The Mediating Role of Orthorexia in the Relationship between Physical Activity and Fear of COVID-19 among University Students in Poland
Abstract
:1. Introduction
1.1. Impact of COVID-19 on Lifestyle
1.2. Healthy Lifestyle among University Students
1.3. Orthorexia Nervosa
1.4. Fear of COVID-19
1.5. The Relationships between Physical Activity, Orthorexia, and Fear of COVID-19
1.6. The Current Study
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Measures
2.4. Statistical Analyses
3. Results
3.1. Descriptive Statistics
3.2. Group Comparisons
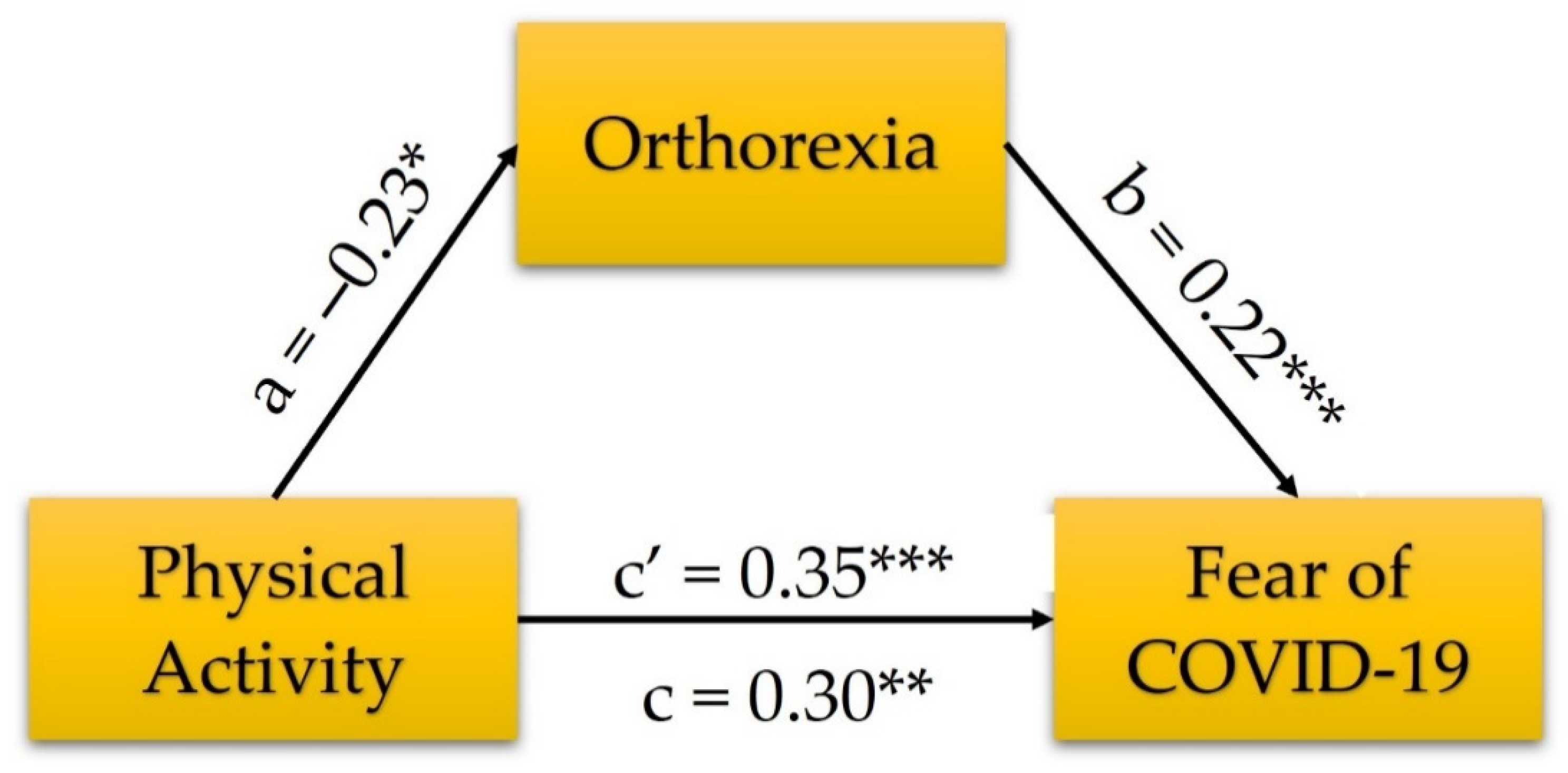
3.3. The Relationships between PA, Orthorexia, and Fear of COVID-19
4. Discussion
4.1. Associations between Variables
4.2. Orthorexia, Fear of COVID-19, and PA among University Students
4.3. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Beltekian, D.; Roser, M. (2020)-Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. Available online: https://ourworldindata.org/coronavirus (accessed on 28 October 2021).
