Comparison of Methods for Estimating Retinal Shape: Peripheral Refraction vs. Optical Coherence Tomography
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
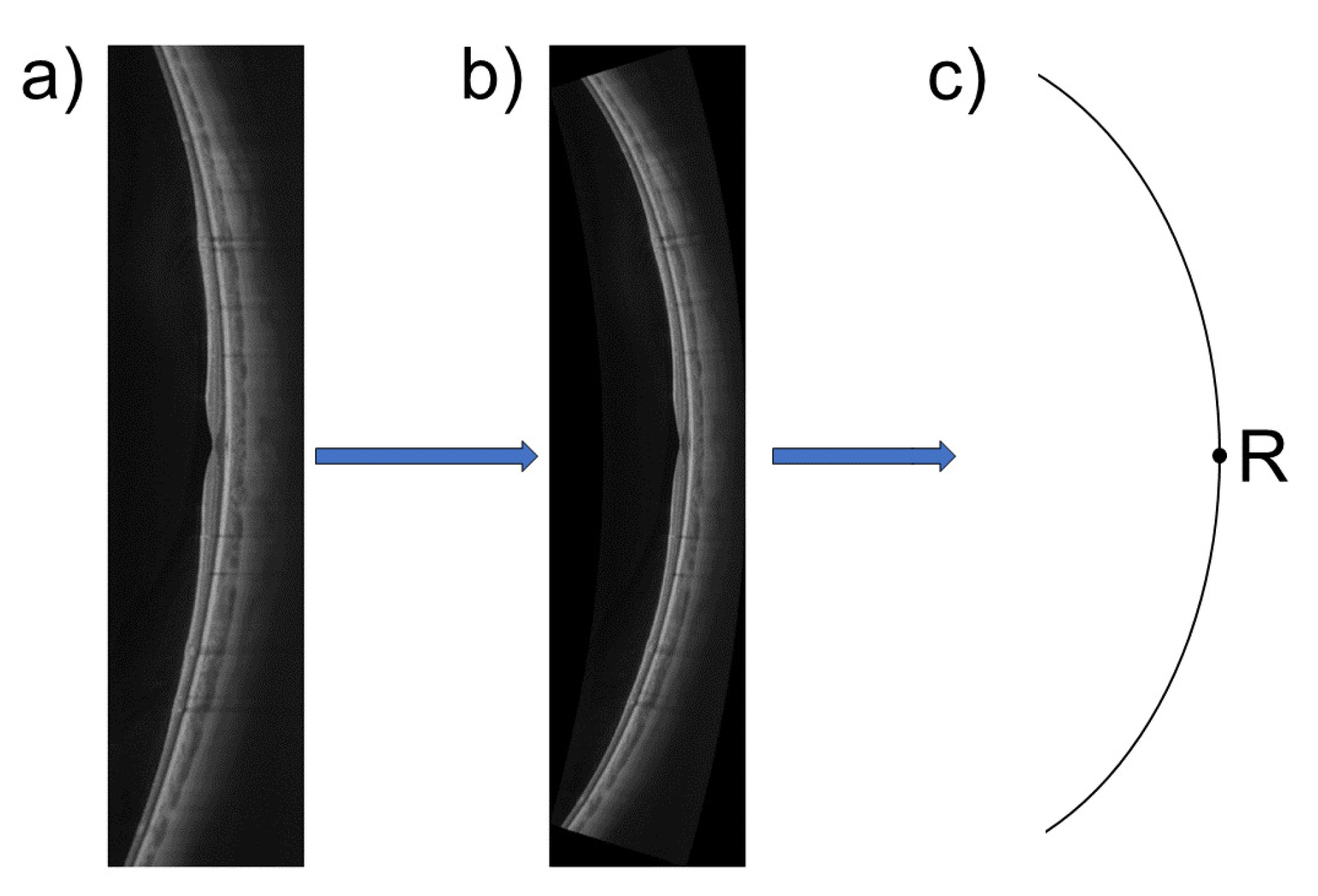
2.2. OCT-Based Retinal Shape Estimation
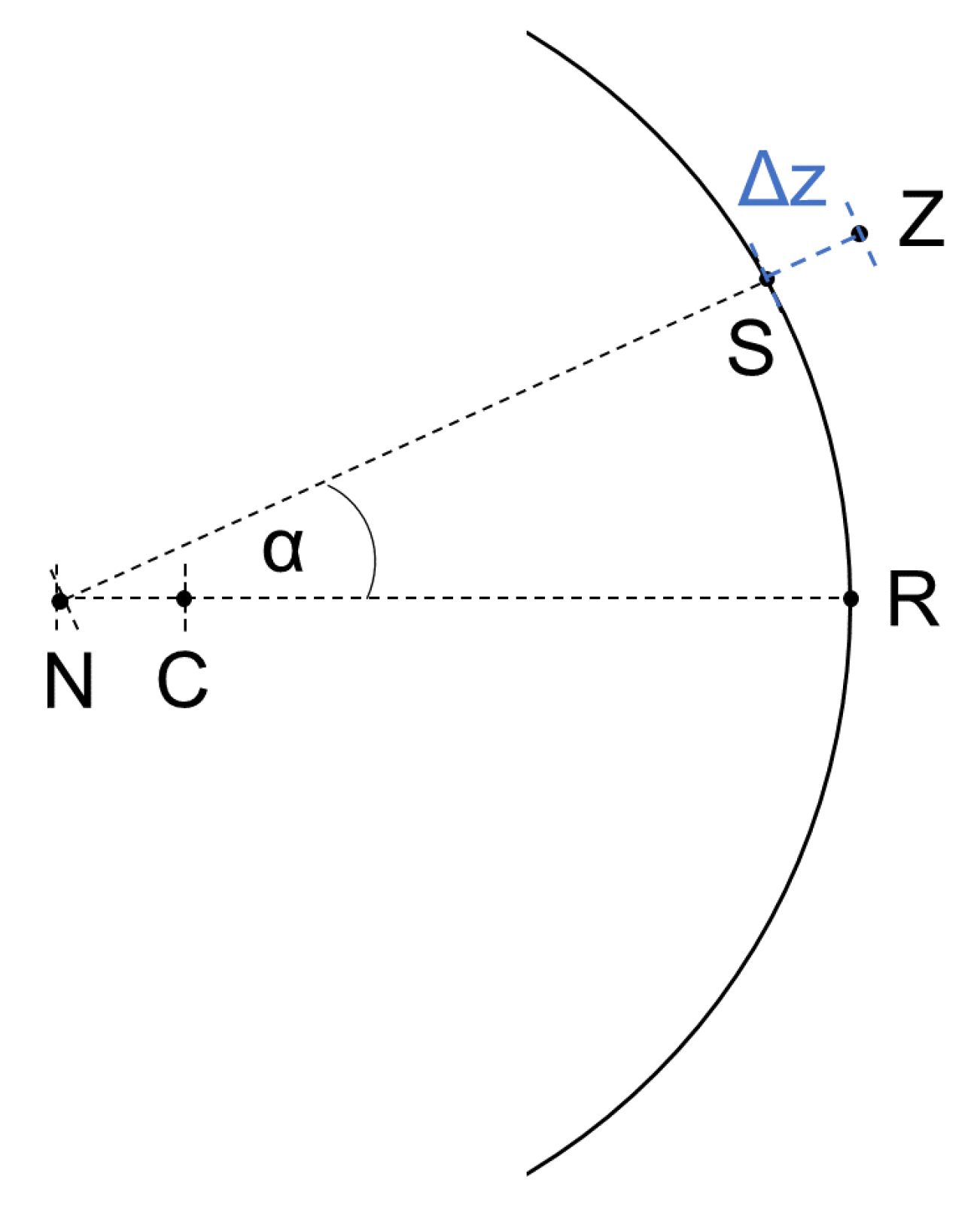
2.3. PRX-Based Retinal Shape Estimation
2.4. Statistical Data Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| OCT | Optical coherence tomography |
| RPE | Retinal pigment epithelium |
| PRX | Peripheral refraction |
| ICC | Intraclass correlation coefficient |
| MRI | Magnet resonance imaging |
References
- Saw, S.M.; Gazzard, G.; Shih-Yen, E.C.; Chua, W.H. Myopia and associated pathological complications. Ophthalmic Physiol. Opt. 2005, 25, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Read, S.A.; Fuss, J.A.; Vincent, S.J.; Collins, M.J.; Alonso-Caneiro, D. Choroidal changes in human myopia: Insights from optical coherence tomography imaging. Clin. Exp. Optom. 2019, 102, 270–285. [Google Scholar] [CrossRef]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.J.; Resnikoff, S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Chiang, P.P.C.; Fenwick, E.; Cheung, C.M.G.; Lamoureux, E.L. Public health impact of pathologic myopia. In Pathologic Myopia; Springer: Berlin/Heidelberg, Germany, 2014; pp. 75–81. [Google Scholar]
- Neil Charman, W.; Radhakrishnan, H. Peripheral refraction and the development of refractive error: A review. Ophthalmic Physiol. Opt. 2010, 30, 321–338. [Google Scholar] [CrossRef] [PubMed]
- Smith, E.L., III; Hung, L.F.; Huang, J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vis. Res. 2009, 49, 2386–2392. [Google Scholar] [CrossRef] [PubMed]
- Rempt, F.; Hoogerheide, J.; Hoogenboom, W. Peripheral retinoscopy and the skiagram. Ophthalmologica 1971, 162, 1–10. [Google Scholar] [CrossRef]
- Millodot, M. Effect of ametropia on peripheral refraction. Am. J. Optom. Physiol. Opt. 1981, 58, 691–695. [Google Scholar] [CrossRef]
