Myofascial Induction Therapy Improves the Sequelae of Medical Treatment in Head and Neck Cancer Survivors: A Single-Blind, Placebo-Controlled, Randomized Cross-Over Study
Abstract
:1. Introduction
2. Materials and Methods
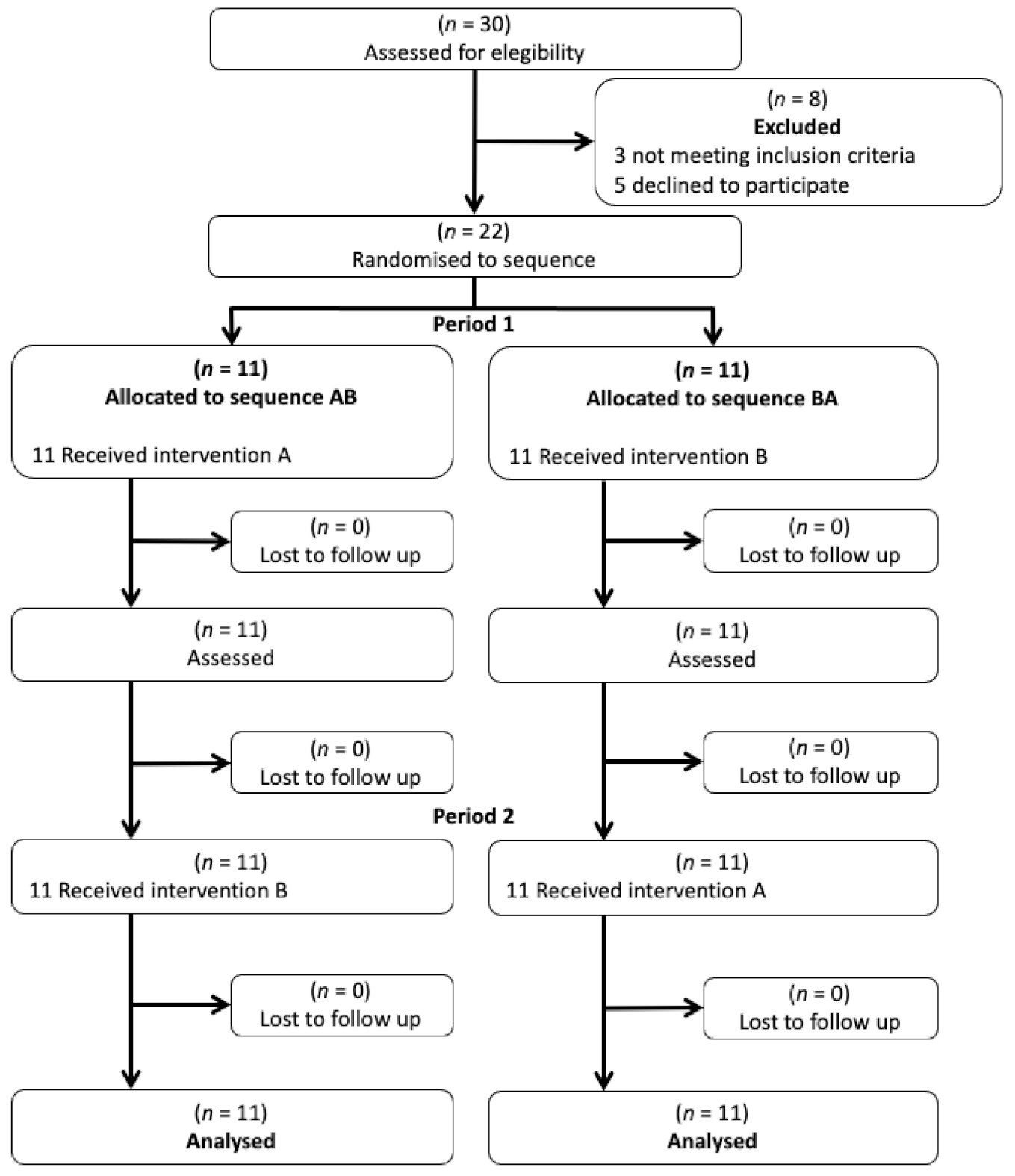
2.1. Study Design
2.2. Participants
2.3. Sample Size
2.4. Randomization to Treatment/Control Group, and Treatment Cross-Over
2.5. Outcome Measures
2.5.1. Pain
2.5.2. Range of Motion
2.5.3. Maximum Mouth Opening
2.5.4. Cervical Muscle Function
2.6. Statistical Analysis
2.7. Ethics Statement
3. Results
3.1. Effects of MIT on Cervical and Shoulder Pain
3.2. Effects of MIT on Cervical and Shoulder Range of Movement
3.3. Effects of MIT on Maximum Mouth Opening and Cervical Muscle Function
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cohen, N.; Fedewa, S.; Chen, A.Y. Epidemiology and Demographics of the Head and Neck Cancer Population. Oral Maxillofac. Surg. Clin. N. Am. 2018, 30, 381–395. [Google Scholar] [CrossRef] [PubMed]
- Aupérin, A. Epidemiology of Head and Neck Cancers: An Update. Curr. Opin. Oncol. 2020, 32, 178–186. [Google Scholar] [CrossRef] [PubMed]
- Shah, J.; Patel, S.; Singh, B.; Wong, R. Head and Neck Surgery and Oncology, 5th ed.; Elsevier: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Gane, E.M.; Michaleff, Z.A.; Cottrell, M.A.; McPhail, S.M.; Hatton, A.L.; Panizza, B.J.; O’Leary, S.P. Prevalence, Incidence, and Risk Factors for Shoulder and Neck Dysfunction after Neck Dissection: A Systematic Review. Eur. J. Surg. Oncol. 2017, 43, 1199–1218. [Google Scholar] [CrossRef] [Green Version]
- Maghami, E.; Ho, A. Multidisciplinary Care of the Head and Neck Cancer Patient; Springer International Publishing: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Baggi, F.; Santoro, L.; Grosso, E.; Zanetti, C.; Bonacossa, E.; Sandrin, F.; Massaro, M.A.; Tradati, N.; Simoncini, M.C. Recupero Motorio e Funzionale Dopo Dissezione Latero-Cervicale Del Collo: Due Programmi Di Fisioterapia Precoce a Confronto. Acta Otorhinolaryngol. Ital. 2014, 34, 230–240. [Google Scholar]
- Huang, J.; Zhang, J.; Shi, C.; Liu, L.; Wei, Y. Survival, Recurrence and Toxicity of HNSCC in Comparison of a Radiotherapy Combination with Cisplatin versus Cetuximab: A Meta-Analysis. BMC Cancer 2016, 16, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Bossi, P.; Giusti, R.; Tarsitano, A.; Airoldi, M.; De Sanctis, V.; Caspiani, O.; Alterio, D.; Tartaro, T.; Alfieri, S.; Siano, M. The Point of Pain in Head and Neck Cancer. Crit. Rev. Oncol./Hematol. 2019, 138, 51–59. [Google Scholar] [CrossRef] [Green Version]
