VEGF Concentration in a Preovulatory Leading Follicle Relates to Ovarian Reserve and Oocyte Maturation during Ovarian Stimulation with GnRH Antagonist Protocol in In Vitro Fertilization Cycle
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Grouping
2.2. Protocol Procedures
2.2.1. Ovarian Stimulation
2.2.2. Follicular Fluid (FF) Samples and Oocyte Retrieval
2.2.3. Measurement of Intrafollicular VEGF Level
2.2.4. Serum Hormone Assays
2.3. Statistical Analysis
3. Results
Main Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chowdhury, M.W.; Scaramuzzi, R.J.; Wheeler-Jones, C.P.; Khalid, M. The expression of angiogenic growth factors and their receptors in ovarian follicles throughout the estrous cycle in the ewe. Theriogenology 2010, 73, 856–872. [Google Scholar] [CrossRef]
- Huey, S.; Abuhamad, A.; Barroso, G.; Hsu, M.I.; Kolm, P.; Mayer, J.; Oehninger, S. Perifollicular blood flow Doppler indices, but not follicular PO2, PCO2, or Ph, predict oocyte developmental competence in in vitro fertilization. Fertil. Steril. 1999, 72, 707–712. [Google Scholar] [CrossRef]
- Bhal, P.S.; Pugh, N.D.; Gregory, L.; O’Brien, S.; Shaw, R.W. Perifollicular vascularity as a potential variable affecting outcome in stimulated intrauterine insemination treatment cycles: A study using transvaginal power Doppler. Hum. Reprod. 2001, 16, 1682–1689. [Google Scholar] [CrossRef] [Green Version]
- Shibuya, M. Vascular endothelial growth factor (Vegf) and its receptor (Vegfr) signaling in angiogenesis: A crucial target for anti- and pro-angiogenic therapies. Genes Cancer 2001, 12, 1097–1105. [Google Scholar] [CrossRef]
- Akiyama, I.; Yoshino, O.; Osuga, Y.; Shi, J.; Harada, M.; Koga, K.; Hirota, Y.; Hirata, T.; Fujii, T.; Saito, S.; et al. Bone morphogenetic protein 7 increased vascular endothelial growth factor (Vegf)—A expression in human granulosa cells and Vegf receptor expression in endothelial cells. Reprod. Sci. 2014, 21, 477–482. [Google Scholar] [CrossRef] [Green Version]
- Berisha, B.; Schams, D.; Rodler, D.; Pfaffl, M.W. Angiogenesis in the ovary—The most important regulatory event for follicle and corpus luteum development and function in cow—An overview. Anat. Histol. Embryol. 2016, 45, 124–130. [Google Scholar] [CrossRef]
- Wulff, C.; Wilson, H.; Wiegand, S.J.; Rudge, J.S.; Fraser, H.M. Prevention of thecal angiogenesis, antral follicular growth, and ovulation in the primate by treatment with vascular endothelial growth factor trap R1r2. Endocrinology 2002, 143, 2797–2807. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.Y.; Fortune, J.E. Vascular endothelial growth factor stimulates the primary to secondary follicle transition in bovine follicles in vitro. Mol. Reprod. Dev. 2007, 74, 1095–1104. [Google Scholar] [CrossRef] [PubMed]
