Evaluation of the Differences in the Expression of Biogenic Amine-Related mRNAs and Proteins in Endometrioid Endometrial Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. RNA Isolation
2.3. mRNA Microarrays
2.4. Real-Time Quantitative Reverse Transcription PCR
2.5. ELISA
2.6. Statistical Analysis
3. Results
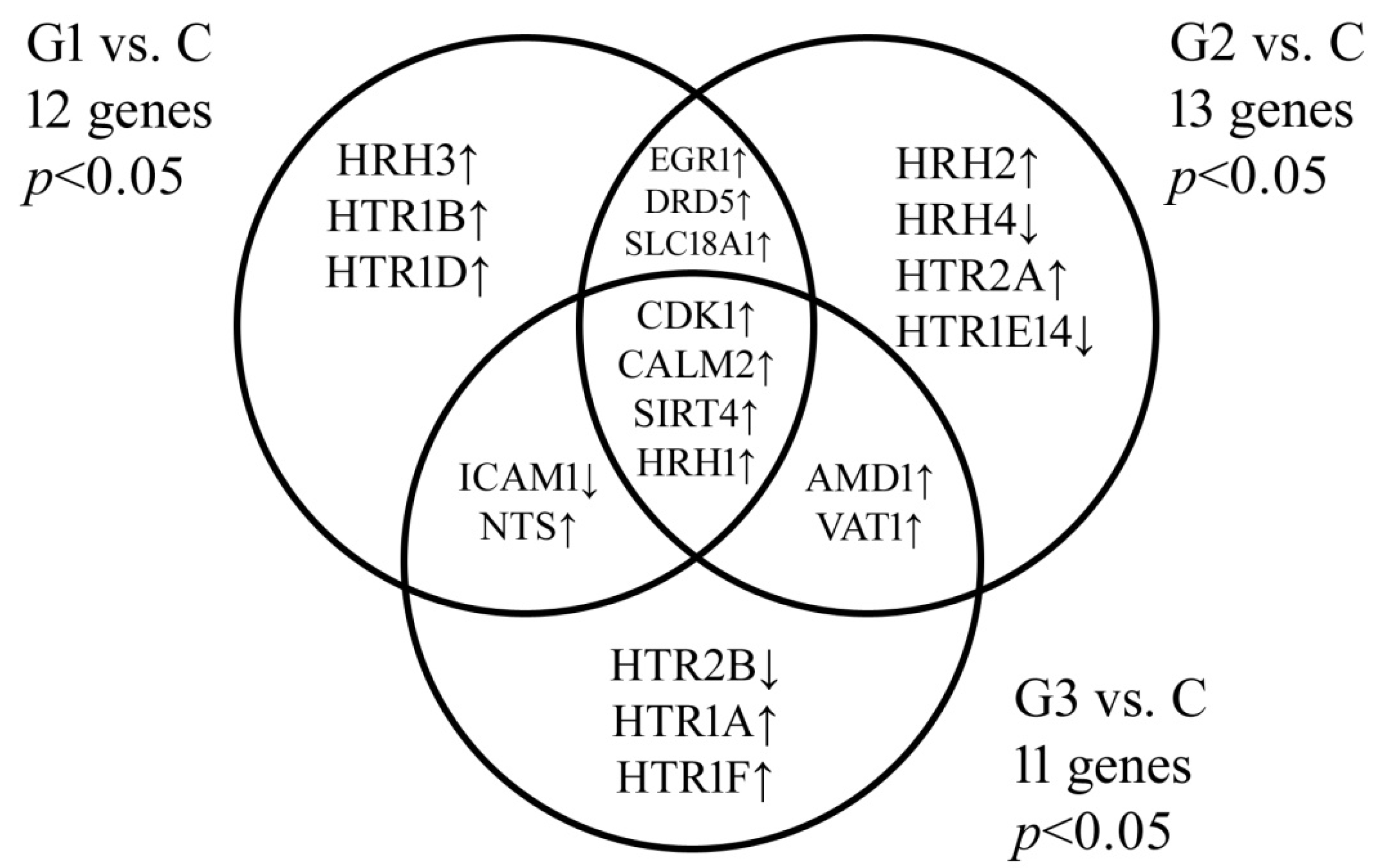
3.1. Biogenic Amine-Related Genes Expression Profile in Endometrial Tissues Determined by Microarrays and RT-qPCR
3.2. Level of Biogenic Amine-Related Proteins in the Serum of Patients Determined by ELISA
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Calzada, J.; del Olmo, A.; Picon, A.; Gaya, P.; Nuñez, M. Reducing Biogenic-Amine-Producing Bacteria, Decarboxylase Activity, and Biogenic Amines in Raw Milk Cheese by High-Pressure Treatments. Appl. Environ. Microbiol. 2012, 79, 1277–1283. [Google Scholar] [CrossRef]
- Doeun, D.; Davaatseren, M.; Chung, M.-S. Biogenic amines in foods. Food Sci. Biotechnol. 2017, 26, 1463–1474. [Google Scholar] [CrossRef] [PubMed]
- Durak-Dados, A.; Michalski, M.; Osek, J. Histamine and other biogenic amines in food. J. Veter. Res. 2020, 64, 281–288. [Google Scholar] [CrossRef]
- Sánchez-Jiménez, F.; Ruiz-Pérez, M.V.; Urdiales, J.L.; Medina, M. Pharmacological potential of biogenic amine-polyamine interactions beyond neurotransmission. Br. J. Pharmacol. 2013, 170, 4–16. [Google Scholar] [CrossRef] [PubMed]
- Plenis, A.; Olędzka, I.; Kowalski, P.; Miękus, N.; Bączek, T. Recent Trends in the quantification of biogenic amines in biofluids as biomarkers of various disorders: A review. J. Clin. Med. 2019, 8, 640. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, L.; Hodges, K.; Meng, F.; Alpini, G.; Francis, H. Histamine and histamine receptor regulation of gastrointestinal cancers. Transl. Gastrointest. Cancer 2012, 1, 215–227. [Google Scholar]