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- Muyor-Rodríguez, J.; Caravaca-Sánchez, F.; Fernández-Prados, J.S. COVID-19 Fear, Resilience, Social Support, Anxiety, and Suicide among College Students in Spain. Int. J. Environ. Res. Public Health 2021, 18, 8156. [Google Scholar] [CrossRef]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746,217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, 181. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors Associated with Mental Health Disorders among University Students in France Confined during the COVID-19 Pandemic. JAMA Netw. Open. 2020, 3, 2025591. [Google Scholar] [CrossRef] [PubMed]
- Aslan, I.; Ochnik, D.; Çınar, O. Exploring Perceived Stress among Students in Turkey during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8961. [Google Scholar] [CrossRef]
- Ochnik, D.; Rogowska, A.M.; Kuśnierz, C.; Jakubiak, M.; Schütz, A.; Held, M.J.; Arzenšek, A.; Benatov, J.; Berger, R.; Korchagina, E.V.; et al. Comparison of Depression and Anxiety among University Students in Nine Countries during the COVID-19 Pandemic. J. Clin. Med. 2021, 10, 2882. [Google Scholar] [CrossRef] [PubMed]
- Rogowska, A.M.; Kuśnierz, C.; Bokszczanin, A. Examining Anxiety, Life Satisfaction, General Health, Stress and Coping Styles during COVID-19 Pandemic in Polish Sample of University Students. Psychol. Res. Behav. Manag. 2020, 13, 797–811. [Google Scholar] [CrossRef]
- Deng, J.; Zhou, F.; Hou, W.; Silver, Z.; Wong, C.Y.; Chang, O.; Drakos, A.; Zuo, Q.K.; Huang, E. The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. 2021, 301, 113863. [Google Scholar] [CrossRef]
- Al-Musharaf, S. Prevalence and Predictors of Emotional Eating among Healthy Young Saudi Women during the COVID-19 Pandemic. Nutrients 2020, 12, 2923. [Google Scholar] [CrossRef]
- Bennett, G.; Young, E.; Butler, I.; Coe, S. The Impact of Lockdown during the COVID-19 Outbreak on Dietary Habits in Various Population Groups: A Scoping Review. Front. Nutr. 2021, 8, 626432. [Google Scholar] [CrossRef]
- Cecchetto, C.; Aiello, M.; Gentili, C.; Ionta, S.; Osimo, S.A. Increased emotional eating during COVID-19 associated with lockdown, psychological and social distress. Appetite 2021, 160, 105122. [Google Scholar] [CrossRef] [PubMed]
- Celorio-Sardà, R.; Comas-Basté, O.; Latorre-Moratalla, M.L.; Zerón-Rugerio, M.F.; Urpi-Sarda, M.; Illán-Villanueva, M.; Farran-Codina, A.; Izquierdo-Pulido, M.; Vidal-Carou, M.d.C. Effect of COVID-19 Lockdown on Dietary Habits and Lifestyle of Food Science Students and Professionals from Spain. Nutrients 2021, 13, 1494. [Google Scholar] [CrossRef]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Enriquez-Martinez, O.G.; Martins, M.C.T.; Pereira, T.S.S.; Pacheco, S.O.S.; Pacheco, F.J.; Lopez, K.V.; Huancahuire-Vega, S.; Silva, D.A.; Mora-Urda, A.I.; Rodriguez-Vásquez, M.; et al. Diet and Lifestyle Changes during the COVID-19 Pandemic in Ibero-American Countries: Argentina, Brazil, Mexico, Peru, and Spain. Front. Nutr. 2021, 8, 671004. [Google Scholar] [CrossRef]
- Galali, Y. The impact of COVID-19 confinement on the eating habits and lifestyle changes: A cross sectional study. Food Sci. Nutr. 2021, 9, 2105–2113. [Google Scholar] [CrossRef] [PubMed]
- Izzo, L.; Santonastaso, A.; Cotticelli, G.; Federico, A.; Pacifico, S.; Castaldo, L.; Colao, A.; Ritieni, A. An Italian Survey on Dietary Habits and Changes during the COVID-19 Lockdown. Nutrients 2021, 13, 1197. [Google Scholar] [CrossRef] [PubMed]
