Esthetic Assessment Succeeding Anterior Atrophic Maxilla Augmentation with Cancellous Bone-Block Allograft and Late Restoration Loading
Abstract
1. Introduction
2. Materials and Methods
- Age ≥ 18 years.
- Missing tooth in the maxillary esthetic area (between canines).
- Bone augmentation performed 6 months prior to implant placement (using allogeneic bone block).
- Implant loading 6 months after placement.
- Patients with unbalanced systemic diseases (e.g., uncontrolled diabetes).
- History of radiation to the head and neck area.
- Poor oral hygiene.
- Mucosal diseases (lichen planus).
- Para-function (bruxism).
- Using bisphosphonates, calcium channels blockers, epileptic drugs.
- Patients with immunosuppression.
- Untreated and uncontrolled periodontal disease.
- Heavy smoking (over 10 cigarettes a day).
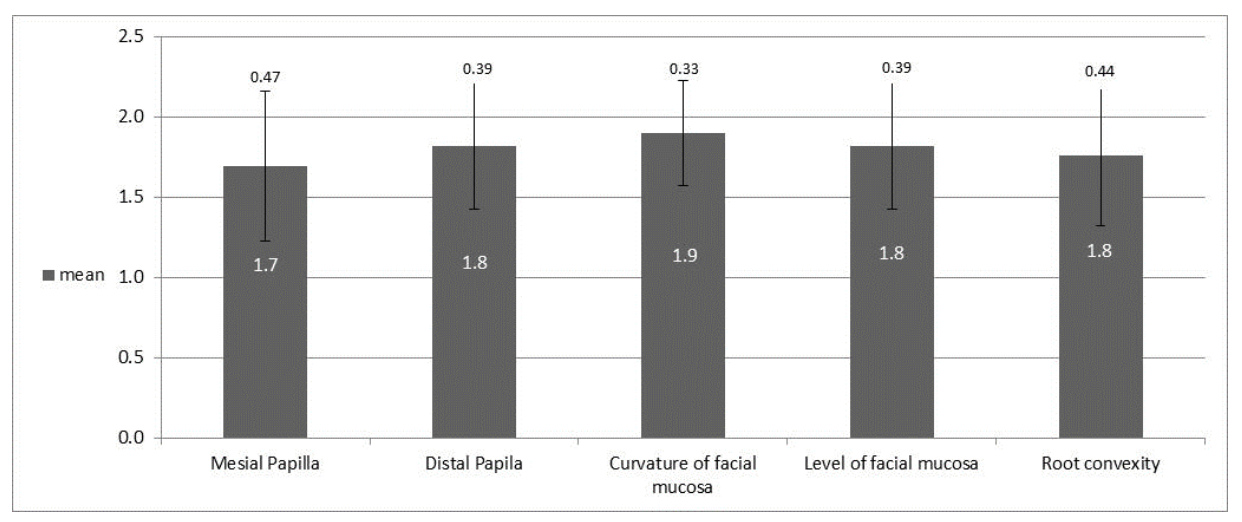
- The presence/absence of mesial papillae
- The presence/absence of the distal papillae
- Curvature contours of the buccal gums
- Height of the buccal gums
- Root convexity/color and soft tissue texture in the buccal aspect of the implant site [15].