- Takaishi, S.; Cui, G.; Frederick, D.M.; Carlson, J.E.; Houghton, J.; Varro, A.; Dockray, G.J.; Ge, Z.; Whary, M.T.; Rogers, A.B.; et al. Synergistic inhibitory effects of gastrin and histamine receptor antagonists on helicobacter-induced gastric cancer. Gastroenterology 2005, 128, 1965–1983. [Google Scholar] [CrossRef]
- Wang, Z.Y.; Ding, Y.; Miki, T.; Warita, K.; Matsumoto, Y.; Takeuchi, Y.; Wang, S.J.; Feng, J.G.; Liu, W.; Wang, Y.D.; et al. Nerve growth factor and receptors are significantly affected by histamine stimulus through H1 receptor in pancreatic carcinoma cells. Mol. Med. Rep. 2010, 3, 103–109. [Google Scholar] [CrossRef][Green Version]
- Losurdo, G.; Principi, M.; Girardi, B.; Pricci, M.; Barone, M.; Ierardi, E.; Di Leo, A. Histamine and Histaminergic Receptors in Colorectal Cancer: From Basic Science to Evidence-based Medicine. Anti-Cancer Agents Med. Chem. 2018, 18, 15–20. [Google Scholar] [CrossRef]
- Zhang, C.; Yu, Y.; Ma, L.; Fu, P. Histamine H3 Receptor Promotes Cell Survival via Regulating PKA/CREB/CDKN1A Signal Pathway in Hepatocellular Carcinoma. OncoTargets Ther. 2020, 13, 3765–3776. [Google Scholar] [CrossRef]
- Francis, H.; Meng, F.; Gaudio, E.; Alpini, G. Histamine regulation of biliary proliferation. J. Hepatol. 2012, 56, 1204–1206. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sarkar, C.; Chakroborty, D.; Chowdhury, U.R.; Dasgupta, P.S.; Basu, S. Dopamine Increases the Efficacy of Anticancer Drugs in Breast and Colon Cancer Preclinical Models. Clin. Cancer Res. 2008, 14, 2502–2510. [Google Scholar] [CrossRef]
- Moreno-Smith, M.; Lu, C.; Shahzad, M.M.; Armaiz-Pena, G.N.; Allen, J.K.; Stone, R.L.; Mangala, L.S.; Han, H.D.; Kim, H.S.; Farley, D.; et al. Dopamine Blocks Stress-Mediated Ovarian Carcinoma Growth. Clin. Cancer Res. 2011, 17, 3649–3659. [Google Scholar] [CrossRef] [PubMed]