- Seidemann, A.; Schaeffel, F.; Guirao, A.; Lopez-Gil, N.; Artal, P. Peripheral refractive errors in myopic, emmetropic, and hyperopic young subjects. JOSA A 2002, 19, 2363–2373. [Google Scholar] [CrossRef]
- Chen, X.; Sankaridurg, P.; Donovan, L.; Lin, Z.; Li, L.; Martinez, A.; Holden, B.; Ge, J. Characteristics of peripheral refractive errors of myopic and non-myopic Chinese eyes. Vis. Res. 2010, 50, 31–35. [Google Scholar] [CrossRef]
- Sng, C.C.; Lin, X.Y.; Gazzard, G.; Chang, B.; Dirani, M.; Chia, A.; Selvaraj, P.; Ian, K.; Drobe, B.; Wong, T.Y.; et al. Peripheral refraction and refractive error in Singapore Chinese children. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1181–1190. [Google Scholar] [CrossRef]
- Atchison, D.A. The Glenn A. Fry Award Lecture 2011: Peripheral optics of the human eye. Optom. Vis. Sci. 2012, 89, E954–E966. [Google Scholar] [CrossRef] [PubMed]
- Atchison, D.A.; Li, S.M.; Li, H.; Li, S.Y.; Liu, L.R.; Kang, M.T.; Meng, B.; Sun, Y.Y.; Zhan, S.Y.; Mitchell, P.; et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Investig. Ophthalmol. Vis. Sci. 2015, 56, 6162–6170. [Google Scholar] [CrossRef] [PubMed]
- Mutti, D.O.; Sinnott, L.T.; Mitchell, G.L.; Jones-Jordan, L.A.; Moeschberger, M.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Zadnik, K. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Investig. Ophthalmol. Vis. Sci. 2011, 52, 199–205. [Google Scholar] [CrossRef]
- Verkicharla, P.K.; Mathur, A.; Mallen, E.A.; Pope, J.M.; Atchison, D.A. Eye shape and retinal shape, and their relation to peripheral refraction. Ophthalmic Physiol. Opt. 2012, 32, 184–199. [Google Scholar] [CrossRef] [PubMed]
- Schmid, G.F. Variability of retinal steepness at the posterior pole in children 7–15 years of age. Curr. Eye Res. 2003, 27, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Mutti, D.O.; Sholtz, R.I.; Friedman, N.E.; Zadnik, K. Peripheral refraction and ocular shape in children. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1022–1030. [Google Scholar]
