Comparison of the Effects of Normocapnia and Mild Hypercapnia on the Optic Nerve Sheath Diameter and Regional Cerebral Oxygen Saturation in Patients Undergoing Gynecological Laparoscopy with Total Intravenous Anesthesia
Abstract
:1. Introduction
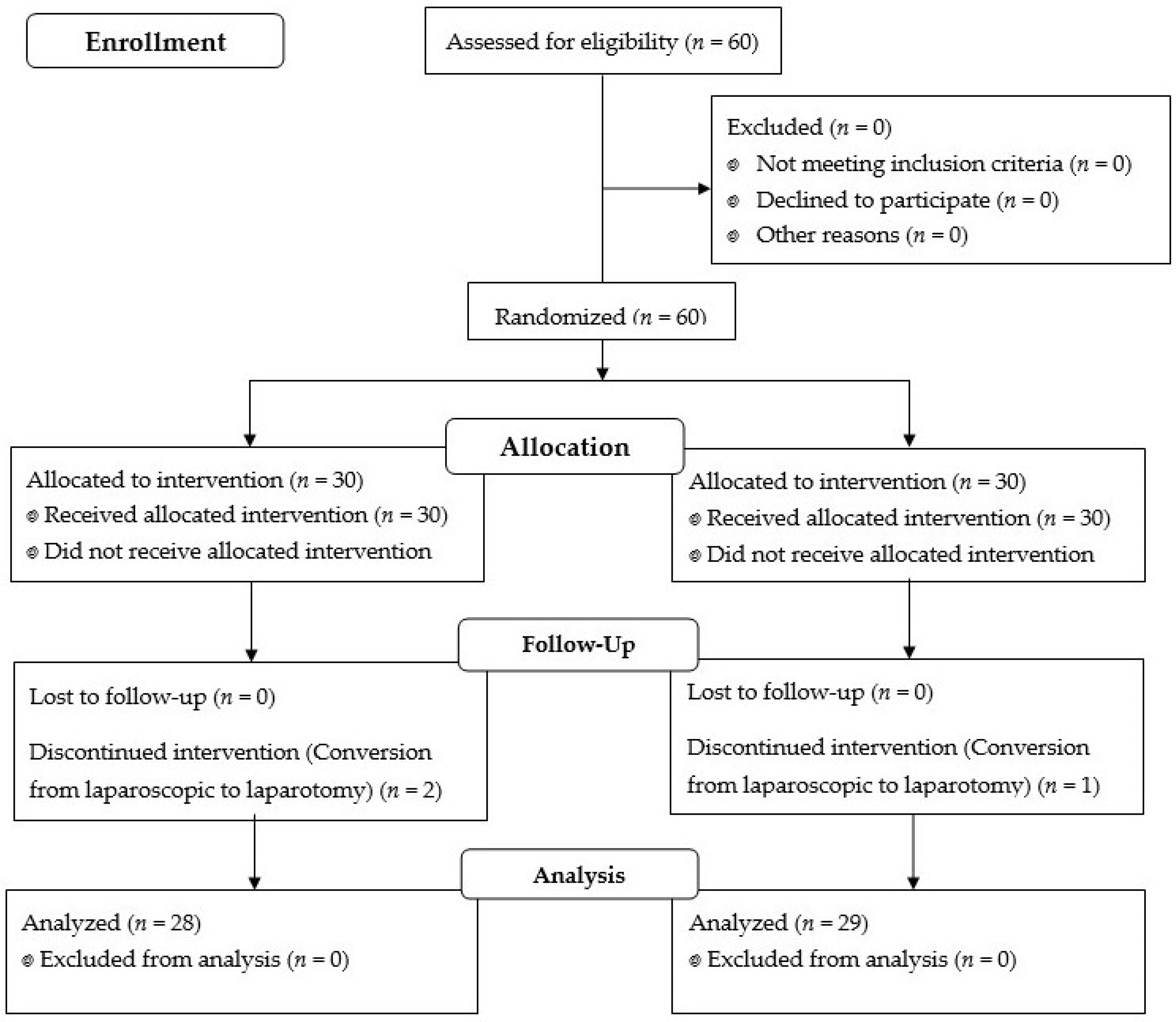
2. Materials and Methods
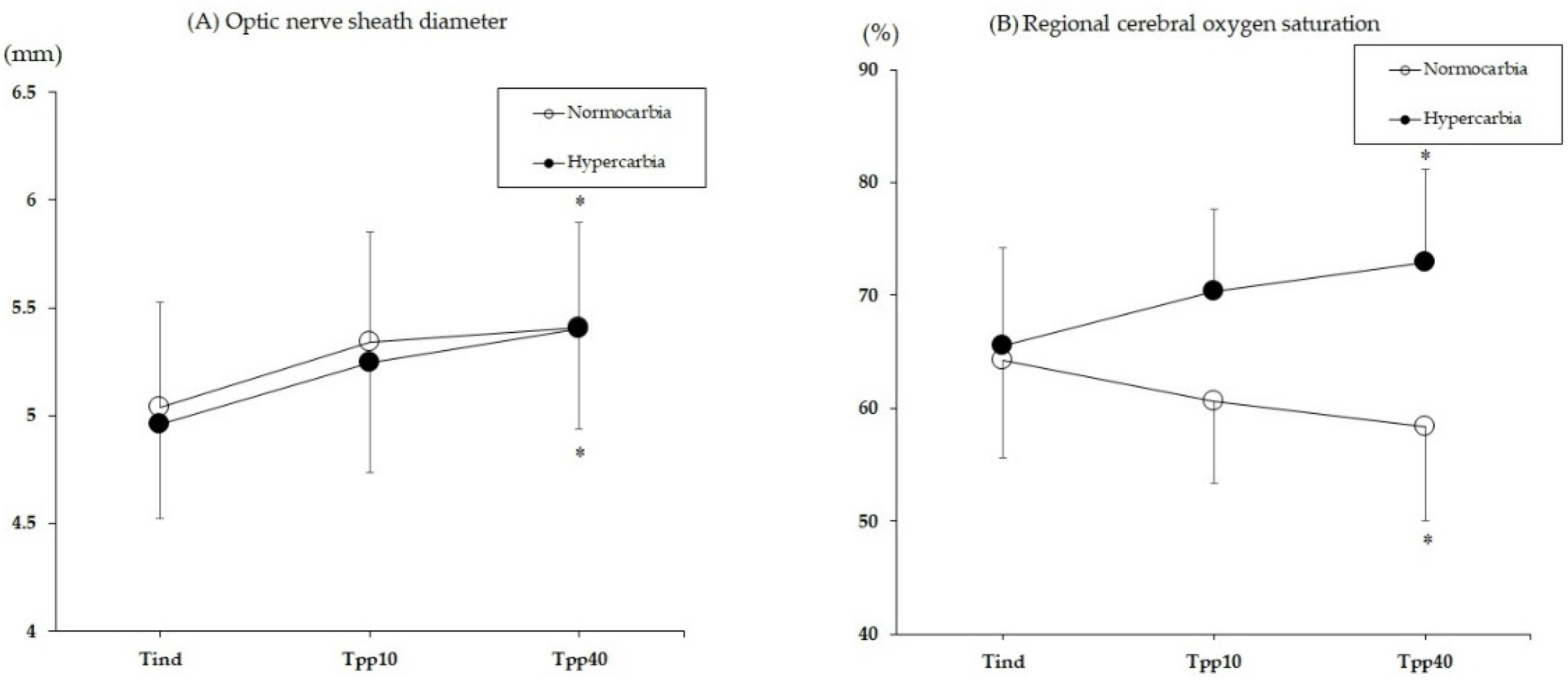
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Huang, D.; Zhou, S.; Yu, Z.; Chen, J.; Xie, H. Lung protective ventilation strategy to reduce postoperative pulmonary complications (PPCs) in patients undergoing robot-assisted laparoscopic radical cystectomy for bladder cancer: A randomized double blinded clinical trial. J. Clin. Anesth. 2021, 71, 110156. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Yang, L.; Yang, J.; Shan, S. Effects of permissive hypercapnia on laparoscopic surgery for rectal carcinoma. Gastroenterol. Res. Pract. 2019, 2019, 3903451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, Q.; Cao, B.; Niu, L.; Cui, X.; Yu, H.; Liu, J.; Li, H.; Li, W. Effects of permissive hypercapnia on transient global cerebral ischemia-reperfusion injury in rats. Anesthesiology 2010, 112, 288–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Este-McDonald, J.R.; Josephs, L.G.; Birkett, D.H.; Hirsch, E.F. Changes in intracranial pressure associated with apneumic retractors. Arch. Surg. 1995, 130, 362–365. [Google Scholar] [CrossRef] [PubMed]
- Moncure, M.; Salem, R.; Moncure, K.; Testaiuti, M.; Marburger, R.; Ye, X.; Brathwaite, C.; Ross, S.E. Central nervous system metabolic and physiologic effects of laparoscopy. Am. Surg. 1999, 65, 168–172. [Google Scholar] [PubMed]
- Kalmar, A.F.; Foubert, L.; Hendrickx, J.F.; Mottrie, A.; Absalom, A.; Mortier, E.P.; Struys, M.M.R.F. Influence of steep Trendelenburg position and CO2 pneumoperitoneum on cardiovascular, cerebrovascular, and respiratory homeostasis during robotic prostatectomy. Br. J. Anaesth. 2010, 104, 433–439. [Google Scholar] [CrossRef] [Green Version]
- Goetz, C.G. Textbook of Clinical Neurology, 2nd ed.; Elsevier: Chicago, IL, USA, 2003; pp. 511–529. [Google Scholar]
