Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention
Abstract
:1. Introduction
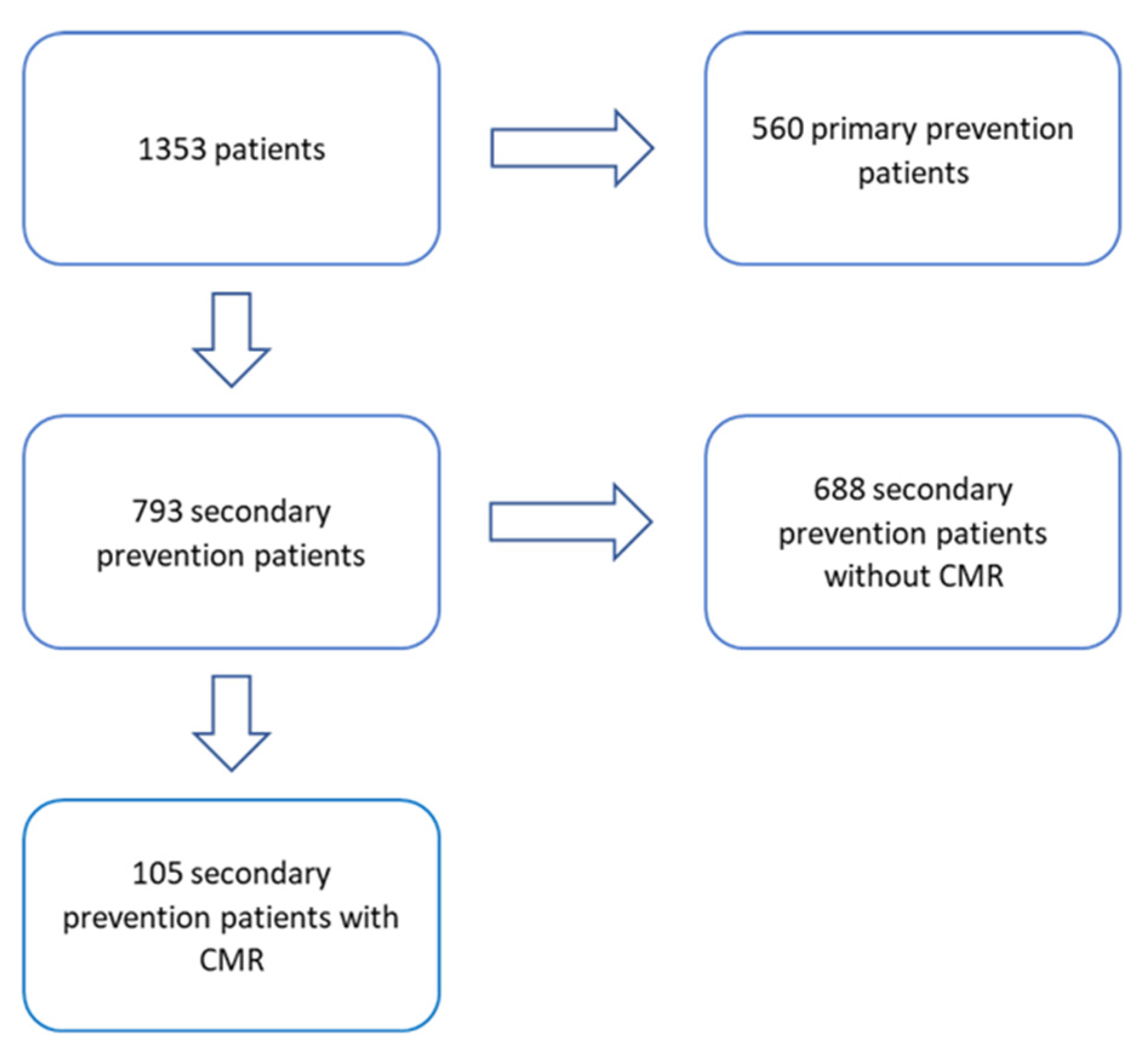
2. Materials and Methods
2.1. Study Design
2.2. Study Endpoints and Follow-Up
2.3. Cardiac Magnetic Resonance
2.4. Defining Etiology
2.5. Device Readout
2.6. Defining the Device Therapies
2.7. ICD Programming
2.8. Statistical Analysis
3. Results
3.1. Study Population
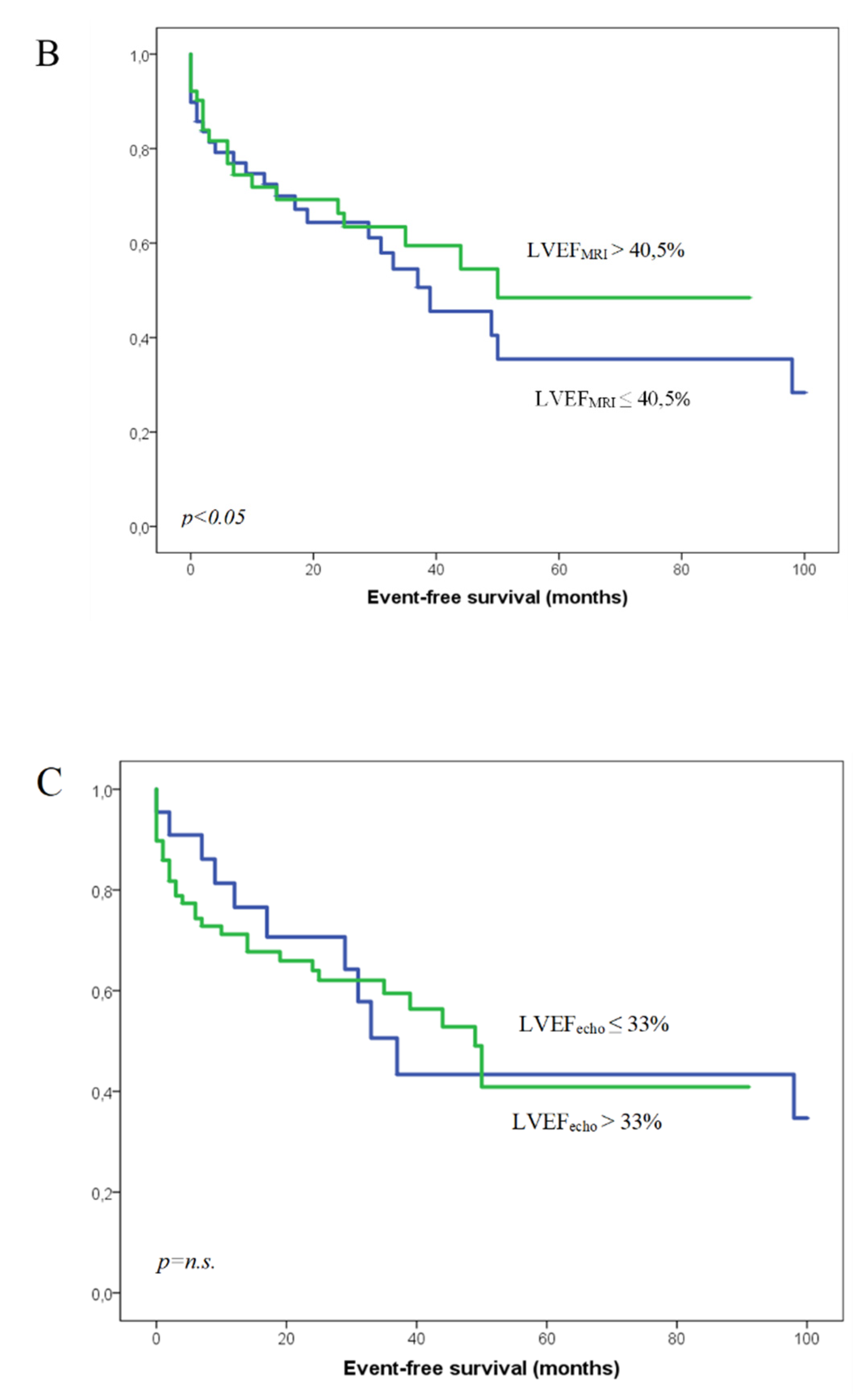
3.2. Calculation of the Best Predictive Value for LVGFI, LVEFMRI, and LVEFecho
3.3. Classifying the Groups According to the LVGFI
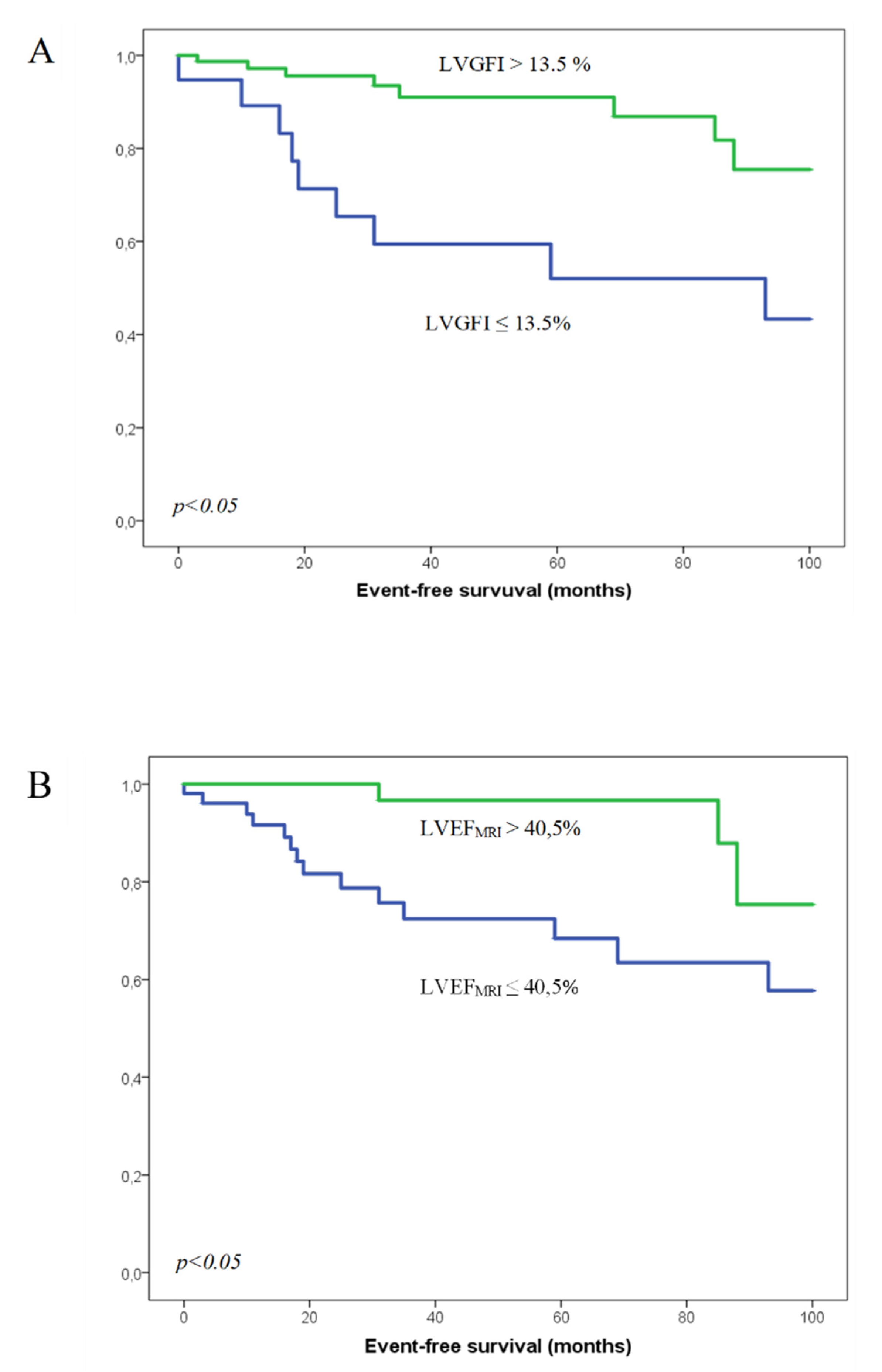
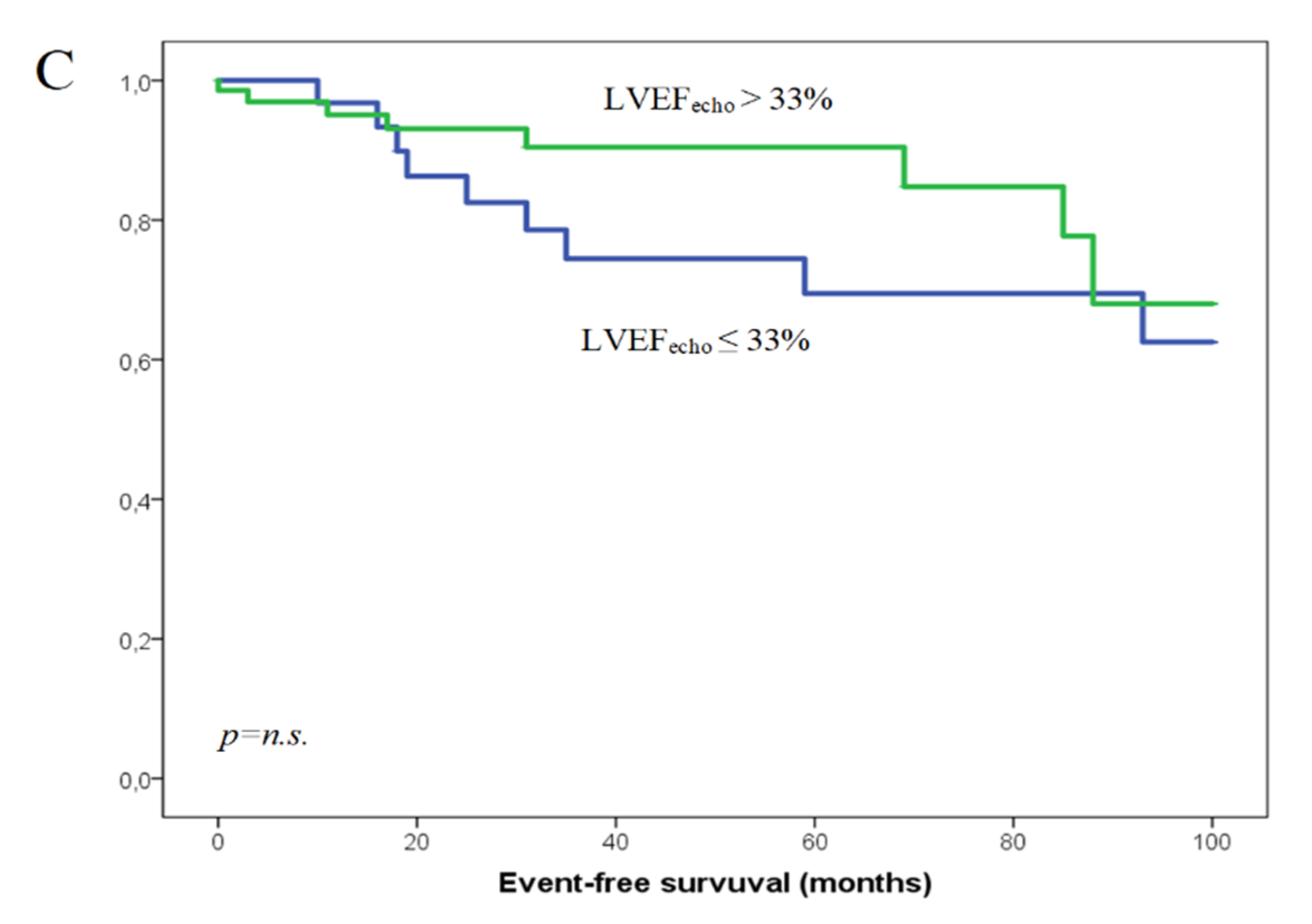
3.4. Combined Endpoint: All-Cause Mortality and Hospitalization Due to Heart Failure
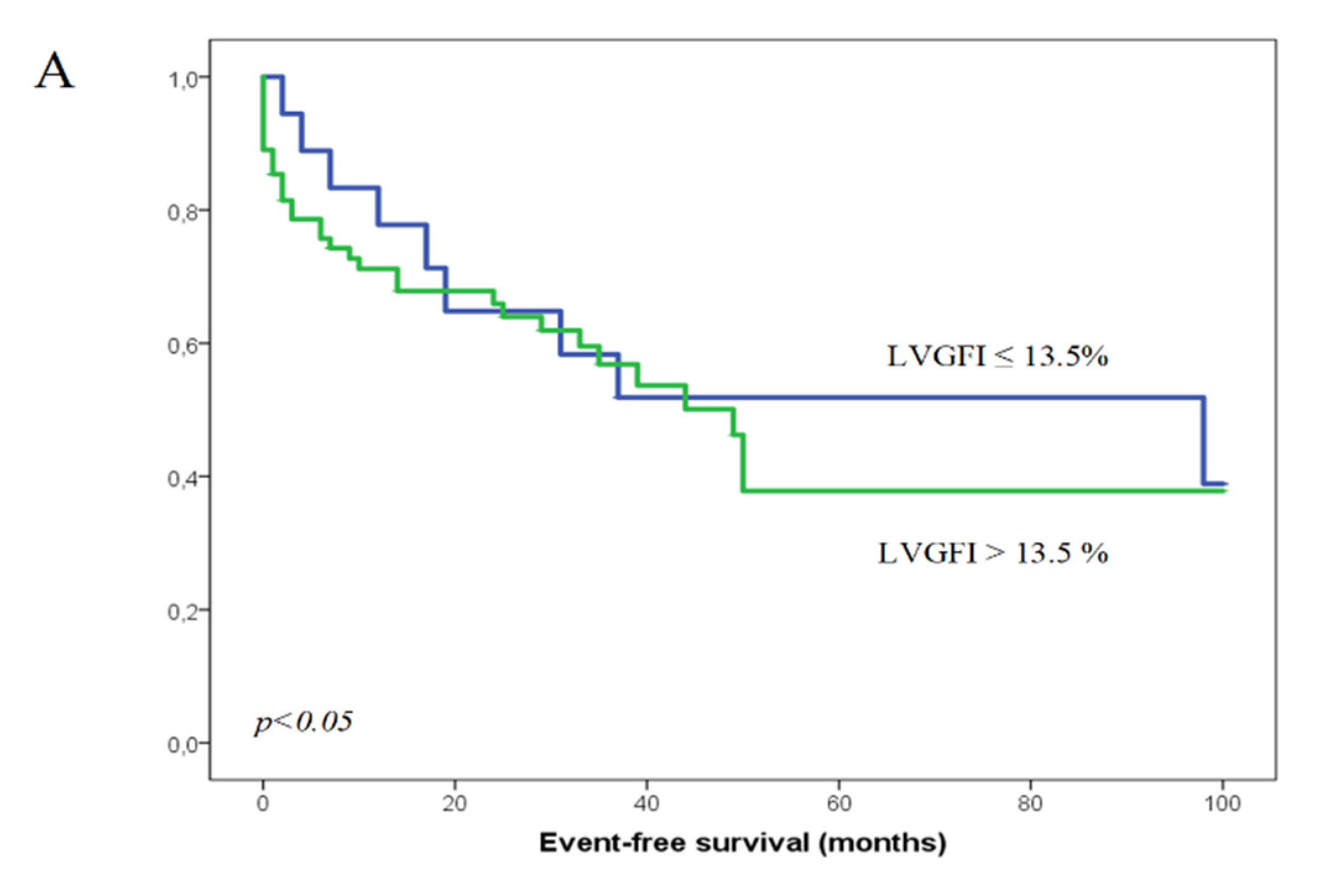
3.5. Appropriate ICD Therapies
3.6. Inappropriate ICD Therapies
3.7. Performance of LVGFI in Predicting the Outcome
3.8. Independent Predictors for Worse Outcome
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Curtis, J.P.; Sokol, S.I.; Wang, Y.; Rathore, S.S.; Ko, D.T.; Jadbabaie, F.; Portnay, E.L.; Marshalko, S.J.; Radford, M.J.; Krumholz, H.M. The association of left ventricular ejection fraction, mortality, and cause of death in stable outpatients with heart failure. J. Am. Coll. Cardiol. 2003, 42, 736–742. [Google Scholar] [CrossRef] [Green Version]
