Conservative Management of Uterine Adenomyosis: Medical vs. Surgical Approach
Abstract
1. Introduction
2. Medical Treatment of Adenomyosis
2.1. Non-Steroidal Anti-Inflammatory Drugs
2.2. Combined Oral Contraceptives
2.3. Progestins
2.4. Ulipristal Acetate
2.5. Gonadotropin-Releasing Hormone (GnRH) Agonists
2.6. Oral GnRH Antagonists
2.7. Experimental Approaches and Preclinical Models
2.7.1. Bromocriptine
2.7.2. Aromatase Inhibitors
2.7.3. Anti-Platelet Therapy
2.7.4. MicroRNAs
2.8. Medical Management of Infertility in Adenomyosis Patients
3. Surgical Management of Adenomyosis
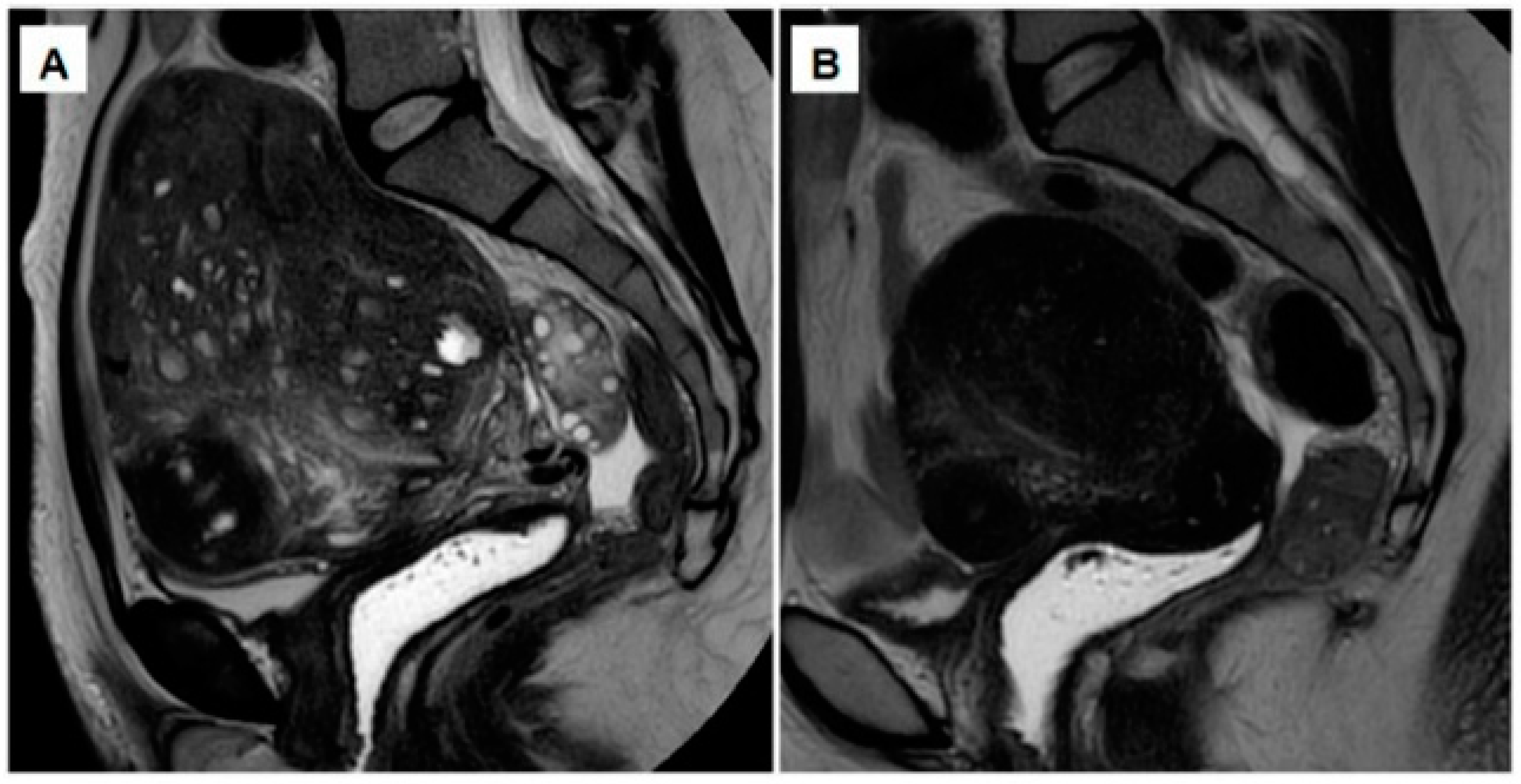
3.1. Partial Reduction Surgery
Wedge Resection
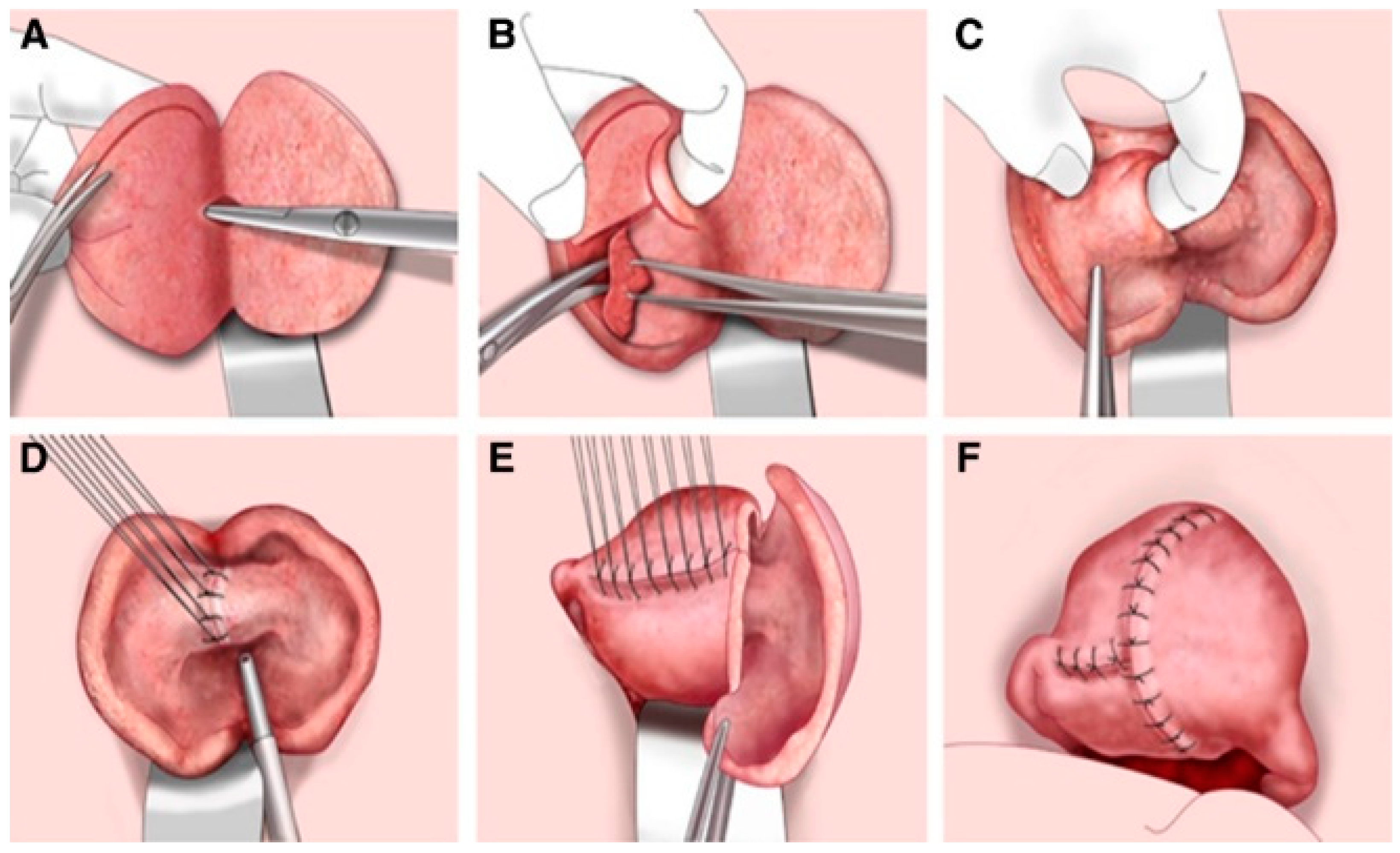
3.2. Complete Adenomyosis Excision
3.2.1. The Triple-Flap Method
3.2.2. Asymmetric Dissection
3.3. Important Remarks on the Surgical Approach
4. Non-Surgical Alternatives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stratopoulou, C.A.; Donnez, J.; Dolmans, M.M. Origin and Pathogenic Mechanisms of Uterine Adenomyosis: What Is Known So Far. Reprod. Sci. 2021, 28, 2087–2097. [Google Scholar] [CrossRef]
- Donnez, J.; Donnez, O.; Dolmans, M.M. Introduction: Uterine adenomyosis, another enigmatic disease of our time. Fertil. Steril. 2018, 109, 369–370. [Google Scholar] [CrossRef]
- Garry, R. The endometriosis syndromes: A clinical classification in the presence of aetiological confusion and therapeutic anarchy. Hum. Reprod. 2004, 19, 760–768. [Google Scholar] [CrossRef][Green Version]
- Habiba, M.; Gordts, S.; Bazot, M.; Brosens, I.; Benagiano, G. Exploring the challenges for a new classification of adenomyosis. Reprod. Biomed. Online 2020, 40, 569–581. [Google Scholar] [CrossRef]
- Yu, O.; Schulze-Rath, R.; Grafton, J.; Hansen, K.; Scholes, D.; Reed, S.D. Adenomyosis incidence, prevalence and treatment: United States population-based study 2006–2015. Am. J. Obstet. Gynecol. 2020, 223, 94.e1–94.e10. [Google Scholar] [CrossRef] [PubMed]
- Vannuccini, S.; Luisi, S.; Tosti, C.; Sorbi, F.; Petraglia, F. Role of medical therapy in the management of uterine adenomyosis. Fertil. Steril. 2018, 109, 398–405. [Google Scholar] [CrossRef]
- Marjoribanks, J.; Ayeleke, R.O.; Farquhar, C.; Proctor, M. Nonsteroidal anti-inflammatory drugs for primary dysmenorrhoea. Cochrane Database Syst. Rev. 2015, 2015, CD001751. [Google Scholar]
- Iacovides, S.; Avidon, I.; Baker, F.C. What we know about primary dysmenorrhea today: A critical review. Hum. Reprod. Update 2015, 21, 762–778. [Google Scholar] [CrossRef] [PubMed]
- Bofill Rodriguez, M.; Lethaby, A.; Farquhar, C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst. Rev. 2019, 9, CD000400. [Google Scholar] [CrossRef] [PubMed]
- Rivera, R.; Yacobson, I.; Grimes, D. The mechanism of action of hormonal contraceptives and intrauterine contraceptive devices. Am. J. Obstet. Gynecol. 1999, 181, 1263–1269. [Google Scholar] [CrossRef]
- Shaaban, O.M.; Ali, M.K.; Sabra, A.M.; Abd El Aal, D.E. Levonorgestrel-releasing intrauterine system versus a low-dose combined oral contraceptive for treatment of adenomyotic uteri. A randomized clinical trial. Contraception 2015, 92, 301–307. [Google Scholar] [CrossRef]
- Hassanin, A.I.; Youssef, A.A.; Yousef, A.M.; Ali, M.K. Comparison of dienogest versus combined oral contraceptive pills in the treatment of women with adenomyosis. A randomized clinical trial. Int. J. Gynaecol. Obstet. 2021, 154, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Berlanda, N.; Somigliana, E.; Viganò, P.; Vercellini, P. Safety of medical treatments for endometriosis. Expert Opin. Drug Saf. 2016, 15, 21–30. [Google Scholar] [CrossRef]
