Survival and Treatment of Lung Cancer in Taiwan between 2010 and 2016
Abstract
:1. Introduction
2. Patients and Methods
Statistical Analysis
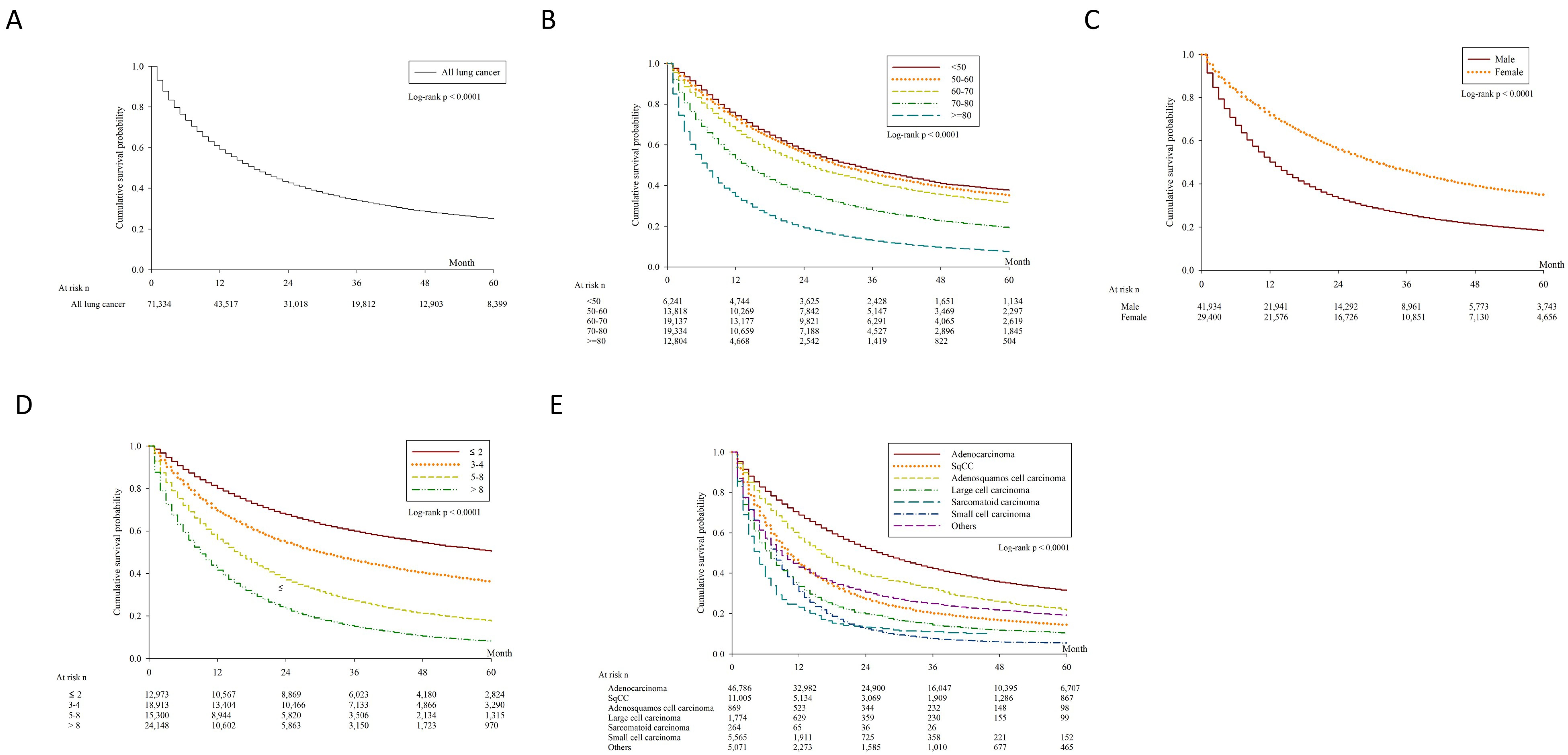
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, Y.-H.; Chiu, C.-H.; Kuo, C.-H.S.; Chou, T.-Y.; Yeh, Y.-C.; Hsu, H.-S.; Yen, S.-H.; Wu, Y.-H.; Yang, J.C.-H.; Liao, B.-C.; et al. Lung Cancer in Republic of China. J. Thorac. Oncol. 2021, 16, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Schabath, M.B.; Cote, M.L. Cancer Progress and Priorities: Lung Cancer. Cancer Epidemiol. Biomark. Prev. 2019, 28, 1563–1579. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allemani, C.; Matsuda, T.; Di Carlo, V.; Harewood, R.; Matz, M.; Nikšić, M.; Bonaventure, A.; Valkov, M.; Johnson, C.J.; Estève, J.; et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): Analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 2018, 391, 1023–1075. [Google Scholar] [CrossRef] [Green Version]
- Wang, B.-Y.; Huang, J.-Y.; Cheng, C.-Y.; Lin, C.-H.; Ko, J.-L.; Liaw, Y.-P. Lung Cancer and Prognosis in Taiwan: A Population-Based Cancer Registry. J. Thorac. Oncol. 2013, 8, 1128–1135. [Google Scholar] [CrossRef] [Green Version]
- Ministry of Health and Welfare, Taiwan. Cause of Death Statistics. Available online: https://www.mohw.gov.tw/lp-4650-2.html (accessed on 1 October 2020).
- Youlden, D.R.; Cramb, S.; Baade, P. The International Epidemiology of Lung Cancer: Geographical Distribution and Secular Trends. J. Thorac. Oncol. 2008, 3, 819–831. [Google Scholar] [CrossRef]
- Vallières, E.; Shepherd, F.A.; Crowley, J.; Van Houtte, P.; Postmus, P.; Carney, D.; Chansky, K.; Shaikh, Z.; Goldstraw, P. The IASLC Lung Cancer Staging Project: Proposals Regarding the Relevance of TNM in the Pathologic Staging of Small Cell Lung Cancer in the Forthcoming (Seventh) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2009, 4, 1049–1059. [Google Scholar] [CrossRef]
- Goldstraw, P.; Chansky, K.; Crowley, J.; Rami-Porta, R.; Asamura, H.; Eberhardt, W.E.; Nicholson, A.G.; Groome, P.; Mitchell, A.; Bolejack, V.; et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J. Thorac. Oncol. 2016, 11, 39–51. [Google Scholar] [CrossRef] [Green Version]