- Moss, A.J.; Zareba, W.; Hall, W.J.; Klein, H.; Wilber, D.J.; Cannom, D.S.; Daubert, J.P.; Higgins, S.L.; Brown, M.W.; Andrews, M.L. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N. Engl. J. Med. 2002, 346, 877–883. [Google Scholar] [CrossRef] [Green Version]
- Steinberg, J.S.; Martins, J.; Sadanandan, S.; Goldner, B.; Menchavez, E.; Domanski, M.; Russo, A.; Tullo, N.; Hallstrom, A. Antiarrhythmic drug use in the implantable defibrillator arm of the Antiarrhythmics Versus Implantable Defibrillators (AVID) Study. Am. Heart J. 2001, 142, 520–529. [Google Scholar] [CrossRef]
- Connolly, S.J.; Gent, M.; Roberts, R.S.; Dorian, P.; Roy, D.; Sheldon, R.S.; Mitchell, L.B.; Green, M.S.; Klein, G.J.; O’Brien, B. Canadian implantable defibrillator study (CIDS): A randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation 2000, 101, 1297–1302. [Google Scholar] [CrossRef] [Green Version]
- Kuck, K.H.; Cappato, R.; Siebels, J.; Rüppel, R. Randomized comparison of antiarrhythmic drug therapy with implantable defibrillators in patients resuscitated from cardiac arrest: The Cardiac Arrest Study Hamburg (CASH). Circulation 2000, 102, 748–754. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reinstadler, S.J.; Klug, G.; Feistritzer, H.-J.; Kofler, M.; Pernter, B.; Göbel, G.; Henninger, B.; Müller, S.; Franz, W.-M.; Metzler, B. Prognostic value of left ventricular global function index in patients after ST-segment elevation myocardial infarction. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 169–176. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mewton, N.; Opdahl, A.; Choi, E.-Y.; Almeida, A.L.C.; Kawel, N.; Wu, C.O.; Burke, G.L.; Liu, S.; Liu, K.; Bluemke, D.A.; et al. Left ventricular global function index by magnetic resonance imaging—A novel marker for assessment of cardiac performance for the prediction of cardiovascular events: The multi-ethnic study of atherosclerosis. Hypertension 2013, 61, 770–778. [Google Scholar] [CrossRef] [Green Version]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.-P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Pezel, T.; Des Besseyre Horts, T.; Schaaf, M.; Croisille, P.; Bière, L.; Garcia-Dorado, D.; Jossan, C.; Roubille, F.; Cung, T.-T.; Prunier, F.; et al. Predictive value of early cardiac magnetic resonance imaging functional and geometric indexes for adverse left ventricular remodelling in patients with anterior ST-segment elevation myocardial infarction: A report from the CIRCUS study. Arch. Cardiovasc. Dis. 2020, 113, 710–720. [Google Scholar] [CrossRef] [PubMed]
- Eitel, I.; Pöss, J.; Jobs, A.; Eitel, C.; de Waha, S.; Barkhausen, J.; Desch, S.; Thiele, H. Left ventricular global function index assessed by cardiovascular magnetic resonance for the prediction of cardiovascular events in ST-elevation myocardial infarction. J. Cardiovasc. Magn. Reson. 