Patient–Ventilator Dyssynchrony in Critically Ill Patients
Abstract
:1. Introduction
1.1. What Is Patient–Ventilator Dyssynchrony?
1.2. Why Should We Care about Patient–Ventilator Dyssynchrony?
2. Classification of Patient–Ventilator Dyssynchrony
3. Dyssynchrony by Respiratory Phases
3.1. Dyssynchrony of the Trigger Phase
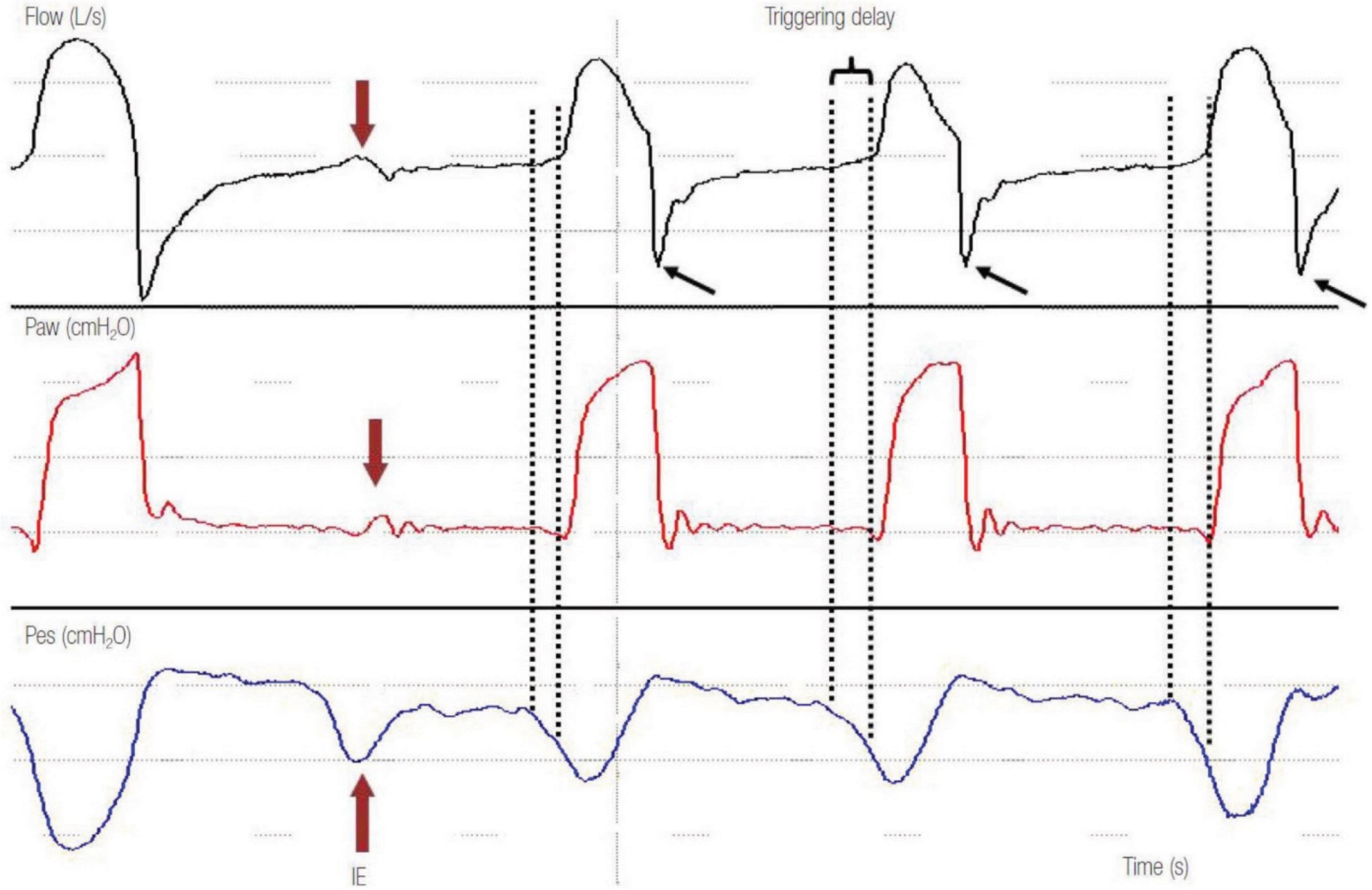
3.1.1. Delayed Triggering and Ineffective Efforts
3.1.2. Autotriggering
3.2. Dyssynchrony of the Flow Phase
3.3. Dyssynchrony of the Cycling Phase
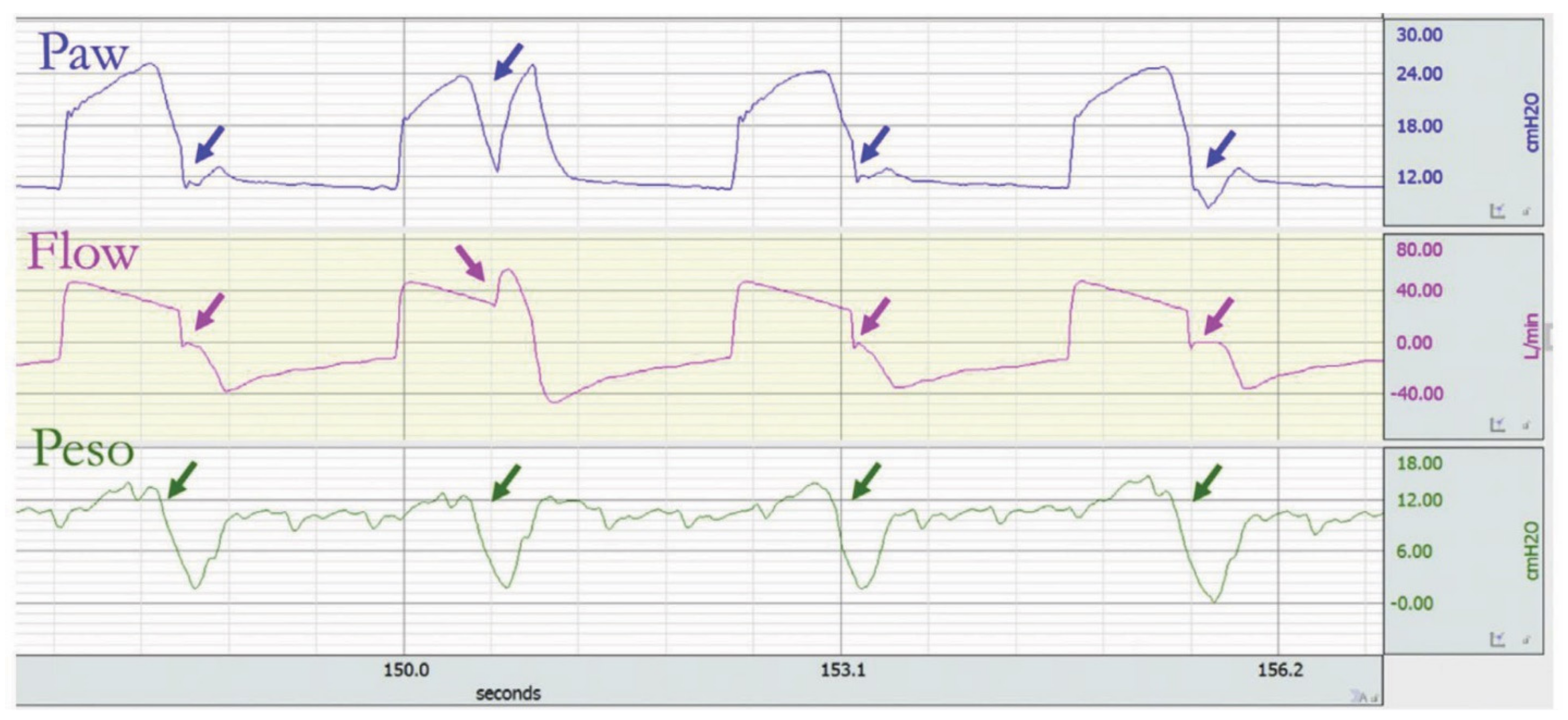
3.3.1. Premature Cycling Off
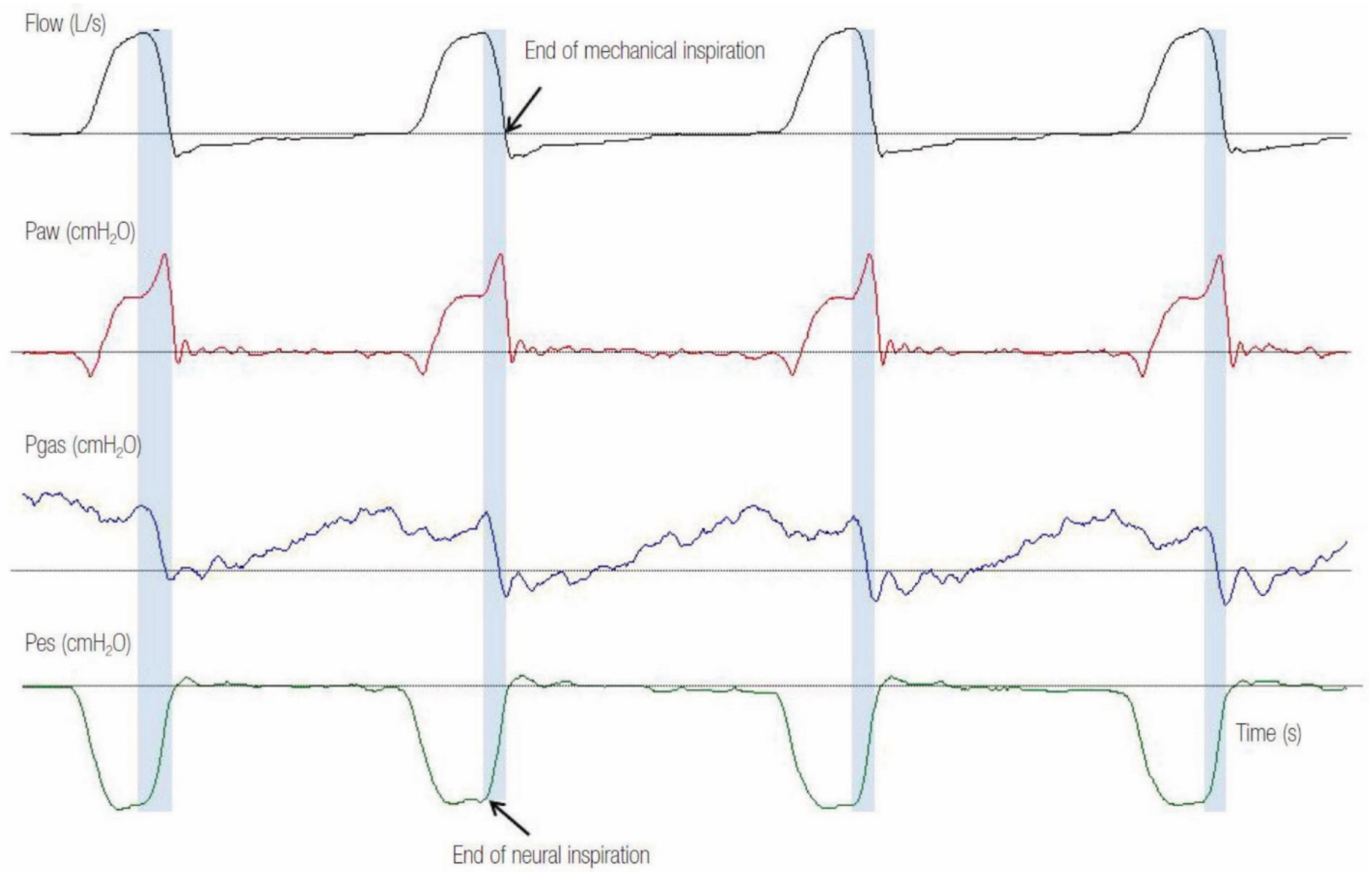
3.3.2. Delayed Cycling Off
3.4. Reverse Triggering
4. Consequences of Dyssynchrony
5. How to Improve Synchrony
5.1. Trigger Synchrony
5.2. Flow Synchrony
5.3. Cycling Synchrony
6. Newer Ventilator Modes and Patient–Ventilator Synchrony
6.1. Neurally Adjusted Ventilatory Assist (NAVA)
6.2. Proportional Assist Ventilation (PAV)
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Mehta, A.B.; Syeda, S.N.; Wiener, R.S.; Walkey, A. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. J. Crit. Care 2015, 30, 1217–1221. [Google Scholar] [CrossRef] [Green Version]
- MacIntyre, N.R. Principles of mechanical ventilation. In Textbook of Respiratory Medicine, 3rd ed.; Murray, J., Nadel, J., Mason, R., Boushey, H., Eds.; WB Saunders: Philadelphia, PA, USA, 2004. [Google Scholar]
- Mora Carpio, A.L.; Mora, J.I. Ventilator Management. In Treasure Island; StatPearls; StatPearls Publishing: San Francisco, CA, USA, 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK448186/ (accessed on 7 May 2021).
- Kalabalik, J.; Brunetti, L.; El-Srougy, R. Intensive care unit delirium: A review of the literature. J. Pharm. Pract. 2014, 27, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Hermans, G.; Van den Berghe, G. Clinical review: Intensive care unit acquired weakness. Crit. Care 2015, 19, 274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strom, T.; Martinussen, T.; Toft, P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: A randomised trial. Lancet 2010, 375, 475–480. [Google Scholar] [CrossRef]