- Geva, E.; Jaffe, R.B. Role of vascular endothelial growth factor in ovarian physiology and pathology. Fertil. Steril. 2000, 74, 429–438. [Google Scholar] [CrossRef]
- Artini, P.G.; Ruggiero, M.; Monteleone, P.; Carpi, A.; Cristello, F.; Cela, V.; Genazzani, A.R. Vascular endothelial growth factor and its soluble receptor in benign and malignant ovarian tumors. Biomed Pharm. 2008, 62, 373–377. [Google Scholar] [CrossRef]
- Stouffer, R.L.; Martinez-Chequer, J.C.; Molskness, T.A.; Xu, F.; Hazzard, T.M. Regulation and action of angiogenic factors in the primate ovary. Arch. Med. Res. 2001, 32, 567–575. [Google Scholar] [CrossRef]
- Ocal, P.; Aydin, S.; Cepni, I.; Idil, S.; Idil, M.; Uzun, H.; Benian, A. Follicular fluid concentrations of vascular endothelial growth factor, inhibin a and inhibin B in Ivf cycles: Are they markers for ovarian response and pregnancy outcome? Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 115, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Bokal, E.V.; Vrtovec, H.M.; Virant Klun, I.; Verdenik, I. Prolonged Hcg action affects angiogenic substances and improves follicular maturation, oocyte quality and fertilization competence in patients with polycystic ovarian syndrome. Hum. Reprod. 2005, 20, 1562–1568. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van der Spuy, Z.M.; Dyer, S.J. The pathogenesis of infertility and early pregnancy loss in polycystic ovary syndrome. Best Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 755–771. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, R.; Jacobs, H.; Payne, N.; Conway, G. Concentration of vascular endothelial growth factor released by cultured human luteinized granulosa cells is higher in women with polycystic ovaries than in women with normal ovaries. Fertil. Steril. 2002, 78, 1164–1169. [Google Scholar] [CrossRef]
- Hirshfield, A.N. Development of follicles in the mammalian ovary. Int. Rev. Cytol. 1991, 124, 43–101. [Google Scholar] [PubMed]
- Kuo, S.W.; Ke, F.C.; Chang, G.D.; Lee, M.T.; Hwang, J.J. Potential role of follicle-stimulating hormone (Fsh) and transforming growth factor (Tgfbeta1) in the regulation of ovarian angiogenesis. J. Cell Physiol. 2011, 226, 1608–1619. [Google Scholar] [CrossRef]
- Anasti, J.N.; Kalantaridou, S.N.; Kimzey, L.M.; George, M.; Nelson, L.M. Human follicle fluid vascular endothelial growth factor concentrations are correlated with luteinization in spontaneously developing follicles. Hum. Reprod. 1998, 13, 1144–1147. [Google Scholar] [CrossRef] [Green Version]