- Logan, N.S.; Gilmartin, B.; Wildsoet, C.F.; Dunne, M.C. Posterior retinal contour in adult human anisomyopia. Investig. Ophthalmol. Vis. Sci. 2004, 45, 2152–2162. [Google Scholar] [CrossRef]
- Verkicharla, P.K.; Suheimat, M.; Schmid, K.L.; Atchison, D.A. Peripheral refraction, peripheral eye length, and retinal shape in myopia. Optom. Vis. Sci. 2016, 93, 1072–1078. [Google Scholar] [CrossRef]
- Breher, K.; Ohlendorf, A.; Wahl, S. Myopia induces meridional growth asymmetry of the retina: A pilot study using wide-field swept-source OCT. Sci. Rep. 2020, 10, 1–8. [Google Scholar] [CrossRef]
- Steidle, M.A.; Straub, J. Estimating the shape of the human eye using widefield optical coherence tomography (OCT). In Biophotonics: Photonic Solutions for Better Health Care VI; International Society for Optics and Photonics: Bellingham, WA, USA, 2018; Volume 10685, p. 106851V. [Google Scholar]
- Schwiegerling, J. Arizona Eye Model. In Field Guide to Visual and Ophthalmic Optics; Spie Bellingham: Bellingham, WA, USA, 2004. [Google Scholar]
- Tabernero, J.; Schaeffel, F. Fast scanning photoretinoscope for measuring peripheral refraction as a function of accommodation. JOSA A 2009, 26, 2206–2210. [Google Scholar] [CrossRef]
- Gekeler, F.; Schaeffel, F.; Howland, H.C.; Wattam-Bell, J. Measurement of astigmatism by automated infrared photoretinoscopy. Optom. Vis. Sci. 1997, 74, 472–482. [Google Scholar] [CrossRef] [PubMed]
- Lilliefors, H.W. On the Kolmogorov-Smirnov test for normality with mean and variance unknown. J. Am. Stat. Assoc. 1967, 62, 399–402. [Google Scholar] [CrossRef]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med Res. 1999, 8, 135–160. [Google Scholar] [CrossRef] [PubMed]
- Shrout, P.E.; Fleiss, J.L. Intraclass correlations: Uses in assessing rater reliability. Psychol. Bull. 1979, 86, 420. [Google Scholar] [CrossRef]