- Cramer, J.D.; Johnson, J.T.; Nilsen, M.L. Pain in Head and Neck Cancer Survivors: Prevalence, Predictors, and Quality-of-Life Impact. Otolaryngol.-Head Neck Surg. 2018, 159, 853–858. [Google Scholar] [CrossRef]
- Ortiz-Comino, L.; Fernández-Lao, C.; Castro-Martín, E.; Lozano-Lozano, M.; Cantarero-Villanueva, I.; Arroyo-Morales, M.; Martín-Martín, L. Myofascial Pain, Widespread Pressure Hypersensitivity, and Hyperalgesia in the Face, Neck, and Shoulder Regions, in Survivors of Head and Neck Cancer. Support. Care Cancer. 2020, 28, 2891–2898. [Google Scholar] [CrossRef] [PubMed]
- Moloney, E.C.; Brunner, M.; Alexander, A.J.; Clark, J. Quantifying Fibrosis in Head and Neck Cancer Treatment: An Overview. Head Neck. 2015, 37, 1225–1231. [Google Scholar] [CrossRef]
- Kraaijenga, S.A.C.; Oskam, I.M.; Van Der Molen, L.; Hamming-Vrieze, O.; Hilgers, F.J.M.; Van Den Brekel, M.W.M. Evaluation of Long Term (10-Years+) Dysphagia and Trismus in Patients Treated with Concurrent Chemo-Radiotherapy for Advanced Head and Neck Cancer. Oral Oncol. 2015, 51, 787–794. [Google Scholar] [CrossRef]
- Galiano-Castillo, N.; Fernández-Lao, C.; Cantarero-Villanueva, I.; Fernández-De-Las-Peñas, C.; Menjón-Beltrán, S.; Arroyo-Morales, M. Altered Pattern of Cervical Muscle Activation during Performance of a Functional Upper Limb Task in Breast Cancer Survivors. Am. J. Phys. Med. Rehabil. 2011, 90, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Ringash, J. Survivorship and Quality of Life in Head and Neck Cancer. J. Clin. Oncol. 2015, 33, 3322–3327. [Google Scholar] [CrossRef]
- Pidlyskyj, K.; Roddam, H.; Rawlinson, G.; Selfe, J. Exploring Aspects of Physiotherapy Care Valued by Breast Cancer Patients. Physiother 2014, 100, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Morishita, S.; Tsubaki, A. Physical Therapy in Patients with Cancer. In Clinical Physical Therapy, 1st ed.; Suzuki, T., Ed.; IntechOpen: London, United Kingdom, 2017. [Google Scholar] [CrossRef] [Green Version]
- Bialosky, J.E.; Beneciuk, J.M.; Bishop, M.D.; Coronado, R.A.; Penza, C.W.; Simon, C.B.; George, S.Z. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J. Orthop. Sports Phys. Ther. 2018, 48, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro da Silva, F.; Moreira, G.M.; Zomkowski, K.; Amaral de Noronha, M.; Flores Sperandio, F. Manual Therapy as Treatment for Chronic Musculoskeletal Pain in Female Breast Cancer Survivors: A Systematic Review and Meta-Analysis. J. Manip. Physiol. Ther. 2019, 42, 503–513. [Google Scholar] [CrossRef]