- Chiang, C.-J.; You, S.-L.; Chen, C.-J.; Yang, Y.-W.; Lo, W.-C.; Lai, M.-S. Quality assessment and improvement of nationwide cancer registration system in Taiwan: A review. Jpn. J. Clin. Oncol. 2015, 45, 291–296. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- The National Lung Screening Trial Research Team; Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D.; Fagerstrom, R.M.; Gareen, I.F.; Gatsonis, C.; Marcus, P.M.; et al. Reduced Lung-Cancer Mortality with Low-Dose Computed Tomographic Screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Koning, H.J.; Van Der Aalst, C.M.; De Jong, P.A.; Scholten, E.T.; Nackaerts, K.; Heuvelmans, M.A.; Lammers, J.-W.J.; Weenink, C.; Yousaf-Khan, U.; Horeweg, N.; et al. Reduced Lung-Cancer Mortality with Volume CT Screening in a Randomized Trial. N. Engl. J. Med. 2020, 382, 503–513. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, F.R.; Scagliotti, G.V.; Mulshine, J.L.; Kwon, R.; Curran, W.J.; Wu, Y.-L.; Paz-Ares, L. Lung cancer: Current therapies and new targeted treatments. Lancet 2017, 389, 299–311. [Google Scholar] [CrossRef]
- Forde, P.M.; Kelly, R.J.; Brahmer, J.R. New Strategies in Lung Cancer: Translating Immunotherapy into Clinical Practice. Clin. Cancer Res. 2014, 20, 1067–1073. [Google Scholar] [CrossRef] [Green Version]
- Alexander, M.; Kim, S.Y.; Cheng, H. Update 2020: Management of Non-Small Cell Lung Cancer. Lung 2020, 198, 897–907. [Google Scholar] [CrossRef]
- Riaz, S.P.; Linklater, K.M.; Page, R.; Peake, M.D.; Møller, H.; Lüchtenborg, M. Recent trends in resection rates among non-small cell lung cancer patients in England. Thorax 2012, 67, 811–814. [Google Scholar] [CrossRef] [Green Version]
- Helminen, O.; Valo, J.; Andersén, H.; Lautamäki, A.; Vuohelainen, V.; Sihvo, E. Real-world guideline-based treatment of lung cancer improves short- and long-term outcomes and resection rate: A population-based study. Lung Cancer 2020, 140, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gunn, J.; Valo, J.; Sipilä, J.; Rautava, P.; Sihvo, E.; Kytö, V. Trends and results of lung cancer surgery in Finland between 2004 and 2014†. Eur. J. Cardio-Thoracic Surg. 2018, 54, 127–133. [Google Scholar] [CrossRef] [Green Version]
- Ginsberg, R.J.; Rubinstein, L.V. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Ann. Thorac. Surg. 1995, 60, 615–623. [Google Scholar] [CrossRef]
- Wood, D.E.; Kazerooni, E.A.; Baum, S.L.; Eapen, G.A.; Ettinger, D.S.; Hou, L.; Jackman, D.M.; Klippenstein, D.; Kumar, R.; Lackner, R.P.; et al. Lung Cancer Screening, Version 3.2018, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Cancer Netw. 2018, 16, 412–441. [Google Scholar] [CrossRef]