- Levy, D.; Christin-Maitre, S.; Leroy, I.; Bergeron, C.; Garcia, E.; Freitas, S.; Coelingh-Bennink, H.J.; Bouchard, P. The endometrial approach in contraception. Ann. N. Y. Acad. Sci. 1997, 828, 59–83. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Dolmans, M.M. Endometriosis and Medical Therapy: From Progestogens to Progesterone Resistance to GnRH Antagonists. A Review. J. Clin. Med. 2021, 10, 1085. [Google Scholar] [CrossRef]
- Hirata, T.; Izumi, G.; Takamura, M.; Saito, A.; Nakazawa, A.; Harada, M.; Hirota, Y.; Koga, K.; Fujii, T.; Osuga, Y. Efficacy of dienogest in the treatment of symptomatic adenomyosis: A pilot study. Gynecol. Endocrinol. 2014, 30, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Osuga, Y.; Hayashi, K.; Kanda, S. Long-term use of dienogest for the treatment of primary and secondary dysmenorrhea. J. Obstet. Gynaecol. Res. 2020, 46, 606–617. [Google Scholar] [CrossRef]
- Osuga, Y.; Watanabe, M.; Hagino, A. Long-term use of dienogest in the treatment of painful symptoms in adenomyosis. J. Obstet. Gynaecol. Res. 2017, 43, 1441–1448. [Google Scholar] [CrossRef]
- Osuga, Y.; Fujimoto-Okabe, H.; Hagino, A. Evaluation of the efficacy and safety of dienogest in the treatment of painful symptoms in patients with adenomyosis: A randomized, double-blind, multicenter, placebo-controlled study. Fertil. Steril. 2017, 108, 673–678. [Google Scholar] [CrossRef]
- Kishi, Y.; Suginami, H.; Kuramori, R.; Yabuta, M.; Suginami, R.; Taniguchi, F. Four subtypes of adenomyosis assessed by magnetic resonance imaging and their specification. Am. J. Obstet. Gynecol. 2012, 207, 111–117. [Google Scholar] [CrossRef]
- Matsubara, S.; Kawaguchi, R.; Akinishi, M.; Nagayasu, M.; Iwai, K.; Niiro, E.; Yamada, Y.; Tanase, Y.; Kobayashi, H. Subtype I (intrinsic) adenomyosis is an independent risk factor for dienogest-related serious unpredictable bleeding in patients with symptomatic adenomyosis. Sci. Rep. 2019, 9, 17654. [Google Scholar] [CrossRef]
- Niu, X.; Luo, Q.; Wang, C.; Zhu, L.; Huang, L. Effects of Etonogestrel implants on pelvic pain and menstrual flow in women suffering from adenomyosis or endometriosis: Results from a prospective, observational study. Medicine 2021, 100, e24597. [Google Scholar] [CrossRef]
- Wu, J.; Huang, Y.; Chen, L.; Hu, J.; Zou, Y. Treatment of Adenomyosis with Subcutaneous Etonogestrel Implants. A Clinical Observational Study in 17 Patients. Med. Sci. Monit. 2018, 24, 6085–6092. [Google Scholar] [CrossRef]
- Nie, L.; Zou, H.; Ma, X.; Cheng, L.; Jiao, J.; Wang, F.; Liang, W.; Zhang, P. A clinical observational study on the efficacy of subcutaneous etonogestrel implants for adenomyosis in 20 patients. Gynecol. Endocrinol. 2021, 37, 735–739. [Google Scholar] [CrossRef]
- Ozdegirmenci, O.; Kayikcioglu, F.; Akgul, M.A.; Kaplan, M.; Karcaaltincaba, M.; Haberal, A.; Akyol, M. Comparison of levonorgestrel intrauterine system versus hysterectomy on efficacy and quality of life in patients with adenomyosis. Fertil. Steril. 2011, 95, 497–502. [Google Scholar] [CrossRef]
- Ekin, M.; Cengiz, H.; Ayağ, M.E.; Kaya, C.; Yasar, L.; Savan, K. Effects of the levonorgestrel-releasing intrauterine system on urinary symptoms in patients with adenomyosis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2013, 170, 517–520. [Google Scholar] [CrossRef]
- Bragheto, A.M.; Caserta, N.; Bahamondes, L.; Petta, C.A. Effectiveness of the levonorgestrel-releasing intrauterine system in the treatment of adenomyosis diagnosed and monitored by magnetic resonance imaging. Contraception 2007, 76, 195–199. [Google Scholar] [CrossRef]