- Ganguly, S.; Basu, B.; Shome, S.; Jadhav, T.; Roy, S.; Majumdar, J.; Dasgupta, P.S.; Basu, S. Dopamine, by acting through its D2 receptor, inhibits insulin-like growth factor-I (IGF-I)-induced gastric cancer cell proliferation via up-regulation of Krüppel-like factor 4 through down-regulation of IGF-IR and AKT phosphorylation. Am. J. Pathol. 2010, 177, 2701–2707. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Remmerie, M.; Janssens, V. Targeted therapies in type II endometrial cancers: Too little, but not too late. Int. J. Mol. Sci. 2018, 19, 2380. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, S.; Femia, M.; Buscarino, V.; Franchi, D.; Garbi, A.; Zanagnolo, V.; Del Grande, M.; Manganaro, L.; Alessi, S.; Giannitto, C.; et al. Endometrial cancer: An overview of novelties in treatment and related imaging keypoints for local staging. Cancer Imaging 2018, 18, 45. [Google Scholar] [CrossRef]
- MacKintosh, M.L.; Crosbie, E.J. Prevention strategies in endometrial carcinoma. Curr. Oncol. Rep. 2018, 20, 101. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Shao, H.; Ban, X.; Zhang, H.; You, Y.; Zhou, N.; Mao, X.; Zhao, H.; Chen, J.; Lu, Z. Detection of POLE subtypes in high-grade endometrioid carcinoma by BaseScope-ISH Assay. Front. Oncol. 2019, 9, 831. [Google Scholar] [CrossRef]
- Razzaghi, H.; Martin, D.N.; Quesnel-Crooks, S.; Hong, Y.; Gregg, E.; Andall-Brereton, G.; Gawryszweski, V.; Saraiya, M. 10-year trends in noncommunicable disease mortality in the Caribbean region. Rev. Panam. Salud Pública 2019, 43, e37. [Google Scholar] [CrossRef]
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; Bray, F. Global Cancer Observatory: Cancer Today. Lyon, France: International Agency for Research on Cancer. Available online: https://gco.iarc.fr/today (accessed on 23 July 2021).