- Narsule, C.K.; Ebright, M.; Fernando, H. Sublobar Versus Lobar Resection. Cancer J. 2011, 17, 23–27. [Google Scholar] [CrossRef] [PubMed]
- Altorki, N.; Kohman, L.J.; Veit, L.J.; You, Y.N.; Boughey, J.C. Limited resection as a cure for early lung cancer: Time to challenge the gold standard? Bull. Am. Coll. Surg. 2015, 100, 57–58. [Google Scholar] [PubMed]
- Blasberg, J.D.; Pass, H.I.; Donington, J.S. Sublobar Resection: A Movement from the Lung Cancer Study Group. J. Thorac. Oncol. 2010, 5, 1583–1593. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakamura, K.; Saji, H.; Nakajima, R.; Okada, M.; Asamura, H.; Shibata, T.; Nakamura, S.; Tada, H.; Tsuboi, M. A Phase III Randomized Trial of Lobectomy Versus Limited Resection for Small-sized Peripheral Non-small Cell Lung Cancer (JCOG0802/WJOG4607L). Jpn. J. Clin. Oncol. 2009, 40, 271–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gadgeel, S.M.; Ramalingam, S.; Cummings, G.; Kraut, M.J.; Wozniak, A.J.; Gaspar, L.E.; Kalemkerian, G.P. Lung Cancer in Patients < 50 Years of Age: The experience of an academic multidisciplinary program. Chest 1999, 115, 1232–1236. [Google Scholar] [CrossRef] [PubMed]
- Radzikowska, E.; Roszkowski, K.; Głaz, P. Lung cancer in patients under 50 years old. Lung Cancer 2001, 33, 203–211. [Google Scholar] [CrossRef]
- Subramanian, J.; Morgensztern, D.; Goodgame, B.; Baggstrom, M.Q.; Gao, F.; Piccirillo, J.; Govindan, R. Distinctive Characteristics of Non-small Cell Lung Cancer (NSCLC) in the Young: A Surveillance, Epidemiology, and End Results (SEER) Analysis. J. Thorac. Oncol. 2010, 5, 23–28. [Google Scholar] [CrossRef] [Green Version]
- Foeglé, J.; Hédelin, G.; Lebitasy, M.-P.; Purohit, A.; Velten, M.; Quoix, E. Specific Features of Non-small Cell Lung Cancer in Women: A Retrospective Study of 1738 Cases Diagnosed in Bas-Rhin between 1982 and 1997. J. Thorac. Oncol. 2007, 2, 466–474. [Google Scholar] [CrossRef] [Green Version]
- Asamura, H.; Goya, T.; Koshiishi, Y.; Sohara, Y.; Eguchi, K.; Mori, M.; Nakanishi, Y.; Tsuchiya, R.; Shimokata, K.; Inoue, H.; et al. A Japanese Lung Cancer Registry Study: Prognosis of 13,010 Resected Lung Cancers. J. Thorac. Oncol. 2008, 3, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Cheng, T.-Y.D.; Cramb, S.; Baade, P.; Youlden, D.; Nwogu, C.; Reid, M.E. The International Epidemiology of Lung Cancer: Latest Trends, Disparities, and Tumor Characteristics. J. Thorac. Oncol. 2016, 11, 1653–1671. [Google Scholar] [CrossRef] [Green Version]