- Cho, S.; Nam, A.; Kim, H.; Chay, D.; Park, K.; Cho, D.J.; Park, Y.; Lee, B. Clinical effects of the levonorgestrel-releasing intrauterine device in patients with adenomyosis. Am. J. Obstet. Gynecol. 2008, 198, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Sheng, J.; Zhang, W.Y.; Zhang, J.P.; Lu, D. The LNG-IUS study on adenomyosis. A 3-year follow-up study on the efficacy and side effects of the use of levonorgestrel intrauterine system for the treatment of dysmenorrhea associated with adenomyosis. Contraception 2009, 79, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Song, S.Y.; Lee, S.Y.; Kim, H.Y.; Park, D.B.; Kim, D.E.; Lee, K.H.; Lee, S.; Yang, J.B.; Yoo, H.J. Long-term efficacy and feasibility of levonorgestrel-releasing intrauterine device use in patients with adenomyosis. Medicine 2020, 99, e20421. [Google Scholar] [CrossRef] [PubMed]
- Vercellini, P.; Buggio, L.; Berlanda, N.; Barbara, G.; Somigliana, E.; Bosari, S. Estrogen-progestins and progestins for the management of endometriosis. Fertil. Steril. 2016, 106, 1552. [Google Scholar] [CrossRef] [PubMed]
- Flores, V.A.; Vanhie, A.; Dang, T.; Taylor, H.S. Progesterone Receptor Status Predicts Response to Progestin Therapy in Endometriosis. J. Clin. Endocrinol. Metab. 2018, 103, 4561–4568. [Google Scholar] [CrossRef]
- Donnez, J.; Tatarchuk, T.F.; Bouchard, P.; Puscasiu, L.; Zakharenko, N.F.; Ivanova, T.; Ugocsai, G.; Mara, M.; Jilla, M.P.; Bestel, E.; et al. Ulipristal acetate versus placebo for fibroid treatment before surgery. N. Engl. J. Med. 2012, 366, 409–420. [Google Scholar] [CrossRef] [PubMed]
- De Milliano, I.; Van Hattum, D.; Ket, J.C.F.; Huirne, J.A.F.; Hehenkamp, W.J.K. Endometrial changes during ulipristal acetate use: A systematic review. Eur. J. Obstet. Gynecol. Reprod. Biol. 2017, 214, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Stratton, P.; Hartog, B.; Hajizadeh, N.; Piquion, J.; Sutherland, D.; Merino, M.; Lee, Y.J.; Nieman, L.K. A single mid-follicular dose of CDB-2914, a new antiprogestin, inhibits folliculogenesis and endometrial differentiation in normally cycling women. Hum. Reprod. 2000, 15, 1092–1099. [Google Scholar] [CrossRef]
- Capmas, P.; Brun, J.L.; Legendre, G.; Koskas, M.; Merviel, P.; Fernandez, H. Ulipristal acetate use in adenomyosis: A randomized controlled trial. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 101978. [Google Scholar] [CrossRef]
- Gracia, M.; Alcalà, M.; Ferreri, J.; Rius, M.; Ros, C.; Saco, M.A.; Martínez-Zamora, M.; Carmona, F. Ulipristal Acetate Improves Clinical Symptoms in Women with Adenomyosis and Uterine Myomas. J. Minim. Invasive Gynecol. 2018, 25, 1274–1280. [Google Scholar] [CrossRef] [PubMed]
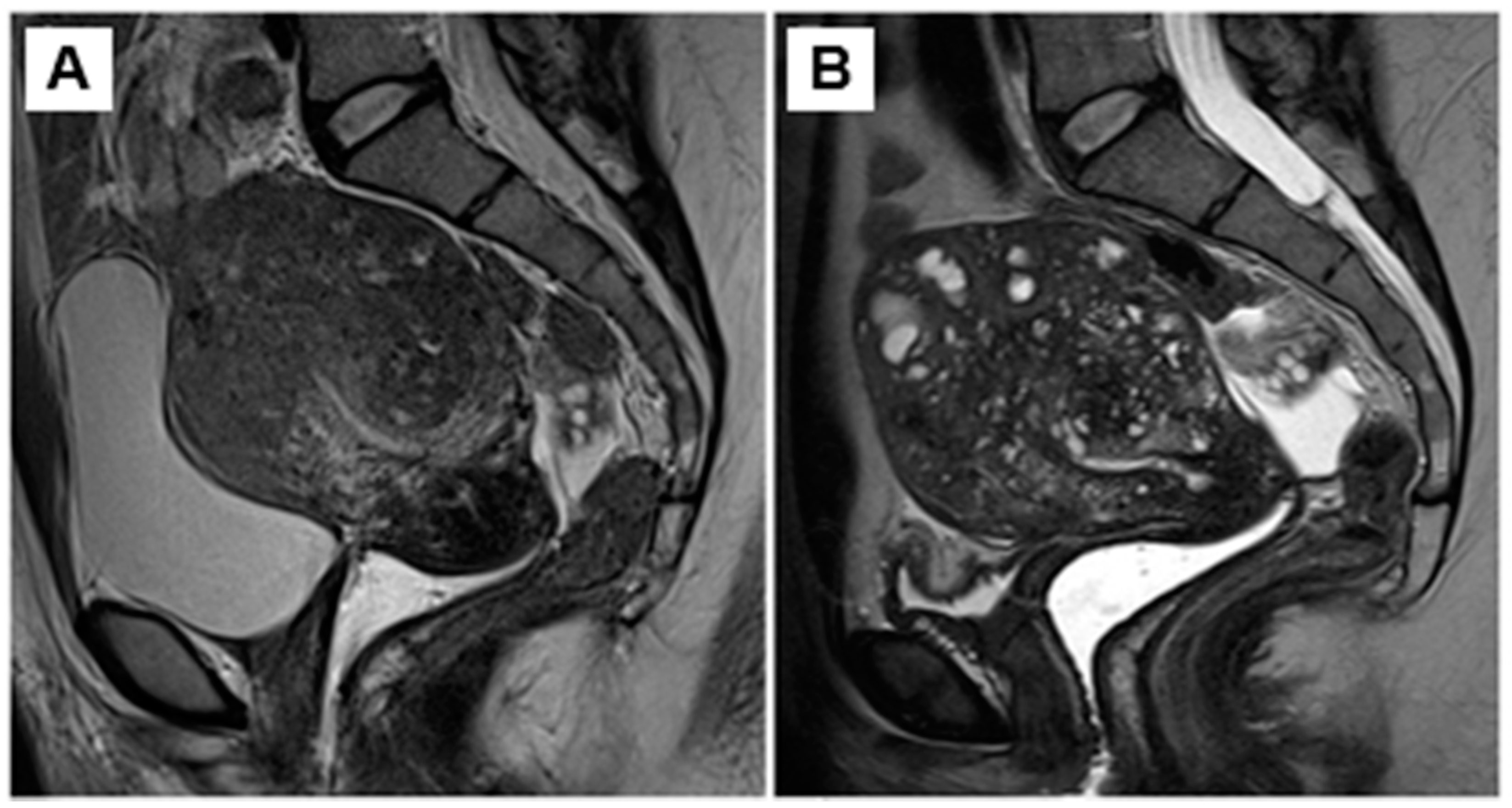
- Donnez, O.; Donnez, J. Gonadotropin-releasing hormone antagonist (linzagolix): A new therapy for uterine adenomyosis. Fertil. Steril. 2020, 114, 640–645. [Google Scholar] [CrossRef]
- Conway, F.; Morosetti, G.; Camilli, S.; Martire, F.G.; Sorrenti, G.; Piccione, E.; Zupi, E.; Exacoustos, C. Ulipristal acetate therapy increases ultrasound features of adenomyosis: A good treatment given in an erroneous diagnosis of uterine fibroids. Gynecol. Endocrinol. 2019, 35, 207–210. [Google Scholar] [CrossRef]
- Calderon, L.; Netter, A.; Grob-Vaillant, A.; Mancini, J.; Siles, P.; Vidal, V.; Agostini, A. Progression of adenomyosis magnetic resonance imaging features under ulipristal acetate for symptomatic fibroids. Reprod. Biomed. Online 2021, 42, 661–668. [Google Scholar] [CrossRef]
