Thyroid Cancer Risk Factors in Children with Thyroid Nodules: A One-Center Study
Abstract
:1. Introduction
1.1. Thyroid Cancer Risk Factors
1.2. Molecular Aspects of Thyroid Cancer
1.3. Physical Examination
1.4. Diagnostics
1.4.1. The Thyroid Gland in Ultrasound Images
1.4.2. Hormonal and Immunological Diagnostics
1.5. FNAB Results and the Choice of Further Treatment
1.5.1. Histopathological Diagnosis and Further Management
Benign Thyroid Nodule
Malignant or Suspicious Lesions
1.5.2. Assessment with TBSRTC and Further Treatment
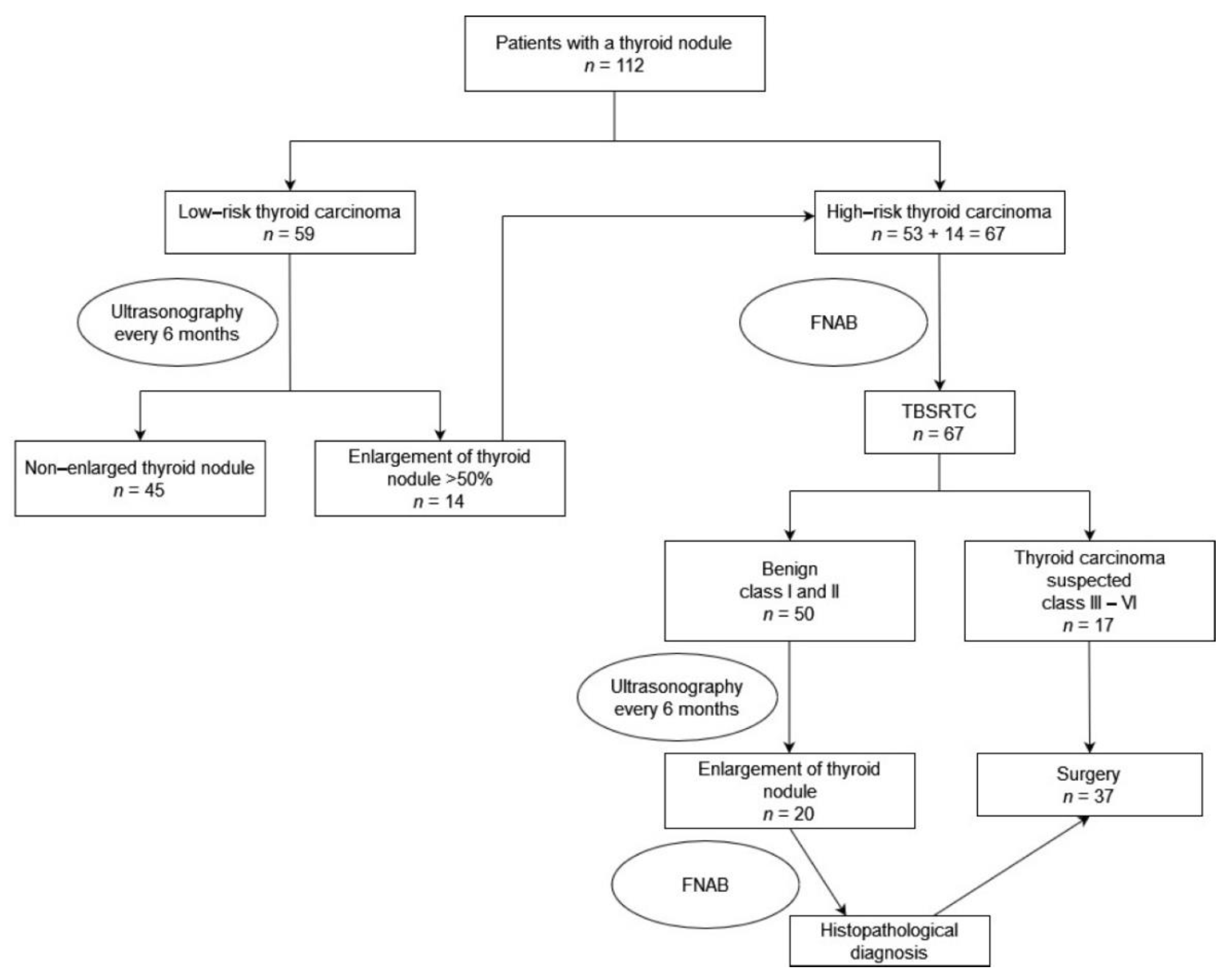
2. Patients, Materials and Methods
Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Suh, J.; Choi, H.S.; Kwon, A.; Chae, H.W.; Kim, H.-S. Adolescents with thyroid nodules: Retrospective analysis of factors predicting malignancy. Eur. J. Pediatr. 2020, 179, 317–325. [Google Scholar] [CrossRef]
- Iakovou, I.; Giannoula, E.; Sachpekidis, C. Imaging and Imaging-Based Management of Pediatric Thyroid Nodules. J. Clin. Med. 2020, 9, 384. [Google Scholar] [CrossRef] [Green Version]
- Al Nofal, A.; Gionfriddo, M.R.; Javed, A.; Haydour, Q.; Brito, J.P.; Prokop, L.J.; Pittock, S.T.; Murad, M.H. Accuracy of thyroid nodule sonography for the detection of thyroid cancer in children: Systematic review and meta-analysis. Clin. Endocrinol. 2016, 84, 423–430. [Google Scholar] [CrossRef]
- Bauer, A.J. Pediatric Thyroid Cancer: Genetics, Therapeutics and Outcome. Endocrinol. Metab. Clin. N. Am. 2020, 49, 589–611. [Google Scholar] [CrossRef]
- Francis, G.L.; Waguespack, S.G.; Bauer, A.J.; Angelos, P.; Benvenga, S.; Cerutti, J.M.; Dinauer, C.A.; Hamilton, J.; Hay, I.D.; Luster, M.; et al. Management Guidelines for Children with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2015, 25, 716–759. [Google Scholar] [CrossRef] [Green Version]
- Paulson, V.A.; Rudzinski, E.R.; Hawkins, D.S. Thyroid Cancer in the Pediatric Population. Genes 2019, 10, 723. [Google Scholar] [CrossRef] [Green Version]
- Drozd, V.; Saenko, V.; Branovan, D.I.; Brown, K.; Yamashita, S.; Reiners, C. A Search for Causes of Rising Incidence of Differentiated Thyroid Cancer in Children and Adolescents after Chernobyl and Fukushima: Comparison of the Clinical Features and Their Relevance for Treatment and Prognosis. Int. J. Environ. Res. Public Health 2021, 18, 3444. [Google Scholar] [CrossRef]
- Cooper, D.S.; Doherty, G.M.; Haugen, B.R.; Hauger, B.R.; Kloos, R.T.; Lee, S.L.; Mandel, S.J.; Mazzaferri, E.L.; McIver, B.; Pacini, F.; et al. Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 2009, 19, 1167–1214. [Google Scholar] [CrossRef] [Green Version]