- López-Moreno, M.; López, M.T.I.; Miguel, M.; Garcés-Rimón, M. Physical and Psychological Effects Related to Food Habits and Lifestyle Changes Derived from COVID-19 Home Confinement in the Spanish Population. Nutrients 2020, 12, 3445. [Google Scholar] [CrossRef]
- Phillipou, A.; Meyer, D.; Neill, E.; Tan, E.J.; Toh, W.L.; Van Rheenen, T.E.; Rossell, S.L. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. Int. J. Eat. Disord. 2020, 53, 1158–1165. [Google Scholar] [CrossRef]
- Sulejmani, E.; Hyseni, A.; Xhabiri, G.; Rodríguez-Pérez, C. Relationship in dietary habits variations during COVID-19 lockdown in Kosovo: The COVIDiet study. Appetite 2021, 164, 105244. [Google Scholar] [CrossRef]
- Jia, P.; Liu, L.; Xie, X.; Yuan, C.; Che, N.H.; Guo, B.; Zhou, J.; Yang, S. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite 2021, 158, 105015. [Google Scholar] [CrossRef]
- Santana, J.D.M.; Milagres, M.P.; Silva Dos Santos, C.; Brazil, J.M.; Lima, E.R.; Pereira, M. Dietary intake of university students during COVID-19 social distancing in the Northeast of Brazil and associated factors. Appetite 2021, 162, 105172. [Google Scholar] [CrossRef]
- Taeymans, J.; Luijckx, E.; Rogan, S.; Haas, K.; Baur, H. Physical Activity, Nutritional Habits, and Sleeping behavior in Students and Employees of a Swiss University during the COVID-19 Lockdown Period: Questionnaire Survey Study. JMIR Public Health Surveill. 2021, 7, 26330. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Pavlova, I.; Kuśnierz, C.; Ochnik, D.; Bodnar, I.; Petrytsa, P. Does Physical Activity Matter for the Mental Health of University Students during the COVID-19 Pandemic? J. Clin. Med. 2020, 9, 3494. [Google Scholar] [CrossRef] [PubMed]
- Rogowska, A.M.; Kuśnierz, C.; Pavlova, I. Healthy behavior of physical education university students. Health Prob. Civiliz. 2020, 14, 247–255. [Google Scholar] [CrossRef]
- Rogowska, A.M. Healthy behavior patterns among physical education students. J. Phys. Educ. Health 2020, 9, 5–11. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Pavlova, J.; Kuśnierz, C.; Kwaśnicka, A.; Koszyk, S.; Hejno, M. Comparison of healthy behavior in Ukrainian and Polish students of physical education. Phys. Act. Rev. 2021, 9, 56–64. [Google Scholar] [CrossRef]
- Cena, H.; Porri, D.; De Giuseppe, R.; Kalmpourtzidou, A.; Salvatore, F.P.; El Ghoch, M.; Itani, L.; Kreidieh, D.; Brytek-Matera, A.; Pocol, C.B.; et al. How Healthy Are Health-Related Behaviors in University Students: The HOLISTic Study. Nutrients 2021, 13, 675. [Google Scholar] [CrossRef]
- Romaguera, D.; Tauler, P.; Bennasar, M.; Pericas, J.; Moreno, C.; Martinez, S.; Aguilo, A. Determinants and patterns of physical activity practice among Spanish university students. J. Sports Sci. 2011, 29, 989–997. [Google Scholar] [CrossRef] [PubMed]
- Carballo-Fazanes, A.; Rico-Díaz, J.; Barcala-Furelos, R.; Rey, E.; Rodríguez-Fernández, J.E.; Varela-Casal, C.; Abelairas-Gómez, C. Physical Activity Habits and Determinants, Sedentary Behaviour and Lifestyle in University Students. Int. J. Environ. Res. Public Health 2020, 17, 3272. [Google Scholar] [CrossRef]
- Badicu, G. Physical Activity and Sleep Quality in Students of the Faculty of Physical Education and Sport of Braşov, Romania. Sustainability 2018, 10, 2410. [Google Scholar] [CrossRef] [Green Version]
- Dąbrowska-Galas, M.; Plinta, R.; Dąbrowska, J.; Skrzypulec-Plinta, V. Physical activity in students of the Medical University of Silesia in Poland. Phys. Ther. 2013, 93, 384–392. [Google Scholar] [CrossRef]
