Temporal Relationship between Atrial Fibrillation and Heart Failure Development Analysis from a Nationwide Database
Abstract
:1. Introduction
2. Methods
2.1. Study Design
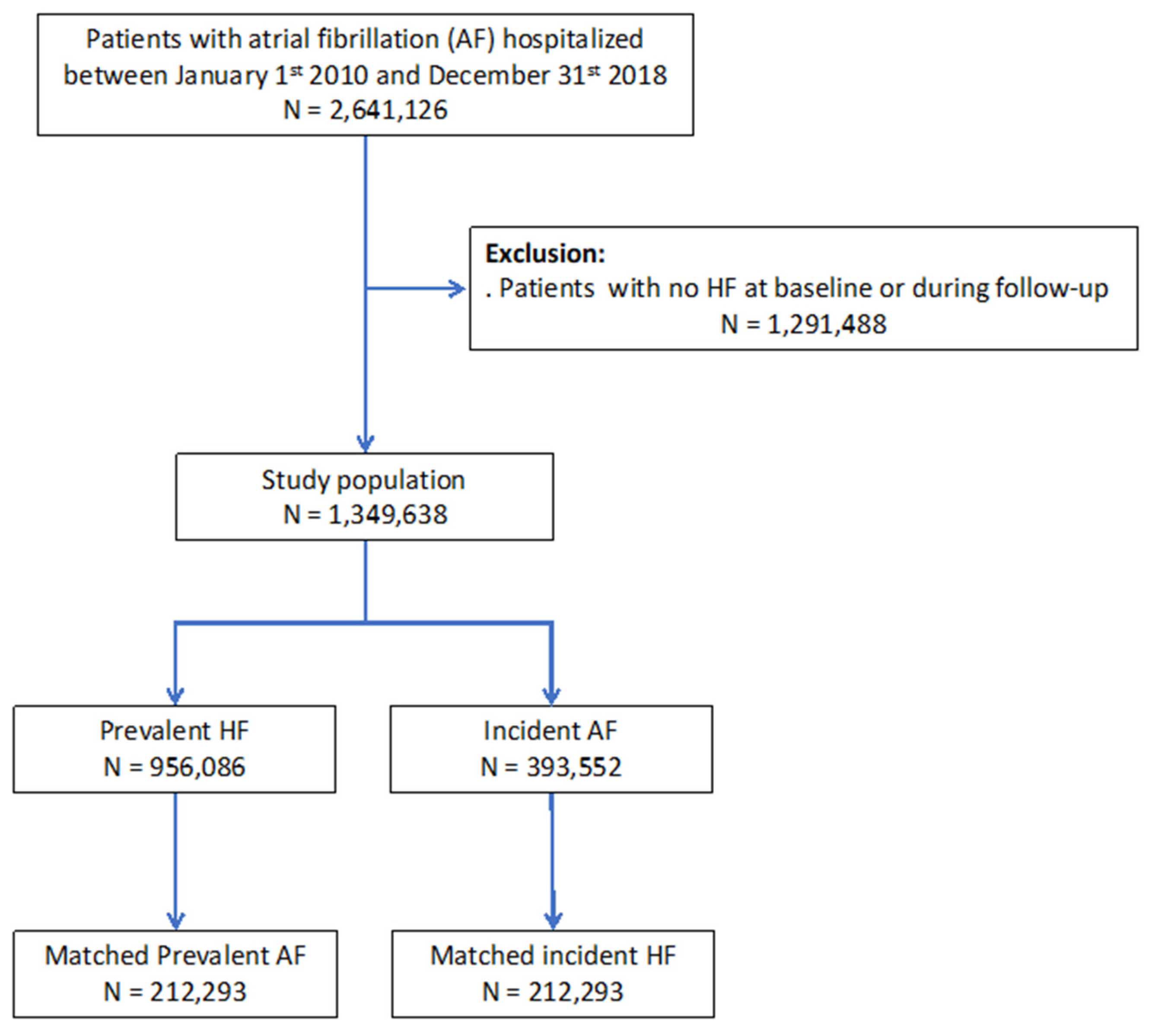
2.2. Study Population
2.3. Outcomes
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Clinical Outcomes in the Unmatched Cohort
3.3. Clinical Outcomes in the Matched Cohort
3.4. Outcomes in Patients with (1) Prevalent HF, (2) AF and HF Diagnosed during the Same Hospitalization or (3) Incident HF
4. Discussion
4.1. Study Population with AF and HF
4.2. Temporality between Onset of Atrial Fibrillation and Heart Failure
4.3. All-Cause Death and Cardiovascular Death
4.4. Higher Incidence of Ischemic Stroke in Patients Hospitalized with “Incident HF”
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kotecha, D.; Piccini, J.P. Atrial fibrillation in heart failure: What should we do? Eur. Heart J. 2015, 36, 3250–3257. [Google Scholar] [CrossRef] [Green Version]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart disease and stroke statistics-2020 update: A report from the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.-A.; Dilaveris, P.E.; et al. ESC Scientific Document Group. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Pokorney, S.D.; Piccini, J.P.; Stevens, S.R.; Patel, M.R.; Pieper, K.S.; Halperin, J.L.; Breithardt, G.; Singer, D.E.; Hankey, G.J.; Hacke, W.; et al. Cause of death and predictors of all-cause mortality in anticoagulated patients with nonvalvular atrial fibrillation: Data from ROCKET AF. J. Am. Heart Assoc. 2016, 5, e002197. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fauchier, L.; Villejoubert, O.; Clementy, N.; Bernard, A.; Pierre, B.; Angoulvant, D.; Ivanes, F.; Babuty, D.; Lip, G.Y.H. Causes of death and influencing factors in patients with atrial fibrillation. Am. J. Med. 2016, 129, 1278–1287. [Google Scholar] [CrossRef]
- Smit, M.D.; Moes, M.L.; Maass, A.H.; Achekar, I.D.; Van Geel, P.P.; Hillege, H.L.; Veldhuisen, D.J.; Van Gelder, I.C. The importance of whether atrial fibrillation or heart failure develops first. Eur. J. Heart Fail. 2012, 14, 1030–1040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dries, D.L.; Exner, D.V.; Gersh, B.J.; Domanski, M.J.; Waclawiw, M.A.; Stevenson, L.W. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: A retrospective analysis of the SOLVD trials. Studies of Left Ventricular Dysfunction. J. Am. Coll. Cardiol. 1998, 32, 695–703. [Google Scholar] [CrossRef] [Green Version]