- Krisciunas, G.P.; Golan, H.; Marinko, L.N.; Pearson, W.; Jalisi, S.; Langmore, S.E. A novel manual therapy programme during radiation therapy for head and neck cancer - our clinical experience with five patients. Clin. Otolaryngol. 2016, 41, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Krisciunas, G.P.; Vakharia, A.; Lazarus, C.; Taborda, S.G.; Martino, R.; Hutcheson, K.; McCulloch, T.; Langmore, S.E. Application of Manual Therapy for Dysphagia in Head and Neck Cancer Patients: A Preliminary National Survey of Treatment Trends and Adverse Events. Glob. Adv. Health Med. 2019, 8, 2164956119844151. [Google Scholar] [CrossRef] [PubMed]
- Pilat, A. Myofascial Therapies: Myofascial Induction; McGraw-Hill Interamericana: Madrid, Spain, 2003. [Google Scholar]
- Castro-Martín, E.; Ortiz-Comino, L.; Gallart-Aragón, T.; Esteban-Moreno, B.; Arroyo-Morales, M.; Galiano-Castillo, N. Myofascial Induction Effects on Neck-Shoulder Pain in Breast Cancer Survivors: Randomized, Single-Blind, Placebo-Controlled Crossover Design. Arch. Phys. Med. Rehabil. 2017, 98, 832–840. [Google Scholar] [CrossRef]
- Castro-Martín, E.; Galiano-Castillo, N.; Ortiz-Comino, L.; Cantarero-Villanueva, I.; Lozano-Lozano, M.; Arroyo-Morales, M.; Fernández-Lao, C. Effects of a Single Myofascial Induction Session on Neural Mechanosensitivity in Breast Cancer Survivors: A Secondary Analysis of a Crossover Study. J. Manip. Physiol. Ther. 2020, 43, 394–404. [Google Scholar] [CrossRef]
- Serra-Añó, P.; Inglés, M.; Bou-Catalá, C.; Iraola-Lliso, A.; Espí-López, G.V. Effectiveness of Myofascial Release after Breast Cancer Surgery in Women Undergoing Conservative Surgery and Radiotherapy: A Randomized Controlled Trial. Support. Care Cancer 2019, 27, 2633–2641. [Google Scholar] [CrossRef] [PubMed]
- Fourie, W.J.; Robb, K.A. Physiotherapy Management of Axillary Web Syndrome Following Breast Cancer Treatment: Discussing the Use of Soft Tissue Techniques. Physiotherapy 2009, 95, 314–320. [Google Scholar] [CrossRef] [PubMed]
- Chamorro Comesaña, A.; Suárez Vicente, M.D.P.; Docampo Ferreira, T.; Pérez-La Fuente Varela, M.D.M.; Porto Quintáns, M.M.; Pilat, A. Effect of Myofascial Induction Therapy on Post-c-Section Scars, More than One and a Half Years Old. Pilot Study. J. Bodyw. Mov. Ther. 2017, 21, 197–204. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Campelo, N.M.; Rubens-Rebelatto, J.; Martín-Vallejo, F.J.; Alburquerque-Sendín, F.; Fernández-De-Las-Peñas, C. The Immediate Efects of Atlanto-Occipital Joint Manipulation and Suboccipital Muscle Inhibition Technique on Active Mouth Opening and Pressure Pain Sensitivity over Latent Myofascial Trigger Points in the Masticatory Muscles. J. Orthop. Sports Phys. Ther. 2010, 40, 310–317. [Google Scholar] [CrossRef] [Green Version]
- Dwan, K.; Li, T.; Altman, D.G.; Elbourne, D. CONSORT 2010 Statement: Extension to Randomised Crossover Trials. BMJ 2019, 366. [Google Scholar] [CrossRef] [Green Version]
