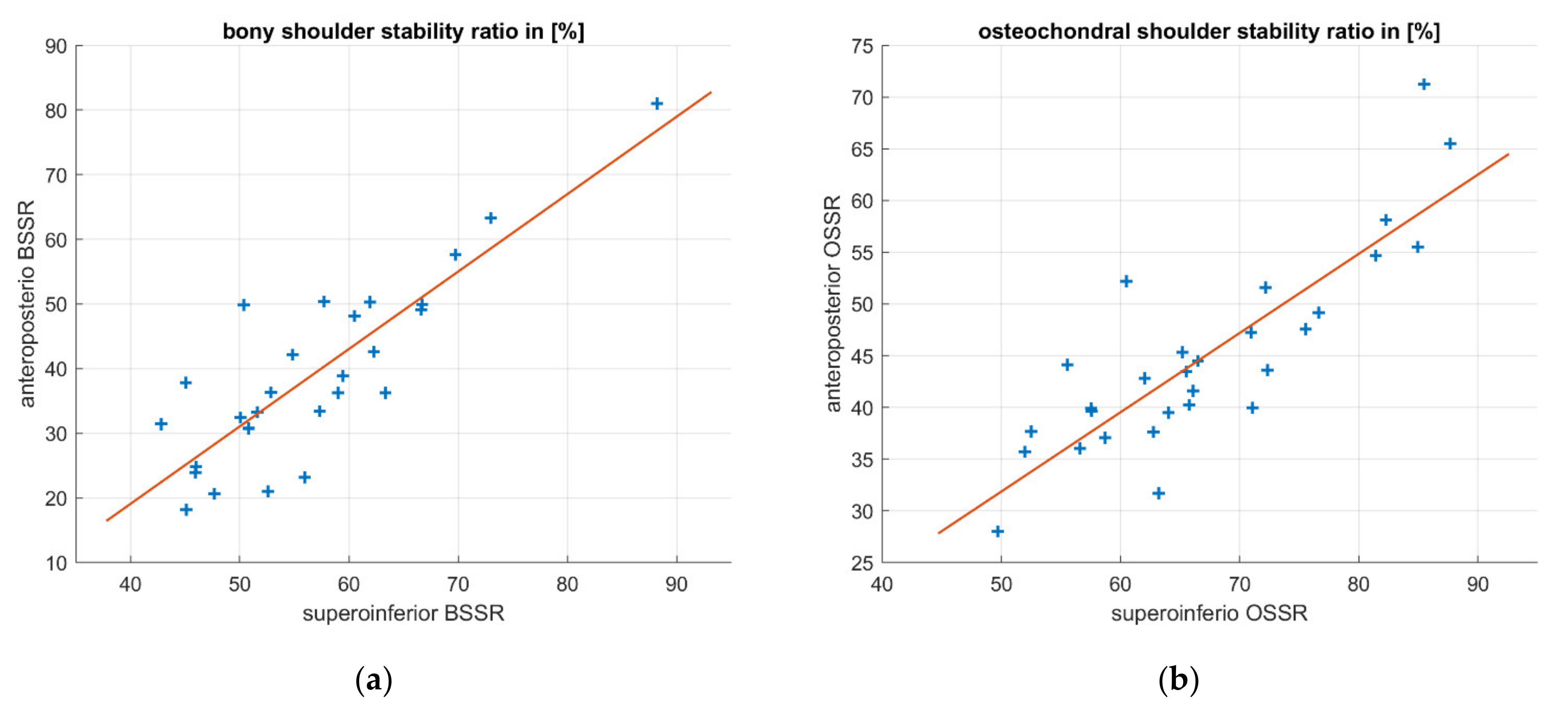
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Schleich, C.; Bittersohl, B.; Antoch, G.; Krauspe, R.; Zilkens, C.; Kircher, J. Thickness Distribution of Glenohumeral Joint Cartilage: A Normal Value Study on Asymptomatic Volunteers Using 3-Tesla Magnetic Resonance Tomography. Cartilage 2017, 8, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Soslowsky, L.J.; Flatow, E.L.; Bigliani, L.U.; Mow, V.C. Articular geometry of the glenohumeral joint. Clin. Orthop. Relat. Res. 1992, 285, 181–190. [Google Scholar] [CrossRef]
- Lippitt, S.; Matsen, F. Mechanisms of Glenohumeral Joint Stability. Clin. Orthop. Relat. Res. 1993, 20–28. [Google Scholar] [CrossRef]
- Wermers, J.; Schliemann, B.; Raschke, M.J.; Michel, P.A.; Heilmann, L.F.; Dyrna, F.; Sußiek, J.; Frank, A.; Katthagen, J.C. Glenoid concavity has a higher impact on shoulder stability than the size of a bony defect. Knee Surg. Sports Traumatol. Arthrosc. 2021. [Google Scholar] [CrossRef] [PubMed]
- Moroder, P.; Damm, P.; Wierer, G.; Böhm, E.; Minkus, M.; Plachel, F.; Märdian, S.; Scheibel, M.; Khatamirad, M. Challenging the Current Concept of Critical Glenoid Bone Loss in Shoulder Instability: Does the Size Measurement Really Tell It All? Am. J. Sports Med. 2019, 47, 688–694. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, M.D.; Sidles, J.A.; Harryman, D.T.; Matsen, F.A. Effect of a Chondral-Labral Defect on Glenoid Concavity and Glenohumeral Stability. A Cadaveric Model. J. Bone Jt. Surg. 1996, 78, 94–102. [Google Scholar] [CrossRef]
- Braman, J.P.; Falicov, A.; Boorman, R.; Matsen, F.A. Alterations in surface geometry in retrieved polyethylene glenoid component. J. Orthop. Res. 2006, 24, 1249–1260. [Google Scholar] [CrossRef]
- Matsen, F.A.; Chebli, C.; Lippitt, S. Principles for the evaluation and management of shoulder instability. J. Bone Jt. Surg. 2006, 88, 648–659. [Google Scholar] [CrossRef]
- Montgomery, W.H.; Wahl, M.; Hettrich, C.; Itoi, E.; Lippitt, S.B.; Matsen, F.A. Anteroinferior bone-grafting can restore stability in osseous glenoid defects. J. Bone Jt. Surg. 2005, 87, 1972–1977. [Google Scholar] [CrossRef]
- Weldon, E.J.; Boorman, R.S.; Smith, K.L.; Matsen, F.A. Optimizing the glenoid contribution to the stability of a humeral hemiarthroplasty without a prosthetic glenoid. J. Bone Jt. Surg.Ser. A 2004, 86, 2022–2029. [Google Scholar] [CrossRef]
- Moroder, P.; Ernstbrunner, L.; Pomwenger, W.; Oberhauser, F.; Hitzl, W.; Tauber, M.; Resch, H.; Moroder, R. Anterior shoulder instability is associated with an underlying deficiency of the bony glenoid concavity. Arthrosc. J. Arthrosc. Relat. Surg. 2015, 31, 1223–1231. [Google Scholar] [CrossRef]