- Stack, B.C.; Twining, C.; Rastatter, J.; Angelos, P.; Baloch, Z.; Diercks, G.; Faquin, W.; Kazahaya, K.; Rivkees, S.; Sheyn, T.; et al. Consensus statement by the American Association of Clinical Endocrinology (AACE) and the American Head and Neck Society Endocrine Surgery Section (AHNS-ES) on Pediatric Benign and Malignant Thyroid Surgery. Head Neck 2021, 43, 1027–1042. [Google Scholar] [CrossRef]
- Szmit-Domagalska, J.; Horodnicka-Józwa, A.; Petriczko, E.; Biczysko-Mokosa, A.; Marcinkiewicz, K.; Walczak, M. Rak brodawkowaty tarczycy u trójki dzieci. Pediatr. Endocrinol. Diabetes Metab. 2019, 25, 202–207. [Google Scholar] [CrossRef]
- Skubisz, K.; Januszkiewicz-Caulier, J.; Cybula, P.; Bakuła-Zalewska, E.; Goryca, K.; Paziewska, A.; Ambrożkiewicz, F.; Woliński, K.; Mikula, M.; Ostrowski, J.; et al. Higher EU-TIRADS-Score Correlated with BRAF V600E Positivity in the Early Stage of Papillary Thyroid Carcinoma. J. Clin. Med. 2021, 10, 2304. [Google Scholar] [CrossRef]
- Abdullah, M.I.; Junit, S.M.; Ng, K.L.; Jayapalan, J.J.; Karikalan, B.; Hashim, O.H. Papillary Thyroid Cancer: Genetic Alterations and Molecular Biomarker Investigations. Int. J. Med. Sci. 2019, 16, 450–460. [Google Scholar] [CrossRef] [Green Version]
- Tirrò, E.; Martorana, F.; Romano, C.; Vitale, S.R.; Motta, G.; Di Gregorio, S.; Massimino, M.; Pennisi, M.S.; Stella, S.; Puma, A.; et al. Molecular Alterations in Thyroid Cancer: From Bench to Clinical Practice. Genes 2019, 10, 709. [Google Scholar] [CrossRef] [Green Version]
- Song, Y.S.; Park, Y.J. Genomic Characterization of Differentiated Thyroid Carcinoma. Endocrinol. Metab. 2019, 34, 1–10. [Google Scholar] [CrossRef]
- Prete, A.; Borges de Souza, P.; Censi, S.; Muzza, M.; Nucci, N.; Sponziello, M. Update on Fundamental Mechanisms of Thyroid Cancer. Front. Endocrinol. 2020, 11, 102. [Google Scholar] [CrossRef]
- Rangel-Pozzo, A.; Sisdelli, L.; Cordioli, M.I.V.; Vaisman, F.; Caria, P.; Mai, S.; Cerutti, J.M. Genetic Landscape of Papillary Thyroid Carcinoma and Nuclear Architecture: An Overview Comparing Pediatric and Adult Populations. Cancers 2020, 12, 3146. [Google Scholar] [CrossRef]
- Mitsutake, N.; Saenko, V. Molecular pathogenesis of pediatric thyroid carcinoma. J. Radiat. Res. 2021, 62, i71–i77. [Google Scholar] [CrossRef]
- Accardo, G.; Conzo, G.; Esposito, D.; Gambardella, C.; Mazzella, M.; Castaldo, F.; Di Donna, C.; Polistena, A.; Avenia, N.; Colantuoni, V.; et al. Genetics of medullary thyroid cancer: An overview. Int. J. Surg. 2017, 41 (Suppl. 1), S2–S6. [Google Scholar] [CrossRef]
