Face-Down Posture versus Non-Face-Down Posture following Large Idiopathic Macular Hole Surgery: A Systemic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis and Statistical Analyses
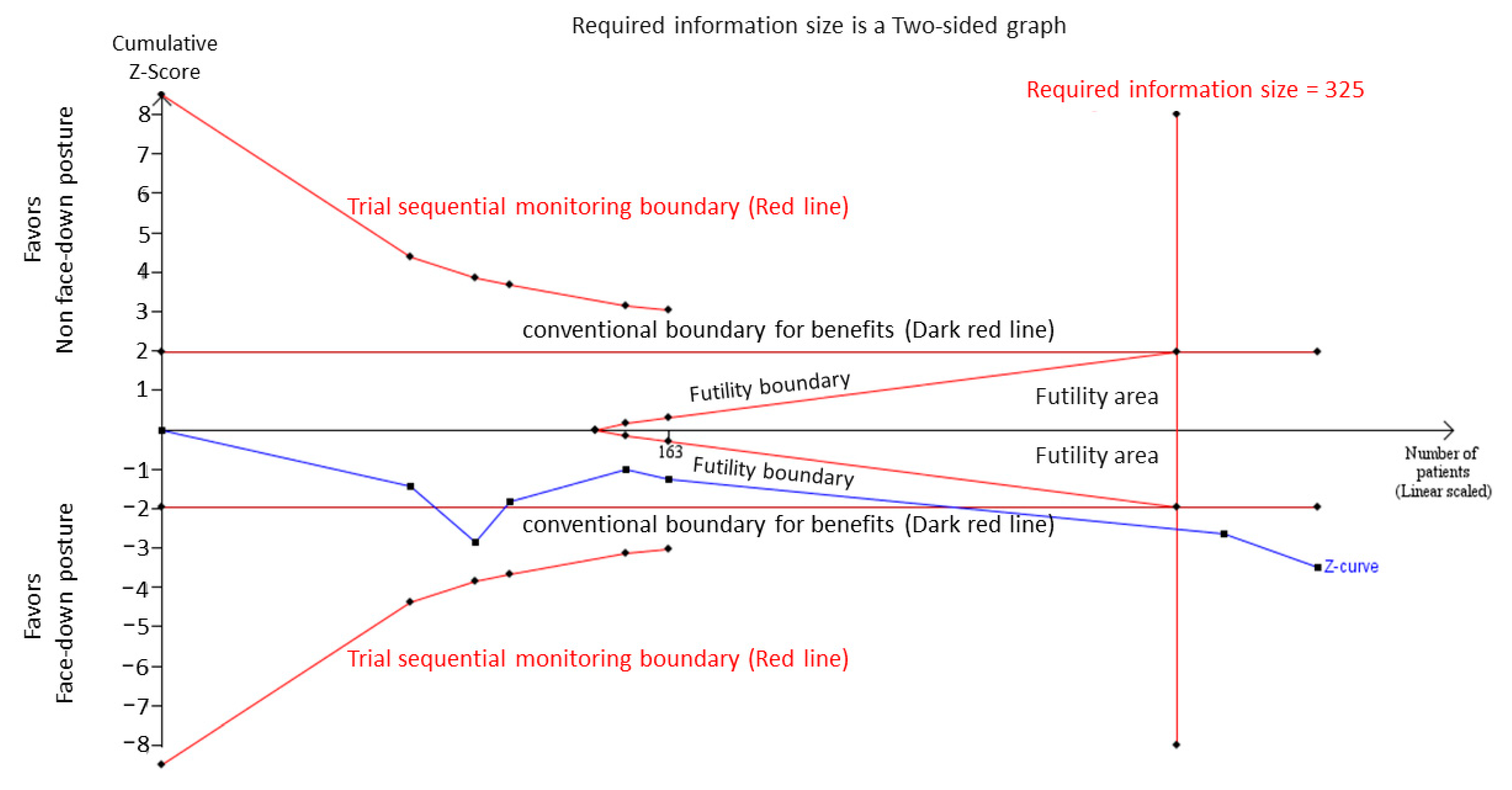
2.7. Trial Sequential Analysis
2.8. Grading of Certainty of Evidence
3. Results
3.1. Search Results
3.2. Study Characteristics
3.3. Risk-of-Bias Assessment
3.4. Pooled Effects of the Large IMH Closure Rate
3.5. Subgroup Analysis
3.6. Trial Sequential Analysis
3.7. Pooled Effects of the Visual Acuity Improved Rate
3.8. Publication Bias
3.9. GRADE Approach for CoE
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Forsaa, V.A.; Lindtjørn, B.; Kvaløy, J.T.; Frøystein, T.; Krohn, J. Epidemiology and morphology of full-thickness macular holes. Acta Ophthalmol. 2018, 96, 397–404. [Google Scholar] [CrossRef] [Green Version]
- Tranos, P.G.; Peter, N.M.; Nath, R.K.; Singh, M.K.; Dimitrakos, S.; Charteris, D.G.; Kon, C. Macular hole surgery without prone positioning. Eye 2007, 21, 802–806. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smiddy, W.E.; Flynn, H.W. Pathogenesis of macular holes and therapeutic implications. Am. J. Ophthalmol. 2004, 137, 525–537. [Google Scholar] [CrossRef] [PubMed]
- Hisatomi, T.; Enaida, H.; Sakamoto, T.; Kanemaru, T.; Kagimoto, T.; Yamanaka, I.; Ueno, A.; Nakamura, T.; Hata, Y.; Ishibashi, T. Cellular migration associated with macular hole: A new method for comprehensive bird’s-eye analysis of the internal limiting membrane. Arch Ophthalmol. 2006, 124, 1005–1011. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, N.E.; Wendel, R.T. Vitreous Surgery for Idiopathic Macular Holes: Results of a Pilot Study. Arch Ophthalmol. 1991, 109, 654–659. [Google Scholar] [CrossRef]
- Stone, T.W. (Ed.) ASRS 2018 Preferences and Trends Membership Survey; American Society of Retina Specialists: Vancouver, BC, USA, 2018. [Google Scholar]
- Ciulla, T.A.; Frederick, A.R., Jr.; Kelly, C.; Amrein, R. Postvitrectomy positioning complicated by ulnar nerve palsy. Am. J. Ophthalmol. 1996, 122, 739–740. [Google Scholar] [CrossRef]
- Brill, D.A.; Fields, T.S.; Badami, A.U.; Kuley, A.J.; Kumar, N.; Desai, U.R. Bilateral pulmonary emboli following macular hole surgery with postoperative prone positioning. Am. J. Ophthalmol. Case Rep. 2019, 15, 100478. [Google Scholar] [CrossRef]
- Treister, G.; Wygnanski, T. Pressure sore in a patient who underwent repair of a retinal tear with gas injection. Graefes. Arch. Clin. Exp. Ophthalmol. 1996, 234, 657–658. [Google Scholar] [CrossRef]
- Tadayoni, R.; Vicaut, E.; Devin, F.; Creuzot-Garcher, C.; Berrod, J.-P.; Le Mer, Y.; Korobelnik, J.-F.; Aout, M.; Massin, P.; Gaudric, A. A Randomized Controlled Trial of Alleviated Positioning after Small Macular Hole Surgery. Ophthalmology 2011, 118, 150–155. [Google Scholar] [CrossRef]