- Halder, A.M.; Kuhl, S.G.; Zobitz, M.E.; Larson, D.; An, K.N. Effects of the Glenoid Labrum and Glenohumeral Abduction on Stability of the Shoulder Joint Through Concavity-Compression. J. Bone Jt. Surg. 2001, 83, 1062–1069. [Google Scholar] [CrossRef]
- Yamamoto, N.; Itoi, E.; Abe, H.; Kikuchi, K.; Seki, N.; Minagawa, H.; Tuoheti, Y. Effect of an anterior glenoid defect on anterior shoulder stability. Am. J. Sports Med. 2009, 37, 949–954. [Google Scholar] [CrossRef]
- Klemt, C.; Nolte, D.; Grigoriadis, G.; Di Federico, E.; Reilly, P.; Bull, A.M.J. The contribution of the glenoid labrum to glenohumeral stability under physiological joint loading using finite element analysis. Comput. Methods Biomech. Biomed. Eng. 2017, 20, 1613–1622. [Google Scholar] [CrossRef]
- Klemt, C.; Toderita, D.; Nolte, D.; Di Federico, E.; Reilly, P.; Bull, A.M.J. The critical size of a defect in the glenoid causing anterior instability of the shoulder after a Bankart repair, under physiological joint loading. Bone Jt. J. 2019, 101, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Lippitt, S.B.; Vanderhooft, J.E.; Harris, S.L.; Sidles, J.A.; Harryman, D.T.; Matsen, F.A. Glenohumeral stability from concavity-compression: A quantitative analysis. J. Shoulder Elb. Surg. 1993, 2, 27–35. [Google Scholar] [CrossRef]
- Gottschalk, L.J.; Walia, P.; Patel, R.M.; Kuklis, M.; Jones, M.H.; Fening, S.D.; Miniaci, A. Stability of the Glenohumeral Joint With Combined Humeral Head and Glenoid Defects. Am. J. Sports Med. 2016, 44, 933–940. [Google Scholar] [CrossRef] [PubMed]
- Haas, M.; Plachel, F.; Wierer, G.; Heuberer, P.; Hoffelner, T.; Schulz, E.; Anderl, W.; Moroder, P. Glenoid morphology is associated with the development of instability arthropathy. J. Shoulder Elb. Surg. 2019, 28, 893–899. [Google Scholar] [CrossRef] [PubMed]
- Jun, B.J.; Iannotti, J.P.; McGarry, M.H.; Yoo, J.C.; Quigley, R.J.; Lee, T.Q. The effects of prosthetic humeral head shape onglenohumeral joint kinematics: A comparison of non-spherical and spherical prosthetic heads to the native humeral head. J. Shoulder Elb. Surg. 2013, 22, 1423–1432. [Google Scholar] [CrossRef]
- Hertel, R.; Knothe, U.; Ballmer, F.T. Geometry of the proximal humerus and implications for prosthetic design. J. Shoulder Elb. Surg. 2002, 11, 331–338. [Google Scholar] [CrossRef]