- Maggi, R.; Cariboni, A.M.; Marelli, M.M.; Moretti, R.M.; Andrè, V.; Marzagalli, M.; Limonta, P. GnRH and GnRH receptors in the pathophysiology of the human female reproductive system. Hum. Reprod. Update 2016, 22, 358–381. [Google Scholar] [CrossRef] [PubMed]
- Grow, D.R.; Filer, R.B. Treatment of adenomyosis with long-term GnRH analogues: A case report. Obstet. Gynecol. 1991, 78, 538–539. [Google Scholar] [PubMed]
- Nelson, J.R.; Corson, S.L. Long-term management of adenomyosis with a gonadotropin-releasing hormone agonist: A case report. Fertil. Steril. 1993, 59, 441–443. [Google Scholar] [CrossRef]
- Imaoka, I.; Ascher, S.M.; Sugimura, K.; Takahashi, K.; Li, H.; Cuomo, F.; Simon, J.; Arnold, L.L. MR imaging of diffuse adenomyosis changes after GnRH analog therapy. J. Magn. Reason. Imaging 2002, 15, 285–290. [Google Scholar] [CrossRef]
- Morelli, M.; Rocca, M.L.; Venturella, R.; Mocciaro, R.; Zullo, F. Improvement in chronic pelvic pain after gonadotropin releasing hormone analogue (GnRH-a) administration in premenopausal women suffering from adenomyosis or endometriosis. A retrospective study. Gynecol. Endocrinol. 2013, 29, 305–308. [Google Scholar] [CrossRef]
- Sauerbrun-Cutler, M.T.; Alvero, R. Short- and long-term impact of gonadotropin-releasing hormone analogue treatment on bone loss and fracture. Fertil. Steril. 2019, 112, 799–803. [Google Scholar] [CrossRef] [PubMed]
- Surrey, E.S. Add-back therapy and gonadotropin-releasing hormone agonists in the treatment of patients with endometriosis: Can a consensus be reached? Add-Back Consensus Working Group. Fertil. Steril. 1999, 71, 420–424. [Google Scholar] [CrossRef]
- Niu, Z.; Chen, Q.; Sun, Y.; Feng, Y. Long-term pituitary downregulation before frozen embryo transfer could improve pregnancy outcomes in women with adenomyosis. Gynecol. Endocrinol. 2013, 29, 1026–1030. [Google Scholar] [CrossRef] [PubMed]
- Donnez, O.; Donnez, J. P-299 Efficacy and safety of linzagolix for the treatment of severe adenomyosis. Initial results from a pilot study. Hum. Reprod. 2021, 36, deab130.298. [Google Scholar] [CrossRef]
- Donnez, J.; Stratopoulou, C.A.; Dolmans, M.-M. Uterine Adenomyosis: From Disease Pathogenesis to a New Medical Approach Using GnRH Antagonists. Int. J. Environ. Res. Public Health 2021, 18, 9941. [Google Scholar] [CrossRef]
- Donnez, J.; Donnez, O.; Brethous, M.; Bestel, E.; Garner, E.; Charpentier, S.; Humberstone, A.; Loumaye, E. Treatment of symptomatic uterine adenomyosis with linzagolix, an oral gonadotropin-releasing hormone receptor antagonist: A pilot study. Reprod. Biomed. Online 2021. [Google Scholar] [CrossRef]
- Borini, A.; Coticchio, G. Gonadotropin-releasing hormone antagonist linzagolix: Possible treatment for assisted reproduction patients presenting with adenomyosis and endometriosis? Fertil. Steril. 2020, 114, 517–518. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Dolmans, M.M. Hormone therapy for intramural myoma-related infertility from ulipristal acetate to GnRH antagonist: A review. Reprod. Biomed. Online 2020, 41, 431–442. [Google Scholar] [CrossRef]
- Taylor, H.S.; Giudice, L.C.; Lessey, B.A.; Abrao, M.S.; Kotarski, J.; Archer, D.F.; Diamond, M.P.; Surrey, E.; Johnson, N.P.; Watts, N.B.; et al. Treatment of Endometriosis-Associated Pain with Elagolix, an Oral GnRH Antagonist. N. Engl. J. Med. 2017, 377, 28–40. [Google Scholar] [CrossRef]
