Lack of Salivary Long Non-Coding RNA XIST Expression Is Associated with Increased Risk of Oral Squamous Cell Carcinoma: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Salivary RNA Extraction
2.3. RT-qPCR
2.4. Statistical Analysis
3. Results
3.1. The Characteristics of Participants
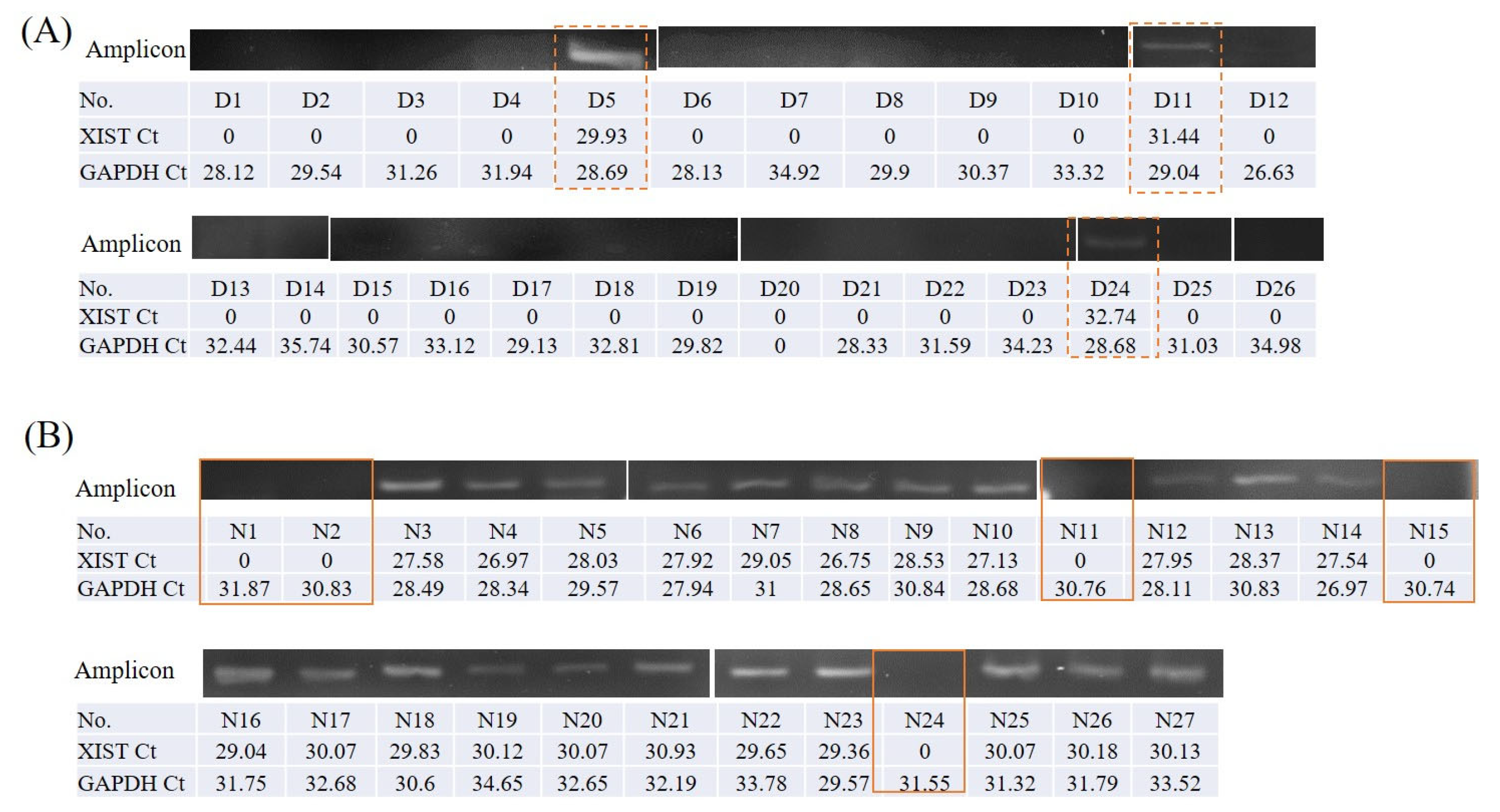
3.2. Salivary lncRNA XIST Was Expressed Only in Females
3.3. Clinical–Pathological Data Difference between Sex among Patients with OSCC
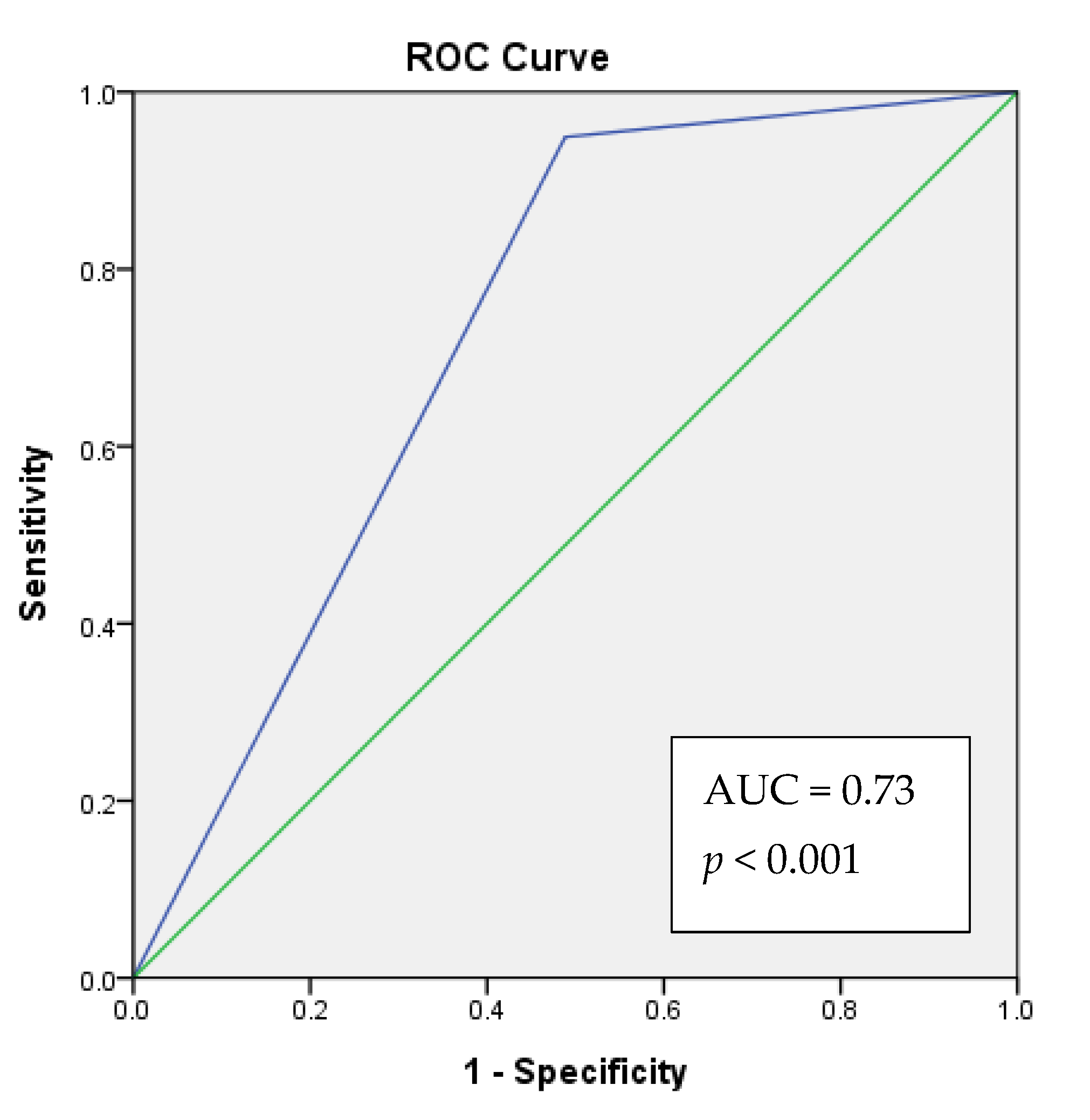
3.4. Increased Risk of OSCC in Individuals without Salivary lncRNA XIST Expression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mathur, P.T.; Dayal, P.K.; Pai, K.M. Correlation of clinical patterns of oral squamous cell carcinoma with age, site, sex and habits. J. Indian Acad. Oral Med. Radiol. 2011, 23, 81–85. [Google Scholar] [CrossRef]
- Petti, S.; Masood, M.; Scully, C. The Magnitude of Tobacco Smoking-Betel Quid Chewing-Alcohol Drinking Interaction Effect on Oral Cancer in South-East Asia. A Meta-Analysis of Observational Studies. PLoS ONE 2013, 8, e78999. [Google Scholar] [CrossRef] [PubMed]
- França, D.C.C.; Monti, L.M.; De Castro, A.L.; Soubhia, A.M.P.; Volpato, L.E.R.; De Aguiar, S.M.H.C.; Goiato, M. Unusual Presentation of Oral Squamous Cell Carcinoma in a Young Woman. Sultan Qaboos Univ. Med. J. 2012, 12, 228–231. [Google Scholar] [CrossRef] [Green Version]
- Song, P.; Ye, L.-F.; Zhang, C.; Peng, T.; Zhou, X.-H. Long non-coding RNA XIST exerts oncogenic functions in human nasopharyngeal carcinoma by targeting miR-34a-5p. Gene 2016, 592, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Shi, Z.; Dragin, N.; Miller, M.L.; Stringer, K.F.; Johansson, E.; Chen, J.; Uno, S.; Gonzalez, F.J.; Rubio, C.A.; Nebert, D.W. Oral benzo[a]pyrene-induced cancer: Two distinct types in different target organs depend on the mouse Cyp1 genotype. Int. J. Cancer 2010, 127, 2334–2350. [Google Scholar] [CrossRef] [Green Version]