- Chamberlain, A.M.; Gersh, B.J.; Alonso, A.; Kopecky, S.L.; Killian, J.M.; Weston, S.A.; Roger, V.L. No decline in the risk of heart failure after incident atrial fibrillation: A community study assessing trends overall and by ejection fraction. Heart Rhythm. 2017, 14, 791–798. [Google Scholar] [CrossRef]
- Chamberlain, A.M.; Redfield, M.M.; Alonso, A.; Weston, S.A.; Roger, V.L. Atrial fibrillation and mortality in heart failure: A community study. Circ. Heart Fail. 2011, 4, 740–746. [Google Scholar] [CrossRef] [Green Version]
- Nieuwlaat, R.; Eurlings, L.W.; Cleland, J.G.; Cobbe, S.M.; Vardas, P.E.; Capucci, A.; López-Sendòn, J.L.; Meeder, J.G.; Pinto, Y.M.; Crijns, H.J.G.M. Atrial fibrillation and heart failure in cardiology practice: Reciprocal impact and combined management from the perspective of atrial fibrillation: Results of the Euro Heart Survey on atrial fibrillation. J. Am. Coll. Cardiol. 2009, 53, 1690–1698. [Google Scholar] [CrossRef] [Green Version]
- Cha, Y.-M.; Redfield, M.M.; Shen, W.-K.; Gersh, B.J. Atrial fibrillation and ventricular dysfunction: A vicious electromechanical cycle. Circulation 2004, 109, 2839–2843. [Google Scholar] [CrossRef] [Green Version]
- Staerk, L.; Wang, B.; Preis, S.R.; Larson, M.G.; Lubitz, S.A.; Ellinor, P.T.; McManus, D.D.; Ko, D.; Weng, L.-C.; Lunetta, K.L.; et al. Lifetime risk of atrial fibrillation according to optimal, borderline, or elevated levels of risk factors: Cohort study based on longitudinal data from the Framingham Heart Study. BMJ 2018, 361, k1453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chantry, A.A.; Deneux-Tharaux, C.; Cans, C.; Ego, A.; Quantin, C.; Bouvier-Colle, M.-H.; GRACE study group. Hospital discharge data can be used for monitoring procedures and intensive care related to severe maternal morbidity. J. Clin. Epidemiol. 2011, 64, 1014–1022. [Google Scholar] [CrossRef] [Green Version]
- Djennaoui, M.; Ficheur, G.; Beuscart, R.; Chazard, E. Improvement of the quality of medical databases: Data-mining-based prediction of diagnostic codes from previous patient codes. Stud. Health Technol. Inform. 2015, 210, 419–423. [Google Scholar] [PubMed]
- Fauchier, L.; Clementy, N.; Pelade, C.; Collignon, C.; Nicolle, E.; Lip, G.Y.H. Patients with ischemic stroke and incident atrial fibrillation: A Nationwide Cohort Study. Stroke 2015, 46, 2432–2437. [Google Scholar] [CrossRef] [Green Version]