- Guillaubey, A.; Malvitte, L.; Lafontaine, P.O.; Jay, N.; Hubert, I.; Bron, A.; Berrod, J.P.; Creuzot-Garcher, C. Comparison of Face-Down and Seated Position After Idiopathic Macular Hole Surgery: A Randomized Clinical Trial. Am. J. Ophthalmol. 2008, 146, 128–134.e1. [Google Scholar] [CrossRef] [Green Version]
- Lange, C.A.K.; Membrey, L.; Ahmad, N.; Wickham, L.; E MacLaren, R.; Solebo, L.; Xing, W.; Bunce, C.; Ezra, E.; Charteris, D.; et al. Pilot randomised controlled trial of face-down positioning following macular hole surgery. Eye 2011, 26, 272–277. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Chen, X.; Hong, L.; Yan, Y.; Zeng, M.; Huang, Z.; Liu, R.; Ding, Q. Facedown positioning after vitrectomy will not facilitate macular hole closure based on swept-source optical coherence tomography imaging in gas-filled eyes: A prospective, randomized comparative interventional study. Retina 2019, 39, 2353–2359. [Google Scholar] [CrossRef]
- Ye, T.; Yu, J.-G.; Liao, L.; Liu, L.; Xia, T.; Yang, L.-L. Macular hole surgery recovery with and without face-down posturing: A meta-analysis of randomized controlled trials. BMC Ophthalmol. 2019, 19, 265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, Z.; Xie, P.; Ding, Y.; Zheng, X.; Yuan, D.; Liu, Q. Face-down or no face-down posturing following macular hole surgery: A meta-analysis. Acta Ophthalmol. 2016, 94, 326–333. [Google Scholar] [CrossRef]
- Solebo, A.L.; Lange, C.A.; Bunce, C.; Bainbridge, J. Face-down positioning or posturing after macular hole surgery. Cochrane Database Syst. Rev. 2011, 12, CD008228. [Google Scholar] [CrossRef]
- Kang, H. Trial sequential analysis: Novel approach for meta-analysis. Anesthesia Pain Med. 2021, 16, 138–150. [Google Scholar] [CrossRef]
- Xia, S.; Zhao, X.-Y.; Wang, E.-Q.; Chen, Y.-X. Comparison of face-down posturing with nonsupine posturing after macular hole surgery: A meta-analysis. BMC Ophthalmol. 2019, 19, 34. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2020. [Google Scholar]
- Translator Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duker, J.S.; Kaiser, P.; Binder, S.; de Smet, M.; Gaudric, A.; Reichel, E.; Sadda, S.R.; Sebag, J.; Spaide, R.F.; Stalmans, P. The International Vitreomacular Traction Study Group Classification of Vitreomacular Adhesion, Traction, and Macular Hole. Ophthalmology 2013, 120, 2611–2619. [Google Scholar] [CrossRef]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid.-Based Heal. 2018, 16, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Brok, J.; Thorlund, K.; Wetterslev, J.; Gluud, C. Apparently conclusive meta-analyses may be inconclusive—Trial sequential analysis adjustment of random error risk due to repetitive testing of accumulating data in apparently conclusive neonatal meta-analyses. Int. J. Epidemiol. 2009, 38, 287–298. [Google Scholar] [CrossRef]