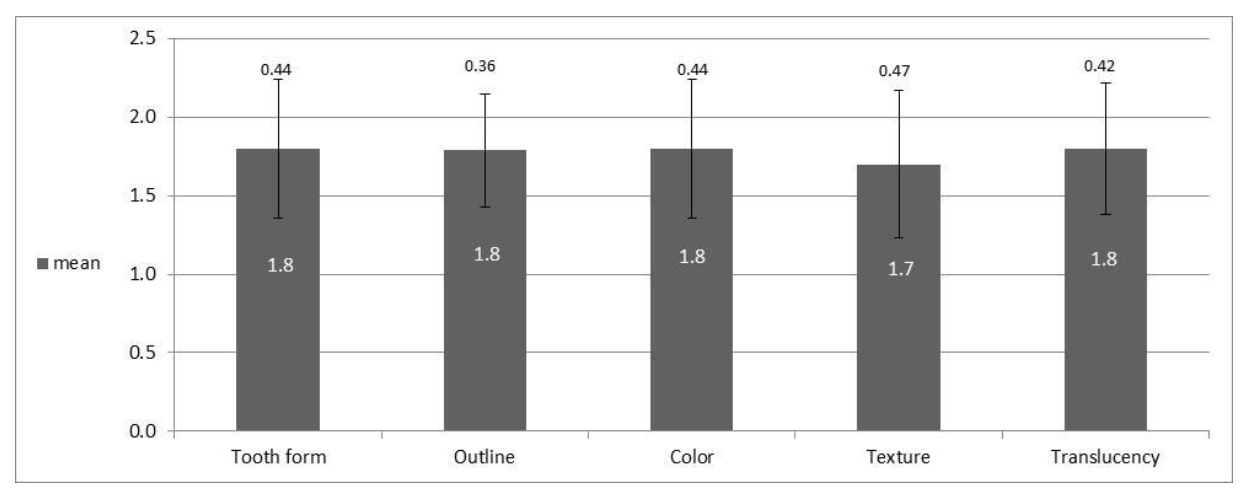
- The shape of the original tooth;
- Outline and volume of the clinical crown;
- A color that includes the evaluation of hue and value indices;
- Surface texture;
- Transparency and characterization.
Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Detailed PES and WES Values of All Patients
3.3. Analysis of Esthetic Results by Index: PES
3.4. Analysis of Esthetic Results by Index: WES
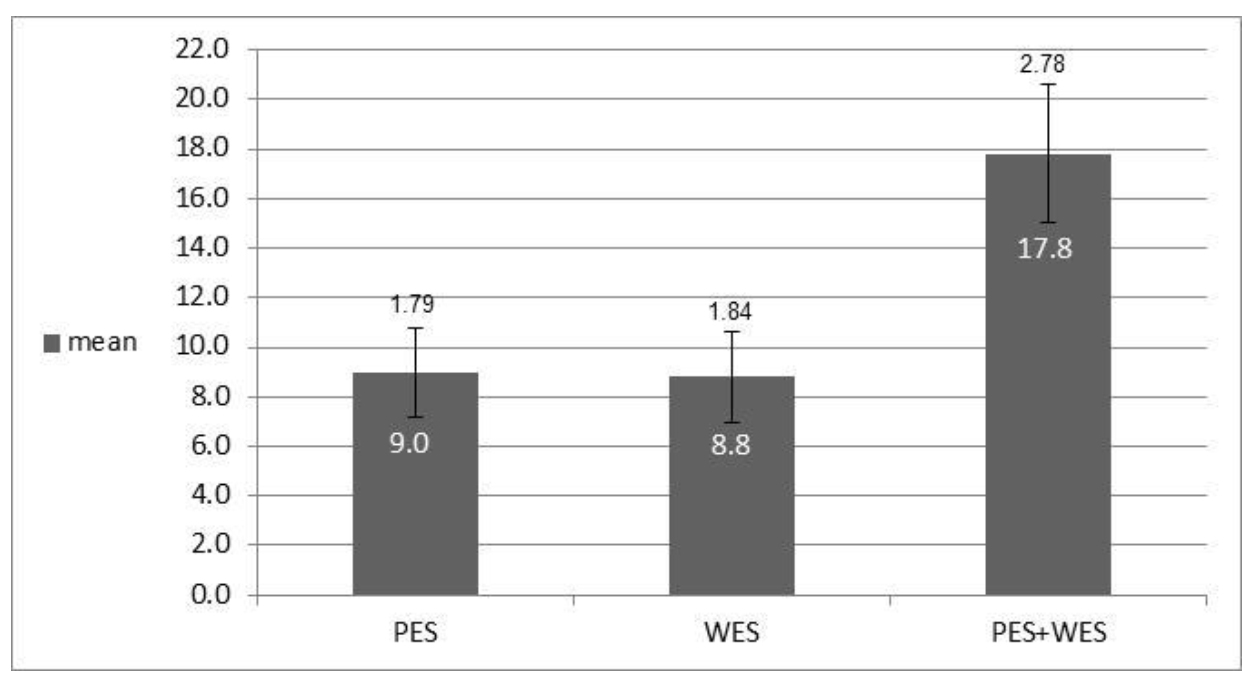
3.5. Analysis of Esthetic Results by Index: PES and WES
3.6. Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yoda, N.; Zheng, K.; Chen, J.; Li, L.; Swain, M.; Sasaki, K.; Li, Q. Bone morphological effects on post-implantation remodeling of maxillary anterior buccal bone: A clinical and biomechanical study. J. Prosthodont. Res. 2017, 61, 393–402. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Martin, W.; Belser, U.C. Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations. Int. J. Oral Maxillofac. Implant. 2004, 19, 43–61. [Google Scholar]
- Nissan, J.; Verted, M.; Gross, O.; Mardinger, O.; Chaushu, G. Histomorphometric analysis following augmentation of the anterior atrophic maxilla with cancellous bone block allograft. Int. J. Oral Maxillofac. Implant. 2020, 27, 84–89. [Google Scholar]
- Nissan, J.; Gross, O.; Mardinger, O.; Ghelfan, O.; Sacco, R.; Chaushu, C. Post-traumatic implant-supported restoration of the anterior maxillary teeth using cancellous bone block allografts. J. Oral Maxillofac. Surg. 2011, 69, 513–518. [Google Scholar] [CrossRef]
- Tolstunov, L. Implant Zones of the Jaws: Implant Location and Related Success Rate. J. Oral Implantol. 2007, 33, 211–220. [Google Scholar] [CrossRef]
- Jensen, J.; Sindet-Pedersen, S. Autogenous mandibular bone grafts and osseointegrated implants for reconstruction of the severely atrophied maxilla: A preliminary report. J. Oral Maxillofac. Surg. 1991, 49, 1277–1287. [Google Scholar] [CrossRef]
- Baldwin, P.; Li, D.; Auston, D.A.; Mir, H.; Yoon, H.; Koval, K.J. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. J. Orthop. Trauma 2019, 33, 203–213. [Google Scholar] [CrossRef]
- Nissan, J.; Mardinger, O.; Calderon, S.; Romanos, G.E.; Chaushu, G. Cancellous Bone Block Allografts for the Augmentation of the Anterior Atrophic Maxilla. Clin. Implant Dent. Relat. Res. 2011, 13, 104–111. [Google Scholar] [CrossRef]
- Nissan, J.; Mardinger, O.; Strauss, M.; Peleg, M.; Sacco, R.; Chaushu, G. Implant-supported restoration of congenitally missing teeth using cancellous bone block-allografts. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2011, 111, 286–291. [Google Scholar] [CrossRef]