- Opitz, M.C.; Newman, E.; Alvarado Vázquez Mellado, A.S.; Robertson, M.D.A.; Sharpe, H. The psychometric properties of Orthorexia Nervosa assessment scales: A systematic review and reliability generalization. Appetite 2020, 155, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Barthels, F.; Meyer, F.; Pietrowsky, R. Orthorexic eating behavior: A new type of disordered eating. Ernahr. Umsch. 2015, 62, 156–161. [Google Scholar] [CrossRef]
- Cena, H.; Barthels, F.; Cuzzolaro, M.; Bratman, S.; Brytek-Matera, A.; Dunn, T.; Varga, M.; Missbach, B.; Donini, L.M. Definition and diagnostic criteria for orthorexia nervosa: A narrative review of the literature. Eat. Weight Disord. 2019, 24, 209–246. [Google Scholar] [CrossRef]
- Moroze, R.; Dunn, T.; Craig Holland, J.; Yager, J.; Weintraub, P. Microthinking about micronutrients: A case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics 2015, 56, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Setnick, J. The Eating Disorders Clinical Pocket Guide, 2nd ed.; Understanding Nutrition: Dallas, TX, USA, 2013. [Google Scholar]
- Dell’Osso, L.; Abelli, M.; Carpita, B.; Pini, S.; Castellini, G.; Carmassi, C.; Ricca, V. Historical evolution of the concept of anorexia nervosa and relationships with orthorexia nervosa, autism, and obsessive–compulsive spectrum. Neuropsychiatr. Dis. Treat. 2016, 12, 1651–1660. [Google Scholar] [CrossRef] [Green Version]
- Brytek-Matera, A. Orthorexia nervosa—An eating disorder, obsessive-compulsive disorder or disturbed eating habit? Arch. Psychiatry Psychother. 2012, 1, 55–60. [Google Scholar]
- Brytek-Matera, A.; Gramaglia, C.; Gambaro, E.; Delicato, C.; Zeppegno, P. The psychopathology of body image in orthorexia nervosa. J. Psychopathol. 2018, 24, 133–140. [Google Scholar]
- Vandereycken, W. Media hype, diagnostic fad or genuine disorder? Professionals’ opinions about night eating syndrome, orthorexia, muscle dysmorphia, and emetophobia. Eat. Disord. 2011, 19, 145–155. [Google Scholar] [CrossRef]
- Koven, N.S.; Abry, A.W. The clinical basis of orthorexia nervosa: Emerging perspectives. Neuropsychiatr. Dis. Treat. 2015, 11, 385–394. [Google Scholar] [CrossRef] [Green Version]
- Dunn, T.M.; Bratman, S. On orthorexia nervosa: A review of the literature and proposed diagnostic criteria. Eat. Behav. 2016, 21, 11–17. [Google Scholar] [CrossRef]
- Niedzielski, A.; Kaźmierczak-Wojtaś, N. Prevalence of Orthorexia Nervosa and Its Diagnostic Tools—A Literature Review. Int. J. Environ. Res. Public Health 2021, 18, 5488. [Google Scholar] [CrossRef]
- Varga, M.; Dukay-Szabó, S.; Túry, F.; van Furth, E.F. Evidence and gaps in the literature on orthorexia nervosa. Eat. Weight Disord. 2013, 18, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Strahler, J.; Hermann, A.; Walter, B.; Stark, R. Orthorexia nervosa: A behavioral complex or a psychological condition? J. Behav. Addict. 2018, 7, 1143–1156. [Google Scholar] [CrossRef] [PubMed]
- Rogowska, A.M.; Kwaśnicka, A.; Ochnik, D. Development and Validation of the Test of Orthorexia Nervosa (TON-17). J. Clin. Med. 2021, 10, 1637. [Google Scholar] [CrossRef] [PubMed]
- Brytek-Matera, A.; Onieva-Zafra, M.D.; Parra-Fernández, M.L.; Staniszewska, A.; Modrzejewska, J.; Fernández-Martínez, E. Evaluation of Orthorexia Nervosa and Symptomatology Associated with Eating Disorders among European University Students: A Multicentre Cross-Sectional Study. Nutrients 2020, 12, 3716. [Google Scholar] [CrossRef] [PubMed]
- Al-Kattan, M. The Prevalence of Orthorexia Nervosa in Lebanese University Students and the Relationship between Orthorexia Nervosa and Body Image, Body Weight and Physical Activity. Master’s Thesis, University of Chester, Chester, UK, 2016. [Google Scholar]