- Mauri, T.; The PLeUral Pressure Working Group (PLUG—Acute Respiratory Failure Section of the European Society of Intensive Care Medicine); Yoshida, T.; Bellani, G.; Goligher, E.; Carteaux, G.; Rittayamai, N.; Mojoli, F.; Chiumello, D.A.; Piquilloud, L.; et al. Esophageal and transpulmonary pressure in the clinical setting: Meaning, usefulness and perspectives. Intensive Care Med. 2016, 42, 1360–1373. [Google Scholar] [CrossRef]
- Georgopoulos, D.; Prinianakis, G.; Kondili, E. Bedside waveforms interpretation as a tool to identify patient-ventilator asynchronies. Intensive Care Med. 2006, 32, 34–47. [Google Scholar] [CrossRef]
- Chao, D.C.; Scheinhorn, D.J.; Stearn-Hassenpflug, M. Patient-ventilator trigger asynchrony in prolonged mechanical ventilation. Chest 1997, 112, 1592–1599. [Google Scholar] [CrossRef]
- Thille, A.W.; Rodriguez, P.; Cabello, B.; Lellouche, F.; Brochard, L. Patient-ventilator asynchrony during assisted mechanical ventilation. Intensive Care Med. 2006, 32, 1515–1522. [Google Scholar] [CrossRef]
- De Wit, M.; Pedram, S.; Best, A.M. Observational study of patient-ventilator asynchrony and relationship to sedation level. J. Crit. Care 2009, 24, 74–80. [Google Scholar] [CrossRef] [Green Version]
- Colombo, D.; Cammarota, G.; Alemani, M.; Epstein, S.K. Efficacy of ventilator waveforms observation in detecting patient-ventilator asynchrony. Crit. Care Med. 2011, 39, 2452–2457. [Google Scholar] [CrossRef]
- Blanch, L.; Villagra, A.; Sales, B.; Montanya, J.; Lucangelo, U.; Luján, M.; García-Esquirol, O.; Chacón, E.; Estruga, A.; Oliva, J.C.; et al. Asynchronies during mechanical ventilation are associated with mortality. Intensive Care Med. 2015, 41, 633–641. [Google Scholar] [CrossRef] [Green Version]
- Thille, A.W.; Cabello, B.; Galia, F.; Lyazidi, A.; Brochard, L. Reduction of patient-ventilator asynchrony by reducing tidal volume during pressure-support ventilation. Intensive Care Med. 2008, 34, 1477–1486. [Google Scholar] [CrossRef] [PubMed]