- Jemal, A.; Miller, K.D.; Ma, J.; Siegel, R.L.; Fedewa, S.A.; Islami, F.; Devesa, S.S.; Thun, M.J. Higher Lung Cancer Incidence in Young Women Than Young Men in the United States. N. Engl. J. Med. 2018, 378, 1999–2009. [Google Scholar] [CrossRef]
- Kawaguchi, T.; Takada, M.; Kubo, A.; Matsumura, A.; Fukai, S.; Tamura, A.; Saito, R.; Maruyama, Y.; Kawahara, M.; Ou, S.-H.I. Performance Status and Smoking Status Are Independent Favorable Prognostic Factors for Survival in Non-small Cell Lung Cancer: A Comprehensive Analysis of 26,957 Patients with NSCLC. J. Thorac. Oncol. 2010, 5, 620–630. [Google Scholar] [CrossRef] [Green Version]
- Chansky, K.; Sculier, J.-P.; Crowley, J.J.; Giroux, D.; Van Meerbeeck, J.; Goldstraw, P. The International Association for the Study of Lung Cancer Staging Project: Prognostic Factors and Pathologic TNM Stage in Surgically Managed Non-small Cell Lung Cancer. J. Thorac. Oncol. 2009, 4, 792–801. [Google Scholar] [CrossRef] [Green Version]
- Wang, B.-Y.; Huang, J.-Y.; Chen, H.-C.; Lin, C.-H.; Lin, S.-H.; Hung, W.-H.; Cheng, Y.-F. The comparison between adenocarcinoma and squamous cell carcinoma in lung cancer patients. J. Cancer Res. Clin. Oncol. 2019, 146, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Rice, T.W.; Blackstone, E.H.; Rusch, V. 7th Edition of the AJCC Cancer Staging Manual: Esophagus and Esophagogastric Junction. Ann. Surg. Oncol. 2010, 17, 1721–1724. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Brambilla, E.; Noguchi, M.; Nicholson, A.G.; Geisinger, K.R.; Yatabe, Y.; Beer, D.G.; Powell, C.; Riely, G.J.; Van Schil, P.E.; et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society International Multidisciplinary Classification of Lung Adenocarcinoma. J. Thorac. Oncol. 2011, 6, 244–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoshizawa, A.; Motoi, N.; Riely, G.J.; Sima, C.S.; Gerald, W.L.; Kris, M.; Park, B.J.; Rusch, V.; Travis, W.D. Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: Prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod. Pathol. 2011, 24, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Butnor, K.J. Controversies and challenges in the histologic subtyping of lung adenocarcinoma. Transl. Lung Cancer Res. 2020, 9, 839–846. [Google Scholar] [CrossRef]
- Tang, E.R.; Schreiner, A.M.; Pua, B.B. Advances in lung adenocarcinoma classification: A summary of the new international multidisciplinary classification system (IASLC/ATS/ERS). J. Thorac. Dis. 2014, 6, S489–S501. [Google Scholar] [CrossRef]


