Immediate Implants in the Aesthetic Zone: Is Socket Shield Technique a Predictable Treatment Option? A Narrative Review
Abstract
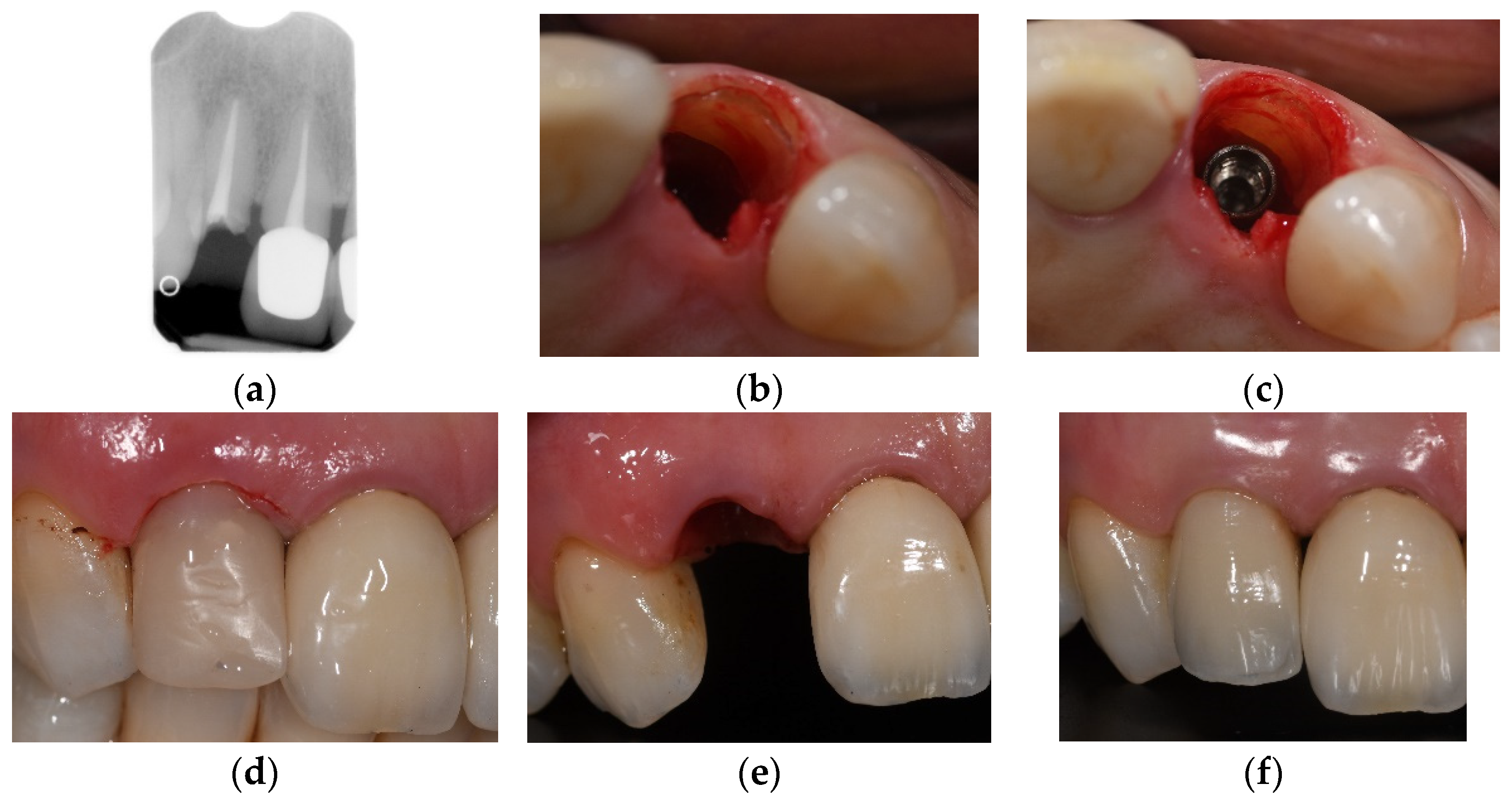
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
4.1. Implant Failure and Marginal Bone Loss
4.2. Root Fragment Exposure
4.3. Bone Grafts and the Socket-Shield Technique
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fickl, S.; Zuhr, O.; Wachtel, H.; Stappert, C.F.J.; Stein, J.M.; Hürzeler, M.B. Dimensional changes of the alveolar ridge contour after different socket preservation techniques. J. Clin. Periodontol. 2008, 35, 906–913. [Google Scholar] [CrossRef]
- Schropp, L.; Wenzel, A.; Kostopoulos, L.; Karring, T. Bone healing and soft tissue contour changes following single-tooth extraction: A clinical and radiographic 12-month prospective study. Int. J. Periodontics Restor. Dent. 2003, 23, 313–323. [Google Scholar]
- Araujo, M.G.; Lindhe, J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 212–218. [Google Scholar] [CrossRef]
- Cardaropoli, G.; Araujo, M.; Hayacibara, R.; Sukekava, F.; Lindhe, J. Healing of extraction sockets and surgically pro-duced-augmented and non-augmented-defects in the alveolar ridge. An experimental study in the dog. J. Clin. Periodontol. 2005, 32, 435–440. [Google Scholar] [CrossRef]
- Botticelli, D.; Berglundh, T.; Lindhe, J. Hard-tissue alterations following immediate implant placement in extraction sites. J. Clin. Periodontol. 2004, 31, 820–828. [Google Scholar] [CrossRef] [PubMed]
- Araújo, M.; Linder, E.; Wennström, J.; Lindhe, J. The influence of Bio-Oss Collagen on healing of an extraction socket: An experimental study in the dog. Int. J. Periodontics Restor. Dent. 2008, 28, 123–135. [Google Scholar]
- Lekovic, V.; Kenney, E.B.; Weinlaender, M.; Han, T.; Klokkevold, P.; Nedic, M.; Orsini, M. A Bone Regenerative Approach to Alveolar Ridge Maintenance Following Tooth Extraction. Report of 10 Cases. J. Periodontol. 1997, 68, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Colombo, E.; Zekiy, A.; Aicardi, S.; Benedicenti, S.; De Angelis, N. Interaction between Laser Light and Osteoblasts: Photobiomodulation as a Trend in the Management of Socket Bone Preservation—A Review. Biology 2020, 9, 409. [Google Scholar] [CrossRef] [PubMed]
- Covani, U.; Giammarinaro, E.; Marconcini, S.; Aizcorbe-Vicente, J.; Peñarrocha-Diago, M. Diagnosis and Planning in Immediate Loading: Implant Selection. In Atlas of Immediate Dental Implant Loading; Peñarrocha-Diago, M., Covani, U., Cuadrado, L., Eds.; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Braut, V.; Bornstein, M.M.; Belser, U.; Buser, D. Thickness of the anterior maxillary facial bone wall-a retrospective radiographic study using cone beam computed tomography. Int. J. Periodontics Restor. Dent. 2011, 31, 125–131. [Google Scholar]
- Januário, A.L.; Duarte, W.R.; Barriviera, M.; Mesti, J.C.; Araújo, M.G.; Lindhe, J. Dimension of the facial bone wall in the anterior maxilla: A cone-beam computed tomography study. Clin. Oral Implant. Res. 2011, 22, 1168–1171. [Google Scholar] [CrossRef] [PubMed]