- Bezin, J.; Pariente, A.; Lassalle, R.; Dureau-Pournin, C.; Abouelfath, A.; Robinson, P.; Moore, N.; Droz-Perroteau, C.; Fourrier-Reglat, A. Use of the recommended drug combination for secondary prevention after a first occurrence of acute coronary syndrome in France. Eur. J. Clin. Pharmacol. 2014, 70, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Massoullié, G.; Wintzer-Wehekind, J.; Chenaf, C.; Mulliez, A.; Pereira, B.; Authier, N.; Eschalier, A.; Clerfond, G.; Souteyrand, G.; Tabassome, S.; et al. Prognosis and management of myocardial infarction: Comparisons between the French FAST-MI 2010 registry and the French public health database. Arch. Cardiovasc. Dis. 2016, 109, 303–310. [Google Scholar] [CrossRef]
- Eschalier, R.; Chenaf, C.; Mulliez, A.; Yalioua, A.; Clerfond, G.; Authier, N.; Vorilhon, C.; Citron, B.; Pereira, B.; Jean, F.; et al. Impact of clinical characteristics and management on the prognosis of unselected heart failure patients. Cardiovasc. Drugs Ther. 2015, 29, 89–98. [Google Scholar] [CrossRef]
- Fauchier, L.; Bodin, A.; Bisson, A.; Herbert, J.; Spiesser, P.; Clementy, N.; Babuty, D.; Chao, T.-F.; Lip, G.Y.H. Incident comorbidities, aging and the risk of stroke in 608,108 patients with atrial fibrillation: A Nationwide Analysis. J. Clin. Med. 2020, 9, 1234. [Google Scholar] [CrossRef]
- Shelton, R.J.; Clark, A.L.; Kaye, G.C.; Cleland, J.G.F. The atrial fibrillation paradox of heart failure. Congest Heart Fail. 2010, 16, 3–9. [Google Scholar] [CrossRef]
- Potpara, T.S.; Stankovic, G.R.; Beleslin, B.D.; Polovina, M.M.; Marinkovic, J.M.; Ostojic, M.C.; Lip, G.Y.H. A 12-year follow-up study of patients with newly diagnosed lone atrial fibrillation: Implications of arrhythmia progression on prognosis: The Belgrade Atrial Fibrillation study. Chest 2012, 141, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Santhanakrishnan, R.; Wang, N.; Larson, M.G.; Magnani, J.W.; McManus, D.D.; Lubitz, S.A.; Ellinor, P.T.; Cheng, S.; Vasan, R.S.; Lee, D.S. Atrial fibrillation begets heart failure and vice versa: Temporal associations and differences in preserved versus reduced ejection fraction. Circulation 2016, 133, 484–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McManus, D.D.; Hsu, G.; Sung, S.H.; Saczynski, J.S.; Smith, D.H.; Magid, D.J.; Gurwitz, J.H.; Goldberg, R.J.; Go, A.S. Cardiovascular Research Network PRESERVE Study. Atrial fibrillation and outcomes in heart failure with preserved versus reduced left ventricular ejection fraction. J. Am. Heart Assoc. 2013, 2, e005694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotecha, D.; Lam, C.S.P.; Van Veldhuisen, D.J.; Van Gelder, I.C.; Voors, A.A.; Rienstra, M. Heart failure with preserved ejection fraction and atrial fibrillation: Vicious Twins. J. Am. Coll. Cardiol. 2016, 68, 2217–2228. [Google Scholar] [CrossRef]