- Chanques, G.; Kress, J.P.; Pohlman, A.; Patel, S.; Poston, J.; Jaber, S.; Hall, J.B. Impact of ventilator adjustment and sedation-analgesia practices on severe asynchrony in patients ventilated in assist-control mode. Crit. Care Med. 2013, 41, 2177–2187. [Google Scholar] [CrossRef] [PubMed]
- Gilstrap, D.; MacIntyre, N. Patient-ventilator interactions. Implications for clinical management. Am. J. Respir. Crit. Care Med. 2013, 188, 1058–1068. [Google Scholar] [CrossRef] [PubMed]
- Pham, T.; Telias, I.; Piraino, T.; Yoshida, T.; Brochard, L.J. Asynchrony Consequences and Management. Crit. Care Clin. 2018, 34, 325–341. [Google Scholar] [CrossRef] [PubMed]
- Antonogiannaki, E.M.; Georgopoulos, D.; Akoumianaki, E. Patient-Ventilator Dyssynchrony. Korean J. Crit. Care Med. 2017, 32, 307–322. [Google Scholar] [CrossRef] [PubMed]
- De Wit, M. Monitoring of Patient-Ventilator Interaction at the Bedside. Respir. Care 2011, 56, 61–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leung, P.; Jubran, A.; Tobin, M.J. Comparison of assisted ventilator modes on triggering, patient effort, and dyspnea. Am. J. Respir. Crit. Care Med. 1997, 155, 1940–1948. [Google Scholar] [CrossRef] [PubMed]
- Younes, M.; Kun, J.; Webster, K.; Roberts, D. Response of ventilator-dependent patients to delayed opening of exhalation valve. Am. J. Respir. Crit. Care Med. 2002, 166, 21–30. [Google Scholar] [CrossRef]
- MacIntyre, N.R.; Cheng, K.C.; McConnell, R. Applied PEEP during pressure support reduces the inspiratory threshold load of intrinsic PEEP. Chest 1997, 111, 188–193. [Google Scholar] [CrossRef]
- Nava, S.; Bruschi, C.; Rubini, F.; Palo, A.; Iotti, G.A.; Braschi, A. Respiratory response and inspiratory effort during pressure support ventilation in COPD patients. Intensive Care Med. 1995, 21, 871–879. [Google Scholar] [CrossRef]
- Rossi, A.; Polese, G.; Brandi, G.; Conti, G. Intrinsic positive end-expiratory pressure (PEEPi). Intensive Care Med. 1995, 21, 522–536. [Google Scholar] [CrossRef] [PubMed]
