Ultrasound-Guided Anterior Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Related Side Effects in Patients Undergoing Total Hip Replacement Arthroplasty: A Propensity Score-Matched Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
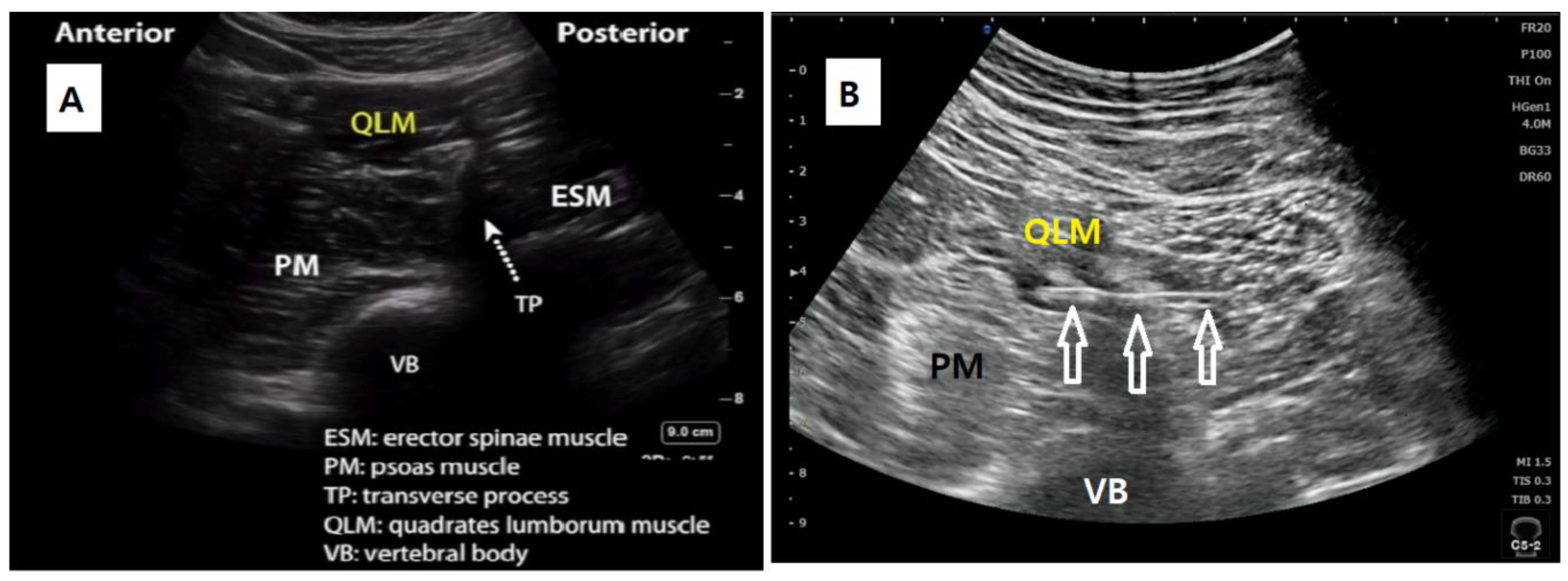
2.2. Quadratus Lumborum Block
2.3. Anesthesia and Perioperative Management
2.4. Postoperative Analgesia
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Murphy, P.; Stack, D.; Kinirons, B.; Laffey, J. Optimizing the dose of intrathecal morphine in older patients undergoing hip arthroplasty. Anesth. Analg. 2003, 97, 1709–1715. [Google Scholar] [CrossRef] [PubMed]
- Choi, P.; Bhandari, M.; Scott, J.; Douketis, J.D. Epidural analgesia for pain relief following hip or knee replacement. Cochrane Database Syst. Rev. 2003. [Google Scholar] [CrossRef] [PubMed]
- Brull, R.; McCartney, C.J.; Chan, V.W.; El-Beheiry, H. Neurological complications after regional anesthesia: Contemporary estimates of risk. Anesth. Analg. 2007, 104, 965–974. [Google Scholar] [CrossRef] [PubMed]
- Fowler, S.; Symons, J.; Sabato, S.; Myles, P. Epidural analgesia compared with peripheral nerve blockade after major knee surgery: A systematic review and meta-analysis of randomized trials. Br. J. Anaesth. 2008, 100, 154–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, C.R.; Checketts, M.R. Analgesia for primary hip and knee arthroplasty: The role of regional anaesthesia. Contin. Educ. Anaesth. Crit. Care Pain 2008, 8, 56–61. [Google Scholar] [CrossRef]
- Bugada, D.; Bellini, V.; Lorini, L.F.; Mariano, E.R. Update on selective regional analgesia for hip surgery patients. Anesthesiol. Clin. 2018, 36, 403–415. [Google Scholar] [CrossRef]
- Dam, M.; Moriggl, B.; Hansen, C.K.; Hoermann, R.; Bendtsen, T.F.; Børglum, J. The pathway of injectate spread with the transmuscular quadratus lumborum block: A cadaver study. Anesth. Analg. 2017, 125, 303–312. [Google Scholar] [CrossRef]
- Elsharkawy, H.; El-Boghdadly, K.; Barrington, M. Quadratus lumborum block: Anatomical concepts, mechanisms, and techniques. Anesthesiology 2019, 130, 322–335. [Google Scholar] [CrossRef]
- La Colla, L.; Uskova, A.; Ben-David, B. Single-shot quadratus lumborum block for postoperative analgesia after minimally invasive hip arthroplasty: A new alternative to continuous lumbar plexus block? Reg. Anesth. Pain Med. 2017, 42, 125–126. [Google Scholar] [CrossRef]
- Tulgar, S.; Ermis, M.N.; Ozer, Z. Combination of lumbar erector spinae plane block and transmuscular quadratus lumborum block for surgical anaesthesia in hemiarthroplasty for femoral neck fracture. Indian J. Anaesth. 2018, 62, 802. [Google Scholar] [CrossRef] [PubMed]
- Elsharkawy, H.; El-Boghdadly, K.; Kolli, S.; Esa, W.A.; DeGrande, S.; Soliman, L.M.; Drake, R.L. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block. Eur. J. Anaesthesiol. 2017, 34, 587–595. [Google Scholar] [CrossRef]
- Hockett, M.M.; Hembrador, S.; Lee, A. Continuous quadratus lumborum block for postoperative pain in total hip arthroplasty: A case report. A&A Pract. 2016, 7, 129–131. [Google Scholar] [CrossRef]