- Patel, S.G.; Shah, J.P. TNM Staging of Cancers of the Head and Neck: Striving for Uniformity Among Diversity. CA Cancer J. Clin. 2005, 55, 242–258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diagnóstico Pela Anamnese da Disfunção Craniomandibular–ScienceOpen. Available online: https://www.scienceopen.com/document?vid=ca2c5ce5-8697-4e9b-85c9-88c70931a0da (accessed on 5 May 2021).
- Su, T.L.; Chen, A.N.; Leong, C.P.; Huang, Y.C.; Chiang, C.W.; Chen, I.H.; Lee, Y.Y. The Effect of Home-Based Program and Outpatient Physical Therapy in Patients with Head and Neck Cancer: A Randomized, Controlled Trial. Oral Oncol. 2017, 74, 130–134. [Google Scholar] [CrossRef] [PubMed]
- Audette, I.; Dumas, J.P.; Côté, J.N.; De Serres, S.J. Validity and Between-Day Reliability of the Cervical Range of Motion (CROM) Device. J. Orthop. Sports Phys. Ther. 2010, 40, 318–323. [Google Scholar] [CrossRef]
- Kolber, M.J.; Fuller, C.; Marshall, J.; Wright, A.; Hanney, W.J. The Reliability and Concurrent Validity of Scapular Plane Shoulder Elevation Measurements Using a Digital Inclinometer and Goniometer. Physiother. Theory Pract. 2012, 28, 161–168. [Google Scholar] [CrossRef]
- Rauch, A.; Schierz, O. Reliability of Mandibular Movement Assessments Depending on TMD. Cranio-J. Craniomandib. Pract. 2018, 36, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Harris, K.D.; Heer, D.M.; Roy, T.C.; Santos, D.M.; Whitman, J.M.; Wainner, R.S. Reliability of a Measurement of Neck Flexor Muscle Endurance. Phys. Ther. 2005, 85, 1349–1355. [Google Scholar] [CrossRef]
- Lee, J.S.; Hobden, E.; Stiell, I.G.; Wells, G.A. Clinically Important Change in the Visual Analog Scale after Adequate Pain Control. Acad. Emerg. Med. 2003, 10, 1128–1130. [Google Scholar] [CrossRef]
- Muir, S.W.; Corea, C.L.; Beaupre, L. Evaluating Change in Clinical Status: Reliability and Measures of Agreement for the Assessment of Glenohumeral Range of Motion. N. Am. J. Sports Phys. Ther. 2010, 5, 98–110. [Google Scholar] [PubMed]
- Lourenço, A.S.; Lameiras, C.; Silva, A.G. Neck Flexor and Extensor Muscle Endurance in Subclinical Neck Pain: Intrarater Reliability, Standard Error of Measurement, Minimal Detectable Change, and Comparison With Asymptomatic Participants in a University Student Population. J. Manipulative Physiol. Ther. 2016, 39, 427–433. [Google Scholar] [CrossRef]
- Pilat, A. Myofascial Induction Therapy (MIT). In Fascia in Osteopahty; Liem, T., Tozzi, P.C., Eds.; Handspring: Edinburgh, UK, 2017. [Google Scholar]
- Boyd, C.; Crawford, C.; Paat, C.F.; Price, A.; Xenakis, L.; Zhang, W.; Buckenmaier, C.; Buckenmaier, P.; Cambron, J.; Deery, C.; et al. The Impact of Massage Therapy on Function in Pain Populations–a Systematic Review and Meta-Analysis of Randomized Controlled Trials: Part II, Cancer Pain Populations. Pain Med. 2016, 17, 1553–1568. [Google Scholar] [CrossRef] [PubMed]