- Robba, C.; Cardim, D.; Donnelly, J.; Bertuccio, A.; Bacigaluppi, S.; Bragazzi, N.; Cabella, B.; Liu, X.; Matta, B.; Lattuada, M.; et al. Effects of pneumoperitoneum and Trendelenburg position on intracranial pressure assessed using different non-invasive methods. Br. J. Anaesth. 2016, 117, 783–791. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, M.S.; Bai, S.J.; Lee, J.R.; Choi, Y.D.; Kim, Y.J.; Choi, S.H. Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep Trendelenburg positioning proven by ultrasonographic measurement of optic nerve sheath diameter. J. Endourol. 2014, 28, 801–806. [Google Scholar] [CrossRef]
- Lee, J.R.; Lee, P.B.; Do, S.H.; Jeon, Y.T.; Lee, J.M.; Hwang, J.Y.; Han, S.H. The effect of gynaecological laparoscopic surgery on cerebral oxygenation. J. Int. Med. Res. 2006, 34, 531–536. [Google Scholar] [CrossRef] [Green Version]
- McCulloch, T.J.; Visco, E.; Lam, A.M. Graded hypercapnia and cerebral autoregulation during sevoflurane or propofol anesthesia. Anesthesiology 2000, 93, 1205–1209. [Google Scholar] [CrossRef]
- Preethi, J.; Bidkar, P.U.; Cherian, A.; Dey, A.; Srinivasan, S.; Adinarayanan, S.; Ramesh, A.S. Comparison of total intravenous anesthesia vs. inhalational anesthesia on brain relaxation, intracranial pressure, and hemodynamics in patients with acute subdural hematoma undergoing emergency craniotomy: A randomized control trial. Eur. J. Trauma Emerg. Surg. 2021, 47, 831–837. [Google Scholar] [CrossRef]
- Gattinoni, L.; Tonetti, T.; Cressoni, M.; Cadringher, P.; Herrmann, P.; Moerer, O.; Protti, A.; Gotti, M.; Chiurazzi, C.; Carlesso, E.; et al. Ventilator-related causes of lung injury: The mechanical power. Intensive Care Med. 2016, 42, 1567–1575. [Google Scholar] [CrossRef]
- Dietl, P.; Frick, M.; Mair, N.; Bertocchi, C.; Haller, T. Pulmonary consequences of a deep breath revisited. Biol. Neonate 2004, 85, 299–304. [Google Scholar] [CrossRef]
- Dinsmore, M.; Han, J.S.; Fisher, J.A.; Chan, V.W.; Venkatraghavan, L. Effects of acute controlled changes in end-tidal carbon dioxide on the diameter of the optic nerve sheath: A transorbital ultrasonographic study in healthy volunteer. Anaesthesia 2017, 72, 618–623. [Google Scholar] [CrossRef]
- In, J.; Kang, H.; Kim, J.H.; Kim, T.K.; Ahn, E.J.; Lee, D.K.; Lee, S.; Park, J.H. Tips for troublesome sample-size calculation. Korean J. Anesthesiol. 2020, 73, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Hong, J.H.; Park, J.Y.; Hwang, J.H.; Cho, S.S.; Kim, Y.K. Propofol attenuates the increase of sonographic optic nerve sheath diameter during robot-assisted laparoscopic prostatectomy: A randomized clinical trial. BMC Anesthesiol. 2018, 18, 72. [Google Scholar] [CrossRef] [Green Version]