- Corrias, A.; Mussa, A. Thyroid nodules in pediatrics: Which ones can be left alone, which ones must be investigated, when and how. J. Clin. Res. Pediatr. Endocrinol. 2013, 5 (Suppl. 1), 57–69. [Google Scholar] [CrossRef]
- Guille, J.T.; Opoku-Boateng, A.; Thibeault, S.L.; Chen, H. Evaluation and management of the pediatric thyroid nodule. Oncologist 2015, 20, 19–27. [Google Scholar] [CrossRef] [Green Version]
- Sohn, Y.-M.; Kwak, J.Y.; Kim, E.-K.; Moon, H.J.; Kim, S.J.; Kim, M.J. Diagnostic approach for evaluation of lymph node metastasis from thyroid cancer using ultrasound and fine-needle aspiration biopsy. AJR Am. J. Roentgenol. 2010, 194, 38–43. [Google Scholar] [CrossRef]
- Koltin, D.; O’Gorman, C.S.; Murphy, A.; Ngan, B.; Daneman, A.; Navarro, O.M.; García, C.; Atenafu, E.G.; Wasserman, J.D.; Hamilton, J.; et al. Pediatric thyroid nodules: Ultrasonographic characteristics and inter-observer variability in prediction of malignancy. J. Pediatr. Endocrinol. Metab. 2016, 29, 789–794. [Google Scholar] [CrossRef]
- Anil, G.; Hegde, A.; Chong, F.H.V. Thyroid nodules: Risk stratification for malignancy with ultrasound and guided biopsy. Cancer Imaging 2011, 11, 209–223. [Google Scholar] [CrossRef]
- Richman, D.M.; Benson, C.B.; Doubilet, P.M.; Peters, H.E.; Huang, S.A.; Asch, E.; Wassner, A.J.; Smith, J.R.; Cherella, C.E.; Frates, M.C. Thyroid Nodules in Pediatric Patients: Sonographic Characteristics and Likelihood of Cancer. Radiology 2018, 288, 591–599. [Google Scholar] [CrossRef] [Green Version]
- Mussa, A.; de Andrea, M.; Motta, M.; Mormile, A.; Palestini, N.; Corrias, A. Predictors of Malignancy in Children with Thyroid Nodules. J. Pediatr. 2015, 167, 886–892.e1. [Google Scholar] [CrossRef]
- Russ, G.; Bonnema, S.J.; Erdogan, M.F.; Durante, C.; Ngu, R.; Leenhardt, L. European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: The EU-TIRADS. Eur. Thyroid J. 2017, 6, 225–237. [Google Scholar] [CrossRef] [Green Version]
- Gupta, A.; Ly, S.; Castroneves, L.A.; Frates, M.C.; Benson, C.B.; Feldman, H.A.; Wassner, A.J.; Smith, J.R.; Marqusee, E.; Alexander, E.K.; et al. A standardized assessment of thyroid nodules in children confirms higher cancer prevalence than in adults. J. Clin. Endocrinol. Metab. 2013, 98, 3238–3245. [Google Scholar] [CrossRef] [Green Version]
- Bossowski, A. Diagnostyka i Leczenie Chorób Tarczycy Dzieci i Młodzieży; Medical Tribune Polska: Warszawa, Poland, 2020; ISBN 9788395667763. [Google Scholar]