- Falzone, L.; Salomone, S.; Libra, M. Evolution of cancer pharmacological treatments at the turn of the third millennium. Front. Pharmacol. 2018, 9, 1300. [Google Scholar] [CrossRef] [PubMed]
- Oh, M.; Huh, E.; Oh, M.S.; Jeong, J.-S.; Hong, S.-P. Development of a diagnostic method for Parkinson’s disease by reverse-phase high-performance liquid chromatography coupled with integrated pulsed amperometric detection. J. Pharm. Biomed. Anal. 2018, 153, 110–116. [Google Scholar] [CrossRef]
- Taj, A.; Jamil, N. Cerebrospinal fluid concentrations of biogenic amines: Potential biomarkers for diagnosis of bacterial and viral meningitis. Pathogens 2018, 7, 39. [Google Scholar] [CrossRef] [PubMed]
- Parksepp, M.; Leppik, L.; Koch, K.; Uppin, K.; Kangro, R.; Haring, L.; Vasar, E.; Zilmer, M. Metabolomics approach revealed robust changes in amino acid and biogenic amine signatures in patients with schizophrenia in the early course of the disease. Sci. Rep. 2020, 10, 13983. [Google Scholar] [CrossRef] [PubMed]
- Nelson, T.; Borgogna, J.-L.; Brotman, R.; Ravel, J.; Walk, S.T.; Yeoman, C.J. Vaginal biogenic amines: Biomarkers of bacterial vaginosis or precursors to vaginal dysbiosis? Front. Physiol. 2015, 6, 253. [Google Scholar] [CrossRef]
- Maráková, K.; Piešťanský, J.; Zelinková, Z.; Mikuš, P. Simultaneous determination of twelve biogenic amines in human urine as potential biomarkers of inflammatory bowel diseases by capillary electrophoresis—tandem mass spectrometry. J. Pharm. Biomed. Anal. 2020, 186, 113294. [Google Scholar] [CrossRef]
- Miękus, N.; Olędzka, I.; Plenis, A.; Kowalski, P.; Bień, E.; Miękus, A.; Krawczyk, M.A.; Adamkiewicz-Drożyńska, E.; Bączek, T. Determination of urinary biogenic amines’ biomarker profile in neuroblastoma and pheochromocytoma patients by MEKC method with preceding dispersive liquid–liquid microextraction. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 2016, 1036–1037, 114–123. [Google Scholar] [CrossRef]
- Kao, Y.-Y.; Liu, K.-T.; Huang, M.-F.; Chiu, T.-C.; Chang, H.-T. Analysis of amino acids and biogenic amines in breast cancer cells by capillary electrophoresis using polymer solutions containing sodium dodecyl sulfate. J. Chromatogr. A 2010, 1217, 582–587. [Google Scholar] [CrossRef]
- Fritz, I.; Wagner, P.; Olsson, H. Improved survival in several cancers with use of H1-antihistamines desloratadine and loratadine. Transl. Oncol. 2021, 14, 101029. [Google Scholar] [CrossRef]
- Medina, V.; Rivera, E.S. Histamine receptors and cancer pharmacology. Br. J. Pharmacol. 2010, 161, 755–767. [Google Scholar] [CrossRef]
- Blaya, B.; Nicolau-Galmes, F.; Jangi, S.M.; Ortega-Martinez, I.; Alonso-Tejerina, E.; Burgos-Bretones, J.; Perezyarza, G.; Asumendi, A.; Boyano, M.D. Histamine and Histamine Receptor Antagonists in Cancer Biology. Inflamm. Allergy-Drug Targets 2010, 9, 146–157. [Google Scholar] [CrossRef]