- Wong, C.; Churilov, L.; Cowie, D.; Tan, C.O.; Hu, R.; Tremewen, D.; Pearce, B.; Pillai, P.; Karalapillai, D.; Bellomo, R.; et al. Randomised controlled trial to investigate the relationship between mild hypercapnia and cerebral oxygen saturation in patients undergoing major surgery. BMJ Open 2020, 10, e029159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murphy, G.S.; Szokol, J.W.; Avram, M.J.; Greenberg, S.B.; Shear, T.D.; Vender, J.S.; Levin, S.D.; Koh, J.; Parikh, K.N.; Patel, S.S. Effect of ventilation on cerebral oxygenation in patients undergoing surgery in the beach chair position: A randomized controlled trial. Br. J. Anaesth. 2014, 113, 618–627. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ide, K.; Eliasziw, M.; Poulin, M.J. Relationship between middle cerebral artery blood velocity and end-tidal PCO2 in the hypocapnic-hypercapnic range in humans. J. Appl. Physiol. 2003, 95, 129–137. [Google Scholar] [CrossRef]
- Balanos, G.M.; Talbot, N.P.; Dorrington, K.L.; Robbins, P.A. Human pulmonary vascular response to 4 h of hypercapnia and hypocapnia measured using Doppler echocardiography. J. Appl. Physiol. 2003, 94, 1543–1551. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dorrington, K.L.; Balanos, G.M.; Talbot, N.P.; Robbins, P.A. Extent to which pulmonary vascular responses to PCO2 and PO2 play a functional role within the healthy human lung. J. Appl. Physiol. 2010, 108, 1084–1096. [Google Scholar] [CrossRef] [Green Version]
- Wang, Y.; Wang, H.; Wang, H.; Zhao, X.; Li, S.; Chen, L. Exploring the intraoperative lung protective ventilation of different positive end-expiratory pressure levels during abdominal laparoscopic surgery with Trendelenburg position. Ann. Transl. Med. 2019, 7, 171. [Google Scholar] [CrossRef]
- Kwak, H.J.; Lee, J.Y.; Wha Lee, J.; Kim, H.S.; Hur, H.J.; Kim, J.Y. Effect of mild hypercapnia on lung oxygenation in sitting position during shoulder arthroscopy under general anesthesia. Med. Sci. Monit. 2017, 23, 843–849. [Google Scholar] [CrossRef] [Green Version]