- Jarząb, B.; Dedecjus, M.; Słowińska-Klencka, D.; Lewiński, A.; Adamczewski, Z.; Anielski, R.; Bagłaj, M.; Bałdys-Waligórska, A.; Barczyński, M.; Bednarczuk, T.; et al. Guidelines of Polish National Societies Diagnostics and Treatment of Thyroid Carcinoma. 2018 Update. Endokrynol. Pol. 2018, 69, 34–74. [Google Scholar] [CrossRef]
- Niedziela, M. Thyroid nodules. Best Pract. Res. Clin. Endocrinol. Metab. 2014, 28, 245–277. [Google Scholar] [CrossRef]
- Wells, S.A.; Asa, S.L.; Dralle, H.; Elisei, R.; Evans, D.B.; Gagel, R.F.; Lee, N.; Machens, A.; Moley, J.F.; Pacini, F.; et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid 2015, 25, 567–610. [Google Scholar] [CrossRef]
- Heider, A.; Arnold, S.; Jing, X. Bethesda System for Reporting Thyroid Cytopathology in Pediatric Thyroid Nodules: Experience of a Tertiary Care Referral Center. Arch. Pathol. Lab. Med. 2020, 144, 473–477. [Google Scholar] [CrossRef] [Green Version]
- Cibas, E.S.; Ali, S.Z. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017, 27, 1341–1346. [Google Scholar] [CrossRef]
- Tessler, F.N.; Middleton, W.D.; Grant, E.G.; Hoang, J.K.; Berland, L.L.; Teefey, S.A.; Cronan, J.J.; Beland, M.D.; Desser, T.S.; Frates, M.C.; et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J. Am. Coll. Radiol. 2017, 14, 587–595. [Google Scholar] [CrossRef] [Green Version]
- Weller, A.; Sharif, B.; Qarib, M.H.; St Leger, D.; de Silva, H.S.; Lingam, R.K. British Thyroid Association 2014 classification ultrasound scoring of thyroid nodules in predicting malignancy: Diagnostic performance and inter-observer agreement. Ultrasound 2020, 28, 4–13. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [Green Version]
- Lim-Dunham, J.E. Ultrasound guidelines for pediatric thyroid nodules: Proceeding with caution. Pediatr. Radiol. 2019, 49, 851–853. [Google Scholar] [CrossRef] [Green Version]
- Richman, D.M.; Benson, C.B.; Doubilet, P.M.; Wassner, A.J.; Asch, E.; Cherella, C.E.; Smith, J.R.; Frates, M.C. Assessment of American College of Radiology Thyroid Imaging Reporting and Data System (TI-RADS) for Pediatric Thyroid Nodules. Radiology 2020, 294, 415–420. [Google Scholar] [CrossRef]
- Polat, Y.D.; Öztürk, V.S.; Ersoz, N.; Anık, A.; Karaman, C.Z. Is Thyroid Imaging Reporting and Data System Useful as an Adult Ultrasonographic Malignancy Risk Stratification Method ın Pediatric Thyroid Nodules? J. Med. Ultrasound 2019, 27, 141–145. [Google Scholar] [CrossRef]