| Variable | Number of Patients | 5-Year Survival(%, 95% C.I.) | Median Survival Time(Months, 95% C.I.) | p |
|---|---|---|---|---|
| All | 71,334 | 25.00 (24.64–25.35) | 25.27 (24.62–25.92) | |
| Age (years) | <0.0001 | |||
| <50 | 6241 | 37.59 (36.26–38.92) | 33.28 (31.72–34.85) | |
| 50–60 | 13,818 | 35.07 (34.18–35.96) | 30.45 (29.52–31.38) | |
| 60–70 | 19,137 | 31.35 (30.60–32.09) | 25.27 (24.62–25.92) | |
| 70–80 | 19,334 | 19.28 (18.66–19.90) | 14.51 (14.08–14.94) | |
| ≥80 | 12,804 | 7.46 (6.96–7.99) | 7.26 (7.03–7.48) | |
| Sex | <0.0001 | |||
| Male | 41,934 | 18.23 (17.82–18.64) | 13.02 (12.79–13.26) | |
| Female | 29,400 | 34.71 (34.10–35.33) | 31.08 (30.36–31.80) | |
| CCI | <0.0001 | |||
| ≤2 | 12,973 | 50.35 (49.38–51.32) | 61.62 (58.57–64.66) | |
| 3–4 | 18,913 | 36.04 (35.28–36.80) | 30.61 (29.56–31.66) | |
| 5–8 | 15,300 | 17.55 (16.87–18.23) | 16.15 (15.70–16.60) | |
| >8 | 24,148 | 8.01 (7.63–8.41) | 9.74 (9.54–9.94) | |
| Cell type | <0.0001 | |||
| Adenocarcinoma | 46,786 | 31.25 (30.77–31.72) | 27.08 (26.60–27.55) | |
| SqCC | 11,005 | 14.33 (13.62–15.04) | 10.77 (10.47–11.07) | |
| Adenosquamous cell carcinoma | 869 | 21.58 (18.59–24.72) | 16.75 (15.14–18.36) | |
| Large cell carcinoma | 1774 | 10.12 (8.67–11.70) | 7.28 (6.67–7.89) | |
| Sarcomatoid carcinoma | 264 | 9.16 (6.02–13.09) | 5.12 (4.18–6.05) | |
| Small cell carcinoma | 5565 | 5.31 (4.69–5.98) | 8.35 (8.11–8.59) | |
| Others or unknown | 5071 | 19.04 (17.87–20.24) | 9.43 (8.90–9.97) | |
| Clinical T | <0.0001 | |||
| 1a | 7464 | 74.11 (72.95–75.23) | Not estimated | |
| 1b | 5880 | 49.72 (48.27–51.16) | 60.19 (57.94–62.44) | |
| 2a | 11,903 | 33.10 (32.16–34.05) | 29.91 (29.00–30.82) | |
| 2b | 3427 | 15.37 (14.05–16.75) | 14.34 (13.29–15.38) | |
| 3 | 10,717 | 13.40 (12.69–14.14) | 12.93 (12.56–13.29) | |
| 4 | 26,755 | 7.93 (7.56–8.32) | 10.69 (10.48–10.90) | |
| X | 2859 | 33.80 (31.85–35.77) | 20.31 (18.13–22.50) | |
| Missing | 2329 | 24.48 (22.64–26.35) | 16.98 (14.83–19.13) | |
| Clinical N | <0.0001 | |||
| 0 | 22,510 | 53.77 (53.03–54.50) | 72.44 (70.55–74.34) | |
| 1 | 5194 | 22.18 (20.93–23.46) | 20.29 (19.27–21.31) | |
| 2 | 17,145 | 11.48 (10.94–12.03) | 13.61 (13.29–13.92) | |
| 3 | 23,039 | 6.56 (6.19–6.94) | 9.93 (9.73–10.12) | |
| X | 2742 | 32.71 (30.75–34.69) | 19.10 (16.53–21.67) | |
| Missing | 704 | 41.43 (37.63–45.18) | 31.01 (22.91–39.11) | |