- Cressoni, M.; Gotti, M.; Chiurazzi, C.; Massari, D.; Algieri, I.; Amini, M.; Cammaroto, A.; Brioni, M.; Montaruli, C.; Nikolla, K.; et al. Mechanical power and development of ventilator-induced lung injury. Anesthesiology 2016, 124, 1100–1108. [Google Scholar] [CrossRef] [Green Version]
- Fogagnolo, A.; Montanaro, F.; Al-Husinat, L.; Turrini, C.; Rauseo, M.; Mirabella, L.; Ragazzi, R.; Ottaviani, I.; Cinnella, G.; Volta, C.; et al. Management of intraoperative mechanical ventilation to prevent postoperative complications after general anesthesia: A narrative review. J. Clin. Med. 2021, 10, 2656. [Google Scholar] [CrossRef]
- Balanos, G.M.; Pugh, K.; Frise, M.C.; Dorrington, K.L. Exaggerated pulmonary vascular response to acute hypoxia in older men. Exp. Physiol. 2015, 100, 1187–1198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.N.; Shallwani, H.; Khan, M.U.; Shamim, M.S. Noninvasive monitoring intracranial pressure—A review of available modalities. Surg. Neurol. Int. 2017, 8, 51. [Google Scholar] [PubMed]
- Végh, T.; Szatmári, S.; Juhász, M.; Laszlo, I.; Vaško, A.; Takács, I.; Szegedi, L.; Fulesdi, B. One-lung ventilation does not result in cerebral desaturation during application of lung protective strategy if normocapnia is maintained. Acta Physiol. Hung. 2013, 100, 163–172. [Google Scholar] [CrossRef] [PubMed]
| Normocapnia (n = 28) | Hypercapnia (n = 29) | p Value | |
|---|---|---|---|
| Age (years) | 48 ± 5 | 48 ± 7 | 0.959 |
| Body mass index (kg/m2) | 24 ± 3 | 25 ± 3 | 0.168 |
| Anesthesia time (min) | 94 ± 31 | 103 ± 42 | 0.360 |
| Operation time (min) | 65 ± 30 | 74 ± 42 | 0.359 |
| Pneumoperitoneum time (min) | 53 ± 24 | 60 ± 35 | 0.343 |
| Total infused propofol (mg) | 676 ± 227 | 754 ± 249 | 0.474 |
| Total infused remifentanil (ug) | 587 ± 220 | 633 ± 249 | 0.474 |
| Variables | Group | Tind | Tpp10 | Tpp40 |
|---|---|---|---|---|
| Ppeak (cmH2O) | Normocapnia | 14 ± 4 | 21 ± 4 * | 21 ± 4 * |
| Hypercapnia | 13 ± 2 | 20 ± 3 * | 19 ± 3 * | |
| Pplat (cmH2O) | Normocapnia | 11 ± 4 | 17 ± 4 * | 17 ± 4 * |
| Hypercapnia | 11 ± 2 | 17 ± 3 * | 17 ± 4 * | |
| RR (breaths/min) | Normocapnia | 15 ± 3 | 20 ± 4 * | 20 ± 4 * |
| Hypercapnia | 14 ± 4 | 11 ± 2 * | 12 ± 2 | |
| Cdyn (l/cmH2O) | Normocapnia | 36 ± 10 | 21 ± 5 * | 21 ± 5 * |
| Hypercapnia | 37 ± 9 | 22 ± 4 * | 23 ± 7 * | |