- Fabry, B.; Guttmann, J.; Eberhard, L.; Bauer, T.; Haberthür, C.; Wolff, G. An analysis of desynchronization between the spontaneously breathing patient and ventilator during inspiratory pressure support. Chest 1995, 107, 1387–1394. [Google Scholar] [CrossRef]
- Epstein, S.K. How often does patient–ventilator asynchrony occur and what are the consequences? Respir. Care 2011, 56, 25–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Imanaka, H.; Nishimura, M.; Takeuchi, M.; Kimball, W.R.; Yahagi, N.; Kumon, K. Autotriggering caused by cardiogenic oscillation during flow-triggered mechanical ventilation. Crit. Care Med. 2000, 28, 402–407. [Google Scholar] [CrossRef] [PubMed]
- Hill, L.L.; Pearl, R.G. Flow triggering, pressure triggering, and autotriggering during mechanical ventilation. Crit. Care Med. 2000, 28, 579–581. [Google Scholar] [CrossRef]
- Marini, J.J.; Capps, J.S.; Culver, B.H. The inspiratory work of breathing during assisted mechanical ventilation. Chest 1985, 87, 612–618. [Google Scholar] [CrossRef]
- Marini, J.J.; Rodriguez, R.M.; Lamb, V. The inspiratory workload of patient initiated mechanical ventilation. Am. Rev. Respir. Dis. 1986, 134, 902–909. [Google Scholar] [CrossRef]
- Yang, L.Y.; Huang, Y.C.; Macintyre, N.R. Patient–ventilator synchrony during pressure-targeted versus flow-targeted small tidal volume assisted ventilation. J. Crit. Care 2007, 22, 252–257. [Google Scholar] [CrossRef]
- Kallet, R.H.; Campbell, A.R.; Alonso, J.A.; Morabito, D.J.; Mackersie, R.C. The effects of pressure control versus volume control assisted ventilation on patient work of breathing in acute lung injury and acute respiratory distress syndrome. Respir. Care 2000, 45, 1085–1096. [Google Scholar]
- Kondili, E.; Xirouchaki, N.; Georgopoulos, D. Modulation and treatment of patient-ventilator dyssynchrony. Curr. Opin. Crit. Care 2007, 13, 84–89. [Google Scholar] [CrossRef]
- Gentile, M.A. Cycling of the mechanical ventilator breath. Respir. Care 2011, 56, 52–60. [Google Scholar] [CrossRef] [Green Version]
- Pierson, D.J. Patient–ventilator interaction. Respir. Care 2011, 56, 214–228. [Google Scholar] [CrossRef] [Green Version]