- Tropea, A.; Miceli, F.; Minici, F.; Tiberi, F.; Orlando, M.; Gangale, M.F.; Romani, F.; Catino, S.; Mancuso, S.; Navarra, P.; et al. Regulation of vascular endothelial growth factor synthesis and release by human luteal cells in vitro. J. Clin. Endocrinol. Metab. 2006, 91, 2303–2309. [Google Scholar] [CrossRef] [Green Version]
- Taylor, P.D.; Wilson, H.; Hillier, S.G.; Wiegand, S.J.; Fraser, H.M. Effects of inhibition of vascular endothelial growth factor at time of selection on follicular angiogenesis, expansion, development and atresia in the marmoset. Mol. Hum. Reprod. 2007, 13, 729–736. [Google Scholar] [CrossRef] [Green Version]
- Broekmans, F.J.; Kwee, J.; Hendriks, D.J.; Mol, B.W.; Lambalk, C.B. A systematic review of tests predicting ovarian reserve and ivf outcome. Hum. Reprod. Update 2006, 12, 685–718. [Google Scholar] [CrossRef] [Green Version]
- Abdalla, H.; Thum, M.Y. An elevated basal fsh reflects a quantitative rather than qualitative decline of the ovarian reserve. Hum. Reprod. 2004, 19, 893–898. [Google Scholar] [CrossRef] [Green Version]
- Tolikas, A.; Tsakos, E.; Gerou, S.; Prapas, Y.; Loufopoulos, A. Anti-Mullerian hormone (Amh) levels in serum and follicular fluid as predictors of ovarian response in stimulated (ivf and icsi) cycles. Hum. Fertil. 2001, 14, 246–253. [Google Scholar] [CrossRef] [PubMed]
- La Marca, A.; Broekmans, F.J.; Volpe, A.; Fauser, B.C.; Macklon, N.S. Eshre Special Interest Group for Reproductive Endocrinology--AMH Round Table. Anti-Mullerian hormone (Amh): What do we still need to know? Hum. Reprod. 2009, 24, 2264–2275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, A.Z.; Herring, A.H.; Kesner, J.S.; Meadows, J.W.; Stanczyk, F.Z.; Hoberman, S.; Baird, D.D. Antimullerian hormone as a predictor of natural fecundability in women aged 30-42 years. Obstet. Gynecol. 2011, 117, 798–804. [Google Scholar] [CrossRef] [Green Version]
- Jaswa, E.G.; McCulloch, C.E.; Simbulan, R.; Cedars, M.I.; Rosen, M.P. Diminished ovarian reserve is associated with reduced euploid rates via preimplantation genetic testing for aneuploidy independently from age: Evidence for concomitant reduction in oocyte quality with quantity. Fertil. Steril. 2021, 115, 966–973. [Google Scholar] [CrossRef] [PubMed]
- Datta, A.K.; Campbell, S.; Felix, N.; Singh, J.S.H.; Nargund, G. Oocyte or embryo number needed to optimize live birth and cumulative live birth rates in mild stimulation IVF cycles. Reprod. Biomed Online 2021, 43, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Hariton, E.; Kim, K.; Mumford, S.L.; Palmor, M.; Bortoletto, P.; Cardozo, E.R.; Karmon, A.E.; Sabatini, M.E.; Styer, A.K. Total number of oocytes and zygotes are predictive of live birth pregnancy in fresh donor oocyte in vitro fertilization cycles. Fertil. Steril. 2017, 108, 262–268. [Google Scholar] [CrossRef] [Green Version]