- Reynolds, R. Is the prevalence of orthorexia nervosa in an Australian university population 6.5%? Eat. Weight Disord. 2018, 23, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Parra-Fernández, M.L.; Onieva-Zafra, M.D.; Fernández-Martínez, E.; Abreu-Sánchez, A.; Fernández-Muñoz, J.J. Assessing the Prevalence of Orthorexia Nervosa in a Sample of University Students Using Two Different Self-Report Measures. Int. J. Environ. Res. Public Health 2019, 16, 2459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McComb, S.E.; Mills, J.S. Orthorexia nervosa: A review of psychosocial risk factors. Appetite 2019, 140, 50–75. [Google Scholar] [CrossRef]
- Strahler, J. The Dark Side of Healthy Eating: Links between Orthorexic Eating and Mental Health. Nutrients 2020, 12, 3662. [Google Scholar] [CrossRef]
- Rogowska, A.M.; Kwaśnicka, A.; Ochnik, D. Validation and Polish Adaptation of the Authorized Bratman Orthorexia Self-Test (ABOST): Comparison of Dichotomous and Continuous Likert-Type Response Scales. Psychol. Res. Behav. Manag. 2021, 14, 921–931. [Google Scholar] [CrossRef] [PubMed]
- Gawrych, M.; Cichoń, E.; Kiejna, A. COVID-19 pandemic fear, life satisfaction and mental health at the initial stage of the pandemic in the largest cities in Poland. Psychol. Health Med. 2021, 26, 107–113. [Google Scholar] [CrossRef]
- Tzur Bitan, D.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and Initial Validation. Int. J. Ment. Health Addict. 2020, 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dymecka, J.; Gerymski, R.; Machnik-Czerwik, A. Fear of COVID-19 as a buffer in the relationship between perceived stress and life satisfaction in the Polish population at the beginning of the global pandemic. Health Psychol. Rep. 2021, 9, 149–159. [Google Scholar] [CrossRef]
- Martínez-Lorca, M.; Martínez-Lorca, A.; Criado-Álvarez, J.J.; Armesilla, M.D.C.; Latorre, J.M. The fear of COVID-19 scale: Validation in spanish university students. Psychiatry Res. 2020, 293, 113350. [Google Scholar] [CrossRef]
- Morales-Rodríguez, F.M. Fear, Stress, Resilience and Coping Strategies during COVID-19 in Spanish University Students. Sustainability 2021, 13, 5824. [Google Scholar] [CrossRef]
- Beisland, E.G.; Gjeilo, K.H.; Andersen, J.R.; Bratås, O.; Bø, B.; Haraldstad, K.; Hjelmeland, I.H.H.; Iversen, M.M.; Løyland, B.; Norekvål, T.M.; et al. Quality of life and fear of COVID-19 in 2600 baccalaureate nursing students at five universities: A cross-sectional study. Health Qual. Life Outcomes 2021, 19, 198. [Google Scholar] [CrossRef]
- Montag, C.; Sindermann, C.; Rozgonjuk, D.; Yang, S.; Elhai, J.D.; Yang, H. Investigating Links between Fear of COVID-19, Neuroticism, Social Networks Use Disorder, and Smartphone Use Disorder Tendencies. Front. Psychol. 2021, 12, 682837. [Google Scholar] [CrossRef]
- Nguyen, H.T.; Do, B.N.; Pham, K.M.; Kim, G.B.; Dam, H.T.B.; Nguyen, T.T.; Nguyen, T.T.P.; Nguyen, Y.H.; Sørensen, K.; Pleasant, A.; et al. Fear of COVID-19 Scale—Associations of Its Scores with Health Literacy and Health-Related Behaviors among Medical Students. Int. J. Environ. Res. Public Health 2020, 17, 4164. [Google Scholar] [CrossRef]
- Rodríguez-Hidalgo, A.J.; Pantaleón, Y.; Dios, I.; Falla, D. Fear of COVID-19, Stress, and Anxiety in University Undergraduate Students: A Predictive Model for Depression. Front. Psychol. 2020, 11, 591797. [Google Scholar] [CrossRef]
- Yalçın, İ.; Can, N.; Mançe Çalışır, Ö.; Yalçın, S.; Çolak, B. Latent profile analysis of COVID-19 fear, depression, anxiety, stress, mindfulness, and resilience. Curr. Psychol. 2021, 31, 1–11. [Google Scholar] [CrossRef]