- Thorlund, K.; Devereaux, P.; Wetterslev, J.; Guyatt, G.; A Ioannidis, J.P.; Thabane, L.; Gluud, L.L.; Als-Nielsen, B.; Gluud, C. Can trial sequential monitoring boundaries reduce spurious inferences from meta-analyses? Int. J. Epidemiol. 2009, 38, 276–286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wetterslev, J.; Thorlund, K.; Brok, J.; Gluud, C. Estimating required information size by quantifying diversity in random-effects model meta-analyses. BMC Med Res. Methodol. 2009, 9, 86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wetterslev, J.; Thorlund, K.; Brok, J.; Gluud, C. Trial sequential analysis may establish when firm evidence is reached in cumula-tive meta-analysis. J. Clin. Epidemiol. 2008, 61, 64–75. [Google Scholar] [CrossRef]
- Pasu, S.; Bell, L.; Zenasni, Z.; Lanz, D.; Simmonds, I.A.; Thompson, A.; Yorston, D.; Laidlaw, D.A.H.; Bunce, C.; Hooper, R.; et al. Facedown positioning following surgery for large full-thickness macular hole: A multicenter randomized clinical trial. JAMA Ophthalmol. 2020, 138, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [Green Version]
- Yorston, D.; Siddiqui, M.A.R.; A Awan, M.; Walker, S.; Bunce, C.; Bainbridge, J. Pilot randomised controlled trial of face-down posturing following phacovitrectomy for macular hole. Eye 2011, 26, 267–271. [Google Scholar] [CrossRef] [Green Version]
- Veith, M.; Vránová, J.; Němčanský, J.; Studnička, J.; Penčák, M.; Straňák, Z.; Mojžíš, P.; Studený, P.; Piñero, D.P. Surgical treatment of idiopathic macular hole using different types of tamponades and different postoperative positioning regimens. J. Ophthalmol. 2020, 2020, 8858317. [Google Scholar] [CrossRef]
- Alberti, M.; la Cour, M. Nonsupine positioning in macular hole surgery: A noninferiority randomized clini-cal trial. Retina 2016, 36, 2072–2079. [Google Scholar] [CrossRef]
- Castellini, G.; Bruschettini, M.; Gianola, S.; Gluud, C.; Moja, L. Assessing imprecision in Cochrane systematic reviews: A com-parison of GRADE and Trial Sequential Analysis. Syst Rev. 2018, 7, 110. [Google Scholar] [CrossRef] [Green Version]
- Steel, D.H.; A Madi, H.; Masri, I. Optimal management of idiopathic macular holes. Clin. Ophthalmol. 2016, 10, 97–116. [Google Scholar] [CrossRef] [Green Version]
- Berger, J.W.; Brucker, A.J. The magnitude of the bubble buoyant pressure: Implications for macular hole surgery. Retina 1998, 18, 84–86. [Google Scholar] [CrossRef]
- Shah, S.P.; Manjunath, V.; Rogers, A.H.; Baumal, C.R.; Reichel, E.; Duker, J.S. Optical coherence tomography–guided facedown positioning for macular hole surgery. Retina 2013, 33, 356–362. [Google Scholar] [CrossRef] [Green Version]