- Martinez-Rios, C.; Daneman, A.; Bajno, L.; van der Kaay, D.C.M.; Moineddin, R.; Wasserman, J.D. Utility of adult-based ultrasound malignancy risk stratifications in pediatric thyroid nodules. Pediatr. Radiol. 2018, 48, 74–84. [Google Scholar] [CrossRef]
- Creo, A.; Alahdab, F.; Al Nofal, A.; Thomas, K.; Kolbe, A.; Pittock, S.T. Ultrasonography and the American Thyroid Association Ultrasound-Based Risk Stratification Tool: Utility in Pediatric and Adolescent Thyroid Nodules. Horm. Res. Paediatr. 2018, 90, 93–101. [Google Scholar] [CrossRef]
- Gannon, A.W.; Langer, J.E.; Bellah, R.; Ratcliffe, S.; Pizza, J.; Mostoufi-Moab, S.; Cappola, A.R.; Bauer, A.J. Diagnostic Accuracy of Ultrasound With Color Flow Doppler in Children With Thyroid Nodules. J. Clin. Endocrinol. Metab. 2018, 103, 1958–1965. [Google Scholar] [CrossRef]
- Lyshchik, A.; Drozd, V.; Demidchik, Y.; Reiners, C. Diagnosis of thyroid cancer in children: Value of gray-scale and power doppler US. Radiology 2005, 235, 604–613. [Google Scholar] [CrossRef]
- Lingam, R.K.; Qarib, M.H.; Tolley, N.S. Evaluating thyroid nodules: Predicting and selecting malignant nodules for fine-needle aspiration (FNA) cytology. Insights Imaging 2013, 4, 617–624. [Google Scholar] [CrossRef] [Green Version]
- Essenmacher, A.C.; Joyce, P.H.; Kao, S.C.; Epelman, M.; Pesce, L.M.; D’Alessandro, M.P.; Sato, Y.; Johnson, C.M.; Podberesky, D.J. Sonographic Evaluation of Pediatric Thyroid Nodules. Radiographics 2017, 37, 1731–1752. [Google Scholar] [CrossRef]
- Borysewicz-Sanczyk, H.; Dzieciol, J.; Sawicka, B.; Bossowski, A. Practical Application of Elastography in the Diagnosis of Thyroid Nodules in Children and Adolescents. Horm. Res. Paediatr. 2016, 86, 39–44. [Google Scholar] [CrossRef]
- Cunha, G.B.; Marino, L.C.I.; Yamaya, A.; Kochi, C.; Monte, O.; Longui, C.A.; Cury, A.N.; Fleury, E.D.F.C. Elastography for the evaluation of thyroid nodules in pediatric patients. Radiol. Bras. 2019, 52, 141–147. [Google Scholar] [CrossRef]
- Ahmad, H.; Al-Hadidi, A.; Bobbey, A.; Shah, S.; Stanek, J.; Nicol, K.; Hoffman, R.P.; Aldrink, J.H. Pediatric adaptions are needed to improve the diagnostic accuracy of thyroid ultrasound using TI-RADS. J. Pediatr. Surg. 2021, 56, 1120–1125. [Google Scholar] [CrossRef]
- Kaliszewski, K.; Diakowska, D.; Wojtczak, B.; Sutkowski, K.; Knychalski, B.; Forkasiewicz, Z. Patients with III and IV category of the Bethesda System under levothyroxine non-suppressive therapy have a lower rate of thyroid malignancy. Sci. Rep. 2019, 9, 8409. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Y.; Song, Y.; Xu, G.; Fan, Z.; Ren, W. The Bethesda System for Reporting Thyroid Cytopathology (TBSRTC): A report of 2781 cases in a Chinese population. Chin. J. Cancer Res. 2020, 32, 140–148. [Google Scholar] [CrossRef]