- McAllister, B.S.; Haghighat, K. Bone Augmentation Techniques. J. Periodontol. 2007, 78, 377–396. [Google Scholar] [CrossRef]
- Wittneben, J.G.; Buser, D.; Belser, U.C.; Brägger, U. Peri-implant Soft Tissue Conditioning with Provisional Restorations in the Esthetic Zone: The Dynamic Compression Technique. Int. J. Periodontics Restor. Dent. 2013, 33, 447–455. [Google Scholar] [CrossRef]
- Grunder, U.; Gracis, S.; Capelli, M. Influence of the 3-D bone-to-implant relationship on esthetics. Int. J. Periodontics Restor. Dent. 2005, 25, 113–119. [Google Scholar]
- Esposito, M.; Hirsch, J.M.; Lekholm, U.; Thomsen, P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur. J. Oral Sci. 1998, 106, 527–551. [Google Scholar] [CrossRef]
- Cho, H.L.; Lee, J.K.; Um, H.S.; Chang, B.S. Esthetic evaluation of maxillary single-tooth implants in the esthetic zone. J. Periodontal Implant Sci. 2010, 40, 188–193. [Google Scholar] [CrossRef]
- Belser, U.C.; Grütter, L.; Vailati, F.; Bornstein, M.; Weber, H.P.; Buser, D. Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores. J. Periodontol. 2009, 80, 140–151. [Google Scholar] [CrossRef]
- Yildiz, P.; Zortuk, M.; Kiliç, E.; Dinçel, M.; Albayrak, H. Clinical outcomes after immediate and late implant loading for a single missing tooth in the anterior maxilla. Implant Dent. 2016, 25, 504–509. [Google Scholar] [CrossRef]
- Gapski, R.; Wang, H.L.; Mascarenhas, P.; Lang, N.P. Critical review of immediate implant loading. Clin. Oral Implant. Res. 2003, 14, 515–527. [Google Scholar] [CrossRef]
- Den Hartog, L.; Huddleston Slater, J.J.R.; Vissink, A.; Meijer, H.J.A.; Raghoebar, G.M. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: A systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. J. Clin. Periodontol. 2008, 35, 1073–1086. [Google Scholar] [CrossRef]
- D’Addona, A.; Ghassemian, M.; Raffaelli, L.; Manicone, P.F. Soft and hard tissue management in implant therapy-Part I: Surgical concepts. Int. J. Biomater. 2012, 2012, 1687–8787. [Google Scholar] [CrossRef][Green Version]
- Belser, U.C.; Med, P.; Bruno, D.; Higginbottom, D.M.D.F. Outcome Analysis of Implant Restorations Located in the Anterior Maxilla: A Review of the Recent Literature. Int. J. Oral Maxillofac. Implant. 2004, 19, 30–42. [Google Scholar]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Cardaropoli, G.; Wennstro, J.L. Tissue alterations at implant-supported single-tooth replacements: A 1-year prospective clinical study. Clin. Oral Implant. Res. 2006, 17, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Spray, J.R.; Black, C.G.; Morris, H.F.; Ochi, S. The Influence of Bone Thickness on Facial Marginal Bone Response: Stage 1 Placement Through Stage 2 Uncovering. Ann. Periodontol. 2000, 5, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Jurczyk, K.; Belser, U.; Sculean, A. The Management of Peri-implant Mucosa Deficiencies in Esthetic Sites: Case Report of a Combined Surgical-Prosthetic Approach. Int. J. Periodontics Restor. Dent. 2017, 37, 809–817. [Google Scholar] [CrossRef]