2015, 17, 62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, S.; Xu, H.-Y.; Diao, K.-Y.; Shi, K.; He, Y.; He, S.; Zhang, Y.; Gao, Y.; Shen, M.-T.; Guo, Y.-K.; et al. Left ventricular global function index by magnetic resonance imaging—A novel marker for differentiating cardiac amyloidosis from hypertrophic cardiomyopathy. Sci. Rep. 2020, 10, 4707. [Google Scholar] [CrossRef] [PubMed]
- Aquaro, G.D.; Camastra, G.; Monti, L.; Lombardi, M.; Pepe, A.; Castelletti, S.; Maestrini, V.; Todiere, G.; Masci, P.; Di Giovine, G.; et al. Reference values of cardiac volumes, dimensions, and new functional parameters by MR: A multicenter, multivendor study. J. Magn. Reson. Imaging 2017, 45, 1055–1067. [Google Scholar] [CrossRef] [PubMed]
- Nwabuo, C.C.; Moreira, H.T.; Vasconcellos, H.D.; Mewton, N.; Opdahl, A.; Ogunyankin, K.O.; Ambale-Venkatesh, B.; Schreiner, P.J.; Armstrong, A.A.C.; Lewis, C.E.; et al. Left ventricular global function index predicts incident heart failure and cardiovascular disease in young adults: The coronary artery risk development in young adults (CARDIA) study. Eur. Heart J. Cardiovasc. Imaging 2018, 20, 533–540. [Google Scholar] [CrossRef] [PubMed]
| Total Study Cohort (105) | |
|---|---|
| Age | 56 (43; 65) |
| Male sex | 80 (76.2%) |
| Device | |