- Botelho, S.V.; Perussolo, J.; Misawa, M.Y.; Zadeh, H.H.; Araújo, M.G. The Basal Bone and Alveolar Process in the Maxillary Anterior Region in Humans: A Cone Beam Computed Tomographic Study. Int. J. Periodontics Restor. Dent. 2020, 40, 907–914. [Google Scholar] [CrossRef] [PubMed]
- Misawa, M.; Lindhe, J.; Araújo, M.G. The alveolar process following single-tooth extraction: A study of maxillary incisor and premolar sites in man. Clin. Oral Implant. Res. 2015, 27, 884–889. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, N.; Felice, P.; Pellegrino, G.; Camurati, A.; Gambino, P.; Esposito, M. Guided bone regeneration with and without a bone substitute at single post-extractive implants: 1-year post-loading results from a pragmatic multicentre randomised controlled trial. Eur. J. Oral Implantol. 2011, 4, 313–325. [Google Scholar] [PubMed]
- Fickl, S.; Schneider, D.; Zuhr, O.; Hinze, M.; Ender, A.; Jung, R.E.; Hürzeler, M.B. Dimensional changes of the ridge contour after socket preservation and buccal overbuilding: An animal study. J. Clin. Periodontol. 2009, 36, 442–448. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Studer, S.P.; Lehner, C.; Bucher, A.; Schärer, P. Soft tissue correction of a single-tooth pontic space: A comparative quantitative volume assessment. J. Prosthet. Dent. 2000, 83, 402–411. [Google Scholar] [CrossRef]
- Esposito, M.; Grusovin, M.G.; Felice, P.; Karatzopoulos, G.; Worthington, H.V.; Coulthard, P. The Efficacy of Horizontal and Vertical Bone Augmentation Procedures for Dental Implants: A Cochrane Systematic Review. Evid.-Based Pract. Towar. Optim. Clin. Outcomes 2010, 2, 195–218. [Google Scholar] [CrossRef]
- Andersson, L.; Emami-Kristiansen, Z.; Högström, J. Single-tooth implant treatment in the anterior region of the maxilla for treatment of tooth loss after trauma: A retrospective clinical and interview study. Dent. Traumatol. 2003, 19, 126–131. [Google Scholar] [CrossRef]
- Sapir, S.; Shapira, J. Decoronation for the management of an ankylosed young permanent tooth. Dent. Traumatol. 2008, 24, 131–135. [Google Scholar] [CrossRef]
- Filippi, A.; Pohl, Y.; Von Arx, T. Decoronation of an ankylosed tooth for preservation of alveolar bone prior to implant placement. Dent. Traumatol. 2001, 17, 93–95. [Google Scholar] [CrossRef]
- Hürzeler, M.B.; Zuhr, O.; Schupbach, P.; Rebele, S.F.; Emmanouilidis, N.; Fickl, S. The socket-shield technique: A proof-of-principle report. J. Clin. Periodontol. 2010, 37, 855–862. [Google Scholar] [CrossRef]
- Abadzhiev, M.; Nenko, P.; Velcheva, P. Conventional immediate implant placement and immediate placement with sock-et-shield technique—Which is better. Int. J. Clin. Med. Res. 2014, 1, 176–180. [Google Scholar]
- Msc, A.A.; Shaheen, M.; Askar, N.; Atef, M. Socket shield technique vs. conventional immediate implant placement with immediate temporization. Randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2020, 22, 602–611. [Google Scholar] [CrossRef]
- Abitbol, J.; Antoun, H.; Degorce, T. Implant insertion after tooth extraction: Clinical outcomes with different approaches (including socket preservation, immediate, early and delayed placement). Clin. Oral Implants Res. 2016, 27, 530. [Google Scholar]