- Steward, R.G.; Lan, L.; Shah, A.A.; Yeh, J.S.; Price, T.M.; Goldfarb, J.M.; Muasher, S.J. Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: An analysis of 256,381 in vitro fertilization cycles . Fertil. Steril. 2014, 101, 967–973. [Google Scholar] [CrossRef]
- Esteves, S.C.; Roque, M.; Sunkara, S.K.; Conforti, A.; Ubaldi, F.M.; Humaidan, P.; Alviggi, C. Oocyte quantity, as well as oocyte quality, plays a significant role for the cumulative live birth rate of a POSEIDON criteria patient. Hum. Reprod. 2019, 34, 2555–2557. [Google Scholar] [CrossRef]
- Vermey, B.G.; Chua, S.J.; Zafarmand, M.H.; Wang, R.; Longobardi, S.; Cottell, E.; Beckers, F.; Mol, B.W.; Venetis, C.A.; D’Hooghe, T. Is there an association between oocyte number and embryo quality? A systematic review and meta-analysis. Reprod. Biomed Online 2019, 39, 751–763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liang, C.; Zhang, X.; Qi, C.; Hu, H.; Zhang, Q.; Zhu, X.; Fu, Y. UHPLC-MS-MS analysis of oxylipins metabolomics components of follicular fluid in infertility individuals with diminished ovarian reserve. Reprod. Biol. Endocrinol. 2021, 19, 143. [Google Scholar] [CrossRef]
- Poormoosavi, S.M.; Behmanesh, M.A.; Varzi, H.N.; Mansouri, S.; Janati, S. The effect of follicular fluid selenium concentration on oocyte maturation in women woth polycystic ovarian syndrome undergoing in vitro fertilization/Intracytoplasmic sperm injection: A cross-sectional study. Int. J. Reprod. Biomed 2021, 19, 689–698. [Google Scholar]
- Vural, F.; Vural, B.; Doger, E.; Cakiroglu, Y.; Cekmen, M. Perifollicular blood flow and its relationship with endometrial vascularity, follicular fluid Eg-Vegf, Igf-1, and Inhibin-a levels and Ivf outcomes. J. Assist. Reprod. Genet. 2016, 33, 1355–1362. [Google Scholar] [CrossRef] [Green Version]
- Dumesic, D.A.; Meldrum, D.R.; Katz-Jaffe, M.G.; Krisher, R.L.; Schoolcraft, W.B. Oocyte environment: Follicular fluid and cumulus cells are critical for oocyte health. Fertil. Steril. 2015, 103, 303–316. [Google Scholar] [CrossRef] [PubMed]
- Kaya, A.; Atabekoglu, C.S.; Kahraman, K.; Taskin, S.; Ozmen, B.; Berker, B.; Sonmezer, M. Follicular fluid concentrations of Igf-I, Igf-Ii, Igfbp-3, Vegf, Amh, and Inhibin-B in women undergoing controlled ovarian hyperstimulation using Gnrh agonist or Gnrh antagonist. Eur. J. Obstet. Gynecol. Reprod. Biol. 2012, 164, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Artini, P.G.; Monti, M.; Matteucci, C.; Valentino, V.; Cristello, F.; Genazzani, A.R. Vascular endothelial growth factor and basic fibroblast growth factor in polycystic ovary syndrome during controlled ovarian hyperstimulation. Gynecol. Endocrinol. 2006, 22, 465–470. [Google Scholar] [CrossRef]