- Gea, J.; Zhu, E.; Gáldiz, J.B.; Comtois, N.; Salazkin, I.; Fiz, J.A.; Grassino, A. Functional consequences of eccentric contractions of the diaphragm. Arch. Bronconeumol. 2009, 45, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Pohlman, M.C.; McCallister, K.E.; Schweickert, W.D.; Pohlman, A.S.; Nigos, C.P.; Krishnan, J.A.; Charbeneau, J.T.; Gehlbach, B.K.; Kress, J.P.; Hall, J.B. Excessive tidal volume from breath stacking during lung-protective ventilation for acute lung injury. Crit. Care Med. 2008, 36, 3019–3023. [Google Scholar] [CrossRef] [PubMed]
- Tokioka, H.; Tanaka, T.; Ishizu, T.; Fukushima, T.; Iwaki, T.; Nakamura, Y.; Kosogabe, Y. The effect of breath termination criterion on breathing patterns and the work of breathing during pressure support ventilation. Anesth Analg. 2001, 92, 161–165. [Google Scholar] [CrossRef] [PubMed]
- Vaporidi, K.; Babalis, D.; Chytas, A.; Lilitsis, E.; Kondili, E.; Amargianitakis, V.; Chouvarda, I.; Maglaveras, N.; Georgopoulos, D. Clusters of ineffective efforts during mechanical ventilation: Impact on outcome. Intensive Care Med. 2017, 43, 184–191. [Google Scholar] [CrossRef]
- Fernandez, R.; Mendez, M.; Younes, M. Effect of ventilator flow rate on respiratory timing in normal humans. Am. J. Respir. Crit. Care Med. 1999, 159, 710–719. [Google Scholar] [CrossRef]
- Chiumello, D.; Polli, F.; Tallarini, F.; Chierichetti, M.; Motta, G.; Azzari, S.; Colombo, R.; Rech, R.; Pelosi, P.; Raimondi, F.; et al. Effect of different cycling-off criteria and positive end-expiratory pressure during pressure support ventilation in patients with chronic obstructive pulmonary disease. Crit. Care Med. 2007, 35, 2547–2552. [Google Scholar] [CrossRef]
- Kondili, E.; Prinianakis, G.; Georgopoulos, D. Patient-ventilator interaction. Br. J. Anaesth. 2003, 91, 106–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akoumianaki, E.; Lyazidi, A.; Rey, N.; Matamis, D.; Perez-Martinez, N.; Giraud, R.; Mancebo, J.; Brochard, L.; Richard, J.-C.M. Mechanical ventilation-induced reverse-triggered breaths: A frequently unrecognized form of neuromechanical coupling. Chest 2013, 143, 927–938. [Google Scholar] [CrossRef]
