Cardiopulmonary Exercise Test Parameters in Athletic Population: A Review
Abstract
:1. Introduction
- -
- Measurement of baseline fitness and assessment of physiological function of body’s systems;
- -
- Evaluation of the integrated cardiopulmonary response in asymptomatic athletes with cardiac diseases;
- -
- Diagnosis of latent disease and/or evaluation of minor nonspecific symptoms;
- -
- Exercise prescription with specific purposes in different sports disciplines.
2. Cardiorespiratory Fitness
2.1. VO2max
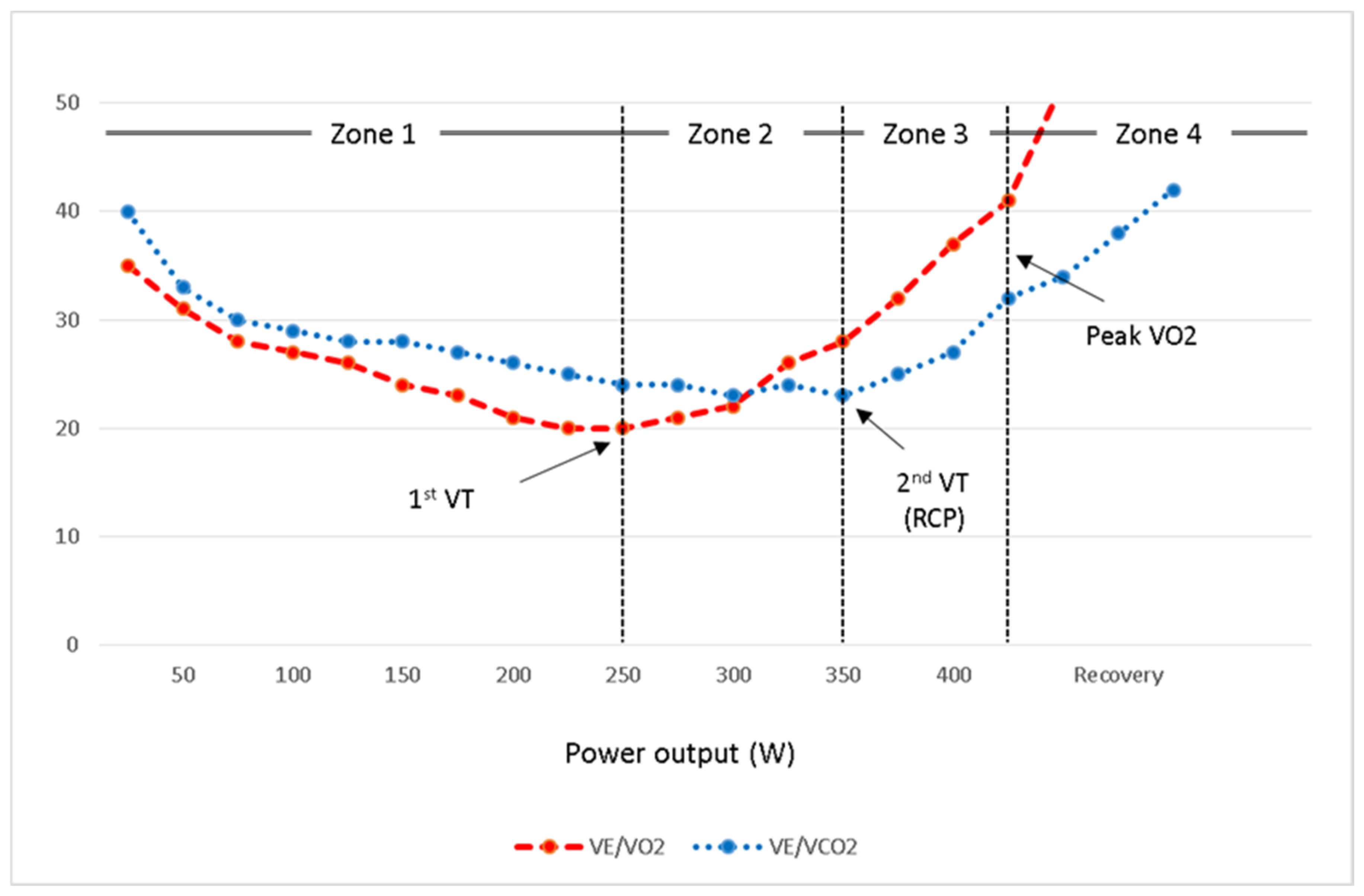
2.2. Ventilatory Threshold (VT)