- Friedman, C.I.; Danforth, D.R.; Herbosa-Encarnacion, C.; Arbogast, L.; Alak, B.M.; Seifer, D.B. Follicular fluid vascular endothelial growth factor concentrations are elevated in women of advanced reproductive age undergoing ovulation induction. Fertil. Steril. 1997, 68, 607–612. [Google Scholar] [CrossRef]
- Klein, N.A.; Battaglia, D.E.; Woodruff, T.K.; Padmanabhan, V.; Giudice, L.C.; Bremner, W.J.; Soules, M.R. Ovarian follicular concentrations of activin, follistatin, inhibin, insulin-like growth factor I (Igf-I), Igf-Ii, Igf-binding protein-2 (Igfbp-2), Igfbp-3, and vascular endothelial growth factor in spontaneous menstrual cycles of normal women of advanced reproductive age. J. Clin. Endocrinol. Metab. 2000, 85, 4520–4525. [Google Scholar] [PubMed] [Green Version]
- Artini, P.G.; Monti, M.; Cristello, F.; Matteucci, C.; Bruno, S.; Valentino, V.; Genazzani, A.R. Vascular endothelial growth factor in females of reproductive age. Gynecol. Endocrinol. 2003, 17, 477–492. [Google Scholar] [CrossRef]
- Schafer, G.; Cramer, T.; Suske, G.; Kemmner, W.; Wiedenmann, B.; Hocker, M. Oxidative stress regulates vascular endothelial growth factor-a gene transcription through Sp1- and Sp3-dependent activation of two proximal Gc-rich promoter elements. J. Biol. Chem. 2003, 278, 8190–8198. [Google Scholar] [CrossRef]
- Wang, G.L.; Jiang, B.H.; Rue, E.A.; Semenza, G.L. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-pas heterodimer regulated by cellular O2 tension. Proc. Natl. Acad. Sci. USA 1995, 92, 5510–5514. [Google Scholar] [CrossRef] [Green Version]
- Gaulden, M.E. Maternal age effect: The enigma of Down syndrome and other trisomic conditions. Mutat. Res. 1992, 296, 69–88. [Google Scholar] [CrossRef]
- Ferrara, N.; Frantz, G.; LeCouter, J.; Dillard-Telm, L.; Pham, T.; Draksharapu, A. Differential expression of the angiogenic factor genes vascular endothelial growth factor (VEGF) and endocrine gland-derived VEGF in normal and polycystic human ovaries. Am. J. Pathol. 2003, 162, 1881–1892. [Google Scholar] [CrossRef] [Green Version]
- Delgado-Rosas, F.; Gaytan, M.; Morales, C.; Gomez, R.; Gaytan, F. Superficial ovarian cortex vascularization is inversely related to the follicle reserve in normal cycling ovaries and is increased in polycystic ovary syndrome. Hum. Reprod. 2009, 24, 1142–1151. [Google Scholar] [CrossRef] [Green Version]