- Aslan, S. Improved volume and contour stability with thin socket-shield preparation in immediate implant placement and provisionalization in the esthetic zone. Int. J. Esthet. Dent. 2018, 13, 172–183. [Google Scholar] [PubMed]
- Baumer, D.; Zuhr, O.; Rebele, S.; Schneider, D.; Schupbach, P.; Hürzeler, M. The Socket-Shield Technique: First Histological, Clinical and Volumetrical Observations after Separation of the Buccal Tooth Segment—A Pilot Study. Clin. Implant. Dent. Relat. Res. 2013, 17, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Baumer, D.; Zuhr, O.; Rebele, S.; Hürzeler, M. Socket shield technique for immediate implant placement—clinical, radiographic and volumetric data after 5 years. Clin. Oral Implants Res. 2017, 28, 1450–1458. [Google Scholar] [CrossRef] [PubMed]
- Bramanti, E.; Norcia, A.; Cicciù, M.; Matacena, G.; Cervino, G.; Troiano, G.; Zhurakivska, K.; Laino, L. Postextraction dental implant in the aesthetic zone, socket-shield technique versus conventional protocol. J. Craniofac. Surg. 2018, 29, 1037–1041. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.C.; Chen, C.L. A preliminary clinical study of buccal bone alteration using the socket-shield technique and immediate implant placement. J. Taiwan Acad. Periodontol. 2016, 21, 137–145. [Google Scholar]
- Cherel, F.; Etienne, D. Papilla preservation between two implants: A modified socket-shield technique to maintain the scalloped anatomy? A case report. Quintessence Int. 2014, 45, 23–30. [Google Scholar] [CrossRef]
- Chen, C.; Pan, Y. Socket shield technique for ridge preservation: A case report. J. Prosthodont. Implantol. 2013, 2, 16–21. [Google Scholar]
- Dayakar, M.M.; Waheed, A.; Bhat, H.S.; Gurpur, P.P. The socket-shield technique and immediate implant placement. J. Indian Soc. Periodontol. 2018, 22, 451–455. [Google Scholar] [CrossRef]
- Gluckman, H.; Salama, M.; Du Toit, J. A retrospective evaluation of 128 socket-shield cases in the esthetic zone and posterior sites: Partial extraction therapy with up to 4 years follow-up. Clin. Implant. Dent. Relat. Res. 2017, 20, 122–129. [Google Scholar] [CrossRef]
- Gluckman, H.; Du Toit, J. The management of recession midfacial to immediately placed implants in the aesthetic zone. Int. Dent. Afr. Ed. 2015, 5, 6–15. [Google Scholar]
- Guo, T.; Nie, R.; Xin, X.; Wang, H.; Qi, M.; Yu, K.; Wang, Y.; Du, L.; Zhou, Y. Tissue preservation through socket-shield technique and plateletrich fibrin in immediate implant placement: A case report. Medicine (Baltimore) 2018, 97, e1375:1–e1375:6. [Google Scholar] [CrossRef] [PubMed]
- Han, C.-H.; Park, K.-B.; Mangano, F.G. The Modified Socket Shield Technique. J. Craniofacial Surg. 2018, 29, 2247–2254. [Google Scholar] [CrossRef] [PubMed]
- Hinze, M.; Janousch, R.; Goldhahn, S.; Schlee, M. Volumetric alterations around single-tooth implants using the socket-shield technique: Preliminary results of a prospective case series. Int. J. Esthet. Dent. 2018, 13, 146–170. [Google Scholar] [PubMed]
- Petsch, M.; Spies, B.; Kohal, R.-J. Socket Shield Technique for Implant Placement in the Esthetic Zone: A Case Report. Int. J. Periodontics Restor. Dent. 2017, 37, 853–860. [Google Scholar] [CrossRef] [Green Version]