| Clinical M | <0.0001 | |||
| 0 | 28,915 | 49.92 (49.28–50.56) | 60.46 (59.21–61.72) | |
| 1A | 13,726 | 10.38 (9.80–10.99) | 13.73 (13.34–14.11) | |
| 1B | 27,393 | 4.68 (4.39–4.99) | 9.50 (9.32–9.68) | |
| B | 816 | 80.67 (77.04–83.79) | Not estimated | |
| Missing | 484 | 28.91 (24.74–33.21) | 14.33 (11.94–16.73) | |
| Clinical stage | ||||
| IA | 9208 | 81.77 (80.80–82.70) | Not estimated | |
| IB | 4087 | 63.13 (61.41–64.79) | 94.34 (88.00–100.67) | |
| IIA | 1702 | 48.78 (46.10–51.41) | 57.74 (46.73–68.75) | |
| IIB | 1454 | 41.55 (38.75–44.32) | 41.17 (38.29–44.05) | |
| IIIA | 5309 | 28.59 (27.26–29.94) | 25.49 (24.40–26.59) | |
| IIIB | 6316 | 15.32 (14.33–16.34) | 14.83 (14.30–15.36) | |
| IV | 41,458 | 6.65 (6.37–6.94) | 10.70 (10.53–10.87) | |
| BBB | 811 | 80.96 (77.33–84.08) | Not estimated | |
| Unknown | 989 | 61.10 (57.77–64.26) | Not estimated | |
| Grade | <0.0001 | |||
| Well differentiated | 5056 | 71.24 (69.83–72.60) | Not estimated | |
| Moderately differentiated | 17,163 | 45.63 (44.78–46.47) | 49.77 (47.73–51.82) | |
| Poorly differentiated | 13,520 | 20.27 (19.50–21.06) | 14.74 (14.27–15.21) | |
| Undifferentiated | 434 | 23.27 (19.17–27.62) | 12.30 (10.26–14.34) | |
| Missing | 35,161 | 10.39 (10.04–10.76) | 11.98 (11.78–12.19) | |
| Treatment | <0.0001 | |||
| Any treatment | 65,436 | 27.09 (26.71–27.47) | 21.28 (20.97–21.58) | |
| Chemotherapy | 35,705 | 17.77 (17.34–18.21) | 15.37 (15.12–15.62) | |
| Surgery | 20,131 | 69.93 (69.19–70.66) | Not estimated | |
| Radiotherapy | 20,312 | 10.79 (10.32–11.28) | 12.51 (12.26–12.77) | |
| Target therapy | 18,914 | 12.62 (12.05–13.21) | 19.10 (18.74–19.46) | |
| Surgical method | <0.0001 | |||
| No surgery | 51,203 | 7.70 (7.43–7.97) | 11.29 (11.13–11.44) | |
| Pneumonectomy | 171 | 43.99 (35.99–51.69) | 39.55 (35.98–43.11) | |
| Bilobectomy | 172 | 53.67 (45.56–61.09) | 74.77 (68.17–81.38) | |
| Lobectomy | 13,713 | 71.16 (70.29–72.01) | Not estimated | |
| Segmentectomy | 1375 | 83.37 (80.29–86.01) | Not estimated | |
| Wedge resection | 4537 | 65.72 (64.02–67.36) | 103.30 (101.87–104.73) | |
| Others | 163 | 33.58 (25.83–41.48) | 32.18 (26.26–38.10) |
| Variable | aHR | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Age | |||
| <50 | 0.901 | 0.851–0.955 | 0.0005 |
| 50–60 | 0.906 | 0.867–0.946 | <0.0001 |
| 60–70 (reference) | 1 | ||
| 70–80 | 1.387 | 1.336–1.439 | <0.0001 |
| ≥80 | 1.960 | 1.877–2.046 | <0.0001 |