- Wang, M.; Wei, X.; Shi, L.; Chen, B.; Zhao, G.; Yang, H. Integrative genomic analyses of the histamine H1 receptor and its role in cancer prediction. Int. J. Mol. Med. 2014, 33, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Nogueira, P.; Noguera-Castells, A.; Fuster, G.; Recalde-Percaz, L.; Moragas, N.; López-Plana, A.; Enreig, E.; Jauregui, P.; Carbó, N.; Almendro, V.; et al. Histamine receptor 1 inhibition enhances antitumor therapeutic responses through extracellular signal-regulated kinase (ERK) activation in breast cancer. Cancer Lett. 2018, 424, 70–83. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Hou, Y.; Yin, C.; Hu, J.; Gao, T.; Huang, X.; Zhang, X.; Xing, J.; An, J.; Wan, S.; et al. Upregulation of histamine receptor H1 promotes tumor progression and contributes to poor prognosis in hepatocellular carcinoma. Oncogene 2019, 39, 1724–1738. [Google Scholar] [CrossRef]
- Matsumoto, N.; Ebihara, M.; Oishi, S.; Fujimoto, Y.; Okada, T.; Imamura, T. Histamine H1 receptor antagonists selectively kill cisplatin-resistant human cancer cells. Sci. Rep. 2021, 11, 1492. [Google Scholar] [CrossRef]
- Shi, Z.; Fultz, R.; Engevik, M.A.; Gao, C.; Hall, A.; Major, A.; Mori-Akiyama, Y.; Versalovic, J. Distinct roles of histamine H1- and H2-receptor signaling pathways in inflammation-associated colonic tumorigenesis. Am. J. Physiol. Gastrointest. Liver Physiol. 2019, 316, G205–G216. [Google Scholar] [CrossRef]
- Gao, C.; Ganesh, B.; Shi, Z.; Shah, R.R.; Fultz, R.; Major, A.; Venable, S.; Lugo, M.; Hoch, K.; Chen, X.; et al. Gut microbe–mediated suppression of inflammation-associated colon carcinogenesis by luminal histamine production. Am. J. Pathol. 2017, 187, 2323–2336. [Google Scholar] [CrossRef] [PubMed]
- Medina, V.; Croci, M.; Crescenti, E.; Mohamad, N.; Sanchez-Jiménez, F.; Massari, N.; Nuñez, M.; Cricco, G.; Martin, G.; Bergoc, R.; et al. The role of histamine in human mammary carcinogenesis: H3 and H4 receptors as potential therapeutic targets for breast cancer treatment. Cancer Biol. Ther. 2008, 7, 28–35. [Google Scholar] [CrossRef]
- Chen, J.; Hu, X. Inhibition of histamine receptor H3R suppresses prostate cancer growth, invasion and increases apoptosis via the AR pathway. Oncol. Lett. 2018, 16, 4921–4928. [Google Scholar] [CrossRef]
- Sterle, H.; Nicoud, M.B.; Massari, N.A.; Delgado, M.A.T.; Ducloux, M.V.H.; Cremaschi, G.A.; Medina, V.A. Immunomodulatory role of histamine H4 receptor in breast cancer. Br. J. Cancer 2018, 120, 128–138. [Google Scholar] [CrossRef]
- Fang, Z.; Yao, W.; Xiong, Y.; Li, J.; Liu, L.; Shi, L.; Zhang, W.; Zhang, C.; Nie, L.; Wan, J. Attenuated expression of HRH4 in colorectal carcinomas: A potential influence on tumor growth and progression. BMC Cancer 2011, 11, 195. [Google Scholar] [CrossRef] [PubMed]
- Salem, A.; Almahmoudi, R.; Listyarifah, D.; Siponen, M.; Maaninka, K.; Eklund, K.K.; Al-Samadi, A.; Salo, T. Histamine H4 receptor signalling in tongue cancer and its potential role in oral carcinogenesis—A short report. Cell. Oncol. 2017, 40, 621–630. [Google Scholar] [CrossRef] [PubMed]