- Schwimer C, Pette GA, Gluckman H, Salama M, Du Toit Human Histologic Evidence of New Bone Formation and Osseoin-tegration Between Root Dentin (Unplanned Socket-Shield) and Dental Implant: Case Report. J. Int. Oral Maxillofac. Implants 2018, 33, e19–e23. [CrossRef]
- Siormpas, K.; Mitsias, M.; Kontsiotou-Siormpa, E.; Garber, D.; Kotsakis, G. Immediate Implant Placement in the Esthetic Zone Utilizing the “Root-Membrane” Technique: Clinical Results up to 5 Years Postloading. Int. J. Oral Maxillofac. Implant. 2014, 29, 1397–1405. [Google Scholar] [CrossRef] [Green Version]
- Staehler, P.; Abraha, S.M.; Bastos, J.; Zuhr, O.; Hürzeler, M. The socket-shield technique: A step-by-step protocol after 12 years of experience. Int. J. Esthet. Dent. 2020, 15, 288–305. [Google Scholar]
- Sun, C.; Zhao, J.; Liu, Z.; Tan, L.; Huang, Y.; Zhao, L.; Tao, H. Comparing conventional flap-less immediate implantation and socket-shield technique for esthetic and clinical outcomes: A randomized clinical study. Clin. Oral Implant. Res. 2019, 31, 181–191. [Google Scholar] [CrossRef] [PubMed]
- Troiano, M.; Benincasa, M.; Sánchez, P.; Calvo-Guirado, J. Bundle bone preservation with Root-T-Belt: Case study. Ann. Oral. Maxillofac. Surg. 2014, 2, 7:1–7:6. [Google Scholar]
- Verma, N.; Lata, J.; Kaur, J. Socket shield technique—A new approach to immediate implant placement. Indian J. Compr. Dent. Care 2018, 8, 1181–1183. [Google Scholar]
- Zhu, Y.B.; Qiu, L.X.; Chen, L.; Gao, M.; Yu, H.J.; Wang, J. Clinical evaluation of socket shield technique in maxillary anterior region. Chin. J. Stomatol. 2018, 53, 665–668. [Google Scholar]
- Zuhr, O.; Staehler, P.; Huerzeler, M. Complication Management of a Socket Shield Case After 6 Years of Function. Int. J. Periodontics Restor. Dent. 2020, 40, 409–415. [Google Scholar] [CrossRef]
- Zhang, Z.; Dong, Y.; Yang, J.; Xu, R.; Deng, F. Effect of socket-shield technique on alveolar ridge soft and hard tissue in dogs. J. Clin. Periodontol. 2019, 46, 256–263. [Google Scholar] [CrossRef]
- Viña-Almunia, J.; Candel-Martí, M.E.; Cervera-Ballester, J.; García-Mira, B.; Calvo-Guirado, J.L.; Peñarrocha-Oltra, D.; Peñarrocha-Diago, M. Buccal bone crest dynamics after immediate implant placement and ridge preservation techniques: Review of morphometric studies in animals. Implant. Dent. 2013, 22, 155–160. [Google Scholar] [CrossRef]
- Mitsias, M.M.; Bratos, M.; Siormpas, K.; Pikos, M.A.; Kotsakis, G.A. Root Membrane Group Longitudinal Soft Tissue Changes During Periodontal Ligament-Mediated Immediate Implant Placement with the Root-Membrane Technique. Int. J. Oral Maxillofac. Implants. 2020, 35, 379–385. [Google Scholar] [CrossRef]
- Botticelli, D.; Berglundh, T.; Buser, D.; Lindhe, J. The jumping distance revisited: An experimental study in the dog. Clin. Oral Implants Res. 2003, 14, 35–42. [Google Scholar] [CrossRef]
- Siormpas, K.D.; Mitsias, M.E.; Kotsakis, G.A.; Tawil, I.; Pikos, M.A.; Mangano, F.G. The root membrane technique: A retro-spective clinical study with up to 10 years of follow-up. Implant. Dent. 2018, 27, 564–574. [Google Scholar] [CrossRef]