| 1C | 62 (59.0%) |
| 2C | 25 (23.8%) |
| CRT-D | 7 (6.7%) |
| S-ICD | 11 (10.5%) |
| LVEF ≤ 35% | 25 (23.8%) |
| LVEF (Echo) | 45.0 (35.0; 57.0) |
| LVEF (MRI) | 41.0 (27.6; 56.5) |
| LVGFI | 24.5 (15.1; 33.7) |
| LGE | 68 (64.8%) |
| NYHA ≥ II | 64 (61%) |
| MI | 27 (25.7%) |
| CAD | 43 (41.0%) |
| Cardiomyopathy | |
| DCM | 20 (19.0%) |
| Other cardiomyopathy * | 19 (18.1%) |
| Primary VF | 10 (9.5%) |
| Long-QT-Syndrome | 7 (6.7%) |
| Short-QT-Syndrome | 1 (0.9%) |
| Idiopathic VT | 5 (4.8%) |
| peripheral arterial occlusive disease (PAOD) | 6 (5.7%) |
| Valve surgery | 3 (3.1%) |
| AF | 20 (19.0%) |
| Hypertension | 51 (48.6%) |
| Diabetes | 17 (16.2%) |
| Renal insufficiency | 12 (11.4%) |
| TIA/stroke | 5 (4.8%) |
| Smoking | 48 (45.7%) |
| COPD | 5 (4.8%) |
| ACE-inhibitors/ATI/Entresto | 74 (70.5%) |
| Beta-Blocker | 77 (73.3%) |
| Ca-Antagonists | 10 (9.5%) |
| Diuretics | 42 (40.0%) |
| Spironolactone | 45 (42.9%) |
| ASS | 39 (37.1%) |
| Macumar/NOAKs | 22 (21.0%) |
| P2Y12 | 13 (12.4%) |
| Amiodaron/Sotalol | 5 (4.8%) |
| Digitalis | 5 (4.8%) |
| Statin | 41 (39.0%) |
| Ivabradin | 1 (1.0%) |
| Monomorph VT | 46 (43.8%) |
| Polymorph VT | 5 (4.8%) |
| Ventricular Flutter | 1 (1.0%) |
| Ventricular Fibrillation | 48 (45.6%) |
| Asystole | 5 (4.8%) |
| LVGFI ≤ 13.5% (19) | LVGFI > 13.5% (86) | p | |
|---|---|---|---|
| Age | 58 (47; 68) | 55 (40.8; 64.0) | 0.316 |