- Xing, F.; Liu, Y.; Wu, S.-Y.; Wu, K.; Sharma, S.; Mo, Y.-Y.; Feng, J.; Sanders, S.; Jin, G.; Singh, R.; et al. Loss of XIST in Breast Cancer Activates MSN-c-Met and Reprograms Microglia via Exosomal miRNA to Promote Brain Metastasis. Cancer Res. 2018, 78, 4316–4330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, Y.-J.; Lin, S.-C.; Kao, T.; Chang, C.-S.; Hong, P.-S.; Shieh, T.-M.; Chang, K.-W. Genome-wide profiling of oral squamous cell carcinoma. J. Pathol. 2004, 204, 326–332. [Google Scholar] [CrossRef]
- Li, Q.; Sun, Q.; Zhu, B. LncRNA XIST Inhibits the Progression of Oral Squamous Cell Carcinoma via Sponging miR-455-3p/BTG2 Axis. OncoTargets Ther. 2020, 13, 11211–11220. [Google Scholar] [CrossRef]
- Chiang, C.-J.; Lo, W.-C.; Yang, Y.-W.; You, S.-L.; Chen, C.-J.; Lai, M.-S. Incidence and survival of adult cancer patients in Taiwan, 2002–2012. J. Formos. Med. Assoc. 2016, 115, 1076–1088. [Google Scholar] [CrossRef] [Green Version]
- Spielmann, N.; Ilsley, D.; Gu, J.; Lea, K.; Brockman, J.; Heater, S.; Setterquist, R.; Wong, D.T.W. The Human Salivary RNA Transcriptome Revealed by Massively Parallel Sequencing. Clin. Chem. 2012, 58, 1314–1321. [Google Scholar] [CrossRef]
- Bonne, N.J.; Wong, D.T. Salivary biomarker development using genomic, proteomic and metabolomic approaches. Genome Med. 2012, 4, 82. [Google Scholar] [CrossRef] [PubMed]
- Ishikawa, S.; Sugimoto, M.; Kitabatake, K.; Sugano, A.; Nakamura, M.; Kaneko, M.; Ota, S.; Hiwatari, K.; Enomoto, A.; Soga, T.; et al. Identification of salivary metabolomic biomarkers for oral cancer screening. Sci. Rep. 2016, 6, 31520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, T.; Gao, G.; Cao, Y. Long Noncoding RNAs as Novel Biomarkers Have a Promising Future in Cancer Diagnostics. Dis. Markers 2016, 2016, 9085195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, H.; Wu, Z.; Zhang, J.; Su, B. Salivary lncRNA as a potential marker for oral squamous cell carcinoma diagnosis. Mol. Med. Rep. 2013, 7, 761–766. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.-J.; Chen, J.-H.; Hsia, S.-M.; Liao, C.-C.; Chang, H.-W.; Shieh, T.-M.; Shih, Y.-H. Salivary LDOC1 is a gender-difference biomarker of oral squamous cell carcinoma. PeerJ 2019, 7, e6732. [Google Scholar] [CrossRef] [Green Version]
- Gardner, R.L.; Lyon, M.F. Biological Sciences: X Chromosome Inactivation studied by Injection of a Single Cell into the Mouse Blastocyst. Nature 1971, 231, 385–386. [Google Scholar] [CrossRef]
- Knuutila, S.; Aalto, Y.; Autio, K.; Björkqvist, A.-M.; El-Rifai, W.; Hemmer, S.; Huhta, T.; Kettunen, E.; Kiuru-Kuhlefelt, S.; Larramendy, M.L.; et al. DNA Copy Number Losses in Human Neoplasms. Am. J. Pathol. 1999, 155, 683–694. [Google Scholar] [CrossRef] [Green Version]
- Bottarelli, L.; Azzoni, C.; Necchi, F.; Lagrasta, C.; Tamburini, E.; D’Adda, T.; Pizzi, S.; Sarli, L.; Rindi, G.; Bordi, C. Sex Chromosome Alterations Associate with Tumor Progression in Sporadic Colorectal Carcinomas. Clin. Cancer Res. 2007, 13, 4365–4370. [Google Scholar] [CrossRef] [Green Version]
- Jiang, F.; Richter, J.; Schraml, P.; Bubendorf, L.; Gasser, T.; Sauter, G.; Mihatsch, M.J.; Moch, H. Chromosomal Imbalances in Papillary Renal Cell Carcinoma: Genetic Differences between Histological Subtypes. Am. J. Pathol. 1998, 153, 1467–1473. [Google Scholar] [CrossRef]
- Indsto, J.O.; Nassif, N.; Kefford, R.; Mann, G.J. Frequent loss of heterozygosity targeting the inactive X chromosome in melanoma. Clin. Cancer Res. 2003, 9. [Google Scholar]
- Azzoni, C.; Bottarelli, L.; Pizzi, S.; D’Adda, T.; Rindi, G.; Bordi, C. Xq25 and Xq26 identify the common minimal deletion region in malignant gastroenteropancreatic endocrine carcinomas. Virchows Arch. 2005, 448, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Meyers, D.; Freije, D.; Isaacs, S.; Wiley, K.; Nusskern, D.; Ewing, C.; Wilkens, E.; Bujnovszky, P.; Bova, G.S.; et al. Evidence for a prostate cancer susceptibility locus on the X chromosome. Nat. Genet. 