- Edwards, A.L. An Introduction to Linear Regression and Correlation; Technical Report; Freeman: New York, NY, USA, 1984. [Google Scholar]
- Gustafsson, J.; Terenius, E.; Buchheister, J.; Unsbo, P. Peripheral astigmatism in emmetropic eyes. Ophthalmic Physiol. Opt. 2001, 21, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Lotmar, W.; Lotmar, T. Peripheral astigmatism in the human eye: Experimental data and theoretical model predictions. JOSA 1974, 64, 510–513. [Google Scholar] [CrossRef] [PubMed]
- Calver, R.; Radhakrishnan, H.; Osuobeni, E.; O’Leary, D. Peripheral refraction for distance and near vision in emmetropes and myopes. Ophthalmic Physiol. Opt. 2007, 27, 584–593. [Google Scholar] [CrossRef]
- Lundström, L.; Rosén, R. Peripheral aberrations. In Handbook of Visual Optics; Artal, P., Ed.; CRC Press: London, UK, 2017. [Google Scholar]
- Lan, W.; Lin, Z.; Yang, Z.; Artal, P. Two-dimensional peripheral refraction and retinal image quality in emmetropic children. Sci. Rep. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Wang, S.; Lin, Z.; Xi, X.; Lu, Y.; Pan, L.; Li, X.; Artal, P.; Lan, W.; Yang, Z. Two-Dimensional, High-Resolution Peripheral Refraction in Adults with Isomyopia and Anisomyopia. Investig. Ophthalmol. Vis. Sci. 2020, 61, 16. [Google Scholar] [CrossRef]
- Verkicharla, P.K.; Suheimat, M.; Pope, J.M.; Sepehrband, F.; Mathur, A.; Schmid, K.L.; Atchison, D.A. Validation of a partial coherence interferometry method for estimating retinal shape. Biomed. Opt. Express 2015, 6, 3235–3247. [Google Scholar] [CrossRef]
- Dunne, M.; Barnes, D.; Clement, R. A model for retinal shape changes in ametropia. Ophthalmic Physiol. Opt. 1987, 7, 159–160. [Google Scholar] [CrossRef] [PubMed]