- Kan, J.Y.K.; Rungcharassaeng, K. Proximal Socket Shield for Interimplant Papilla Preservation in the Esthetic Zone. Int. J. Periodontics Restor. Dent. 2013, 33, e24–e31. [Google Scholar] [CrossRef] [Green Version]
- Gher, M.E.; Quintero, G.; Assad, D.; Monaco, E.; Richardson, A.C. Bone Grafting and Guided Bone Regeneration for Immediate Dental Implants in Humans. J. Periodontol. 1994, 65, 881–891. [Google Scholar] [CrossRef]
- Chen, S.T.; Darby, I.B.; Reynolds, E.C. A prospective clinical study of non-submerged immediate implants: Clinical out- comes and esthetic results. Clin. Oral Implants Res. 2007, 18, 552–562. [Google Scholar] [CrossRef] [PubMed]
- Esposito, M.; Grusovin, M.G.; Polyzos, I.P.; Felice, P.; Worthington, H.V. Interventions for replacing missing teeth: Dental implants in fresh extraction sockets (immediate, immediate- delayed and delayed implants). Cochrane Database Syst. Rev. 2010, 9, CD005968. [Google Scholar] [CrossRef] [PubMed]
- Mourya, A.; Mishra, S.K.; Gaddale, R.; Chowdhary, R. Socket-shield technique for implant placement to stabilize the facial gingival and osseous architecture: A systematic review. J. Investig. Clin. Dent. 2019, 10, e12449. [Google Scholar] [CrossRef] [PubMed]

| No. | Authors and Publication Year | Type of Study | Sample Size (Number of Patients/Dental Implant) | Dental Implant placement Site/Loading Protocol | Duration n of Follow-Up (Months) | Grafting Materials | Clinical Therapy Regimen Outcomes |
|---|---|---|---|---|---|---|---|
| 1 | Abadzhiev et al., 2014 [22] | Prospective case- control study | 25 patients/ 26 dental implants (10 SST; 16 conventional technique) | Alveolar ridge anterior region (SST)/not specified | 24 | Xeno- bone graft material | Mean crestal bone loss of 0.8 mm (SST *); 5 mm (control group) |
| 2 | Abd-Elrahman et al., 2020 [23] | Randomized clinical trial | 25 patients/ 40 dental implants (20 SST; 20 control) | Alveolar ridge anterior region/ immediate | 6 | Graft not mentioned | One internal root fragment exposure, which did not require treatment, mean horizontal bone loss (0.15 mm SST; 0.32 mm control group), mean vertical bone loss (0.31 mm SST; 0.7 mm control group) |
| 3 | Abitbol et al., 2016 [24] | Case series, retrospective study | 20 patients/23 dental implants | Not mentioned/immediate | 12 | Xenograft/allograft | Probing pocket of 8 mm in the mesio- buccal part of one root fragment; one root fragment exposure |
| 4 | Aslan 2018 [25] | Case report, prospective study | One patient/one dental implant | Alveolar ridge anterior region/immediate | 12 | Demineralized bovine bone | Thin buccal bone plate loss of 0.39 mm, natural convex buccal contour equal to adjacent central incisor |
| 5 | Baumer et al., 2013 [26] | Case report, pilot study | One patient/one dental implant | Alveolar ridge anterior region/delayed | 6 | No graft | Mean labial bone loss of 0.88 mm (range 1.67–0.15 mm) |
| 6 | Baumer et al., 2017 [27] | Case series, | 10 patients/ | Alveolar ridge | 51–63 | No graft | Marginal bone loss of 0.33 ± 0.43 mm |
| retrospective pilot study | 10 dental implants | Posterior region/four immediate six delayed | at mesial aspect and 0.17 ± 0.36 mm at distal aspect | ||||