- Abrao, M.S.; Surrey, E.; Gordon, K.; Snabes, M.C.; Wang, H.; Ijacu, H.; Taylor, H.S. Reductions in endometriosis-associated pain among women treated with elagolix are consistent across a range of baseline characteristics reflective of real-world patients. BMC Women’s Health 2021, 21, 246. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J.; Taylor, H.S.; Taylor, R.N.; Akin, M.D.; Tatarchuk, T.F.; Wilk, K.; Gotteland, J.P.; Lecomte, V.; Bestel, E. Treatment of endometriosis-associated pain with linzagolix, an oral gonadotropin-releasing hormone-antagonist: A randomized clinical trial. Fertil. Steril. 2020, 114, 44–55. [Google Scholar] [CrossRef]
- Diamond, M.P.; Carr, B.; Dmowski, W.P.; Koltun, W.; O’Brien, C.; Jiang, P.; Burke, J.; Jimenez, R.; Garner, E.; Chwalisz, K. Elagolix treatment for endometriosis-associated pain: Results from a phase 2, randomized, double-blind, placebo-controlled study. Reprod. Sci. 2014, 21, 363–371. [Google Scholar] [CrossRef]
- Osuga, Y.; Seki, Y.; Tanimoto, M.; Kusumoto, T.; Kudou, K.; Terakawa, N. Relugolix, an oral gonadotropin-releasing hormone (GnRH) receptor antagonist, in women with endometriosis-associated pain: Phase 2 safety and efficacy 24-week results. BMC Women’s Health 2021, 21, 250. [Google Scholar] [CrossRef]
- Donnez, J.; Dolmans, M.M.; Fellah, L. What if deep endometriotic nodules and uterine adenomyosis were actually two forms of the same disease? Fertil. Steril. 2019, 111, 454–456. [Google Scholar] [CrossRef]
- Stratopoulou, C.A.; Camboni, A.; Donnez, J.; Dolmans, M.-M. Identifying Common Pathogenic Features in Deep Endometriotic Nodules and Uterine Adenomyosis. J. Clin. Med. 2021, 10, 4585. [Google Scholar] [CrossRef]
- Singtripop, T.; Mori, T.; Park, M.K.; Sakamoto, S.; Kawashima, S. Development of uterine adenomyosis after treatment with dopamine antagonists in mice. Life Sci. 1991, 49, 201–206. [Google Scholar] [CrossRef]
- Yamashita, M.; Matsuda, M.; Mori, T. Increased expression of prolactin receptor mRNA in adenomyotic uterus in mice. Life Sci. 1997, 60, 1437–1446. [Google Scholar] [CrossRef]
- Andersson, J.K.; Khan, Z.; Weaver, A.L.; Vaughan, L.E.; Gemzell-Danielsson, K.; Stewart, E.A. Vaginal bromocriptine improves pain, menstrual bleeding and quality of life in women with adenomyosis: A pilot study. Acta Obstet. Gynecol. Scand. 2019, 98, 1341–1350. [Google Scholar] [CrossRef] [PubMed]
- Andersson, J.K.; Pozzi Mucelli, R.; Epstein, E.; Stewart, E.A.; Gemzell-Danielsson, K. Vaginal bromocriptine for treatment of adenomyosis. Impact on magnetic resonance imaging and transvaginal ultrasound. Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 254, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Auriemma, R.S.; Del Vecchio, G.; Scairati, R.; Pirchio, R.; Liccardi, A.; Verde, N.; de Angelis, C.; Menafra, D.; Pivonello, C.; Conforti, A.; et al. The Interplay Between Prolactin and Reproductive System: Focus on Uterine Pathophysiology. Front. Endocrinol. 2020, 11, 594370. [Google Scholar] [CrossRef]
- Kimura, F.; Takahashi, K.; Takebayashi, K.; Fujiwara, M.; Kita, N.; Noda, Y.; Harada, N. Concomitant treatment of severe uterine adenomyosis in a premenopausal woman with an aromatase inhibitor and a gonadotropin-releasing hormone agonist. Fertil. Steril. 2007, 87, 1468.e9–1468.e12. [Google Scholar] [CrossRef]
- Badawy, A.M.; Elnashar, A.M.; Mosbah, A.A. Aromatase inhibitors or gonadotropin-releasing hormone agonists for the management of uterine adenomyosis: A randomized controlled trial. Acta Obstet. Gynecol. Scand. 2012, 91, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Colette, S.; Donnez, J. Endometriosis. N. Engl. J. Med. 2009, 360, 1911–1912. [Google Scholar]