- Li, D.T.S.; Leung, Y.Y. Temporomandibular Disorders: Current Concepts and Controversies in Diagnosis and Management. Diagnostics 2021, 11, 459. [Google Scholar] [CrossRef] [PubMed]
- Loh, S.Y.; Mcleod, R.W.J.; Elhassan, H.A. Trismus Following Different Treatment Modalities for Head and Neck Cancer: A Systematic Review of Subjective Measures. Eur. Arch. Oto-Rhino-Laryngol. 2017, 274, 2695–2707. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kalamir, A.; Pollard, H.; Vitiello, A.; Bonello, R. Intra-Oral Myofascial Therapy for Chronic Myogenous Temporomandibular Disorders: A Randomized, Controlled Pilot Study. J. Man. Manip. Ther. 2010, 18, 139–146. [Google Scholar] [CrossRef] [Green Version]
- Zafar, H.; Nordh, E.; Eriksson, P.O. Temporal Coordination between Mandibular and Head-Neck Movements during Jaw Opening-Closing Tasks in Man. Arch. Oral Biol. 2000, 45, 675–682. [Google Scholar] [CrossRef]
- La Touche, R.; Fernández-De-Las-Peñas, C.; Fernández-Carnero, J.; Escalante, K.; Angulo-Díaz-Parreño, S.; Paris-Alemany, A.; Cleland, J.A. The Effects of Manual Therapy and Exercise Directed at the Cervical Spine on Pain and Pressure Pain Sensitivity in Patients with Myofascial Temporomandibular Disorders. J. Oral Rehabil. 2009, 36, 644–652. [Google Scholar] [CrossRef]
- Namvar, H.; Olyaei, G.; Moghadam, B.A.; Hosseinifar, M. Effect of Myofascial Release Technique on Pain, Disability, Maximum Isometric Contraction of the Extensor Muscles, and Pressure Pain Threshold in Patients with Chronic Nonspecific Neck Pain: Double Blinded Randomized Clinical Trial. Int. J. Med. Res. Heal. Sci. 2016, 5, 500–506. [Google Scholar]
- Gane, E.M.; McPhail, S.M.; Hatton, A.L.; Panizza, B.J.; O’Leary, S.P. Neck and Shoulder Motor Function Following Neck Dissection: A Comparison with Healthy Control Subjects. Otolaryngol.-Head Neck Surg. 2019, 160, 1009–1018. [Google Scholar] [CrossRef] [PubMed]


| Age (y) | 56.55 (12.71) |
|---|---|
| Gender Male Female | 13 (59.1) 9 (40.9) |
| Alcohol consumption None Monthly Weekly Daily | 12 (54.5) 4 (18.2) 4 (18.2) 2 (9.1) |
| Smoking habits Non smoker Ex-smoker Smoker | 8 (36.4) 11 (50) 3 (13.6) |
| Time since diagnosis (months) | 26.33 (16.68) |
| Affected-side Right Left | 11 (50) 11 (50) |
| Cancer stage I II III IV | 5 (22.7) 3 (13.6) 3 (13.6) 9 (40.9) |
| Surgery None MRND RND | 1 (4.5) 9 (40.9) 12 (54.5) |
| Radiotherapy No Yes | 1 (4.5) 21 (95.5) |
| Chemotherapy No Yes | 7 (31.8) 15 (68.2) |
| Fonseca None Light Moderate Severe | 3 (13.6) 4 (18.2) 6 (27.3) 9 (40.9) |