| 7 | Bramanti et al., 2018 [28] | Randomized controlled trial, prospective study | 40 patients/40 dental implants (20 SST; 20 Conventional technique) | Alveolar ridge anterior region/immediate | 36 | Allograft (control group) | Marginal bone loss 0.605 ± 0.06 mm (SST); 1.115 ± 0.131 mm (control group) |
| 8 | Chen and Chen 2016 [29] | Case series, preliminary clinical study | four patients/four dental implants | Alveolar ridge anterior and posterior regions/not specified | 3 | Graft not mentioned | Mean buccal bone loss 0.83 ± 0.178 mm |
| 9 | Cherel and Etienne 2014 [30] | Case report, prospective study | One patient/two dental implants | Alveolar ridge anterior region/immediate | 11 | Deproteinized bovine bone mineral | Coronal part of root fragments visible through mucosal bed after removal of temporary crowns |
| 10 | Chen and Pan 2013 [31] | Case report, prospective study | One patient/one dental implant | Alveolar ridge posterior region/delayed | 12 | No graft | Mean buccal bone loss 0.72 mm |
| 11 | Dayakar et al., 2018 [32] | Case report, prospective study | One patient/one dental implant | Alveolar ridge anterior region/delayed | 3 | Bone graft | Healthy peri-implant tissue found |
| 12 | Gluckmanet al., 2017 [33] | Clinical therapy protocol | One patient/one dental implant | Alveolar ridge anterior region/immediate | 12 | Graft not mentioned | The SST can achieve very positive outcomes, even in the most challenging of clinical scenarios |
| 13 | Gluckman et al., 2015 [34] | Case series, retrospective study | 128 patients/128 dental implants | Alveolar ridge anterior and posterior region/immediate | 48 | Graft not mentioned | Five dental implants failed to osseointegrate, root fragment internal exposures in 12 cases, exceeded external exposures in four cases, three root fragments developed infections, one root fragment migrated |
| 14 | Guo et al., 2018 [35] | Case report, prospective study | One patient/one dental implant | Alveolar ridge anterior region/delayed | 18 | No graft | Marginal bone level was stable in both vertical (13.2 mm) and horizontal (7.0 mm) directions around implant, gingiva showed no contour recession |
| 15 | Han et al., 2018 [36] | Case series, prospective clinical study | 30 patients/40 dental implants | Alveolar ridge anterior and posterior region/immediate | 12 | No graft | Peri-implant tissues showed healthy condtion |
| 16 | Hinze et al., 2018 [37] | Case series, prospective cohort study | 15 patients/17 dental implants | Alveolar ridge anterior and posterior region/immediate | 3 | No graft | Change in soft tissue volume in buccal contour with range-0.37 to 0.32 mm (mean-0.07 ± 0.16), gingival margin with range- 0.84 to 1.58 mm (mean 0.17 ± 0.67), Eight dental implants showed marginal gingival tissue recession |
| 17 | Petsch et al., 2017 [38] | Case report, prospective study | One patient/one dental implant | Alveolar ridge anterior region/ delayed | 24 | Xenograft | No clinical change in soft tissue or plaque accumulation, inter- proximal and palatal pocket probing depths where no retaining root fragment was slight increased (0.5–1 mm) |