- Meng, F.; Han, Y.; Staloch, D.; Francis, T.; Stokes, A.; Francis, H. The H4 histamine receptor agonist, clobenpropit, suppresses human cholangiocarcinoma progression by disruption of epithelial mesenchymal transition and tumor metastasis. Hepatology 2011, 54, 1718–1728. [Google Scholar] [CrossRef]
- He, G.-H.; Ding, J.-Q.; Zhang, X.; Xu, W.-M.; Lin, X.-Q.; Huang, M.-J.; Feng, J.; Wang, P.; Cai, W.-K. Activation of histamine H4 receptor suppresses the proliferation and invasion of esophageal squamous cell carcinoma via both metabolism and non-metabolism signaling pathways. J. Mol. Med. 2018, 96, 951–964. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Jiang, Y.; Ikeda, J.; Tian, T.; Sato, A.; Ohtsu, H.; Morii, E. Roles of histamine on the expression of aldehyde dehydrogenase 1 in endometrioid adenocarcinoma cell line. Cancer Med. 2014, 3, 1126–1135. [Google Scholar] [CrossRef]
- Hao, F.; Tan, M.; Xu, X.; Cui, M.-Z. Histamine induces Egr-1 expression in human aortic endothelial cells via the H1 receptor-mediated protein kinase Cδ-dependent ERK activation pathway. J. Biol. Chem. 2008, 283, 26928–26936. [Google Scholar] [CrossRef]
- Cheng, S.-Y.; Serova, L.I.; Glazkova, D.; Sabban, E.L. Regulation of rat dopamine β-hydroxylase gene transcription by early growth response gene 1 (Egr1). Brain Res. 2008, 1193, 1–11. [Google Scholar] [CrossRef][Green Version]
- Yoon, Y.J.; Kim, D.-K.; Yoon, C.M.; Park, J.; Kim, Y.-K.; Roh, T.-Y.; Gho, Y.S. Egr-1 Activation by cancer-derived extracellular vesicles promotes endothelial cell migration via ERK1/2 and JNK signaling pathways. PLoS ONE 2014, 9, e115170. [Google Scholar] [CrossRef] [PubMed]
- Albitar, L.; Pickett, G.; Morgan, M.; Wilken, J.A.; Maihle, N.J.; Leslie, K.K. EGFR isoforms and gene regulation in human endometrial cancer cells. Mol. Cancer 2010, 9, 166. [Google Scholar] [CrossRef] [PubMed]
- Saegusa, M.; Hashimura, M.; Kuwata, T.; Hamano, M.; Watanabe, J.; Kawaguchi, M.; Okayasu, I. Transcription factor Egr1 acts as an upstream regulator of β-catenin signalling through up-regulation of TCF4 and p300 expression during trans -differentiation of endometrial carcinoma cells. J. Pathol. 2008, 216, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Sobczuk, P.; Łomiak, M.; Cudnoch-Jędrzejewska, A. Dopamine D1 receptor in cancer. Cancers 2020, 12, 3232. [Google Scholar] [CrossRef] [PubMed]
- Kline, C.L.B.; Ralff, M.D.; Lulla, A.R.; Wagner, J.M.; Abbosh, P.H.; Dicker, D.T.; Allen, J.E.; El-Deiry, W.S. Role of dopamine receptors in the anticancer activity of ONC201. Neoplasia 2018, 20, 80–91. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, V.V.; Madhukar, N.S.; Gilvary, C.; Kline, C.L.B.; Oster, S.; El-Deiry, W.S.; Elemento, O.; Doherty, F.C.; Van Engelenburg, A.; Durrant, J.; et al. Dopamine receptor D5 is a modulator of tumor response to dopamine receptor D2 antagonism. Clin. Cancer Res. 2019, 25, 2305–2313. [Google Scholar] [CrossRef] [PubMed]
- Rosas-Cruz, A.; Salinas-Jazmín, N.; Velázquez, M.A.V. Dopamine receptors in cancer: Are they valid therapeutic targets? Technol. Cancer Res. Treat. 2021, 20, 15330338211027913. [Google Scholar] [CrossRef]