| Male sex | 15 (78.9%) | 65 (75.6%) | 0.756 |
| Device | 0.996 | ||
| 1C | 11 (57.8%) | 51 (59.3%) | |
| 2C | 4 (21.1%) | 21 (24.4%) | |
| CRT-D | 4 (21.1%) | 3 (3.5%) | |
| S-ICD | 0 (0%) | 11 (12.8%) | |
| LVEF≤35% | 13 (68.4%) | 12 (14.0%) | <0.001 |
| LVEF (Echo) | 23.0 (19.0; 41.0) | 48.0 (39.8; 58.3) | <0.001 |
| LVEF (MRI) | 16.0 (14.0; 21.0) | 46.0 (36.6; 60.3) | <0.001 |
| LVGFI | 10.2 (8.1; 12.4) | 28.3 (21.0; 36.5) | <0.001 |
| LGE | 13 (68.4%) | 55 (80.1%) | 0.685 |
| NYHA≥II | 16 (84.2%) | 48 (55.8%) | 0.022 |
| MI | 8 (42.1%) | 19 (22.1%) | 0.099 |
| CAD | 11 (57.9%) | 32 (37.2%) | 0.072 |
| Cardiomyopathy | 0.025 | ||
| DCM | 7 (36.8%) | 13 (15.1%) | |
| Other cardiomyopathy * | 1 (5.2%) | 18 (20.9%) | |
| Primary VF | 0 (0%) | 10 (11.6%) | 0.120 |
| Long-QT-Syndrome | 0 (0%) | 7 (8.1%) | 0.200 |
| Short-QT-Syndrome | 0 (0%) | 1 (1.3%) | 0.638 |
| Idiopathic VT | 0 (0%) | 5 (5.8%) | 0.284 |
| PAOD | 1 (5.3%) | 5 (5.8%) | 0.926 |
| Valve surgery | 0 (0%) | 3 (3.5%) | 0.411 |
| AF | 3 (15.8%) | 17 (19.8%) | 0.691 |
| Hypertension | 13 (68.4%) | 38 (44.2%) | 0.057 |
| Diabetes | 6 (31.6%) | 11 (12.8%) | 0.045 |
| Renal insufficiency | 4 (21.1%) | 8 (9.3%) | 0.147 |
| TIA/stroke | 0 (0%) | 5 (5.8%) | 0.284 |
| Smoking | 9 (47.4%) | 39 (45.3%) | 0.934 |
| COPD | 0 (0%) | 5 (5.8%) | 0.284 |
| ACE-inhibitors/ATI/Entresto | 14 (73.7%) | 60 (69.8%) | 0.736 |