1998, 20, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Bray, F.; Ren, J.-S.; Masuyer, E.; Ferlay, J. Global estimates of cancer prevalence for 27 sites in the adult population in 2008. Int. J. Cancer 2013, 132, 1133–1145. [Google Scholar] [CrossRef] [PubMed]
- Gierach, G.L.; Choudhury, P.P.; García-Closas, M. Toward Risk-Stratified Breast Cancer Screening: Considerations for Changes in Screening Guidelines. JAMA Oncol. 2020, 6, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Parmigiani, G.; Berry, D.A.; Aguilar, O. Determining Carrier Probabilities for Breast Cancer–Susceptibility Genes BRCA1 and BRCA2. Am. J. Hum. Genet. 1998, 62, 145–158. [Google Scholar] [CrossRef] [Green Version]
- Tyrer, J.; Duffy, S.W.; Cuzick, J. A breast cancer prediction model incorporating familial and personal risk factors. Stat. Med. 2004, 23, 1111–1130. [Google Scholar] [CrossRef] [Green Version]
- Mazzola, E.; Chipman, J.; Cheng, S.-C.; Parmigiani, G. Recent BRCAPRO Upgrades Significantly Improve Calibration. Cancer Epidemiol. Biomark. Prev. 2014, 23, 1689–1695. [Google Scholar] [CrossRef] [Green Version]
- Antoniou, A.C.; Pharoah, P.P.D.; Smith, P.; Easton, D.F. The BOADICEA model of genetic susceptibility to breast and ovarian cancer. Br. J. Cancer 2004, 91, 1580–1590. [Google Scholar] [CrossRef] [Green Version]
- Samavarchi Tehrani, S.; Zaboli, E.; Sadeghi, F.; Khafri, S.; Karimian, A.; Rafie, M.; Parsian, H. MicroRNA-26a-5p as a potential predictive factor for determining the effectiveness of trastuzumab therapy in HER-2 positive breast cancer patients. BioMedicine 2021, 11, 6. [Google Scholar] [CrossRef]
- Tsai, S.C.S.; Huang, J.Y.; Lin, C.; Liaw, Y.P.; Lin, F.C.F. The association between human papillomavirus infection and head and neck cancer: A population-based cohort study. Medicine 2019, 98, e14436. [Google Scholar] [CrossRef] [PubMed]
| OSCC n = 59 | Control n = 43 | |
|---|---|---|