3. Further Key CPET Parameters
3.1. Oxygen Pulse
3.2. Ventilatory Equivalents (VE/VO2 and VE/VCO2)
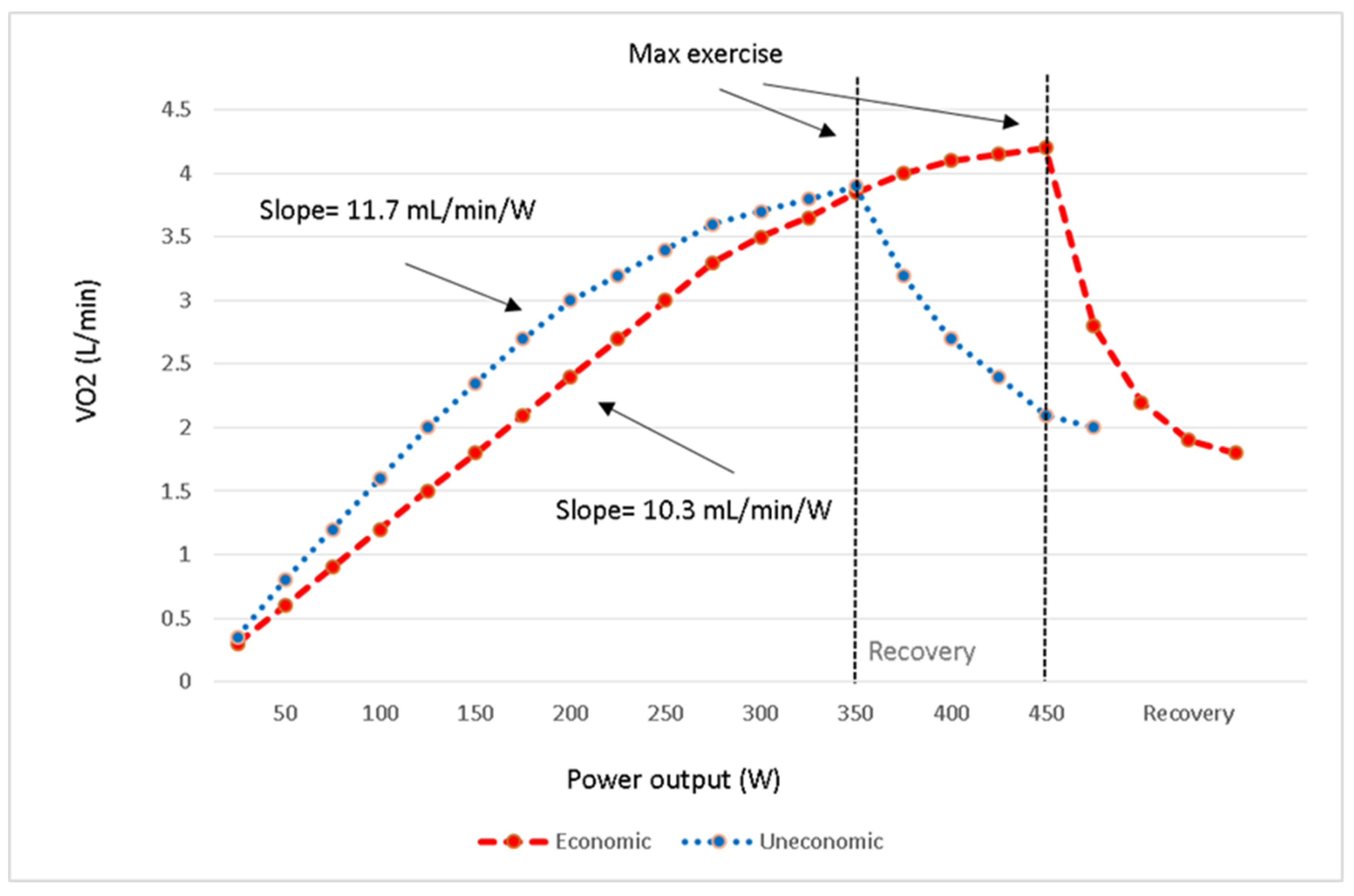
3.3. Exercise Economy (ΔVO2/ΔWorkload)
3.4. Respiratory Compensation Point (RCP)
4. Role of CPET in Diagnostic Workup
5. Exercise Prescription
6. Summary and Practical Implications
- The critical power (CP) is a beneficial parameter for the assessment of an athlete’s endurance status. However, the ventilatory threshold (VT) is a suitable parameter in CPET to set the training loads in a highly individualized manner.