- Cunha-Filho, J.S.; Lemos, N.; Stein, N.; Laranjeira, A.; Passos, E.P. Vascular endothelial growth factor and inhibin a in follicular fluid of infertile patients who underwent in vitro fertilization with a gonadotropin-releasing hormone antagonist. Fertil. Steril. 2005, 83, 902–907. [Google Scholar] [CrossRef] [PubMed]
- Battaglia, C.; Genazzani, A.D.; Regnani, G.; Primavera, M.R.; Petraglia, F.; Volpe, A. Perifollicular Doppler flow and follicular fluid vascular endothelial growth factor concentrations in poor responders. Fertil. Steril. 2000, 74, 809–812. [Google Scholar] [CrossRef]
- Esposito, M.A.; Coutifaris, C.; Barnhart, K.T. A moderately elevated day 3 Fsh concentration has limited predictive value, especially in younger women. Hum. Reprod. 2002, 17, 118–123. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.C.; Li, Y.P.; Pan, S.P.; Chao, K.H.; Chang, C.H.; Yang, J.H.; Chen, S.U. The different impact of stimulation duration on oocyte maturation and pregnancy outcome in fresh cycles with Gnrh antagonist protocol in poor responders and normal responders. Taiwan J. Obstet. Gynecol. 2019, 58, 471–476. [Google Scholar] [CrossRef]
- Fang, L.; Li, Y.; Wang, S.; Li, Y.; Chang, H.-M.; Yi, Y.; Yan, Y.; Thakur, A.; Leung, P.C.K.; Cheng, J.-C.; et al. TGF-beta1 induces VEGF expression in human granulosa-lutein cells: A potential mechanism for the pathogenesis of ovarian hyperstimulation syndrome. Exp. Mol. Med. 2020, 52, 450–460. [Google Scholar] [CrossRef]
- Poseidon Group; Alviggi, C.; Andersen, C.Y.; Buehler, K.; Conforti, A.; De Placido, G.; Esteves, S.; Fischer, R.; Galliano, D.; Polyzos, N.P.; et al. A new more detailed stratification of low responders to ovarian stimulation: From a poor ovarian response to a low prognosis concept. Fertil. Steril. 2016, 105, 1452–1453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haahr, T.; Dosouto, C.; Alviggi, C.; Esteves, S.C.; Humaidan, P. Management strategies for POSEIDON groups 3 and 4. Front. Endocrinol. 2019, 10, 614. [Google Scholar] [CrossRef] [PubMed]
- Pandian, Z.; McTavish, A.R.; Aucott, L.; Hamilton, M.P.; Bhattacharya, S. Interventions for ‘poor responders’ to controlled ovarian hyper stimulation (COH) in in-vitro fertilisation (IVF). Cochrane Database Syst. Rev. 2010, 1, CD004379. [Google Scholar] [CrossRef]
- Revelli, A.; Chiado, A.; Dalmasso, P.; Stabile, V.; Evangelista, F.; Basso, G.; Benedetto, C. “Mild” vs. “long” protocol for controlled ovarian hyperstimulation in patients with expected poor ovarian responsiveness undergoing in vitro fertilization (IVF): A large prospective randomized trial. J. Assist. Reprod. Genet. 2014, 31, 809–815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