- Kotecha, D.; Chudasama, R.; Lane, D.A.; Kirchhof, P.; Lip, G.Y.H. Atrial fibrillation and heart failure due to reduced versus preserved ejection fraction: A systematic review and meta-analysis of death and adverse outcomes. Int. J. Cardiol. 2016, 203, 660–666. [Google Scholar] [CrossRef]
- Zafrir, B.; Lund, L.H.; Laroche, C.; Ruschitzka, F.; Crespo-Leiro, M.G.; Coats, A.J.S.; Anker, S.D.; Filippatos, G.; Seferovic, P.M.; Maggioni, A.P.; et al. Prognostic implications of atrial fibrillation in heart failure with reduced, mid-range, and preserved ejection fraction: A report from 14 964 patients in the European Society of Cardiology Heart Failure Long-Term Registry. Eur. Heart J. 2018, 39, 4277–4284. [Google Scholar] [CrossRef] [Green Version]





| Prevalent HF | Incident HF | Standardized Difference, Prevalent HF vs. Incident HF | Total | |
|---|---|---|---|---|
| (n = 956,086) | (n = 393,552) | (%) | (n = 1,349,638) | |
| Age, years | 79.4 ± 11.2 | 80.7 ± 10.2 | −11.8 | 79.8 ± 10.9 |
| Sex (male) | 506,100 (52.9) | 204,887 (52.1) | −20.2 | 710,987 (52.7) |
| CHA2DS2-VASc score | 4.4 ± 1.4 | 4.7 ± 1.3 | −25.1 | 4.5 ± 1.4 |
| HASBLED score | 1.9 ± 0.8 | 2.1 ± 0.8 | 1.7 | 1.9 ± 0.8 |
| Hypertension | 651,087 (68.1) | 307,749 (78.2) | −22.9 | 958,836 (71.0) |
| Diabetes mellitus | 255,132 (26.7) | 106,430 (27.0) | −0.8 | 361,562 (26.8) |
| Smoker | 75,809 (7.9) | 29,387 (7.5) | 1.7 | 105,196 (7.8) |
| Dyslipidemia | 255,314 (26.7) | 118,970 (30.2) | −7.8 | 374,284 (27.7) |
| Obesity | 173,860 (18.2) | 80,859 (20.5) | −6.0 | 254,719 (18.9) |
| History of pulmonary edema | 65,725 (6.9) | 17,064 (4.3) | 11.1 | 82,789 (6.1) |
| Dilated cardiomyopathy | 184,186 (19.3) | 42,456 (10.8) | 23.9 | 226,642 (16.8) |
| Coronary artery disease | 406,323 (42.5) | 152,115 (38.7) | 7.8 | 558,438 (41.4) |
| Previous myocardial infarction | 146,515 (15.3) | 50,590 (12.9) | 7.1 | 197,105 (14.6) |
| Previous PCI | 72,223 (7.6) | 28,619 (7.3) | 1.1 | 100,842 (7.5) |
| Previous CABG | 60,510 (6.3) | 21,370 (5.4) | 3.8 | 81,880 (6.1) |
| Mitral regurgitation | 101,891 (10.7) | 40,145 (10.2) | 1.5 | 142,036 (10.5) |