- O2 pulse indicates stroke volume and peripheral vascular perfusion/extraction response to exercise. The values at different levels of exercise demonstrate central and peripheral adaptations to exercise training.
- Ventilatory equivalent for oxygen (VE/VO2) indicates the ventilatory cost for O2 and begins to increase at the VT level. The values are lower at submaximal levels of exercise in well-trained athletes.
- Exercise economy is defined as ΔVO2/Δworkload, and the lower amounts are a marker of better endurance performance in elite athletes.
- Respiratory compensation point (RCP) somewhere called the second VT is when there is an exponential increase in VE in response to an excess CO2 production during incremental exercise. Critical power and, to a lesser extent RCP, represent the high to severe intensity of exercise and are useful in setting up an exercise training program for athletes in specific sport disciplines.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guazzi, M.; Bandera, F.; Ozemek, C.; Systrom, D.; Arena, R. Cardiopulmonary exercise testing: What is its value? J. Am. Coll. Cardiol. 2017, 70, 1618–1636. [Google Scholar] [CrossRef] [PubMed]
- Sietsema, K.E.; Sue, D.Y.; Stringer, W.W.; Rossiter, H.B.; Ward, S.A. (Eds.) Exercise Testing and Interpretation. In Wasserman & Whipp’s Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Albouaini, K.; Egred, M.; Alahmar, A.; Wright, D.J. Cardiopulmonary exercise testing and its application. Postgrad. Med. J. 2007, 83, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Opondo, M.A.; Sarma, S.; Levine, B.D. The Cardiovascular Physiology of Sports and Exercise. Clin. Sports Med. 2015, 34, 391–404. [Google Scholar] [CrossRef]
- Lollgen, H.; Leyk, D. Exercise Testing in Sports Medicine. Dtsch. Aerzteblatt Online 2018, 115, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Myers, J. Applications of cardiopulmonary exercise testing in the management of cardiovascular and pulmonary disease. Int. J. Sports Med. 2004, 26, S49–S55. [Google Scholar] [CrossRef] [PubMed]
- Zinner, C.; Sperlich, B.; Wahl, P.; Mester, J. Classification of selected cardiopulmonary variables of elite athletes of different age, gender, and disciplines during incremental exercise testing. SpringerPlus 2015, 4, 544. [Google Scholar] [CrossRef] [Green Version]
- Poole, D.C.; Jones, A.M. Measurement of the maximum oxygen uptake V̇o(2max): V̇o(2peak) is no longer acceptable. J. Appl. Physiol. 2017, 122, 997–1002. [Google Scholar] [CrossRef] [PubMed]
- Dominguez, R.; Mate-Munoz, J.L.; Serra-Paya, N.; Garnacho-Castano, M.V. Lactate Threshold as a Measure of Aerobic Metabolism in Resistance Exercise. Int. J. Sports Med. 2017, 39, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Galán-Rioja, M.; González-Mohíno, F.; Poole, D.C.; González-Ravé, J.M. Relative Proximity of Critical Power and Metabolic/Ventilatory Thresholds: Systematic Review and Meta-Analysis. Sports Med. 2020, 50, 1771–1783. [Google Scholar] [CrossRef] [PubMed]
- Guazzi, M.; Adams, V.; A Conraads, V.M.; Halle, M.; Mezzani, A.; Vanhees, L.; Arena, R.; Fletcher, G.F.; Forman, D.E.; Kitzman, D.W.; et al. EACPR/AHA Joint Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur. Hear. J. 2012, 33, 2917–2927. [Google Scholar] [CrossRef]
- Sharma, S.; Merghani, A.; Mont, L. Exercise and the heart: The good, the bad, and the ugly. Eur. Hear. J. 2015, 36, 1445–1453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mezzani, A. Cardiopulmonary Exercise Testing: Basics of Methodology and Measurements. Ann. Am. Thorac. Soc. 2017, 14, S3–S11. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.G.D.S.E.; A Kaminsky, L.; Arena, R.; Christle, J.; Gil Araujo, C.; Lima, R.; A Ashley, E.; Myers, J. A reference equation for maximal aerobic power for treadmill and cycle ergometer exercise testing: Analysis from the FRIEND registry. Eur. J. Prev. Cardiol. 2018, 25, 742–750. [Google Scholar] [CrossRef]