- Chow, D.R.; Chaudhary, K.M. Optical coherence tomography–based positioning regimen for macular hole surgery. Retina 2015, 35, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Foster, W.; Chou, T. Physical mechanisms of gas and perfluoron retinopexy and sub-retinal fluid displacement. Phys. Med. Biol. 2004, 49, 2989–2997. [Google Scholar] [CrossRef] [Green Version]
- Stopa, M.; Lincoff, A.; Lincoff, H. Analysis of forces acting upon submacular hemorrhage in pneumatic displacement. Retina 2007, 27, 370–374. [Google Scholar] [CrossRef]
- Mendes, D.; Alves, C.; Batel-Marques, F. Number needed to treat (NNT) in clinical literature: An appraisal. BMC Med. 2017, 15, 112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Citrome, L. Quantifying Clinical Relevance. Innov. Clin. Neurosci. 2014, 11, 26–30. [Google Scholar]
- Ittarat, M.; Somkijrungroj, T.; Chansangpetch, S.; Pongsachareonnont, P. Literature Review of Surgical Treatment in Idiopathic Full-Thickness Macular Hole. Clin. Ophthalmol. 2020, 14, 2171–2183. [Google Scholar] [CrossRef]
- Kusuhara, S.; Escaño, M.F.T.; Fujii, S.; Nakanishi, Y.; Tamura, Y.; Nagai, A.; Yamamoto, H.; Tsukahara, Y.; Negi, A. Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am. J. Ophthalmol. 2004, 138, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Michalewska, Z.; Michalewski, J.; Cisiecki, S.; Adelman, R.; Nawrocki, J. Correlation between foveal structure and visual outcome following macular hole surgery: A spectral optical coherence tomography study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2008, 246, 823–830. [Google Scholar] [CrossRef] [PubMed]
- Michalewska, Z.; Michalewski, J.; Adelman, R.A.; Nawrocki, J. Inverted Internal Limiting Membrane Flap Technique for Large Macular Holes. Ophthalmology 2010, 117, 2018–2025. [Google Scholar] [CrossRef]
- Chang, Y.-C.; Lin, W.-N.; Chen, K.-J.; Wu, H.-J.; Lee, C.-L.; Chen, C.-H.; Wu, K.-Y.; Wu, W.-C. Correlation Between the Dynamic Postoperative Visual Outcome and the Restoration of Foveal Microstructures After Macular Hole Surgery. Am. J. Ophthalmol. 2015, 160, 100–106.e1. [Google Scholar] [CrossRef]
- Oh, J.; Smiddy, W.E.; Flynn, H.W., Jr.; Gregori, G.; Lujan, B. Photoreceptor inner/outer segment defect imaging by spectral domain OCT and visual prognosis after macular hole surgery. Investig. Ophthalmol. Vis. Sci. 2010, 51, 1651–1658. [Google Scholar] [CrossRef] [Green Version]
- Kaźmierczak, K.; Stafiej, J.; Stachura, J.; Żuchowski, P.; Malukiewicz, G. Long-term anatomic and functional outcomes after mac-ular hole surgery. J. Ophthalmol. 2018, 2018, 3082194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Purtskhvanidze, K.; Treumer, F.; Junge, O.; Hedderich, J.; Roider, J.; Hillenkamp, J. The long-term course of functional and ana-tomical recovery after macular hole surgery. Investig. Ophthalmol. Vis. Sci. 2013, 54, 4882–4891. [Google Scholar] [CrossRef] [Green Version]