| Aortic regurgitation | 38,757 (4.1) | 16,438 (4.2) | −0.6 | 55,195 (4.1) |
| Aortic stenosis | 100,671 (10.5) | 41,234 (10.5) | 0.2 | 141,905 (10.5) |
| Vascular disease | 256,016 (26.8) | 107,795 (27.4) | −1.4 | 363,811 (27.0) |
| Pacemaker or ICD | 97,026 (10.1) | 55,890 (14.2) | −12.4 | 152,916 (11.3) |
| ICD | 12,705 (1.3) | 1259 (0.3) | 11.2 | 13,964 (1.0) |
| CRT | 6864 (0.7) | 661 (0.2) | 8.3 | 7525 (0.6) |
| Ischemic stroke | 54,539 (5.7) | 37,338 (9.5) | −14.3 | 91,877 (6.8) |
| Alcohol related diagnoses | 57,453 (6.0) | 24,196 (6.1) | −0.6 | 81,649 (6.0) |
| Abnormal renal function | 111,350 (11.6) | 52,274 (13.3) | −5.0 | 163,624 (12.1) |
| Lung disease | 222,083 (23.2) | 101,327 (25.7) | −5.9 | 323,410 (24.0) |
| Sleep apnea syndrome | 64,487 (6.7) | 32,811 (8.3) | −6.0 | 97,298 (7.2) |
| COPD | 132,935 (13.9) | 59,555 (15.1) | −3.5 | 192,490 (14.3) |
| Liver disease | 47,817 (5.0) | 21,837 (5.5) | −2.4 | 69,654 (5.2) |
| Thyroid diseases | 105,783 (11.1) | 64,707 (16.4) | −15.7 | 170,490 (12.6) |
| Inflammatory disease | 71,214 (7.4) | 39,076 (9.9) | −8.8 | 110,290 (8.2) |
| Anemia | 184,967 (19.3) | 103,148 (26.2) | −16.4 | 288,115 (21.3) |
| Previous cancer | 151,136 (15.8) | 84,819 (21.6) | −14.8 | 235,955 (17.5) |
| Poor nutrition | 109,402 (11.4) | 65,127 (16.5) | −14.8 | 174,529 (12.9) |
| Cognitive impairment | 117,339 (12.3) | 69,280 (17.6) | −15.0 | 186,619 (13.8) |
| Prevalent HF | Incident HF | |
|---|---|---|
| (n = 9352) | (n = 4248) | |
| ACE inhibitor or ARB | 4142 (44.3%) | 1635 (38.5%) |
| Beta-blocker | 4577 (48.9%) | 1998 (47.0%) |
| Diuretic | 5384 (57.6%) | 2371 (55.8%) |
| K-sparing diuretics | 1039 (11.1%) | 375 (8.8%) |
| Calcium channel blocker | 1497 (16.0%) | 764 (18.0%) |
| Digoxin | 795 (8.5%) | 378 (8.9%) |
| Anti-arrhythmic agents | 2631 (28.1%) | 994 (23.4%) |
| Amiodarone | 2494 (26.7%) | 907 (21.4%) |
| VKA | 3362 (35.9%) | 1596 (37.6%) |
| Direct oral anti-coagulant | 1532 (16.4%) | 740 (17.4%) |
| Dabigatran | 242 (2.6%) | 124 (2.9%) |
| Rivaroxaban | 617 (6.6%) | 321 (7.6%) |
| Apixaban | 691 (7.4%) | 310 (7.3%) |
| Aspirin | 2462 (26.3%) | 919 (21.6%) |
| P2Y12 inhibitor | 801 (8.6%) | 279 (6.6%) |
| Statin | 2898 (31.0%) | 1121 (26.4%) |
| Antidiabetic | 1677 (17.9%) | 757 (17.8%) |
| Prevalent HF | Incident HF | Standardized Difference, Prevalent HF vs. Incident HF | |
|---|---|---|---|
| (n = 212,293) | (n = 212,293) | (n = 212,293) | |