- Balady, G.J.; Arena, R.; Sietsema, K.; Myers, J.; Coke, L.; Fletcher, G.F.; Forman, D.; Franklin, B.; Guazzi, M.; Gulati, M.; et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: A scientific statement from the American Heart Association. Circulation 2010, 122, 191–225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guazzi, M.; Arena, R.; Halle, M.; Piepoli, M.F.; Myers, J.; Lavie, C.J. 2016 focused update: Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Eur. Hear. J. 2016, 39, 1144–1161. [Google Scholar] [CrossRef]
- Sietsema, K.E. Approaches to Data Summary and Interpretation. In Wasserman & Whipp’s Principles of Exercise Testing and Interpretation: Including Pathophysiology and Clinical Applications, 6th ed.; Sietsema, K.E., Sue, D.Y., Stringer, W.W., Rossiter, H.B., Ward, S.A., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2020. [Google Scholar]
- Miyamoto-Mikami, E.; Zempo, H.; Fuku, N.; Kikuchi, N.; Miyachi, M.; Murakami, H. Heritability estimates of endurance-related phenotypes: A systematic review and meta-analysis. Scand. J. Med. Sci. Sports 2017, 28, 834–845. [Google Scholar] [CrossRef] [PubMed]
- Schutte, N.M.; Nederend, I.; Hudziak, J.J.; Bartels, M.; de Geus, E.J. Twin-sibling study and meta-analysis on the heritability of maximal oxygen consumption. Physiol. Genom. 2016, 48, 210–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, C.J.; Williams, M.G.; Eynon, N.; Ashton, K.J.; Little, J.P.; Wisloff, U.; Coombes, J.S. Genes to predict VO2max trainability: A systematic review. BMC Genom. 2017, 18, 81–110. [Google Scholar] [CrossRef]
- Sarzynski, M.A.; Ghosh, S.; Bouchard, C. Genomic and transcriptomic predictors of response levels to endurance exercise training. J. Physiol. 2016, 595, 2931–2939. [Google Scholar] [CrossRef] [PubMed]
- Poole, D.C.; Rossiter, H.B.; Brooks, G.A.; Gladden, L.B. The anaerobic threshold: 50+ years of controversy. J. Physiol. 2020, 599, 737–767. [Google Scholar] [CrossRef] [PubMed]
- Myers, J.; Arena, R.; Cahalin, L.P.; Labate, V.; Guazzi, M. Cardiopulmonary Exercise Testing in Heart Failure. Curr. Probl. Cardiol. 2015, 40, 322–372. [Google Scholar] [CrossRef]
- Jones, A.M.; Carter, H. The effect of endurance training on parameters of aerobic fitness. Sports Med. 2000, 29, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Sarma, S.; Levine, B.D. Beyond the Bruce Protocol: Advanced Exercise Testing for the Sports Cardiologist. Cardiol. Clin. 2016, 34, 603–608. [Google Scholar] [CrossRef] [PubMed]
- de Sousa, N.M.F.; Magosso, R.F.; Pereira, G.B.; Souza, M.C.; Vieira, A.; Marine, D.A.; Perez, S.A.; Baldissera, V. Acute cardiorespiratory and metabolic responses during resistance exercise in the lactate threshold intensity. Int. J. Sports Med. 2012, 33, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Mate-Munoz, J.L.; Dominguez, R.; Lougedo, J.H.; Garnacho-Castano, M.V. The lactate and ventilatory thresholds in resistance training. Clin. Physiol. Funct. Imaging 2016, 37, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Hughes, E.F.; Turner, S.C.; Brooks, G.A. Effects of glycogen depletion and pedaling speed on “anaerobic threshold”. J. Appl. Physiol. 1982, 52, 1598–1607. [Google Scholar] [CrossRef]
- Hansen, D.; Dendale, P.; Berger, J.; Meeusen, R. Low agreement of ventilatory threshold between training modes in cardiac patients. Graefe’s Arch. Clin. Exp. Ophthalmol. 2007, 101, 547–554. [Google Scholar] [CrossRef]