- Gross, M.D.; Nissan, J.; Samuel, R. Stress distribution around maxillary implants in anatomic photoelastic models of varying geometry. Part I. J. Prosthet. Dent. 2001, 85, 442–449. [Google Scholar] [CrossRef]
- Fürhauser, R.; Florescu, D.; Benesch, T.; Haas, R.; Mailath, G.; Watzek, G. Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score. Clin. Oral Implant. Res. 2005, 16, 639–644. [Google Scholar] [CrossRef]
- Yildiz, P.; Zortuk, M.; Kilic, E.; Dincel, M.; Albayrak, H. Esthetic outcomes after immediate and late implant loading for a single missing tooth in the anterior maxilla. Niger. J. Clin. Pract. 2018, 21, 1164–1170. [Google Scholar]
- Mangano, F.G.; Mastrangelo, P.; Luongo, F.; Blay, A.; Tunchel, S.M.C. Aesthetic outcome of immediately restored single implants placed in extraction sockets and healed sites of the anterior maxilla: A retrospective study on 103 patients with 3 years of follow-up. Clin. Oral Implant. Res. 2016, 28, 272–282. [Google Scholar] [CrossRef]
- Kolerman, R.; Nissan, J.; Mijiritsky, E.; Hamoudi, N.; Mangano, C.; Tal, H. Esthetic assessment of immediately restored implants combined with GBR and free connective tissue graft. Clin. Oral Implant. Res. 2016, 27, 1414–1422. [Google Scholar] [CrossRef]


| Patient | Implant Site | PES | WES | Total | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mesial Papilla | Distal Papilla | Curvature of Facial Mucosa | Level of Facial Mucosa | Root Convexity | Total | Tooth Form | Outline | Color | Texture | Translucency | Total | |||
| 1 | 11 | 1 | 1 | 1 | 1 | 1 | 5 | 2 | 2 | 2 | 2 | 2 | 10 | 15 |
| 2 | 11 | 1 | 1 | 1 | 1 | 1 | 5 | 2 | 2 | 2 | 2 | 2 | 10 | 15 |
| 3 | 12 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 4 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 5 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 6 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 7 | 11 | 1 | 1 | 1 | 1 | 1 | 5 | 1 | 2 | 1 | 1 | 2 | 7 | 12 |
| 8 | 11 | 1 | 1 | 1 | 1 | 1 | 5 | 2 | 2 | 2 | 2 | 2 | 10 | 15 |
| 9 | 11 | 2 | 2 | 2 | 2 | 1 | 9 | 2 | 2 | 2 | 2 | 2 | 10 | 19 |
| 10 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 11 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 12 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 13 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 1 | 1 | 1 | 1 | 1 | 5 | 15 |
| 14 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 1 | 2 | 1 | 1 | 1 | 6 | 16 |