- Graves, C.; Glass, L.; Laporta, D.; Meloche, R.; Grassino, A. Respiratory phase locking during mechanical ventilation in anesthetized human subjects. Am. J. Physiol. 1986, 250, R902–R909. [Google Scholar] [CrossRef] [Green Version]
- Simon, P.M.; Habel, A.M.; Daubenspeck, J.A.; Leiter, J.C. Vagal feedback in the entrainment of respiration to mechanical ventilation in sleeping humans. J. Appl. Physiol. 1985, 2000, 760–769. [Google Scholar] [CrossRef] [Green Version]
- Muzzin, S.; Baconnier, P.; Benchetrit, G. Entrainment of respiratory rhythm by periodic lung inflation: Effect of airflow rate and duration. Am. J. Physiol. 1992, 263, R292–R300. [Google Scholar] [CrossRef]
- Delisle, S.; Charbonney, E.; Albert, M.; Ouellet, P.; Marsolais, P.; Rigollot, M.; Savary, D.; Richard, J.-C.M.; Serri, K. Patient-ventilator asynchrony due to reverse triggering occurring in brain-dead patients: Clinical implications and physiological meaning. Am. J. Respir. Crit. Care Med. 2016, 194, 1166–1168. [Google Scholar] [CrossRef] [PubMed]
- De Wit, M.; Miller, K.B.; Green, D.A.; Ostman, H.E.; Gennings, C.; Epstein, S.K. Ineffective triggering predicts increased duration of mechanical ventilation. Crit. Care Med. 2009, 37, 2740–2745. [Google Scholar] [PubMed]
- Kahn, J.M.; Andersson, L.; Karir, V.; Polissar, N.L.; Neff, M.J.; Rubenfeld, G.D. Low tidal volume ventilation does not increase sedation use in patients with acute lung injury. Crit. Care Med. 2005, 33, 766–771. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshida, T.; Fujino, Y.; Amato, M.B.P.; Kavanagh, B.P. Fifty years of research in ARDS. Spontaneous breathing during mechanical ventilation. Risks, mechanisms, and management. Am. J. Respir. Crit. Care Med. 2017, 195, 985–992. [Google Scholar] [CrossRef]
- Imsand, C.; Feihl, F.; Perret, C.; Fitting, J.W. Regulation of inspiratory neuromuscular output during synchronized intermittent mechanical ventilation. Anesthesiology 1994, 80, 13–22. [Google Scholar] [CrossRef] [PubMed]