| Sex | |||
| Male | 1.459 | 1.412–1.506 | <0.0001 |
| Female (reference) | 1 | ||
| Charlson score | |||
| ≤2 | 0.859 | 0.820–0.900 | <0.0001 |
| 3–4 (reference) | 1 | ||
| 5–8 | 1.233 | 1.185–1.283 | <0.0001 |
| >8 | 1.388 | 1.337–1.441 | <0.0001 |
| Cell type | |||
| Adenocarcinoma (reference) | 1 | ||
| SqCC | 1.392 | 1.337–1.448 | <0.0001 |
| Adenosquamous cell carcinoma | 1.552 | 1.397–1.724 | <0.0001 |
| Large cell carcinoma | 1.632 | 1.496–1.781 | <0.0001 |
| Sarcomatoid carcinoma | 2.394 | 1.937–2.960 | <0.0001 |
| Small cell carcinoma | 1.296 | 1.224–1.373 | <0.0001 |
| Others | 1.261 | 1.176–1.352 | <0.0001 |
| Clinical T | |||
| 1A | 1 | ||
| 1B | 1.552 | 1.430–1.684 | <0.0001 |
| 2A | 1.889 | 1.755–2.033 | <0.0001 |
| 2B | 2.331 | 2.134–2.546 | <0.0001 |
| 3 | 2.278 | 2.108–2.461 | <0.0001 |
| 4 | 2.357 | 2.185–2.541 | <0.0001 |
| X | 2.149 | 1.844–2.504 | <0.0001 |
| Clinical N | |||
| 0 | 1 | ||
| 1 | 1.312 | 1.239–1.389 | <0.0001 |
| 2 | 1.503 | 1.438–1.571 | <0.0001 |
| 3 | 1.677 | 1.603–1.754 | <0.0001 |
| X | 1.645 | 1.435–1.885 | <0.0001 |
| Clinical M | |||
| 0 | 1 | ||
| 1A | 1.503 | 1.434–1.576 | <0.0001 |
| 1B | 2.091 | 2.006–2.178 | <0.0001 |
| B | 0.351 | 0.278–0.444 | <0.0001 |
| Differentiation | |||
| Well (reference) | 1 | ||
| Moderate | 1.365 | 1.287–1.447 | <0.0001 |
| Poor | 1.632 | 1.536–1.733 | <0.0001 |
| Undifferentiated | 1.772 | 1.559–2.015 | <0.0001 |
| Surgery | |||
| No (reference) | 1 | ||
| Yes | 0.370 | 0.352–0.389 | <0.0001 |
| Chemotherapy | |||
| No (reference) | 1 | ||
| Yes | 0.812 | 0.784–0.842 | <0.0001 |
| Radiotherapy | |||
| No (reference) | 1 | ||
| Yes | 1.021 | 0.989–1.055 | 0.1983 |
| Target therapy | |||
| No (reference) | 1 | ||
| Yes | 0.651 | 0.623–0.681 | <0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, Y.-J.; Huang, J.-Y.; Lin, C.-H.; Wang, B.-Y. Survival and Treatment of Lung Cancer in Taiwan between 2010 and 2016. J. Clin. Med. 2021, 10, 4675. https://doi.org/10.3390/jcm10204675
Chang Y-J, Huang J-Y, Lin C-H, Wang B-Y. Survival and Treatment of Lung Cancer in Taiwan between 2010 and 2016. Journal of Clinical Medicine. 2021; 10(20):4675. https://doi.org/10.3390/jcm10204675
Chicago/Turabian StyleChang, Yen-Jung, Jing-Yang Huang, Ching-Hsiung Lin, and Bing-Yen Wang. 2021. "Survival and Treatment of Lung Cancer in Taiwan between 2010 and 2016" Journal of Clinical Medicine 10, no. 20: 4675. https://doi.org/10.3390/jcm10204675