- Børglum, J.; Moriggl, B.; Jensen, K.; Lønnqvist, P.-A.; Christensen, A.F.; Sauter, A.; Bendtsen, T.F. Ultrasound-guided transmuscular quadratus lumborum blockade. BJA Br. J. Anaesth. 2013, 111. [Google Scholar] [CrossRef]
- Dam, M.; Hansen, C.K.; Poulsen, T.D.; Azawi, N.H.; Wolmarans, M.; Chan, V.; Laier, G.H.; Bendtsen, T.F.; Børglum, J. Transmuscular quadratus lumborum block for percutaneous nephrolithotomy reduces opioid consumption and speeds ambulation and discharge from hospital: A single centre randomised controlled trial. Br. J. Anaesth. 2019, 123, e350–e358. [Google Scholar] [CrossRef]
- Gammaitoni, A.R.; Fine, P.; Alvarez, N.; McPherson, M.L.; Bergmark, S. Clinical application of opioid equianalgesic data. Clin. J. Pain 2003, 19, 286–297. [Google Scholar] [CrossRef]
- Kadam, V.R. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J. Anaesthesiol. Clin. Pharmacol. 2013, 29, 550. [Google Scholar] [CrossRef]
- Blanco, R. 271. Tap Block Under Ultrasound Guidance: The Description of a “No Pops” Technique. Reg. Anesth. Pain Med. 2007, 32. [Google Scholar] [CrossRef]
- Ueshima, H.; Otake, H.; Lin, J.-A. Ultrasound-guided quadratus lumborum block: An updated review of anatomy and techniques. BioMed Res. Int. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Carline, L.; McLeod, G.; Lamb, C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. BJA Br. J. Anaesth. 2016, 117, 387–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brixel, S.M.; Biboulet, P.; Swisser, F.; Choquet, O.; Aarab, Y.; Nguyen, H.; Bringuier, S.; Capdevila, X. Posterior Quadratus Lumborum Block in Total Hip Arthroplasty: A Randomized Controlled Trial. Anesthesiology 2021, 134, 722–733. [Google Scholar] [CrossRef]
- Ueshima, H.; Yoshiyama, S.; Otake, H. The ultrasound-guided continuous transmuscular quadratus lumborum block is an effective analgesia for total hip arthroplasty. J. Clin. Anesth. 2016, 31, 35. [Google Scholar] [CrossRef]
- Li, J.; Lam, D.; King, H.; Credaroli, E.; Harmon, E.; Vadivelu, N. Novel regional anesthesia for outpatient surgery. Curr. Pain Headache Rep. 2019, 23, 1–16. [Google Scholar] [CrossRef]
- Simons, M.J.; Amin, N.H.; Cushner, F.D.; Scuderi, G.R. Characterization of the Neural Anatomy in the Hip Joint to Optimize Periarticular Regional Anesthesia in Total Hip Arthroplasty. J. Surg. Orthop. Adv. 2015, 24, 221–224. [Google Scholar]
- Kukreja, P.; MacBeth, L.; Sturdivant, A.; Morgan, C.J.; Ghanem, E.; Kalagara, H.; Chan, V.W. Anterior quadratus lumborum block analgesia for total hip arthroplasty: A randomized, controlled study. Reg. Anesth. Pain Med. 2019, 44, 1075–1079. [Google Scholar] [CrossRef] [PubMed]
- Green, M.S.; Hoffman, C.R.; Iqbal, U.; Ives, O.O.; Hurd, B. Transmuscular quadratus lumborum block reduces length of stay in patients receiving total hip arthroplasty. Anesthesiol. Pain Med. 2018, 8. [Google Scholar] [CrossRef] [Green Version]