- Jubran, A.; Van de Graaff, W.B.; Tobin, M.J. Variability of patient– ventilator interaction with pressure support ventilation in patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 1995, 152, 129–136. [Google Scholar] [CrossRef]
- Tassaux, D.; Gainnier, M.; Battisti, A.; Jolliet, P. Impact of expiratory trigger setting on delayed cycling and inspiratory muscle workload. Am. J. Respir. Crit. Care Med. 2005, 172, 1283–1289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sassoon, C.S. Triggering of the ventilator in patient–ventilator interactions. Respir. Care 2011, 56, 39–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MacIntyre, N.R. Patient–ventilator interactions: Optimizing conventional ventilation modes. Respir. Care 2011, 56, 73–84, discussion 81–84. [Google Scholar] [CrossRef] [Green Version]
- MacIntyre, N.R.; Ho, L.I. Effects of initial flow rate and breath termination criteria on pressure support ventilation. Chest 1991, 99, 134–138. [Google Scholar] [CrossRef]
- Chiumello, D.; Pelosi, P.; Croci, M.; Bigatello, L.M.; Gattinoni, L. The effects of pressurization rate on breathing pattern, work of breathing, gas exchange and patient comfort in pressure support ventilation. Eur. Respir. J. 2001, 18, 107–114. [Google Scholar] [CrossRef] [Green Version]
- Sinderby, C.; Beck, J. Proportional assist ventilation and neurally adjusted ventilatory assist—better approaches to patient ventilator synchrony? Clin. Chest Med. 2008, 29, 329–342. [Google Scholar] [CrossRef]
- Spahija, J.; de Marchie, M.; Albert, M.; Bellemare, P.; Delisle, S.; Beck, J.; Sinderby, C. Patient–ventilator interaction during pressure support ventilation and neurally adjusted ventilatory assist. Crit. Care Med. 2010, 38, 518–526. [Google Scholar] [CrossRef]
- Piquilloud, L.; Vignaux, L.; Bialais, E.; Roeseler, J.; Sottiaux, T.; Laterre, P.-F.; Jolliet, P.; Tassaux, D. Neurally adjusted ventilatory assist improves patient-ventilator interaction. Intensive Care Med. 2011, 37, 263–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mauri, T.; Bellani, G.; Grasselli, G.; Confalonieri, A.; Rona, R.; Patroniti, N.; Pesenti, A. Patient-ventilator interaction in ARDS patients with extremely low compliance undergoing ECMO: A novel approach based on diaphragm electrical activity. Intensive Care Med. 2013, 39, 282–291. [Google Scholar] [CrossRef]