| Cstat (l/cmH2O) | Normocapnia | 61 ± 41 | 28 ± 9 * | 27 ± 8 * |
| Hypercapnia | 58 ± 25 | 28 ± 9 * | 28 ± 12 * | |
| MP (J/min) | Normocapnia | 5 ± 1 | 9 ± 2 * | 9 ± 2 * |
| Hypercapnia | 4 ± 2 | 5 ± 1 | 5 ± 1 |
| Variables | Group | Tind | Tpp40 |
|---|---|---|---|
| ETCO2 (mmHg) | Normocapnia | 34 ± 4 | 30 ± 4 * |
| Hypercapnia | 36 ± 5 | 44 ± 3 * | |
| pH | Normocapnia | 7.44 ± 0.03 | 7.42 ± 0.05 |
| Hypercapnia | 7.42 ± 0.05 | 7.33 ± 0.05 *,† | |
| PaO2 (mmHg) | Normocapnia | 257 ± 61 | 202 ± 54 * |
| Hypercapnia | 263 ± 88 | 206 ± 48 * | |
| PaCO2 (mmHg) | Normocapnia | 37 ± 4 | 38 ± 5 |
| Hypercapnia | 40 ± 6 | 50 ± 6 *,† | |
| Vd/Vt (%) | Normocapnia | 12 ± 9 | 23 ± 8 * |
| Hypercapnia | 13 ± 9 | 16 ± 6 *,† |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, C.-G.; Jung, W.-S.; Park, H.-Y.; Kim, H.-W.; Kwak, H.-J.; Jo, Y.-Y. Comparison of the Effects of Normocapnia and Mild Hypercapnia on the Optic Nerve Sheath Diameter and Regional Cerebral Oxygen Saturation in Patients Undergoing Gynecological Laparoscopy with Total Intravenous Anesthesia. J. Clin. Med. 2021, 10, 4707. https://doi.org/10.3390/jcm10204707
Park C-G, Jung W-S, Park H-Y, Kim H-W, Kwak H-J, Jo Y-Y. Comparison of the Effects of Normocapnia and Mild Hypercapnia on the Optic Nerve Sheath Diameter and Regional Cerebral Oxygen Saturation in Patients Undergoing Gynecological Laparoscopy with Total Intravenous Anesthesia. Journal of Clinical Medicine. 2021; 10(20):4707. https://doi.org/10.3390/jcm10204707
Chicago/Turabian StylePark, Chun-Gon, Wol-Seon Jung, Hee-Yeon Park, Hye-Won Kim, Hyun-Jeong Kwak, and Youn-Yi Jo. 2021. "Comparison of the Effects of Normocapnia and Mild Hypercapnia on the Optic Nerve Sheath Diameter and Regional Cerebral Oxygen Saturation in Patients Undergoing Gynecological Laparoscopy with Total Intravenous Anesthesia" Journal of Clinical Medicine 10, no. 20: 4707. https://doi.org/10.3390/jcm10204707
APA StylePark, C.-G., Jung, W.-S., Park, H.-Y., Kim, H.-W., Kwak, H.-J., & Jo, Y.-Y. (2021). Comparison of the Effects of Normocapnia and Mild Hypercapnia on the Optic Nerve Sheath Diameter and Regional Cerebral Oxygen Saturation in Patients Undergoing Gynecological Laparoscopy with Total Intravenous Anesthesia. Journal of Clinical Medicine, 10(20), 4707. https://doi.org/10.3390/jcm10204707