- Apfel, C.; Heidrich, F.; Jukar-Rao, S.; Jalota, L.; Hornuss, C.; Whelan, R.; Zhang, K.; Cakmakkaya, O. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br. J. Anaesth. 2012, 109, 742–753. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guay, J.; Nishimori, M.; Kopp, S. Epidural local anaesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting and pain after abdominal surgery. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H.; Holte, K. Review of postoperative ileus. Am. J. Surg. 2001, 182, S3–S10. [Google Scholar] [CrossRef]
- Karlsen, A.P.H.; Geisler, A.; Petersen, P.L.; Mathiesen, O.; Dahl, J.B. Postoperative pain treatment after total hip arthroplasty: A systematic review. Pain 2015, 156, 8–30. [Google Scholar] [CrossRef] [PubMed]
- Auroy, Y.; Benhamou, D.; Bargues, L.; Ecoffey, C.; Falissard, B.; Mercier, F.; Bouaziz, H.; Samii, K. Major complications of regional anesthesia in France: The SOS Regional Anesthesia Hotline Service. J. Am. Soc. Anesthesiol. 2002, 97, 1274–1280. [Google Scholar] [CrossRef] [Green Version]
- Biboulet, P.; Morau, D.; Aubas, P.; Bringuier-Branchereau, S.; Capdevila, X. Postoperative analgesia after total-hip arthroplasty: Comparison of intravenous patient-controlled analgesia with morphine and single injection of femoral nerve or psoas compartment block. A prospective, randomized, double-blind study. Reg. Anesth. Pain Med. 2004, 29, 102–109. [Google Scholar] [CrossRef]
- Behrends, M.; Yap, E.N.; Zhang, A.L.; Kolodzie, K.; Kinjo, S.; Harbell, M.W.; Aleshi, P. Preoperative fascia iliaca block does not improve analgesia after arthroscopic hip surgery, but causes quadriceps muscles weakness: A randomized, double-blind trial. Anesthesiology 2018, 129, 536–543. [Google Scholar] [CrossRef]
- Girón-Arango, L.; Peng, P.W.; Chin, K.J.; Brull, R.; Perlas, A. Pericapsular nerve group (PENG) block for hip fracture. Reg. Anesth. Pain Med. 2018, 43, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Aliste, J.; Layera, S.; Bravo, D.; Jara, Á.; Muñoz, G.; Barrientos, C.; Wulf, R.; Brañez, J.; Finlayson, R.J.; Tran, D.Q. Randomized comparison between pericapsular nerve group (PENG) block and suprainguinal fascia iliaca block for total hip arthroplasty. Reg. Anesth. Pain Med. 2021. [Google Scholar] [CrossRef] [PubMed]
- Pascarella, G.; Costa, F.; Del Buono, R.; Pulitanò, R.; Strumia, A.; Piliego, C.; De Quattro, E.; Cataldo, R.; Agrò, F.; Carassiti, M. Impact of the pericapsular nerve group (PENG) block on postoperative analgesia and functional recovery following total hip arthroplasty: A randomised, observer-masked, controlled trial. Anaesthesia 2021, 46, 874–878. [Google Scholar]
- Li, J.; Dai, F.; Ona Ayala, K.E.; Zhou, B.; Schonberger, R.B.; Sharma, A. Transmuscular Quadratus Lumborum and Lateral Femoral Cutaneous Nerve Block in Total Hip Arthroplasty. Clin. J. Pain 2021, 37, 366–371. [Google Scholar] [CrossRef]



| Before Matching | After PS Matching | ||||||
|---|---|---|---|---|---|---|---|
| QLB (n = 126) | Control (n = 173) | p-Value | SMD | QLB (n = 115) | Control (n = 115) | SMD | |
| Age (year) | 54.3 ± 13.3 | 58.6 ± 17.0 | 0.015 | −0.279 | 54.9 ± 13.5 | 54.1 ± 16.8 | 0.051 |