| 18 | Schwimer et al., 2018 [39] | Technique report | One patient/2 dental implants (1 SST; 1 conventional technique) | Alveolar ridge posterior region/delayed | 3–4 | Xenograft | SST may help to maintain the alveolar ridge at immediate molar implant placement sites |
| 19 | Siormpas et al., 2014 [40] | Case series, retrospective study | 182 patients/250 dental implants | Alveolar ridge anterior region/immediate | No graft | Five dental implants failed (two failed toosseointegrate, three had peri-implantitis), three complications due to infection of root fragment, which were treated | |
| 20 | Staehler et al., 2020 [41] | Clinical therapy protocol | One patient/one dental implant | Alveolar ridge anterior region | 144 | No graft | The SST can provide highly asthetic and predictable outcomes |
| 21 | Sun et al., 2020 [42] | Randomized clinical study | 30 patients/30 dental implants (15 SST;15 conventional flap-less approach) | Alveolar ridge anterior region | 24 | Deproteinized bovine bone material | Less reduction in the midfacial mucosal margins and the height of the mesial and distal papillae, as well as higher buccal plate width and height values (SST) |
| 22 | Troiano et al., 2014 [43] | Case series, prospective case study | Seven patients/10 dental implants | Alveolar ridge anterior region/delayed | 6 | No graft | Mean crestal bone loss 1.3 ± 0.2 mm, mesial 0.8 mm, distal 0.7 mm |
| 23 | Verma et al., 2018 [44] | Case report, prospective study | One patient/one dental implant | Alveolar ridge anterior region/immediate | 12 | No graft | Healthy peri-implant soft tissue and ridge were preserved |
| 24 | Zhu et al., 2018 [45] | Case series, prospective clinical study | Nine patients/10 dental implants | Alveolar ridge anterior region/immediate | 12–48 | No graft | Mesial bone loss 0.17 mm; distal bone loss 0.22 mm |
| 25 | Zuhr et al., 2020 [46] | Clinical case report | One patient/one dental implant | Alveolar ridge anterior region/immediate | 72 | No grafts | Shield around the buccal aspect of the dental implant was mobile; 8 mm buccal probing depth detected, which was surgically managed |
| Number | Bone Modifications around Dental Implants | No. of Reported Cases and Percentage |
|---|---|---|
| 1 | Crestal bone loss of 1.3 ± 0.2 mm, mesial bone loss of 0.8 mm, distal bone loss of 0.7 mm (Troiano et al., 2014) [43] | 10 |
| 2 | Buccal bone loss of 0.88 mm (Baumer et al., 2013) [22] | 1 |
| 3 | Buccal bone loss of 0.83 ± 0.178 mm (Chen and Chen 2016) [29] | 4 |
| 4 | Crestal bone loss of 0.8 mm (Abadzhiev et al., 2014) | 10 |
| 5 | Buccal bone loss of 0.72 mm (Chen and Pan 2013) | 1 |
| 6 | Mesial bone loss of 0.17 mm, distal bone loss of 0.22 mm (Zhu et al., 2018) [45] | 10 |
| 7 | Marginal bone loss of 0.605 ± 0.06 mm (Bramanti et al., 2018) [28] | 20 |
| 8 | Mesial bone loss of 0.33 ± 0.43 mm, distal bone loss of 0.17 ± 0.36 mm (Baumer et al., 2017) [27] | 10 |
| 9 | Horizontal bone loss of 0.15 mm, vertical bone loss of 0.31 mm (Abd-Elrahman et al., 2020) [23] | 20 |
| 10 | Changes ranged from 0.19 mm in the midfacial region 6 mm apical to the mucosal zenith to −0.06 mm at 5 mm apical to the base of the distal papilla Mitsias et al., 2020 [4] |