| ID | mRNA | Microarray | qRT-PCR | ||||
|---|---|---|---|---|---|---|---|
| G1 vs. C | G2 vs. C | G3 vs. C | G1 vs. C | G2 vs. C | G3 vs. C | ||
| 207243_s_at | CALM2 | −9.69 | −10.66 | −14.01 | −11.23 | −10.64 | −15.88 |
| 208486_at | DRD5 | −4.25 | −3.69 | −4.87 | −4.65 | −4.01 | −4.30 |
| 201693_s_at | EGR1 | 11.25 | 10.58 | 14.22 | 10.52 | 10.63 | 13.25 |
| 201694_s_at | EGR1 | 11.26 | 10.41 | 14.03 | |||
| 202637_s_at | ICAM1 | −8.66 | −17.25 | −14.66 | −8.55 | −18.41 | −12.63 |
| 202638_s_at | ICAM1 | −8.41 | −17.77 | −14.69 | |||
| 215485_s_at | ICAM1 | −8.69 | −18.03 | −15.01 | |||
| 205579_at | HRH1 | 1.98 | 2.14 | 2.75 | 1.98 | 2.14 | 2.75 |
| 205580_s_at | HRH1 | 1.99 | 2.47 | 2.81 | |||
| 220805_at | HRH2 | 3.11 | 3.02 | 2.14 | 3.44 | 2.65 | 2.14 |
| 220447_at | HRH3 | 2.74 | 6.14 | 5.75 | 2.74 | 7.01 | 5.75 |
| 221663_x_at | HRH3 | 2.66 | 6.74 | 5.98 | |||
| 221169_s_at | HRH4 | −2.14 | −3.66 | 2.88 | −2.14 | −3.66 | 2.88 |
| 221170_at | HRH4 | −2.36 | −3.41 | 2.54 | |||
| Proteins | Group | |||
|---|---|---|---|---|
| C | G1 | G2 | G3 | |
| CALM2 | 2047.55 ± 15.25 | 2365.14 ± 8.96 | 524.06 ± 4.58 | 109.99 ± 2.74 |
| DRD5 | 4.58 ± 0.85 | 2.01 ± 0.74 | 0.89 ± 0.11 | 0.66 ± 0.36 |
| EGR1 | 365.54 ± 7.77 | 1254.01 ± 2.36 | 541.36 ± 3.41 | 1698.36 ± 11.25 |
| ICAM1 | 1854.63 ± 3.14 | 654.01 ± 2.11 | 402.01 ± 4.08 | 107.33 ± 3.54 |
| HRH1 | 4.44 ± 0.48 | 9.58 ± 1.22 | 10.44 ± 0.94 | 16.74 ± 1.07 |
| HRH2 | 1.47 ± 0.26 | 2.44 ± 0.55 | 4.66 ± 1.04 | 8.14 ± 1.58 |
| HRH3 | 2.18 ± 0.73 | 3.44 ± 0.26 | 4.69 ± 0.37 | 7.11 ± 0.12 |
| HRH4 | 9.12 ± 0.25 | 7.64 ± 0.49 | 3.14 ± 0.19 | 1.01 ± 0.34 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Czerwiński, M.; Bednarska-Czerwińska, A.; Zmarzły, N.; Boroń, D.; Oplawski, M.; Grabarek, B.O. Evaluation of the Differences in the Expression of Biogenic Amine-Related mRNAs and Proteins in Endometrioid Endometrial Cancer. J. Clin. Med. 2021, 10, 4872. https://doi.org/10.3390/jcm10214872
Czerwiński M, Bednarska-Czerwińska A, Zmarzły N, Boroń D, Oplawski M, Grabarek BO. Evaluation of the Differences in the Expression of Biogenic Amine-Related mRNAs and Proteins in Endometrioid Endometrial Cancer. Journal of Clinical Medicine. 2021; 10(21):4872. https://doi.org/10.3390/jcm10214872
Chicago/Turabian StyleCzerwiński, Michał, Anna Bednarska-Czerwińska, Nikola Zmarzły, Dariusz Boroń, Marcin Oplawski, and Beniamin Oskar Grabarek. 2021. "Evaluation of the Differences in the Expression of Biogenic Amine-Related mRNAs and Proteins in Endometrioid Endometrial Cancer" Journal of Clinical Medicine 10, no. 21: 4872. https://doi.org/10.3390/jcm10214872
APA StyleCzerwiński, M., Bednarska-Czerwińska, A., Zmarzły, N., Boroń, D., Oplawski, M., & Grabarek, B. O. (2021). Evaluation of the Differences in the Expression of Biogenic Amine-Related mRNAs and Proteins in Endometrioid Endometrial Cancer. Journal of Clinical Medicine, 10(21), 4872. https://doi.org/10.3390/jcm10214872