- Colette, S.; Lousse, J.C.; Defrère, S.; Curaba, M.; Heilier, J.F. Van Langendonckt, A.; Mestdagt, M.; Foidart, J.M.; Loumaye, E.; Donnez, J. Absence of aromatase protein and mRNA expression in endometriosis. Hum. Reprod. 2009, 24, 2133–2141. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kitawaki, J.; Noguchi, T.; Amatsu, T.; Maeda, K.; Tsukamoto, K.; Yamamoto, T.; Fushiki, S.; Osawa, Y.; Honjo, H. Expression of aromatase cytochrome P450 protein and messenger ribonucleic acid in human endometriotic and adenomyotic tissues but not in normal endometrium. Biol. Reprod. 1997, 57, 514–519. [Google Scholar] [CrossRef]
- Zhu, B.; Chen, Y.; Shen, X.; Liu, X.; Guo, S.W. Anti-platelet therapy holds promises in treating adenomyosis: Experimental evidence. Reprod. Biol. Endocrinol. 2016, 14, 66. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Shen, M.; Qi, Q.; Zhang, H.; Guo, S.W. Corroborating evidence for platelet-induced epithelial-mesenchymal transition and fibroblast-to-myofibroblast transdifferentiation in the development of adenomyosis. Hum. Reprod. 2016, 31, 734–749. [Google Scholar] [CrossRef]
- Mosele, S.; Stratopoulou, C.A.; Camboni, A.; Donnez, J.; Dolmans, M.M. Investigation of the role of platelets in the aetiopathogenesis of adenomyosis. Reprod. Biomed. Online 2021, 42, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Herndon, C.N.; Aghajanova, L.; Balayan, S.; Erikson, D.; Barragan, F.; Goldfien, G.; Vo, K.C.; Hawkins, S.; Giudice, L.C. Global Transcriptome Abnormalities of the Eutopic Endometrium From Women With Adenomyosis. Reprod. Sci. 2016, 23, 1289–1303. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.H.; Duan, H.; Wang, S.; Wang, Y.Y.; Lv, C.X. Upregulated microRNA let-7a accelerates apoptosis and inhibits proliferation in uterine junctional zone smooth muscle cells in adenomyosis under conditions of a normal activated hippo-YAP1 axis. Reprod. Biol. Endocrinol. 2021, 19, 81. [Google Scholar] [CrossRef]
- Wang, Y.Y.; Duan, H.; Wang, S.; Quan, Y.J.; Huang, J.H.; Guo, Z.C. Talin1 Induces Epithelial-Mesenchymal Transition to Facilitate Endometrial Cell Migration and Invasion in Adenomyosis Under the Regulation of microRNA-145-5p. Reprod. Sci. 2021, 28, 1523–1539. [Google Scholar] [CrossRef]
- Hu, H.; Li, H.; He, Y. MicroRNA-17 downregulates expression of the PTEN gene to promote the occurrence and development of adenomyosis. Exp. Ther. Med. 2017, 14, 3805–3811. [Google Scholar] [CrossRef]
- Yu, K.; Cui, S.; Xue, T. LncRNA MIR22HG is downregulated in adenomyosis and upregulates miR-2861 through demethylation to inhibit endometrial cell proliferation. J. Obstet. Gynaecol. Res. 2021, 47, 1837–1845. [Google Scholar] [CrossRef]
- Younes, G.; Tulandi, T. Effects of adenomyosis on in vitro fertilization treatment outcomes: A meta-analysis. Fertil. Steril. 2017, 108, 483. [Google Scholar] [CrossRef]
- Horton, J.; Sterrenburg, M.; Lane, S.; Maheshwari, A.; Li, T.C.; Cheong, Y. Reproductive, obstetric, and perinatal outcomes of women with adenomyosis and endometriosis: A systematic review and meta-analysis. Hum. Reprod. Update 2019, 25, 592–632. [Google Scholar] [CrossRef]
- Kissler, S.; Zangos, S.; Wiegratz, I.; Kohl, J.; Rody, A.; Gaetje, R.; Doebert, N.; Wildt, L.; Kunz, G.; Leyendecker, G.; et al. Utero-tubal sperm transport and its impairment in endometriosis and adenomyosis. Ann. N. Y. Acad. Sci. 2007, 1101, 38–48. [Google Scholar] [CrossRef]
- Nisolle, M.; Donnez, J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil. Steril. 1997, 68, 585–596. [Google Scholar] [CrossRef]