- Younes, M. Proportional assist ventilation, a new approach to ventilatory support. Theory Am. Rev. Respir. Dis. 1992, 145, 114–120. [Google Scholar] [CrossRef]
- Alexopoulou, C.; Kondili, E.; Plataki, M.; Georgopoulos, D. Patient-ventilator synchrony and sleep quality with proportional assist and pressure support ventilation. Intensive Care Med. 2013, 39, 1040–1047. [Google Scholar] [CrossRef] [PubMed]
- Xirouchaki, N.; Kondili, E.; Vaporidi, K.; Xirouchakis, G.; Klimathianaki, M.; Gavriilidis, G.; Alexandopoulou, E.; Plataki, M.; Alexopoulou, C.; Georgopoulos, D. Proportional assist ventilation with load adjustable gain factors in critically ill patients: Comparison with pressure support. Intensive Care Med. 2008, 34, 2026–2034. [Google Scholar] [CrossRef] [PubMed]




Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Oliveira, B.; Aljaberi, N.; Taha, A.; Abduljawad, B.; Hamed, F.; Rahman, N.; Mallat, J. Patient–Ventilator Dyssynchrony in Critically Ill Patients. J. Clin. Med. 2021, 10, 4550. https://doi.org/10.3390/jcm10194550
De Oliveira B, Aljaberi N, Taha A, Abduljawad B, Hamed F, Rahman N, Mallat J. Patient–Ventilator Dyssynchrony in Critically Ill Patients. Journal of Clinical Medicine. 2021; 10(19):4550. https://doi.org/10.3390/jcm10194550
Chicago/Turabian StyleDe Oliveira, Bruno, Nahla Aljaberi, Ahmed Taha, Baraa Abduljawad, Fadi Hamed, Nadeem Rahman, and Jihad Mallat. 2021. "Patient–Ventilator Dyssynchrony in Critically Ill Patients" Journal of Clinical Medicine 10, no. 19: 4550. https://doi.org/10.3390/jcm10194550
APA StyleDe Oliveira, B., Aljaberi, N., Taha, A., Abduljawad, B., Hamed, F., Rahman, N., & Mallat, J. (2021). Patient–Ventilator Dyssynchrony in Critically Ill Patients. Journal of Clinical Medicine, 10(19), 4550. https://doi.org/10.3390/jcm10194550