- Bockmann, B.; Venjakob, A.J.; Reichwein, F.; Hagenacker, M.; Nebelung, W. Mapping of glenoid bone loss in recurrent anterior shoulder instability: Is there a particular deficit pattern? J. Shoulder Elb. Surg. 2017, 26, 1676–1680. [Google Scholar] [CrossRef] [PubMed]
- Saito, H.; Itoi, E.; Sugaya, H.; Minagawa, H.; Yamamoto, N.; Tuoheti, Y. Location of the glenoid defect in shoulders with recurrent anterior dislocation. Am. J. Sports Med. 2005, 33, 889–893. [Google Scholar] [CrossRef]
- Aigner, F.; Longato, S.; Fritsch, H.; Kralinger, F. Anatomical considerations regarding the “bare spot” of the glenoid cavity. Surg. Radiol. Anat. 2004, 26, 308–311. [Google Scholar] [CrossRef] [PubMed]
- Giles, J.W.; Owens, B.D.; Athwal, G.S. Estimating glenoid width for instability-related bone loss: A CT evaluation of an MRI formula. Am. J. Sports Med. 2015, 43, 1726–1730. [Google Scholar] [CrossRef] [PubMed]
- Owens, B.D.; Burns, T.C.; Campbell, S.E.; Svoboda, S.J.; Cameron, K.L. Simple method of glenoid bone loss calculation using ipsilateral magnetic resonance imaging. Am. J. Sports Med. 2013, 41, 622–624. [Google Scholar] [CrossRef] [PubMed]


| Method | Directions | Measurements | Outcome Parameter |
|---|---|---|---|
| CT scan | Anterosuperior (AS) | Depth (d) | BSSR |
| Measuring arm | Anterior/posterior (A/P) | Sphere radius (rs) | OSSR |
| Anteroinferior (AI) | Circle radius (rc) | ||
| Superior/inferior (S/I) | |||
| Posteroinferior (PI) | |||
| Posterosuperior (PS) |
| Direction | BSSR in [%] | OSSR in [%] |
|---|---|---|
| Anterosuperior (AS) | 37.1 ± 15.0 | 42.9 ± 11.1 |
| Anterior/posterior (A/P) | 40.6 ± 16.2 | 41.0 ± 11.0 |
| Anteroinferior (AI) | 56.6 ± 16.3 | 61.1 ± 13.1 |
| Superior/inferior (S/I) | 57.0 ± 10.3 | 65.9 ± 11.9 |
| Posteroinferior (PI) | 51.0 ± 15.9 | 57.7 ± 14.1 |
| Posterosuperior (PS) | 42.4 ± 13.2 | 47.4 ± 10.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wermers, J.; Raschke, M.J.; Wilken, M.; Riegel, A.; Katthagen, J.C. The Anatomy of Glenoid Concavity—Bony and Osteochondral Assessment of a Stability-Related Parameter. J. Clin. Med. 2021, 10, 4316. https://doi.org/10.3390/jcm10194316
Wermers J, Raschke MJ, Wilken M, Riegel A, Katthagen JC. The Anatomy of Glenoid Concavity—Bony and Osteochondral Assessment of a Stability-Related Parameter. Journal of Clinical Medicine. 2021; 10(19):4316. https://doi.org/10.3390/jcm10194316
Chicago/Turabian StyleWermers, Jens, Michael J. Raschke, Marcel Wilken, Arne Riegel, and J. Christoph Katthagen. 2021. "The Anatomy of Glenoid Concavity—Bony and Osteochondral Assessment of a Stability-Related Parameter" Journal of Clinical Medicine 10, no. 19: 4316. https://doi.org/10.3390/jcm10194316