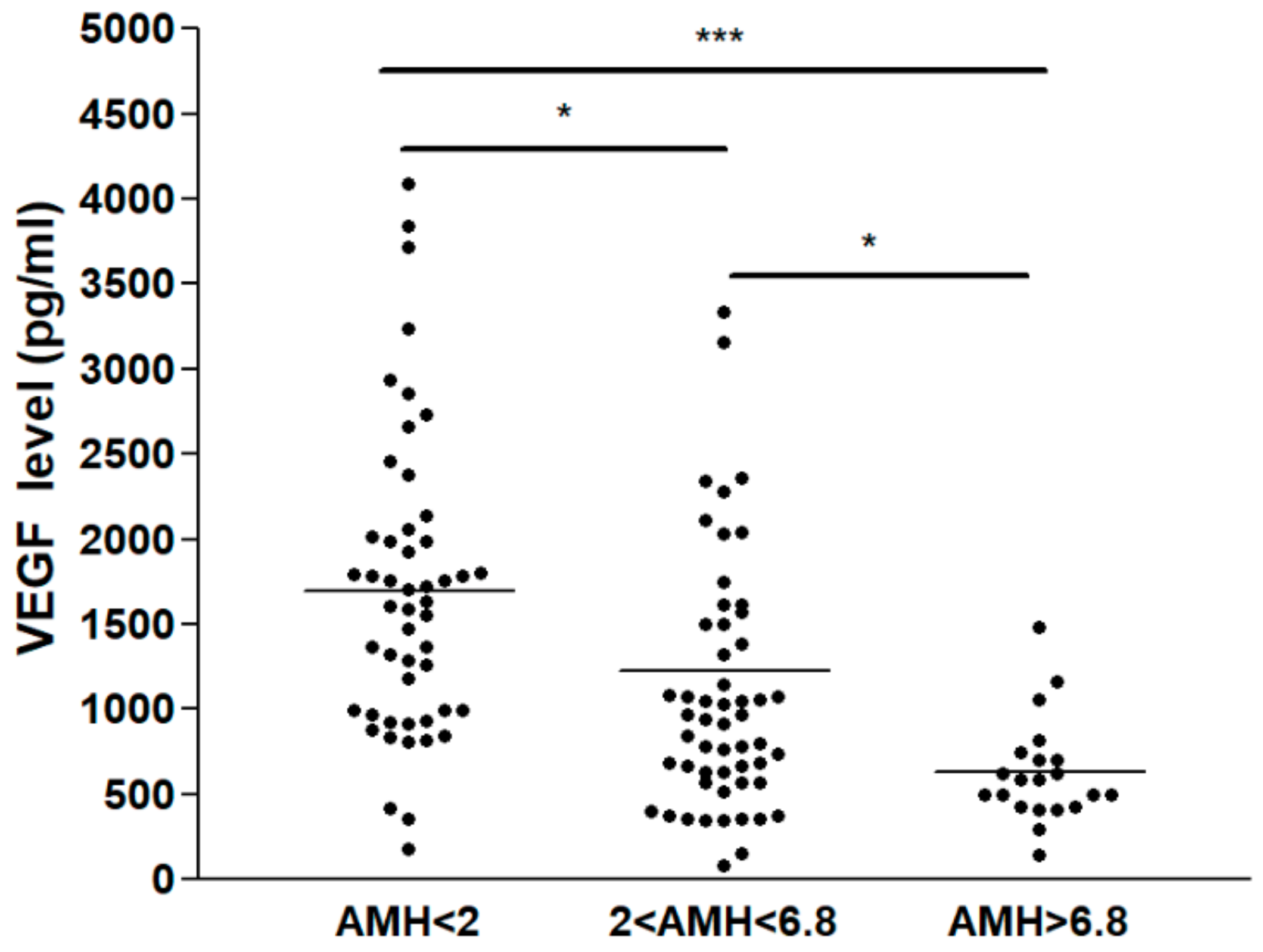


| Group A (AMH < 2.0 ng/mL) | Group B (2.0 ≤ AMH ≤ 6.8 ng/mL) | Group C (AMH > 6.8 ng/mL) | p-Value | |
|---|---|---|---|---|
| No. of patients | 81 | 81 | 23 | |
| Age (y) | 40.8 ± 3.7 | 36.9 ± 4.4 | 34.0 ± 5.1 | <0.05 |
| BMI (kg/m2) | 21.5 ± 0.5 | 22.2 ± 0.6 | 21.7 ± 0.6 | 0.56 |
| AMH (ng/mL) | 0.8 ± 0.5 | 3.7 ± 2.5 | 11.0 ± 4.3 | <0.05 |
| AFC (No.) | 5.3 ± 3.1 | 13.5 ± 5.7 | 25.1 ± 11.4 | <0.05 |
| Basal FSH (mIU/mL) | 10.0 ± 3.9 | 7.2 ± 2.2 | 6.7 ± 2.9 | <0.05 |
| Basal LH (mIU/mL) | 5.0 ± 2.2 | 5.2 ± 2.0 | 6.0 ± 3.2 | 0.247 |
| Basal E2 (pg/mL) | 32.8 ± 19.0 | 31.7 ± 20.9 | 37.9 ± 20.3 | 0.482 |
| Basal P4 (ng/mL) | 0.5 ± 0.5 | 0.4 ± 0.3 | 0.5 ± 0.4 | 0.929 |
| Total FSH dose (IU) | 1975.5 ± 796.6 | 2136.9 ± 856.4 | 1966.7 ± 720.1 | 0.514 |
| Total LH dose (IU) | 703.1 ± 529.8 | 757.7 ± 711.3 | 900.0 ± 710.8 | 0.632 |
| Stimulation duration (d) | 9.0 ± 1.1 | 9.3 ± 1.1 | 8.6 ± 1.0 | <0.05 |
| E2 on hCG day (pg/mL) | 1039.8 ± 736.5 | 1793.7 ± 756.6 | 3569.3 ± 2133.4 | <0.05 |
| LH on hCG day (mIU/mL) | 7.1 ± 6.9 | 2.7 ± 2.2 | 3.6 ± 2.9 | <0.05 |
| P4 on hCG day (ng/mL) | 0.7 ± 0.6 | 1.2 ± 1.9 | 1.2 ± 0.8 | 0.17 |
| VEGF in FF (pg/mL) | 1692.2 ± 124.1 | 1222.4 ± 137.8 | 627.9 ± 66.7 | <0.05 |
| Oocyte No. | 3.7 ± 3.6 | 12.0 ± 7.3 | 23.7 ± 12.0 | <0.05 |
| MII oocyte No. | 3.3 ± 0.6 | 7.7 ± 0.9 | 18.3 ± 1.9 | <0.05 |
| Oocyte maturation rate * | 264/398 (66.3%) | 694/961 (72.2%) | 499/659 (75.7%) | <0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, W.-B.; Chen, H.-T.; Lin, J.-J.; Lai, T.-H. VEGF Concentration in a Preovulatory Leading Follicle Relates to Ovarian Reserve and Oocyte Maturation during Ovarian Stimulation with GnRH Antagonist Protocol in In Vitro Fertilization Cycle. J. Clin. Med. 2021, 10, 5032. https://doi.org/10.3390/jcm10215032
Wu W-B, Chen H-T, Lin J-J, Lai T-H. VEGF Concentration in a Preovulatory Leading Follicle Relates to Ovarian Reserve and Oocyte Maturation during Ovarian Stimulation with GnRH Antagonist Protocol in In Vitro Fertilization Cycle. Journal of Clinical Medicine. 2021; 10(21):5032. https://doi.org/10.3390/jcm10215032
Chicago/Turabian StyleWu, Wen-Bin, Hsuan-Ting Chen, Jun-Jie Lin, and Tsung-Hsuan Lai. 2021. "VEGF Concentration in a Preovulatory Leading Follicle Relates to Ovarian Reserve and Oocyte Maturation during Ovarian Stimulation with GnRH Antagonist Protocol in In Vitro Fertilization Cycle" Journal of Clinical Medicine 10, no. 21: 5032. https://doi.org/10.3390/jcm10215032