| Average age, y (mean ± SD) | ||
| Male | 53.9 ± 2.2 | 49.7 ± 2.5 |
| Female | 58.2 ± 2.3 | 39.1 ± 1.3 |
| Variable | n (%) | n (%) |
| Sex | ||
| Male | 33 (55.9) | 16 (37.2) |
| Female | 26 (44.1) | 27 (62.8) |
| Salivary lncRNA XIST expression | ||
| Male | 0 | 0 |
| Female | 3 (11%) | 22 (81%) |
| Alcohol drinking | ||
| Yes | 21 (35.6) | 0 (0) |
| No | 38 (64.4) | 43 (100) |
| Betel nut chewing | ||
| Yes | 24 (40.7) | 0 (0) |
| No | 35(59.3) | 43 (100) |
| Cigarette smoking | ||
| Yes | 31 (52.5) | 0 (0) |
| No | 28(47.5) | 43 (100) |
| Primary tumor stage | ||
| T1-T2 | 28 (47.5) | |
| T3-T4 | 31 (52.5) | |
| Differentiation | ||
| Well | 30 (50.8) | |
| Moderate | 24 (40.7) | |
| Poor | 5 (8.5) | |
| Clinical stage | ||
| I-II | 21 (35.6) | |
| III-IV | 38 (64.4) | |
| Distant metastasis (M) | ||
| Yes | 2 (3.4) | |
| No | 57 (96.6) | |
| Recurrence | ||
| Yes | 0 (0) | |
| No | 59 (100) | |
| Tumor site | ||
| Buccal | 17 (28.8) | |
| Tongue | 20 (33.9) | |
| Others | 22 (37.3) |
| Sex | |||
|---|---|---|---|
| Variable | Male n = 33 | Female n = 26 | p |
| Smoking | |||
| Yes | 20 | 4 | <0.001 *** |
| No | 13 | 22 | |
| Alcohol drinking | |||
| Yes | 28 | 3 | <0.001 *** |
| No | 5 | 23 | |
| Betel nut chewing | |||
| Yes | 20 | 1 | <0.001 *** |
| No | 13 | 25 | |
| Differentiation | |||
| Low grade or well | 22 | 9 | 0.019 * |
| moderate or poor | 11 | 17 | |
| Diagnosis | |||
| Tongue Ca. | 6 | 14 | 0.026 * |
| Buccal Ca. | 13 | 4 | |
| Gingiva Ca. | 7 | 5 | |
| Others | 7 | 3 | |
| Sex | Alcohol | Betel | Cigarette | Death | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| XIST expression | F | M | No | Yes | No | Yes | No | Yes | No | Yes |
| Yes | 3 | 0 | 3 | 0 | 3 | 0 | 2 | 1 | 3 | 0 |
| No | 23 | 33 | 25 | 31 | 35 | 21 | 33 | 23 | 38 | 18 |
| Fishe’s exact test p (two-tailed) | 0.08 | 0.1 | 0.546 | 1 | 0.546 | |||||
| Phi | 0.261 * | 0.244 | 0.172 | 0.035 | 0.153 | |||||
| OSCC | Alcohol | Betel Nut | Cigarette | |||||