| 15 | 11 | 2 | 2 | 2 | 2 | 1 | 9 | 1 | 2 | 1 | 1 | 1 | 6 | 15 |
| 16 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 17 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 1 | 2 | 9 | 19 |
| 18 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 19 | 21 | 1 | 1 | 2 | 1 | 1 | 6 | 1 | 1 | 2 | 1 | 1 | 6 | 12 |
| 20 | 11 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 21 | 21 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 22 | 22 | 1 | 2 | 2 | 2 | 2 | 9 | 1 | 1 | 1 | 1 | 1 | 5 | 14 |
| 23 | 12 | 1 | 2 | 2 | 2 | 2 | 9 | 2 | 2 | 1 | 2 | 2 | 9 | 18 |
| 24 | 22 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 25 | 12 | 2 | 2 | 2 | 2 | 2 | 10 | 1 | 1 | 1 | 1 | 1 | 5 | 15 |
| 26 | 21 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 1 | 2 | 9 | 19 |
| 27 | 22 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 1 | 2 | 9 | 19 |
| 28 | 12 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 29 | 23 | 1 | 1 | 2 | 1 | 1 | 6 | 1 | 1 | 1 | 2 | 1 | 6 | 12 |
| 30 | 22 | 1 | 2 | 2 | 2 | 2 | 9 | 2 | 2 | 2 | 2 | 2 | 10 | 19 |
| 31 | 12 | 1 | 2 | 2 | 2 | 2 | 9 | 2 | 2 | 2 | 2 | 2 | 10 | 19 |
| 32 | 22 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| 33 | 12 | 2 | 2 | 2 | 2 | 2 | 10 | 2 | 2 | 2 | 2 | 2 | 10 | 20 |
| Mean | 1.7 | 1.8 | 1.9 | 1.8 | 1.8 | 9 | 1.8 | 1.8 | 1.8 | 1.7 | 1.8 | 8.8 | 17.8 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naishlos, S.; Zenziper, E.; Zelikman, H.; Nissan, J.; Mizrahi, S.; Chaushu, G.; Matalon, S.; Chaushu, L. Esthetic Assessment Succeeding Anterior Atrophic Maxilla Augmentation with Cancellous Bone-Block Allograft and Late Restoration Loading. J. Clin. Med. 2021, 10, 4635. https://doi.org/10.3390/jcm10204635
Naishlos S, Zenziper E, Zelikman H, Nissan J, Mizrahi S, Chaushu G, Matalon S, Chaushu L. Esthetic Assessment Succeeding Anterior Atrophic Maxilla Augmentation with Cancellous Bone-Block Allograft and Late Restoration Loading. Journal of Clinical Medicine. 2021; 10(20):4635. https://doi.org/10.3390/jcm10204635
Chicago/Turabian StyleNaishlos, Sarit, Eran Zenziper, Helena Zelikman, Joseph Nissan, Shaked Mizrahi, Gavriel Chaushu, Shlomo Matalon, and Liat Chaushu. 2021. "Esthetic Assessment Succeeding Anterior Atrophic Maxilla Augmentation with Cancellous Bone-Block Allograft and Late Restoration Loading" Journal of Clinical Medicine 10, no. 20: 4635. https://doi.org/10.3390/jcm10204635
APA StyleNaishlos, S., Zenziper, E., Zelikman, H., Nissan, J., Mizrahi, S., Chaushu, G., Matalon, S., & Chaushu, L. (2021). Esthetic Assessment Succeeding Anterior Atrophic Maxilla Augmentation with Cancellous Bone-Block Allograft and Late Restoration Loading. Journal of Clinical Medicine, 10(20), 4635. https://doi.org/10.3390/jcm10204635