- Dunne, M.C. A computing scheme for determination of retinal contour from peripheral refraction, keratometry and A-scan ultrasonography. Ophthalmic Physiol. Opt. 1995, 15, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Kuo, A.N.; Verkicharla, P.K.; McNabb, R.P.; Cheung, C.Y.; Hilal, S.; Farsiu, S.; Chen, C.; Wong, T.Y.; Ikram, M.K.; Cheng, C.Y.; et al. Posterior eye shape measurement with retinal OCT compared to MRI. Investig. Ophthalmol. Vis. Sci. 2016, 57, OCT196–OCT203. [Google Scholar] [CrossRef] [PubMed]
- Zheng, F.; Wong, C.W.; Sabanayagam, C.; Cheung, Y.B.; Matsumura, S.; Chua, J.; Man, R.E.K.; Ohno-Matsui, K.; Wong, T.Y.; Cheng, C.Y.; et al. Prevalence, risk factors and impact of posterior staphyloma diagnosed from wide-field optical coherence tomography in Singapore adults with high myopia. Acta Ophthalmol. 2020. [Google Scholar] [CrossRef]
- Atchison, D.A.; Pritchard, N.; Schmid, K.L. Peripheral refraction along the horizontal and vertical visual fields in myopia. Vis. Res. 2006, 46, 1450–1458. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; Amorim-de Sousa, A.; Lopes-Ferreira, D.; Villa-Collar, C.; Gutiérrez, Á.R.; González-Méijome, J.M. Relative peripheral refraction across 4 meridians after orthokeratology and LASIK surgery. Eye Vis. 2018, 5, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; González-Méijome, J.M.; Jorge, J.; Villa-Collar, C.; Gutiérrez, A.R. Peripheral refraction in myopic patients after orthokeratology. Optom. Vis. Sci. 2010, 87, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Berntsen, D.A.; Barr, C.D.; Mutti, D.O.; Zadnik, K. Peripheral defocus and myopia progression in myopic children randomly assigned to wear single vision and progressive addition lenses. Investig. Ophthalmol. Vis. Sci. 2013, 54, 5761–5770. [Google Scholar] [CrossRef] [PubMed]
- Kang, P.; Fan, Y.; Oh, K.; Trac, K.; Zhang, F.; Swarbrick, H.A. The effect of multifocal soft contact lenses on peripheral refraction. Optom. Vis. Sci. 2013, 90, 658–666. [Google Scholar] [CrossRef] [PubMed]