| VAS | MIT Session | Placebo Session | p Value * |
|---|---|---|---|
| VAS cervical Pre-intervention Post-intervention Pre–post change score | 5.32 ± 2.43 1.41 ± 2.30 −3.91 ± 2.77 † | 5.68 ± 2.47 3.59 ± 2.70 −2.09 ± 2.45 † | p = 0.026 |
| VAS affected-side shoulder Pre-intervention Post-intervention Pre–post differences | 4.41 ± 2.93 0.77 ± 1.92 −3.64 ± 3.1 † | 4.55 ± 2.89 3.95 ± 3.06 −0.59 ± 2.36 | p = 0.001 |
| VAS unaffected-side shoulder Pre-intervention Post-intervention Pre–post differences | 1.55 ± 2.80 0.36 ± 1.33 −1.18 ± 2.34 | 2.32 ± 3.19 1.27 ± 2.58 −1.05 ± 3.33 | p = 0.876 |
| Cervical ROM (deg) | MIT Session | Placebo Session | p Value * |
|---|---|---|---|
| Flexion (deg) Pre-intervention Post-intervention Pre–post change score | 47.18 ± 9.56 55.59 ± 9.06 8.41 ± 8.26 † | 43.82 ± 13.12 43.41 ± 12.28 −0.41 ± 9.66 | p = 0.002 |
| Extension (deg) Pre-intervention Post-intervention Pre–post change score | 43.86 ± 15.04 56.09 ± 14.93 12.23 ± 6.55 † | 46.27 ± 15.27 41.95 ± 15.28 −4.32 ± 8.3 | p < 0.001 |
| Affected-side rotation (deg) Pre-intervention Post-intervention Pre–post change score | 51.00 ± 15.84 65.27 ± 12.87 14.27 ± 11.05 † | 51.73 ± 12.43 52.14 ± 16.38 0.41 ± 8.12 | p < 0.001 |
| Unaffected-side rotation (deg) Pre-intervention Post-intervention Pre–post change score | 51.41 ± 15.25 63.14 ± 10.03 11.73 ± 8.65 † | 51.45 ± 15.70 50.68 ± 12.46 −0.77 ± 8.56 | p < 0.001 |
| Affected-side lateroflexion (deg) Pre-intervention Post-intervention Pre–post change score | 30.14 ± 9.04 38.09 ± 8.77 7.95 ± 5.1 † | 31.64 ± 11.35 29.55 ± 8.76 −2.09 ± 7.88 | p < 0.001 |
| Unaffected-side lateroflexion (deg) ** Pre-intervention Post-intervention Pre–post change score | 30.75 ± 9.39 38.32 ± 10.06 9.55 ± 6.6 † | 32.73 ± 11.47 29.36 ± 9.51 −3.36 ± 10.71 | p = 0.003 |
| Shoulder ROM (deg) | MIT Session | Placebo Session | p Value * |
|---|---|---|---|
| Affected-side flexion (deg) Pre-intervention Post-intervention Pre–post change score | 152.86 ± 25.23 161.41 ± 23.28 8.55 ± 7.63 | 142.23 ± 29.51 144.86 ± 31.63 2.64 ± 13.45 | p = 0.080 |
| Unaffected-side flexion (deg) Pre-intervention Post-intervention Pre–post change score | 161.05 ± 18.04 161.27 ± 21.15 3.61 ± 6.86 | 154.10 ± 20.78 154.32 ± 25.14 3.28 ± 9.86 | p = 0.900 |
| Affected-side abduction (deg) Pre-intervention Post-intervention Pre–post change score | 138.09 ± 34.01 148.09 ± 35.73 10 ± 17.32 | 126.36 ± 43.28 131.27 ± 42.71 4.91 ± 19.24 | p = 0.362 |
| Unaffected-side abduction (deg) Pre-intervention Post-intervention Pre–post change score | 151.43 ± 33.80 154.41 ± 27.30 5.10 ± 10.70 | 132.14 ± 41.23 139.36 ± 37.58 7.23 ± 26.18 | p = 0.731 |