- Sauter, J.L.; Lehrke, H.; Zhang, X.; Al Badri, O.T.; Rodriguez-Gutierrez, R.; Delivanis, D.A.; Singh Ospina, N.; Donegan, D.; Hamidi, O.; Iñiguez-Ariza, N.; et al. Assessment of The Bethesda System for Reporting Thyroid Cytopathology. Am. J. Clin. Pathol. 2019, 152, 502–511. [Google Scholar] [CrossRef] [Green Version]
- Yaprak Bayrak, B.; Eruyar, A.T. Malignancy rates for Bethesda III and IV thyroid nodules: A retrospective study of the correlation between fine-needle aspiration cytology and histopathology. BMC Endocr. Disord. 2020, 20, 48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alshaikh, S.; Harb, Z.; Aljufairi, E.; Almahari, S.A. Classification of thyroid fine-needle aspiration cytology into Bethesda categories: An institutional experience and review of the literature. Cytojournal 2018, 15, 4. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Mehrad, M.; Ely, K.A.; Liang, J.; Solórzano, C.C.; Neblett, W.W.; Coogan, A.C.; Weiss, V.L. Incidence and malignancy rates of indeterminate pediatric thyroid nodules. Cancer Cytopathol. 2019, 127, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Karagiannis, A.; Kassi, E.; Chatzigeorgiou, A.; Koutsilieris, M. IGF Bioregulation System in Benign and Malignant Thyroid Nodular Disease: A Systematic Review. In Vivo 2020, 34, 3069–3091. [Google Scholar] [CrossRef] [PubMed]







| Clinical Features of Increased Risk of Malignancy | Ultrasonographic Features of Increased Risk of Malignancy |
|---|---|
| Lymph node metastasis or distant metastasis | Features indicating the possibility of metastasis of thyroid cancer to cervical lymph node microcalcifications, lithocystic character, hyperechogenicity, round shape, transverse dimension > 5 mm, lack of an echogenic fatty cavity, marginal or chaotic vascularization of lymph nodes |
| History of neck exposure to ionizing radiation | Features of infiltration of the thyroid capsule with or without infiltration of the surrounding organs |
| History of familial thyroid cancer (for medullary thyroid cancer) | Presence of microcalcifications in the focal lesion of the thyroid gland |
| Rapid growth of the nodule | Hypoechoic nature of a focal lesion |
| Hard nodule, attached to the surroundings | Shape of the focal lesion (longer than the width) |
| Diameter of the nodule > 4 cm | Diffuse margins |
| Appearance of a thyroid nodule before the age of 20 or after the age of 60 years | Features of increased, chaotic vascular flow centrally in the lesion |