| Number of Clinical Studies | Total Number of Patients/Immediate Dental Implant Placement/Immediate Dental Implant Placement in Conjunction with the Socket-Shield Technique | Total of Dental Implant Failures Complications and Undesired Adverse Effects |
|---|---|---|
| 25 | 537 patients/642 dental implants/570 dental iimplants in conjunction with the socket-shield technique | 10 dental implants failed (1.75%)/123 complications and undesired adverse effects (21.58%) |
| Consecutive Number of the Study | Type of Complication/Author | Percentage and Number of Cases |
|---|---|---|
| Root fragment exposure | Total 20 (15.04%) | |
| 1 | Coronal part of root fragment exposed through mucosal bed (Cherel and Etienne 2014) [30] | 2 |
| 2 | Root fragment exposure (Abitbol et al., 2016) [24] | 1 |
| 3 | Root fragment internal (12 cases) and external (four cases) exposures (Gluckman et al., 2017) [33] | 16 |
| 4 | Root fragment internal (12 cases) and external (four cases) exposures (Gluckman et al., 2017) [33] | 1 |
| Dental implant failures | Total 10 (7.5%) | |
| 5 | Failure to osseointegrate (Siormpas et al., 2018) [40] | 2 |
| 6 | Due to peri-implantitis (Siormpas et al., 2018) [40] | 3 |
| 7 | Failure to osseointegrate (Gluckman et al., 2017) [33] | 5 |
| Root fragment with deep probing pocket depth | Total 2 (1.5%) | |
| 8 | Mesio-buccal part of 8 mm (Abitbol et al., 2016) [24] | 1 |
| 9 | Buccal probing depth of 8 mm (Zuhr et al., 2020) [46] | 1 |
| Root fragment infections | Total 6 (4.5%) | |
| 10 | Root fragment infections (Siormpas. et al., 2018) [40] | 3 |
| 11 | Root fragment infections (Gluckman et al., 2017) [33] | 3 |
| Changes in soft tissue contour | Total 8 (6%) | |
| 12 | Marginal gingival tissue recession (Hinze et al., 2018) [37] | 8 |
| Root fragment migration | Total 1 (0.75%) | |
| 13 | Migration of the fragment (Gluckman et al., 2017) [33] | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Angelis, N.; Signore, A.; Alsayed, A.; Hai Hock, W.; Solimei, L.; Barberis, F.; Amaroli, A. Immediate Implants in the Aesthetic Zone: Is Socket Shield Technique a Predictable Treatment Option? A Narrative Review. J. Clin. Med. 2021, 10, 4963. https://doi.org/10.3390/jcm10214963
De Angelis N, Signore A, Alsayed A, Hai Hock W, Solimei L, Barberis F, Amaroli A. Immediate Implants in the Aesthetic Zone: Is Socket Shield Technique a Predictable Treatment Option? A Narrative Review. Journal of Clinical Medicine. 2021; 10(21):4963. https://doi.org/10.3390/jcm10214963
Chicago/Turabian StyleDe Angelis, Nicola, Antonio Signore, Arwa Alsayed, Wong Hai Hock, Luca Solimei, Fabrizio Barberis, and Andrea Amaroli. 2021. "Immediate Implants in the Aesthetic Zone: Is Socket Shield Technique a Predictable Treatment Option? A Narrative Review" Journal of Clinical Medicine 10, no. 21: 4963. https://doi.org/10.3390/jcm10214963
APA StyleDe Angelis, N., Signore, A., Alsayed, A., Hai Hock, W., Solimei, L., Barberis, F., & Amaroli, A. (2021). Immediate Implants in the Aesthetic Zone: Is Socket Shield Technique a Predictable Treatment Option? A Narrative Review. Journal of Clinical Medicine, 10(21), 4963. https://doi.org/10.3390/jcm10214963