| Study (First Author, Year) | Country | Study Design | Posturing Protocol | Gas Use | ILM Peeling | Number of Cases | Mean Age (Years) | MH Size | Definition of Visual Acuity Improvement | Follow-Up Periods | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FDP | nFDP | <400 µm (F/N) | >400 µm (F/N) | |||||||||
| Alberti, 2016 [32] | Denmark | RCT | 3 days; 16 h/day | C3F8 | Yes | 68 | 69.8 | 69.3 | 18/13 | 16/21 | ≥15 letters (ETDRS) gain | 3 months |
| Guillaubey, 2008 [11] | France | RCT | 5 days; 8 h/day | C3F8, C2F8, SF6 | Yes | 150 | 69.0 | 68.0 | 37/33 | 41/39 | NA | 6 months |
| Lange, 2012 [12] | UK | RCT | 10 days; 50 min/h | C3F8 | Yes | 30 | 66.8 | 71.0 | 4/5 | 11/10 | ≥0.2 logMAR units gain | 6–8 weeks |
| Pasu, 2020 [28] | UK | RCT | 5 days; 8 h/day | C3F8 | Yes | 178 | 69 | 69 | NA | 90/88 | ≥0.3 logMAR units gain | 3 months |
| Veith, 2020 [31] | Spain | RCT | 3 days; 24 h/day | Air | Yes | 51 | 69.2 | 71.3 | 12/9 | 14/16 | NA | 6 months |
| Yorston, 2012 [30] | UK | RCT | 10 days; 50 min/h | C3F8 | Yes | 30 | 71.1 | 68.0 | 10/9 | 6/5 | ≥6/18 (Snellen) | 6 months |
| Zhang, 2018 [13] | China | RCT | 3 days; 16 h/day | C3F8 | Yes | 80 | 62.35 | 62.85 | 33/33 | 7/7 | NA | 3 months |
| Large IMH Closure Rate | ||||
|---|---|---|---|---|
| Subgroups | No. of Trials | Pooled OR (95% CI) | p-Value | I2 (%) |
| Posturing periods | ||||
| ≤3 days | 3 | 1.76 (0.32 to 9.70) | 0.52 | 22.21 |
| ≥5 days | 4 | 4.05 (1.60 to 10.22) | <0.01 * | 9.30 |
| Follow-up periods | ||||
| ≤3 months | 4 | 2.91 (0.71 to 11.98) | 0.14 | 30.73 |
| ≥6 months | 3 | 3.51 (1.18 to 10.39) | 0.02 * | 3.22 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, H.-R.; Chen, T.-L.; Chang, C.-Y.; Huang, H.-K.; Lee, Y.-C. Face-Down Posture versus Non-Face-Down Posture following Large Idiopathic Macular Hole Surgery: A Systemic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 4895. https://doi.org/10.3390/jcm10214895
Tsai H-R, Chen T-L, Chang C-Y, Huang H-K, Lee Y-C. Face-Down Posture versus Non-Face-Down Posture following Large Idiopathic Macular Hole Surgery: A Systemic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(21):4895. https://doi.org/10.3390/jcm10214895
Chicago/Turabian StyleTsai, Hou-Ren, Tai-Li Chen, Chun-Yu Chang, Huei-Kai Huang, and Yuan-Chieh Lee. 2021. "Face-Down Posture versus Non-Face-Down Posture following Large Idiopathic Macular Hole Surgery: A Systemic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 21: 4895. https://doi.org/10.3390/jcm10214895