| Gender, male | 66 (52.3) | 77 (44.5) | 0.178 | 0.158 | 56 (48.7) | 59 (51.3) | −0.052 |
| BMI (kg/m2) | 25.5 ± 3.6 | 24.5 ± 3.9 | 0.037 | 0.245 | 25.2 ± 3.6 | 24.9 ± 3.8 | 0.097 |
| ASA PS I/II/III | 7.94/86.51/5.56 | 8.67/75.14/16.19 | 0.022 | 0.303 | 8.7/85.22/6.09 | 7.83/86.96/5.22 | 0.058 |
| HTN | 39 (30.95) | 76 (43.93) | 0.022 | −0.270 | 38 (33.04) | 37 (32.17) | 0.018 |
| DM | 16 (12.7) | 28 (16.18) | 0.400 | −0.099 | 14 (12.17) | 13 (11.3) | 0.027 |
| IHD | 5 (3.97) | 9 (5.2) | 0.617 | −0.059 | 3 (2.61) | 2 (1.74) | 0.059 |
| CVA | 6 (4.76) | 12 (6.94) | 0.435 | −0.122 | 6 (5.22) | 6 (5.22) | 0 |
| Preoperative NRS | 2.59 ± 0.69 | 2.54 ± 0.82 | 0.897 | 0.055 | 2.61 ± 0.66 | 2.66 ± 0.67 | −0.071 |
| Duration of anesthesia (min) | 147.34 ± 25.48 | 141.49 ± 28.22 | 0.066 | 0.217 | 145.86 ± 26.02 | 139.34 ± 21.79 | 0.271 |
| Duration of surgery (min) | 94.84 ± 26.29 | 95.31 ± 30.41 | 0.888 | −0.016 | 93.65 ± 26.13 | 95.10 ± 25.13 | −0.056 |
| Anesthetic method Spinal anesthesia General anesthesia | |||||||
| 120 (95.24) | 152 (87.86) | 0.028 | 0.267 | 109 (94.78) | 111 (96.52) | −0.071 | |
| 6 (4.76) | 21 (12.14) | 6 (5.22) | 4 (3.48) | ||||
| QLB (n = 115) | Control (n = 115) | p-Value | |
|---|---|---|---|
| Opioid related adverse events | |||
| Nausea and vomiting | |||
| 24 h | 13 (11.3) | 50 (43.48) | <0.0001 |
| 48 h | 15 (13.04) | 52 (45.22) | <0.0001 |
| Use of antiemetics | |||
| 24 h | 22 (19.13) | 73 (63.48) | <0.0001 |
| 48 h | 23 (20) | 73 (64.35) | <0.0001 |
| Hypotension | |||
| 24 h | 2 (1.74) | 7 (6.09) | 0.1104 |
| 48 h | 3 (2.61) | 9 (7.83) | 0.0899 |
| Urinary retention | 46 (40) | 38 (33.04) | 0.2738 |
| Other adverse events | |||
| Hepatic dysfunction | 5 (4.35) | 6 (5.22) | |
| Pulmonary complication | 0 (5) | 11 (15.9) | |
| Op-related complication | 2 (1.6) | 1 (1.4) | |
| Fever | 0 (0) | 2 (1.74) | |
| Pruritis | 0 (0) | 2 (1.74) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, Y.-J.; Kim, H.-T.; Kim, H.-J.; Yoon, P.-W.; Park, J.-I.; Lee, S.-H.; Ro, Y.-J.; Koh, W.-U. Ultrasound-Guided Anterior Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Related Side Effects in Patients Undergoing Total Hip Replacement Arthroplasty: A Propensity Score-Matched Cohort Study. J. Clin. Med. 2021, 10, 4632. https://doi.org/10.3390/jcm10204632
Kim Y-J, Kim H-T, Kim H-J, Yoon P-W, Park J-I, Lee S-H, Ro Y-J, Koh W-U. Ultrasound-Guided Anterior Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Related Side Effects in Patients Undergoing Total Hip Replacement Arthroplasty: A Propensity Score-Matched Cohort Study. Journal of Clinical Medicine. 2021; 10(20):4632. https://doi.org/10.3390/jcm10204632
Chicago/Turabian StyleKim, Yeon-Ju, Hyung-Tae Kim, Ha-Jung Kim, Pil-Whan Yoon, Ji-In Park, Sun-Hyung Lee, Young-Jin Ro, and Won-Uk Koh. 2021. "Ultrasound-Guided Anterior Quadratus Lumborum Block Reduces Postoperative Opioid Consumption and Related Side Effects in Patients Undergoing Total Hip Replacement Arthroplasty: A Propensity Score-Matched Cohort Study" Journal of Clinical Medicine 10, no. 20: 4632. https://doi.org/10.3390/jcm10204632