- Arora, A.; Jha, A.K.; Alat, P.; Das, S.S. Understanding coronaphobia. Asian J. Psychiatr. 2020, 54, 102384. [Google Scholar] [CrossRef] [PubMed]
- Rodgers, R.F.; Lombardo, C.; Cerolini, S.; Franko, D.L.; Omori, M.; Fuller-Tyszkiewicz, M.; Linardon, J.; Courtet, P.; Guillaume, S. The impact of the COVID-19 pandemic on eating disorder risk and symptoms. Int. J. Eat. Disord. 2020, 53, 1166–1170. [Google Scholar] [CrossRef] [PubMed]
- De Pasquale, C.; Sciacca, F.; Conti, D.; Pistorio, M.L.; Hichy, Z.; Cardullo, R.L.; Di Nuovo, S. Relations between Mood States and Eating Behavior during COVID-19 Pandemic in a Sample of Italian College Students. Front. Psychol. 2021, 12, 684195. [Google Scholar] [CrossRef]
- Devrim-Lanpir, A.; Güzeldere, H.K.B.; Çintesun, E.E. The COVID-19 Pandemic Drives People to Orthorexia and Anxiety with the Influence of Social Media: A Cross-Sectional Study of 525 Adults in Semi-Quarantine. BMC J. Eat. Disord. 2021, submitted. [Google Scholar] [CrossRef]
- Almeida, C.; Vieira Borba, V.; Santos, L. Orthorexia nervosa in a sample of Portuguese fitness participants. Eat. Weight Disord. 2018, 23, 443–451. [Google Scholar] [CrossRef]
- Bert, F.; Gualano, M.R.; Voglino, G.; Rossello, P.; Perret, J.P.; Siliquini, R. Orthorexia Nervosa: A cross-sectional study among athletes competing in endurance sports in Northern Italy. PLoS ONE 2019, 14, e0221399. [Google Scholar] [CrossRef]
- Clifford, T.; Blyth, C. A pilot study comparing the prevalence of orthorexia nervosa in regular students and those in University sports teams. Eat. Weight Disord. 2019, 24, 473–480. [Google Scholar] [CrossRef] [Green Version]
- Eriksson, L.; Baigi, A.; Marklund, B.; Lindgren, E.C. Social physique anxiety and sociocultural attitudes toward appearance impact on orthorexia test in fitness participants. Scand. J. Med. Sci. Sports 2008, 18, 389–394. [Google Scholar] [CrossRef] [Green Version]
- Gabriel, S. Exploring the Relationship between Physical Activity, Gender, Social Media and Orthorexia Nervosa in University Students. Bachelor’s Thesis, University of Twente, Enschede, The Netherlands, 2021. [Google Scholar]
- Håman, L.; Barker-Ruchti, N.; Patriksson, G.; Lindgren, E.C. Orthorexia nervosa: An integrative literature review of a lifestyle syndrome. Int. J. Qual. Stud. Health Well-Being 2015, 10, 26799. [Google Scholar] [CrossRef]
- He, J.; Zhao, Y.; Zhang, H.; Lin, Z. Orthorexia nervosa is associated with positive body image and life satisfaction in Chinese elderly: Evidence for a positive psychology perspective. Int. J. Eat. Disord. 2020, 54, 212–221. [Google Scholar] [CrossRef]
- Kiss-Leizer, M.; Tóth-Király, I.; Rigó, A. How the obsession to eat healthy food meets with the willingness to do sports: The motivational background of orthorexia nervosa. Eat. Weight Disord. 2019, 24, 465–472. [Google Scholar] [CrossRef] [Green Version]
- Malmborg, J.; Bremander, A.; Olsson, M.C.; Bergman, S. Health status, physical activity, and orthorexia nervosa: A comparison between exercise science students and business students. Appetite 2017, 109, 137–143. [Google Scholar] [CrossRef]
- Oberle, C.D.; Watkins, R.S.; Burkot, A.J. Orthorexic eating behaviors related to exercise addiction and internal motivations in a sample of university students. Eat. Weight Disord. 2018, 23, 67–74. [Google Scholar] [CrossRef]
- Rudolph, S. The connection between exercise addiction and orthorexia nervosa in German fitness sports. Eat. Weight Disord. 2018, 23, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Segura-García, C.; Papaianni, M.C.; Caglioti, F.; Procopio, L.; Nisticò, C.G.; Bombardiere, L.; Ammendolia, A.; Rizza, P.; De Fazio, P.; Capranica, L. Orthorexia nervosa: A frequent eating disordered behavior in athletes. Eat. Weight. Disord. 2012, 17, 226–233. [Google Scholar] [CrossRef]