- Large, M.J.; DeMayo, F.J. The regulation of embryo implantation and endometrial decidualization by progesterone receptor signaling. Mol. Cell Endocrinol. 2012, 358, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Tremellen, K.P.; Russell, P. The distribution of immune cells and macrophages in the endometrium of women with recurrent reproductive failure. II: Adenomyosis and macrophages. J. Reprod. Immunol. 2012, 93, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Xie, M.; Yu, H.; Zhang, X.; Wang, W.; Ren, Y. Elasticity of adenomyosis is increased after GnRHa therapy and is associated with spontaneous pregnancy in infertile patents. J. Gynecol. Obstet. Hum. Reprod. 2019, 48, 849–853. [Google Scholar] [CrossRef]
- Hirata, J.D.; Moghissi, K.S.; Ginsburg, K.A. Pregnancy after medical therapy of adenomyosis with a gonadotropin-releasing hormone agonist. Fertil. Steril. 1993, 59, 444–445. [Google Scholar] [CrossRef]
- Silva, P.D.; Perkins, H.E.; Schauberger, C.W. Live birth after treatment of severe adenomyosis with a gonadotropin-releasing hormone agonist. Fertil. Steril. 1994, 61, 171–172. [Google Scholar] [CrossRef]
- Agrawala, S.; Patil, J.; Campbell, S.; Woodard, T.L. A rare case of extensive placenta accreta in twin pregnancy after GnRH agonist treatment of adenomyosis. Fertil. Res. Pract. 2021, 7, 5. [Google Scholar] [CrossRef]
- Park, C.W.; Choi, M.H.; Yang, K.M.; Song, I.O. Pregnancy rate in women with adenomyosis undergoing fresh or frozen embryo transfer cycles following gonadotropin-releasing hormone agonist treatment. Clin. Exp. Reprod. Med. 2016, 43, 169–173. [Google Scholar] [CrossRef]
- Al Jama, F.E. Management of adenomyosis in subfertile women and pregnancy outcome. Oman. Med. J. 2011, 26, 178–181. [Google Scholar] [CrossRef]
- Huang, B.S.; Seow, K.M.; Tsui, K.H.; Huang, C.Y.; Lu, Y.F.; Wang, P.H. Fertility outcome of infertile women with adenomyosis treated with the combination of a conservative microsurgical technique and GnRH agonist: Long-term follow-up in a series of nine patients. Taiwan J. Obstet. Gynecol. 2012, 51, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Lan, J.; Wu, Y.; Wu, Z.; Wu, Y.; Yang, R.; Liu, Y.; Lin, H.; Jiao, X.; Zhang, Q. Ultra-Long GnRH Agonist Protocol During IVF/ICSI Improves Pregnancy Outcomes in Women With Adenomyosis: A Retrospective Cohort Study. Front. Endocrinol. 2021, 12, 609771. [Google Scholar] [CrossRef] [PubMed]
- Hou, X.; Xing, J.; Shan, H.; Mei, J.; Sun, Y.; Yan, G.; Sun, H.; Wang, J. The effect of adenomyosis on IVF after long or ultra-long GnRH agonist treatment. Reprod. Biomed. Online 2020, 41, 845–853. [Google Scholar] [CrossRef]
- Hyams, L.L. Adenomyosis; its conservative surgical treatment (hysteroplasty) in young women. N. Y. State J. Med. 1952, 52, 2778–2784. [Google Scholar] [PubMed]
- Osada, H. Uterine adenomyosis and adenomyoma: The surgical approach. Fertil. Steril. 2018, 109, 406–417. [Google Scholar] [CrossRef]
- Fujishita, A.H.K.; Kitajima, M.; Matsumoto, Y.; Satoh, H.; Masuzaki, H. Shikyusenkinsho to shikyu no onzon-chiryo. Uterine adenomyosis and uterine preservation treatment. J. Obstet. Gynecol. Pract. 2010, 59, 769–776. [Google Scholar]
- Osada, H.; Silber, S.; Kakinuma, T.; Nagaishi, M.; Kato, K.; Kato, O. Surgical procedure to conserve the uterus for future pregnancy in patients suffering from massive adenomyosis. Reprod. Biomed. Online 2011, 22, 94–99. [Google Scholar] [CrossRef]
- Osada, H.; Teramoto, S. Shikyukin furappuho niyoru shikyu-senkinsho tekishutsujutsu: Rinshoteki choki-yogo oyobi shikyuharetsu-yobokoka no kento. Adenomyomectomy by uterine muscle flap method: Clinical outcome and investigation of the preventive effect on uterine rupture. Obstet. Gynecol. 2017, 84, 1303–1315. [Google Scholar]