| Age, years | 81.5 ± 9.8 | 81.4 ± 10.0 | −1.1 |
| Sex (male) | 101,838 (48.0) | 102,423 (48.2) | 0.9 |
| CHA2DS2-VASc score | 4.5 ± 1.2 | 4.5 ± 1.3 | 0.3 |
| HASBLED score | 1.9 ± 0.7 | 1.9 ± 0.7 | 0.6 |
| Hypertension | 159,619 (75.2) | 160,555 (75.6) | 1.0 |
| Diabetes mellitus | 45,788 (21.6) | 47,155 (22.2) | 1.5 |
| Smoker | 8091 (3.8) | 8926 (4.2) | 1.5 |
| Dyslipidemia | 48,405 (22.8) | 50,225 (23.7) | 1.9 |
| Obesity | 30,053 (14.2) | 30,939 (14.6) | 1.1 |
| History of pulmonary edema | 5751 (2.7) | 6750 (3.2) | 2.0 |
| Dilated cardiomyopathy | 21,158 (10.0) | 22,755 (10.7) | 2.1 |
| Coronary artery disease | 70,625 (33.3) | 72,363 (34.1) | 1.7 |
| Previous myocardial infarction | 22,837 (10.8) | 24,018 (11.3) | 1.6 |
| Previous PCI | 11,389 (5.4) | 12,098 (5.7) | 1.3 |
| Previous CABG | 7865 (3.7) | 8183 (3.9) | 0.6 |
| Mitral regurgitation | 14,108 (6.6) | 14,734 (6.9) | 1.0 |
| Aortic regurgitation | 4493 (2.1) | 4811 (2.3) | 0.8 |
| Aortic stenosis | 14,791 (7.0) | 15,659 (7.4) | 1.3 |
| Vascular disease | 41,500 (19.5) | 43,398 (20.4) | 2.0 |
| Pacemaker or ICD | 18,855 (8.9) | 19,279 (9.1) | 0.6 |
| ICD | 282 (0.1) | 308 (0.1) | 0.1 |
| CRT | 129 (0.1) | 142 (0.1) | 0.1 |
| Ischemic stroke | 11,027 (5.2) | 11,630 (5.5) | 1.1 |
| Alcohol related diagnoses | 6062 (2.9) | 6738 (3.2) | 1.3 |
| Abnormal renal function | 17,156 (8.1) | 18,138 (8.5) | 1.4 |
| Lung disease | 39,514 (18.6) | 40,366 (19.0) | 0.9 |
| Sleep apnea syndrome | 9262 (4.4) | 9878 (4.7) | 1.1 |
| COPD | 23,494 (11.1) | 23,993 (11.3) | 0.7 |
| Liver disease | 5139 (2.4) | 5682 (2.7) | 1.1 |
| Thyroid diseases | 23,649 (11.1) | 23,923 (11.3) | 0.4 |
| Inflammatory disease | 11,570 (5.5) | 11,901 (5.6) | 0.6 |
| Anemia | 38,038 (17.9) | 39,034 (18.4) | 1.1 |
| Previous cancer | 33,252 (15.7) | 34,512 (16.3) | 1.5 |
| Poor nutrition | 23,329 (11.0) | 24,008 (11.3) | 0.9 |
| Cognitive impairment | 29,406 (13.9) | 28,925 (13.6) | −0.6 |
| Prevalent HF (n = 956,086) | Incident HF (n = 393,552) | HR (95% CI) for Prevalent HF vs. Incident HF | p (Uncorrected) | p (Bonferroni Correction) | |
|---|---|---|---|---|---|
| All-cause death | 316,729 (19.0) | 126,688 (21.8) | 0.91 (0.91–0.92) | <0.0001 | <0.0001 |
| Cardiovascular death | 117,294 (7.1) | 41,431 (7.1) | 1.04 (1.03–1.06) * | <0.0001 | <0.0001 |
| Non-cardiovascular death | 199,435 (12.0) | 85,257 (14.7) | 0.85 (0.84–0.86) | <0.0001 | <0.0001 |