| Beta-Blocker | 16 (84.2%) | 61 (70.9%) | 0.238 |
| Ca-Antagonists | 2 (10.5%) | 8 (9.3%) | 0.870 |
| Diuretics | 16 (84.2%) | 26 (30.2%) | <0.001 |
| Spironolactone | 14 (73.7%) | 31 (36.0%) | 0.003 |
| ASS | 9 (47.4%) | 30 (34.9%) | 0.310 |
| Macumar/NOAKs | 6 (31.6%) | 16 (18.6%) | 0.211 |
| P2Y12 | 4 (21.1%) | 9 (10.5%) | 0.207 |
| Amiodaron/Sotalol | 3 (15.8%) | 2 (2.3%) | 0.013 |
| Digitalis | 2 (10.5%) | 3 (3.5%) | 0.194 |
| Statin | 7 (36.8%) | 34 (39.5%) | 0.800 |
| Ivabradin | 0 (0%) | 1 (1.2%) | 0.630 |
| Monomorph VT | 11 (57.9%) | 35 (40.7%) | 0.174 |
| Polymorph VT | 0 (0%) | 5 (5.8%) | 0.284 |
| Ventricular Flutter | 0 (0%) | 1 (1.2%) | 0.638 |
| Ventricular Fibrillation | 6 (31.6%) | 42 (48.8%) | 0.174 |
| Asystole | 2 (10.5%) | 3 (3.5%) | 0.194 |
| Hazard-Ratio | p | |
|---|---|---|
| LVGFI | 0.938 (0.887–0.991) | 0.023 |
| Older age at implantation | 1.060 (1.014–1.107) | 0.010 |
| LVEF (MRI) | 1.021 (0.926–1.124) | 0.673 |
| LVEF (Echo) | 0.984 (0.930–1.041) | 0.876 |
| NYHA ≥ II | 0.488 (0.129–1.841) | 0.483 |
| presence of diabetes | 0.714 (0.194–2.622) | 0.384 |
| diuretic usage | 1.476 (0.426–5.119) | 0.331 |
| Spironolactone usage | 0.513 (0.183–1.438) | 0.271 |
| Amiodaron or Sotalol usage | 4.081 (0.518–32.149) | 0.150 |