- Strahler, J.; Wachten, H.; Mueller-Alcazar, A. Obsessive healthy eating and orthorexic eating tendencies in sport and exercise contexts: A systematic review and meta-analysis. J. Behav. Addict. 2021. [Google Scholar] [CrossRef] [PubMed]
- Varga, M.; Thege, B.K.; Dukay-Szabó, S.; Túry, F.; van Furth, E.F. When eating healthy is not healthy: Orthorexia nervosa and its measurement with the ORTO-15 in Hungary. BMC Psychiatry. 2014, 14, 59. [Google Scholar] [CrossRef] [Green Version]
- Yılmaz, H.; Karakuş, G.; Tamam, L.; Demirkol, M.E.; Namlı, Z.; Yeşiloğlu, C. Association of Orthorexic Tendencies with Obsessive-Compulsive Symptoms, Eating Attitudes and Exercise. Neuropsychiatr. Dis. Treat. 2020, 16, 3035–3044. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Song, J.; Brytek-Matera, A.; Zhang, H.; He, J. The Relationships between Sleep and Mental and Physical Health of Chinese Elderly: Exploring the Mediating Roles of Diet and Physical Activity. Nutrients 2021, 13, 1316. [Google Scholar] [CrossRef]
- Guo, F.; Tian, Y.; Zhong, F.; Wu, C.; Cui, Y.; Huang, C. Intensity of Physical Activity and Depressive Symptoms in College Students: Fitness Improvement Tactics in Youth (FITYou) Project. Psychol. Res. Behav. Manag. 2020, 13, 787–796. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Be Active during COVID-19. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/be-active-during-covid-19 (accessed on 5 June 2020).
- Aron, A.; Aron, E.N. Statistics for Psychology; Pearson Education: Upper Saddle River, NJ, USA, 2012. [Google Scholar]
- George, D.; Mallery, P. IBM SPSS Statistics 26 Step by Step: A Simple Guide and Reference; Routledge: New York, NY, USA, 2019. [Google Scholar]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2018. [Google Scholar]
- Cohen, J.; Cohen, P. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences; Lawrence Erlbaum: Hillsdale, NJ, USA, 1975. [Google Scholar]
- Conger, A.J. A revised definition for suppressor variables: A guide to their identification and interpretation. Educ. Psychol. Meas. 1974, 34, 35–46. [Google Scholar] [CrossRef]
- Tzelgov, J.; Henik, A. Suppression Situations in Psychological Research: Definitions, Implications, and Applications. Psychol. Bull. 1991, 109, 524–536. [Google Scholar] [CrossRef]
- Solymosi, R.; Jackson, J.; Pósch, K.; Yesberg, J.A.; Bradford, B.; Kyprianides, A. Functional and dysfunctional fear of COVID-19: A classification scheme. Crime Sci. 2021, 10, 4. [Google Scholar] [CrossRef]
- Castellini, G.; Cassioli, E.; Rossi, E.; Innocenti, M.; Gironi, V.; Sanfilippo, G.; Felciai, F.; Monteleone, A.M.; Ricca, V. The impact of COVID-19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int. J. Eat. Disord. 2020, 53, 1855–1862. [Google Scholar] [CrossRef]
- Parsons, H.; Murphy, B.; Malone, D.; Holme, I. Review of Ireland’s First Year of the COVID-19 Pandemic Impact on People Affected by Eating Disorders: ‘Behind Every Screen There Was a Family Supporting a Person with an Eating Disorder’. J. Clin. Med. 2021, 10, 3385. [Google Scholar] [CrossRef]
- Hou, W.K.; Lai, F.T.; Ben-Ezra, M.; Goodwin, R. Regularizing daily routines for mental health during and after the COVID-19 pandemic. J. Glob. Health 2020, 10, 020315. [Google Scholar] [CrossRef] [PubMed]
- Yahia, N.; Wang, D.; Rapley, M.; Dey, R. Assessment of weight status, dietary habits and beliefs, physical activity, and nutritional knowledge among university students. Perspect. Public Health 2016, 136, 231–244. [Google Scholar] [CrossRef] [PubMed]