| Ischemic stroke | 40,670 (2.5) | 14,266 (2.6) | 0.97 (0.95–0.99) † | 0.006 | 0.02 |
| Re-hospitalization for HF | 254,885 (19.3) | 45,877 (13.8) | 1.43 (1.42–1.45) | <0.0001 | <0.0001 |
| Cancer | 73,528 (4.7) | 25,214 (4.9) | 0.96 (0.94–0.97) | <0.0001 | <0.0001 |
| Prevalent HF (n = 212,293) | Incident HF (n = 212,293) | HR (95% CI) for Prevalent HF vs. Incident HF | p (Uncorrected) | p (Bonferroni Correction) | |
|---|---|---|---|---|---|
| All-cause death | 68,150 (21.6) | 64,643 (19.3) | 1.10 (1.08–1.11) | <0.0001 | <0.0001 |
| Cardiovascular death | 24,156 (7.7) | 21,874 (6.5) | 1.14 (1.12–1.16) * | <0.0001 | <0.0001 |
| Non-cardiovascular death | 43,994 (14.0) | 42,769 (12.8) | 1.07 (1.06–1.09) | <0.0001 | <0.0001 |
| Ischemic stroke | 3775 (1.2) | 7824 (2.4) | 0.50 (0.48–0.52) † | <0.0001 | <0.0001 |
| Re-hospitalization for HF | 49,763 (19.4) | 24,785 (13.2) | 1.44 (1.41–1.46) | <0.0001 | <0.0001 |
| Cancer | 14,558 (4.9) | 15,176 (5.0) | 0.97 (0.95–0.99) | 0.005 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cottin, Y.; Maalem Ben Messaoud, B.; Monin, A.; Guilleminot, P.; Bisson, A.; Eicher, J.-C.; Bodin, A.; Herbert, J.; Juillière, Y.; Zeller, M.; et al. Temporal Relationship between Atrial Fibrillation and Heart Failure Development Analysis from a Nationwide Database. J. Clin. Med. 2021, 10, 5101. https://doi.org/10.3390/jcm10215101
Cottin Y, Maalem Ben Messaoud B, Monin A, Guilleminot P, Bisson A, Eicher J-C, Bodin A, Herbert J, Juillière Y, Zeller M, et al. Temporal Relationship between Atrial Fibrillation and Heart Failure Development Analysis from a Nationwide Database. Journal of Clinical Medicine. 2021; 10(21):5101. https://doi.org/10.3390/jcm10215101
Chicago/Turabian StyleCottin, Yves, Brahim Maalem Ben Messaoud, Antoine Monin, Pierre Guilleminot, Arnaud Bisson, Jean-Christophe Eicher, Alexandre Bodin, Julien Herbert, Yves Juillière, Marianne Zeller, and et al. 2021. "Temporal Relationship between Atrial Fibrillation and Heart Failure Development Analysis from a Nationwide Database" Journal of Clinical Medicine 10, no. 21: 5101. https://doi.org/10.3390/jcm10215101
APA StyleCottin, Y., Maalem Ben Messaoud, B., Monin, A., Guilleminot, P., Bisson, A., Eicher, J.-C., Bodin, A., Herbert, J., Juillière, Y., Zeller, M., & Fauchier, L. (2021). Temporal Relationship between Atrial Fibrillation and Heart Failure Development Analysis from a Nationwide Database. Journal of Clinical Medicine, 10(21), 5101. https://doi.org/10.3390/jcm10215101