- Hue, O.; Le Gallais, D.; Chollet, D.; Prefaut, C. Ventilatory threshold and maximal oxygen uptake in present triathletes. Can. J. Appl. Physiol. 2000, 25, 102–113. [Google Scholar] [CrossRef] [Green Version]
- La Gerche, A.; Burns, A.T.; Taylor, A.J.; Macisaac, A.I.; Heidbuchel, H.; Prior, D.L. Maximal oxygen consumption is best predicted by measures of cardiac size rather than function in healthy adults. Graefe’s Arch. Clin. Exp. Ophthalmol. 2012, 112, 2139–2147. [Google Scholar] [CrossRef] [PubMed]
- Roca, J.; Agusti, A.G.; Alonso, A.; Poole, D.C.; Viegas, C.; Barbera, J.A.; Rodriguez-Roisin, R.; Ferrer, A.; Wagner, P.D. Effects of training on muscle O2 transport at VO2max. J. Appl. Physiol. 1992, 73, 1067–1076. [Google Scholar] [CrossRef] [PubMed]
- Riley, M.S.; Nicholls, D.P.; Cooper, C.B. Cardiopulmonary Exercise Testing and Metabolic Myopathies. Ann. Am. Thorac. Soc. 2017, 14, S129–S139. [Google Scholar] [CrossRef] [PubMed]
- Bhambhani, Y.; Singh, M. The effects of three training intensities on VO2 max and VE/VO2 ratio. Can. J. Appl. Sport Sci. J. Can. Sci. Appl. Sport 1985, 10, 44–51. [Google Scholar]
- di Paco, A.; Dube, B.P.; Laveneziana, P. Changes in Ventilatory Response to Exercise in Trained Athletes: Respiratory Physiological Benefits Beyond Cardiovascular Performance. Arch. Bronconeumol. 2017, 53, 237–244. [Google Scholar] [CrossRef]
- Salazar-Martinez, E.; de Matos, T.R.; Arrans, P.; Santalla, A.; Orellana, J.N. Ventilatory efficiency response is unaffected by fitness level, ergometer type, age or body mass index in male athletes. Biol. Sport 2018, 35, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Salazar-Martinez, E.; Santalla, A.; Orellana, J.N.; Strobl, J.; Burtscher, M.; Menz, V. Influence of high-intensity interval training on ventilatory efficiency in trained athletes. Respir. Physiol. Neurobiol. 2018, 250, 19–23. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.G.; Hansen, J.E.; Stringer, W.W. Oxygen uptake efficiency plateau: Physiology and reference values. Graefe’s Arch. Clin. Exp. Ophthalmol. 2012, 112, 919–928. [Google Scholar] [CrossRef]
- Mourot, L.; Perrey, S.; Tordi, N.; Rouillon, J.D. Evaluation of fitness level by the oxygen uptake efficiency slope after a short-term intermittent endurance training. Int. J. Sports Med. 2004, 25, 85–91. [Google Scholar] [CrossRef]
- Beattie, K.; Kenny, I.C.; Lyons, M.; Carson, B.P. The effect of strength training on performance in endurance athletes. Sports Med. 2014, 44, 845–865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barnes, K.R.; Kilding, A.E. Strategies to improve running economy. Sports Med. 2014, 45, 37–56. [Google Scholar] [CrossRef] [PubMed]
- Dolci, F.; Hart, N.H.; Kilding, A.; Chivers, P.; Piggott, B.; Spiteri, T. Movement Economy in Soccer: Current Data and Limitations. Sports 2018, 6, 124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mezzani, A.; Hamm, L.F.; Jones, A.M.; E McBride, P.; Moholdt, T.; A Stone, J.; Urhausen, A.; A Williams, M. Aerobic exercise intensity assessment and prescription in cardiac rehabilitation: A joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation and the Canadian Association of Cardiac Rehabilitation. Eur. J. Prev. Cardiol. 2013, 20, 442–467. [Google Scholar] [CrossRef]
- Binder, R.K.; Wonisch, M.; Corra, U.; Cohen-Solal, A.; Vanhees, L.; Saner, H.; Schmid, J.-P. Methodological approach to the first and second lactate threshold in incremental cardiopulmonary exercise testing. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 726–734. [Google Scholar] [CrossRef]
- Palermo, P.; Corra, U. Exercise Prescriptions for Training and Rehabilitation in Patients with Heart and Lung Disease. Ann. Am. Thorac. Soc. 2017, 14, S59–S66. [Google Scholar] [CrossRef] [PubMed]