| Demographic Variable | n | % |
|---|---|---|
| Gender | ||
| Women | 222 | 47% |
| Men | 251 | 53% |
| Relationship status | ||
| In a relationship | 281 | 59% |
| Single | 192 | 41% |
| Place of residence | ||
| Village | 232 | 49% |
| Town | 172 | 36% |
| City | 61 | 13% |
| Agglomeration | 8 | 2% |
| Department | ||
| Civil Engineering and Architecture | 61 | 13% |
| Economics and Management | 104 | 22% |
| Electrical Engineering, Automatic Control, and Informatics | 96 | 20% |
| Production Engineering and Logistics | 17 | 4% |
| Mechanical | 23 | 5% |
| Physical Education and Physiotherapy | 172 | 36% |
| Study level | ||
| First degree (Bachelor’s, three-years) | 322 | 68% |
| Second degree (Master’s, two-years) | 74 | 16% |
| Uniform Master’s study (five-years) | 74 | 16% |
| Doctoral | 3 | 1% |
| Year of study | ||
| 1 | 162 | 34% |
| 2 | 158 | 33% |
| 3 | 115 | 24% |
| 4 | 29 | 6% |
| 5 | 9 | 2% |
| Type of study | ||
| Full-time | 428 | 90% |
| Part-time | 45 | 10% |
| Variable | M | SD | Mdn | Min | Max | Skewness | Kurtosis | W | p |
|---|---|---|---|---|---|---|---|---|---|
| Fear of COVID-19 | 12.93 | 5.67 | 11.00 | 7.00 | 35.00 | 1.36 | 1.98 | 0.87 | <0.001 |
| TON-17 total score | 45.84 | 9.66 | 46.00 | 17.00 | 85.00 | −0.04 | 1.17 | 0.99 | <0.001 |
| Control of food quality | 16.34 | 4.57 | 17.00 | 6.00 | 30.00 | −0.01 | −0.07 | 0.99 | <0.001 |
| Fixation on health and healthy diet | 17.87 | 3.89 | 18.00 | 5.00 | 25.00 | −0.68 | 0.52 | 0.96 | <0.001 |
| Disorder symptoms | 11.62 | 4.67 | 11.00 | 6.00 | 30.00 | 1.23 | 1.96 | 0.90 | <0.001 |
| Men | Women | Active | Inactive | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (n = 251) | (n = 222) | (n = 222) | (n = 251) | |||||||||
| Variables | M | SD | M | SD | t (471) | d | M | SD | M | SD | t (471) | d |
| FCV-19S | 12.29 | 5.82 | 13.65 | 5.41 | 2.63 ** | 0.24 | 12.03 | 5.11 | 13.73 | 6.01 | 3.29 ** | 0.30 |
| TON-17 | 45.88 | 10.35 | 45.79 | 8.84 | −0.10 | −0.01 | 47.02 | 8.88 | 44.78 | 10.21 | −2.53 * | −0.23 |
| CFQ | 16.28 | 4.71 | 16.41 | 4.42 | 0.32 | 0.03 | 17.01 | 4.55 | 15.75 | 4.52 | −3.01 ** | −0.28 |
| FHHL | 17.53 | 4.05 | 18.26 | 3.66 | 2.06 * | 0.19 | 18.70 | 3.50 | 17.14 | 4.07 | −4.46 *** | −0.41 |
| DS | 12.07 | 5.29 | 11.11 | 3.80 | −2.24 * | −0.21 | 11.31 | 4.40 | 11.90 | 4.89 | 1.36 | 0.13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuśnierz, C.; Rogowska, A.M.; Kwaśnicka, A.; Ochnik, D. The Mediating Role of Orthorexia in the Relationship between Physical Activity and Fear of COVID-19 among University Students in Poland. J. Clin. Med. 2021, 10, 5061. https://doi.org/10.3390/jcm10215061
Kuśnierz C, Rogowska AM, Kwaśnicka A, Ochnik D. The Mediating Role of Orthorexia in the Relationship between Physical Activity and Fear of COVID-19 among University Students in Poland. Journal of Clinical Medicine. 2021; 10(21):5061. https://doi.org/10.3390/jcm10215061
Chicago/Turabian StyleKuśnierz, Cezary, Aleksandra Maria Rogowska, Aleksandra Kwaśnicka, and Dominika Ochnik. 2021. "The Mediating Role of Orthorexia in the Relationship between Physical Activity and Fear of COVID-19 among University Students in Poland" Journal of Clinical Medicine 10, no. 21: 5061. https://doi.org/10.3390/jcm10215061
APA StyleKuśnierz, C., Rogowska, A. M., Kwaśnicka, A., & Ochnik, D. (2021). The Mediating Role of Orthorexia in the Relationship between Physical Activity and Fear of COVID-19 among University Students in Poland. Journal of Clinical Medicine, 10(21), 5061. https://doi.org/10.3390/jcm10215061