- Nishida, M.; Takano, K.; Arai, Y.; Ozone, H.; Ichikawa, R. Conservative surgical management for diffuse uterine adenomyosis. Fertil. Steril. 2010, 94, 715–719. [Google Scholar] [CrossRef]
- Nishida, M.O.Y.; Ichikawa, Y.; Arai, Y.; Sakanaka, S. Shikyusenkinsho-kakushutsujutsu-go ninshin-ji no shikyuharetsu-yobo ni tsuite (Prevention of uterine rupture during pregnancy after adenomyomectomy). Obstet. Gynecol. Surg. 2016, 27, 69–76. [Google Scholar]
- De Bruijn, A.M.; Smink, M.; Lohle, P.N.M.; Huirne, J.A.F.; Twisk, J.W.R.; Wong, C.; Schoonmade, L.; Hehenkamp, W.J.K. Uterine Artery Embolization for the Treatment of Adenomyosis: A Systematic Review and Meta-Analysis. J. Vasc. Interv. Radiol. 2017, 28, 1629. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Brown, B.; Liang, E. Long-term durability of uterine artery embolisation for treatment of symptomatic adenomyosis. Aust. N. Z. J. Obstet. Gynaecol. 2021, 61, 290–296. [Google Scholar] [CrossRef] [PubMed]
| Medication | Advantages | Drawbacks |
|---|---|---|
| NSAIDs | Effective against mild pain | Extensive use linked to side effects |
| Non-hormonal composition | Inability to treat underlying causes of pain | |
| Safe for women wishing to conceive | Questionable effectiveness against HMB | |
| COCs | Relatively effective in relieving pain | Limited efficacy in reducing HMB and uterine volume |
| Fewer side effects than other drugs | Risk of thromboembolic events | |
| Progestins | Alleviate local hyperestrogenism | Ineffective in about one-third of patients |
| Relieve pain symptoms | Frequently cause metrorrhagia at varying severity | |
| Possibility of long-term symptom management | Doubtful efficacy in diminishing uterine volume | |
| Ample evidence in favor of LNG-IUD use | ||
| UPA | Lower serum estradiol levels | Numerous reports of symptom and imaging feature exacerbation |
| May reduce HMB | Limited to restricted indications by the European Medicines Agency | |
| GnRH agonists | Alleviate pain | Flare-up effect |
| Induce amenorrhea | Severe hypoestrogenic side-effects (i.e., vasomotor syndrome, loss of BMD) | |
| Reduce uterine volume and JZ thickness | Long-term administration not indicated even with add-back therapy | |
| Beneficial as pre-treatment in infertile patients | ||
| GnRH antagonists | Easy and tolerable oral administration | Loss of BMD at high doses |
| Rapid action skipping initial flare-up | Less efficient when combined with add-back medication | |
| Effectively reduce HMB and pain symptoms | ||
| Dose-dependent estradiol suppression with less severe side-effects |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stratopoulou, C.A.; Donnez, J.; Dolmans, M.-M. Conservative Management of Uterine Adenomyosis: Medical vs. Surgical Approach. J. Clin. Med. 2021, 10, 4878. https://doi.org/10.3390/jcm10214878
Stratopoulou CA, Donnez J, Dolmans M-M. Conservative Management of Uterine Adenomyosis: Medical vs. Surgical Approach. Journal of Clinical Medicine. 2021; 10(21):4878. https://doi.org/10.3390/jcm10214878
Chicago/Turabian StyleStratopoulou, Christina Anna, Jacques Donnez, and Marie-Madeleine Dolmans. 2021. "Conservative Management of Uterine Adenomyosis: Medical vs. Surgical Approach" Journal of Clinical Medicine 10, no. 21: 4878. https://doi.org/10.3390/jcm10214878
APA StyleStratopoulou, C. A., Donnez, J., & Dolmans, M.-M. (2021). Conservative Management of Uterine Adenomyosis: Medical vs. Surgical Approach. Journal of Clinical Medicine, 10(21), 4878. https://doi.org/10.3390/jcm10214878