| Female sex | 0.414 (0.150–1.139) | 0.087 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schober, A.L.; Jungbauer, C.; Poschenrieder, F.; Schober, A.D.; Hubauer, U.; Keyser, A.; Fredersdorf-Hahn, S.; Debl, K.; Maier, L.S.; Sossalla, S.; et al. Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention. J. Clin. Med. 2021, 10, 4980. https://doi.org/10.3390/jcm10214980
Schober AL, Jungbauer C, Poschenrieder F, Schober AD, Hubauer U, Keyser A, Fredersdorf-Hahn S, Debl K, Maier LS, Sossalla S, et al. Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention. Journal of Clinical Medicine. 2021; 10(21):4980. https://doi.org/10.3390/jcm10214980
Chicago/Turabian StyleSchober, Andreas Leonhard, Carsten Jungbauer, Florian Poschenrieder, Alexander Daniel Schober, Ute Hubauer, Andreas Keyser, Sabine Fredersdorf-Hahn, Kurt Debl, Lars S. Maier, Samuel Sossalla, and et al. 2021. "Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention" Journal of Clinical Medicine 10, no. 21: 4980. https://doi.org/10.3390/jcm10214980
APA StyleSchober, A. L., Jungbauer, C., Poschenrieder, F., Schober, A. D., Hubauer, U., Keyser, A., Fredersdorf-Hahn, S., Debl, K., Maier, L. S., Sossalla, S., Buchner, S., & Üçer, E. (2021). Cardiac MRI Based Left Ventricular Global Function Index: Association with Disease Severity in Patients with ICD for Secondary Prevention. Journal of Clinical Medicine, 10(21), 4980. https://doi.org/10.3390/jcm10214980