- Queirós, A.; Villa-Collar, C.; Jorge, J.; Gutiérrez, Á.R.; González-Méijome, J.M. Peripheral refraction in myopic eyes after LASIK surgery. Optom. Vis. Sci. 2012, 89, 977–983. [Google Scholar] [CrossRef] [PubMed]
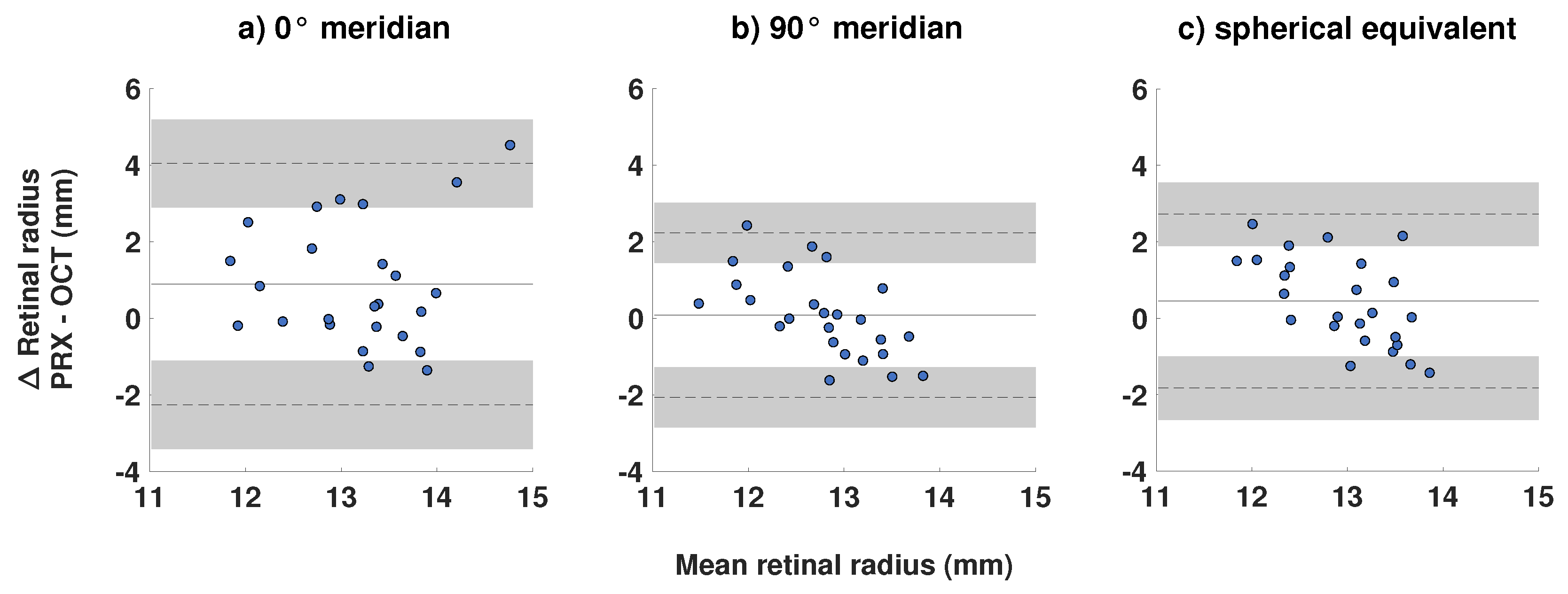

| 0 Meridian | 90 Meridian | Spherical Equivalent | |
|---|---|---|---|
| ICC analysis | |||
| ICC | 0.18 | 0.20 | 0.03 |
| p-value | 0.65 | 0.29 | 0.47 |
| Bland-Altman analysis (mm) | |||
| Mean difference | +0.89 | +0.08 | +0.45 |
| Upper limit of agreement (95% confidence interval) | +4.04 (+2.89 to +5.19) | +2.36 (+1.45 to 3.02) | +2.72 (+1.89 to +3.55) |
| Lower limit of agreement (95% confidence interval) | −2.26 (−1.11 to −3.41) | −2.07 (−1.28 to −2.85) | −1.83 (−1.00 to −2.66) |
| t-test | |||
| H/H | H | H | H |
| p-value | 0.01 | 0.07 | 0.71 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Breher, K.; Calabuig, A.; Kühlewein, L.; Ziemssen, F.; Ohlendorf, A.; Wahl, S. Comparison of Methods for Estimating Retinal Shape: Peripheral Refraction vs. Optical Coherence Tomography. J. Clin. Med. 2021, 10, 174. https://doi.org/10.3390/jcm10020174
Breher K, Calabuig A, Kühlewein L, Ziemssen F, Ohlendorf A, Wahl S. Comparison of Methods for Estimating Retinal Shape: Peripheral Refraction vs. Optical Coherence Tomography. Journal of Clinical Medicine. 2021; 10(2):174. https://doi.org/10.3390/jcm10020174
Chicago/Turabian StyleBreher, Katharina, Alejandro Calabuig, Laura Kühlewein, Focke Ziemssen, Arne Ohlendorf, and Siegfried Wahl. 2021. "Comparison of Methods for Estimating Retinal Shape: Peripheral Refraction vs. Optical Coherence Tomography" Journal of Clinical Medicine 10, no. 2: 174. https://doi.org/10.3390/jcm10020174
APA StyleBreher, K., Calabuig, A., Kühlewein, L., Ziemssen, F., Ohlendorf, A., & Wahl, S. (2021). Comparison of Methods for Estimating Retinal Shape: Peripheral Refraction vs. Optical Coherence Tomography. Journal of Clinical Medicine, 10(2), 174. https://doi.org/10.3390/jcm10020174