|---|---|---|---|---|---|---|---|---|
| XIST expression | No | Yes | No | Yes | No | Yes | No | Yes |
| Yes | 22 | 3 | 25 | 0 | 25 | 0 | 24 | 1 |
| No | 5 | 23 | 25 | 3 | 27 | 1 | 25 | 3 |
| Fisher exact test p (two-tail) | <0.001 | 0.238 | 1 | 0.613 | ||||
| Phi | 0.7 *** | 0.231 | 0.131 | 0.127 | ||||
| B | S.E. | p | OR | ||
|---|---|---|---|---|---|
| All Participants n = 102 | XIST expression | 2.973 | 0.667 | <0.001 | 19.556 |
| constant | −1.992 | 0.615 | 0.001 | 0.136 | |
| Female subjects n = 53 | XIST expression | 3.518 | 0.789 | <0.001 | 33.733 |
| constant | −1.992 | 0.615 | 0.001 | 0.136 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shieh, T.-M.; Liu, C.-J.; Hsia, S.-M.; Ningrum, V.; Liao, C.-C.; Lan, W.-C.; Shih, Y.-H. Lack of Salivary Long Non-Coding RNA XIST Expression Is Associated with Increased Risk of Oral Squamous Cell Carcinoma: A Cross-Sectional Study. J. Clin. Med. 2021, 10, 4622. https://doi.org/10.3390/jcm10194622
Shieh T-M, Liu C-J, Hsia S-M, Ningrum V, Liao C-C, Lan W-C, Shih Y-H. Lack of Salivary Long Non-Coding RNA XIST Expression Is Associated with Increased Risk of Oral Squamous Cell Carcinoma: A Cross-Sectional Study. Journal of Clinical Medicine. 2021; 10(19):4622. https://doi.org/10.3390/jcm10194622
Chicago/Turabian StyleShieh, Tzong-Ming, Chung-Ji Liu, Shih-Min Hsia, Valendriyani Ningrum, Chiu-Chu Liao, Wan-Chen Lan, and Yin-Hwa Shih. 2021. "Lack of Salivary Long Non-Coding RNA XIST Expression Is Associated with Increased Risk of Oral Squamous Cell Carcinoma: A Cross-Sectional Study" Journal of Clinical Medicine 10, no. 19: 4622. https://doi.org/10.3390/jcm10194622
APA StyleShieh, T.-M., Liu, C.-J., Hsia, S.-M., Ningrum, V., Liao, C.-C., Lan, W.-C., & Shih, Y.-H. (2021). Lack of Salivary Long Non-Coding RNA XIST Expression Is Associated with Increased Risk of Oral Squamous Cell Carcinoma: A Cross-Sectional Study. Journal of Clinical Medicine, 10(19), 4622. https://doi.org/10.3390/jcm10194622