| Paralysis of the laryngeal nerves, especially one-sided | Solid character of a focal lesion |
| Nodule Dimensions | Patients without Thyroid Cancer Mean ± SD | Patients with Thyroid Cancer Mean ± SD | p |
|---|---|---|---|
| Length (mm) | 13.7 ± 10.5 | 17.6 ± 10.1 | 0.090 |
| Height (mm) | 9.9 ± 8.3 | 14.1 ± 8.0 | 0.018 |
| Width (mm) | 15.1 ± 12.4 | 19.0 ± 14.8 | 0.296 |
| Volume (mm3) | 4.7 ± 6.5 | 3.5 ± 6.5 | 0.146 |
| TBSRTC | AITD (Hashimoto or Graves’ Disease) | Multinodular Goiter | Benign Follicular Nodule or Adenoma | Papillary Carcinoma | Follicular Carcinoma | Poorly Differentiated Thyroid Carcinoma |
|---|---|---|---|---|---|---|
| I | 0 | 0 | 0 | 0 | 0 | 0 |
| II | 0 | 1 | 13 | 2 | 0 | 0 |
| III | 2 | 2 | 1 | 4 | 0 | 0 |
| IV | 0 | 0 | 2 | 1 | 0 | 0 |
| V | 0 | 0 | 0 | 1 | 3 | 0 |
| VI | 0 | 0 | 0 | 0 | 0 | 1 |
| TBSRTC Class | Number of Cancer Diagnoses of the Number of Biopsies Performed | Percentage of Children Diagnosed with Cancer (%) |
|---|---|---|
| I | 0 out of 3 | 0 |
| II | 2 out of 47 | 4 |
| III | 4 out of 9 | 44 |
| IV | 1 out of 3 | 33 |
| V | 4 out of 4 | 100 |
| VI | 1 out of 1 | 100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ben-Skowronek, I.; Sieniawska, J.; Pach, E.; Wrobel, W.; Skowronek, A.; Tomczyk, Z.; Mlodawska, A.; Makuch, M.; Malka, M.; Cielecki, C.; et al. Thyroid Cancer Risk Factors in Children with Thyroid Nodules: A One-Center Study. J. Clin. Med. 2021, 10, 4455. https://doi.org/10.3390/jcm10194455
Ben-Skowronek I, Sieniawska J, Pach E, Wrobel W, Skowronek A, Tomczyk Z, Mlodawska A, Makuch M, Malka M, Cielecki C, et al. Thyroid Cancer Risk Factors in Children with Thyroid Nodules: A One-Center Study. Journal of Clinical Medicine. 2021; 10(19):4455. https://doi.org/10.3390/jcm10194455
Chicago/Turabian StyleBen-Skowronek, Iwona, Joanna Sieniawska, Emilia Pach, Wiktoria Wrobel, Anna Skowronek, Zaklina Tomczyk, Anna Mlodawska, Magdalena Makuch, Magdalena Malka, Czeslaw Cielecki, and et al. 2021. "Thyroid Cancer Risk Factors in Children with Thyroid Nodules: A One-Center Study" Journal of Clinical Medicine 10, no. 19: 4455. https://doi.org/10.3390/jcm10194455
APA StyleBen-Skowronek, I., Sieniawska, J., Pach, E., Wrobel, W., Skowronek, A., Tomczyk, Z., Mlodawska, A., Makuch, M., Malka, M., Cielecki, C., & Nachulewicz, P. (2021). Thyroid Cancer Risk Factors in Children with Thyroid Nodules: A One-Center Study. Journal of Clinical Medicine, 10(19), 4455. https://doi.org/10.3390/jcm10194455