- Bussotti, M.; Di Marco, S.; Marchese, G. Respiratory disorders in endurance athletes—how much do they really have to endure? Open Access J. Sports Med. 2014, 5, 47–63. [Google Scholar] [CrossRef] [Green Version]
- Stickland, M.K.; Butcher, S.J.; Marciniuk, D.D.; Bhutani, M. Assessing exercise limitation using cardiopulmonary exercise testing. Pulm. Med. 2012, 2012, 1–13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwellnus, M.; Soligard, T.; Alonso, J.-M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.J.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How much is too much? (Part 2) International Olympic Committee consensus statement on load in sport and risk of illness. Br. J. Sports Med. 2016, 50, 1043–1052. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carfagno, D.G.; Hendrix, J.C., 3rd. Overtraining syndrome in the athlete: Current clinical practice. Curr. Sports Med. Rep. 2014, 13, 45–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kreher, J.B.; Schwartz, J.B. Overtraining syndrome: A practical guide. Sports Health 2012, 4, 128–138. [Google Scholar] [CrossRef] [Green Version]
- Le Meur, Y.; Hausswirth, C.; Natta, F.; Couturier, A.; Bignet, F.; Vidal, P.P. A multidisciplinary approach to overreaching detection in endurance trained athletes. J. Appl. Physiol. 2013, 114, 411–420. [Google Scholar] [CrossRef] [PubMed]
- Le Meur, Y.; Louis, J.; Aubry, A.; Guéneron, J.; Pichon, A.; Schaal, K.; Corcuff, J.-B.; Hatem, S.; Isnard, R.; Hausswirth, C. Maximal exercise limitation in functionally overreached triathletes: Role of cardiac adrenergic stimulation. J. Appl. Physiol. 2014, 117, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Laursen, P.B. High-intensity interval training, solutions to the programming puzzle: Part I: Cardiopulmonary emphasis. Sports Med. 2013, 43, 313–338. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Laursen, P.B. High-intensity interval training, solutions to the programming puzzle. Part II: Anaerobic energy, neuromuscular load and practical applications. Sports Med. 2013, 43, 927–954. [Google Scholar] [CrossRef] [PubMed]

| Intensity of Exercise (% VO2max) | |||
|---|---|---|---|
| 50% | 75% | 100% | |
| Reference athlete O2 pulse (mL/beat) | 14 | 18 | 20 |
| Athlete A | ↑ | ↑ | ↑ |
| Athlete B | ↑ | ↑↔ | ↓ |
| Athlete C | ↓ | ↓↔ | ↔↑ |
| Athlete D | ↓ | ↓ | ↓ |
| An Elite Athlete Compare to an Ordinary Peer | |
|---|---|
| VO2 max (mL/kg/min) | ↑↑ |
| VO2 at VT | ↑↑ |
| Watts at VT | ↑↑ |
| O2 pulse/BSA | ↑ |
| VE/VO2 at VT | ↓ |
| VE/VCO2 slope | ↔ |
| PETCO2 | ↔ |
| OUES | ↔ |
| ΔVO2/Δworkload | ↔↓ |
| VO2 at RCP | ↑↑ |
| Watts at RCP | ↑↑ |
| Exercise duration at RCP level | ↑↑ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazaheri, R.; Schmied, C.; Niederseer, D.; Guazzi, M. Cardiopulmonary Exercise Test Parameters in Athletic Population: A Review. J. Clin. Med. 2021, 10, 5073. https://doi.org/10.3390/jcm10215073
Mazaheri R, Schmied C, Niederseer D, Guazzi M. Cardiopulmonary Exercise Test Parameters in Athletic Population: A Review. Journal of Clinical Medicine. 2021; 10(21):5073. https://doi.org/10.3390/jcm10215073
Chicago/Turabian StyleMazaheri, Reza, Christian Schmied, David Niederseer, and Marco Guazzi. 2021. "Cardiopulmonary Exercise Test Parameters in Athletic Population: A Review" Journal of Clinical Medicine 10, no. 21: 5073. https://doi.org/10.3390/jcm10215073
APA StyleMazaheri, R., Schmied, C., Niederseer, D., & Guazzi, M. (2021). Cardiopulmonary Exercise Test Parameters in Athletic Population: A Review. Journal of Clinical Medicine, 10(21), 5073. https://doi.org/10.3390/jcm10215073