| Affected-side external rotation (deg) Pre-intervention Post-intervention Pre–post change score | 67.05 ± 24.08 74.05 ± 21.39 7 ± 11.20 | 73.18 ± 22.65 73.86 ± 22.63 0.68 ± 9.41 | p = 0.049 |
| Unaffected-side external rotation (deg) Pre-intervention Post-intervention Pre–post change score | 72.76 ± 22.68 71.27 ± 22.97 0.48 ± 10.15 | 74.64 ± 18.75 73.36 ± 20.76 −1.27 ± 15.88 | p = 0.671 |
| Affected-side internal rotation (deg) Pre-intervention Post-intervention Pre–post change score | 71.77 ± 15.55 76.55 ± 16.03 4.77 ± 8.04 | 67.32 ± 18.12 67.68 ± 18.34 0.36 ± 11.84 | p = 0.156 |
| Unaffected-side internal rotation (deg) Pre-intervention Post-intervention Pre–post change score | 73.38 ± 14.92 70.73 ± 18.09 −0.71 ± 7.77 | 75.45 ± 19.20 67.73 ± 23.04 −7.73 ± 19.33 | p = 0.130 |
| MIT Session | Placebo Session | p Value * | |
|---|---|---|---|
| MMO (mm) Pre-intervention Post-intervention Pre–post change score | 33.14 ± 10.96 36.5 ± 11.55 3.36 ± 3.4 † | 30.05 ± 10.21 29.68 ± 11.33 −0.36 ± 2.50 | p < 0.001 |
| DCFET (s) Pre-intervention Post-intervention Pre–post change score | 11.10 ± 7.95 19.19 ± 10.05 8.09 ± 6.96 † | 9.70 ± 7.53 9.07 ± 7.86 −0.63 ± 4.26 | p < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castro-Martín, E.; Galiano-Castillo, N.; Fernández-Lao, C.; Ortiz-Comino, L.; Postigo-Martin, P.; Arroyo-Morales, M. Myofascial Induction Therapy Improves the Sequelae of Medical Treatment in Head and Neck Cancer Survivors: A Single-Blind, Placebo-Controlled, Randomized Cross-Over Study. J. Clin. Med. 2021, 10, 5003. https://doi.org/10.3390/jcm10215003
Castro-Martín E, Galiano-Castillo N, Fernández-Lao C, Ortiz-Comino L, Postigo-Martin P, Arroyo-Morales M. Myofascial Induction Therapy Improves the Sequelae of Medical Treatment in Head and Neck Cancer Survivors: A Single-Blind, Placebo-Controlled, Randomized Cross-Over Study. Journal of Clinical Medicine. 2021; 10(21):5003. https://doi.org/10.3390/jcm10215003
Chicago/Turabian StyleCastro-Martín, Eduardo, Noelia Galiano-Castillo, Carolina Fernández-Lao, Lucía Ortiz-Comino, Paula Postigo-Martin, and Manuel Arroyo-Morales. 2021. "Myofascial Induction Therapy Improves the Sequelae of Medical Treatment in Head and Neck Cancer Survivors: A Single-Blind, Placebo-Controlled, Randomized Cross-Over Study" Journal of Clinical Medicine 10, no. 21: 5003. https://doi.org/10.3390/jcm10215003
APA StyleCastro-Martín, E., Galiano-Castillo, N., Fernández-Lao, C., Ortiz-Comino, L., Postigo-Martin, P., & Arroyo-Morales, M. (2021). Myofascial Induction Therapy Improves the Sequelae of Medical Treatment in Head and Neck Cancer Survivors: A Single-Blind, Placebo-Controlled, Randomized Cross-Over Study. Journal of Clinical Medicine, 10(21), 5003. https://doi.org/10.3390/jcm10215003









