Incidence of Mortality, Acute Kidney Injury and Graft Loss in Adult Kidney Transplant Recipients with Coronavirus Disease 2019: Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Study Eligibility Criteria
2.3. Data Extraction and Outcome
2.4. Data Synthesis and Analysis
2.5. Risk of Bias Assessment
3. Results
3.1. Study Characteristics
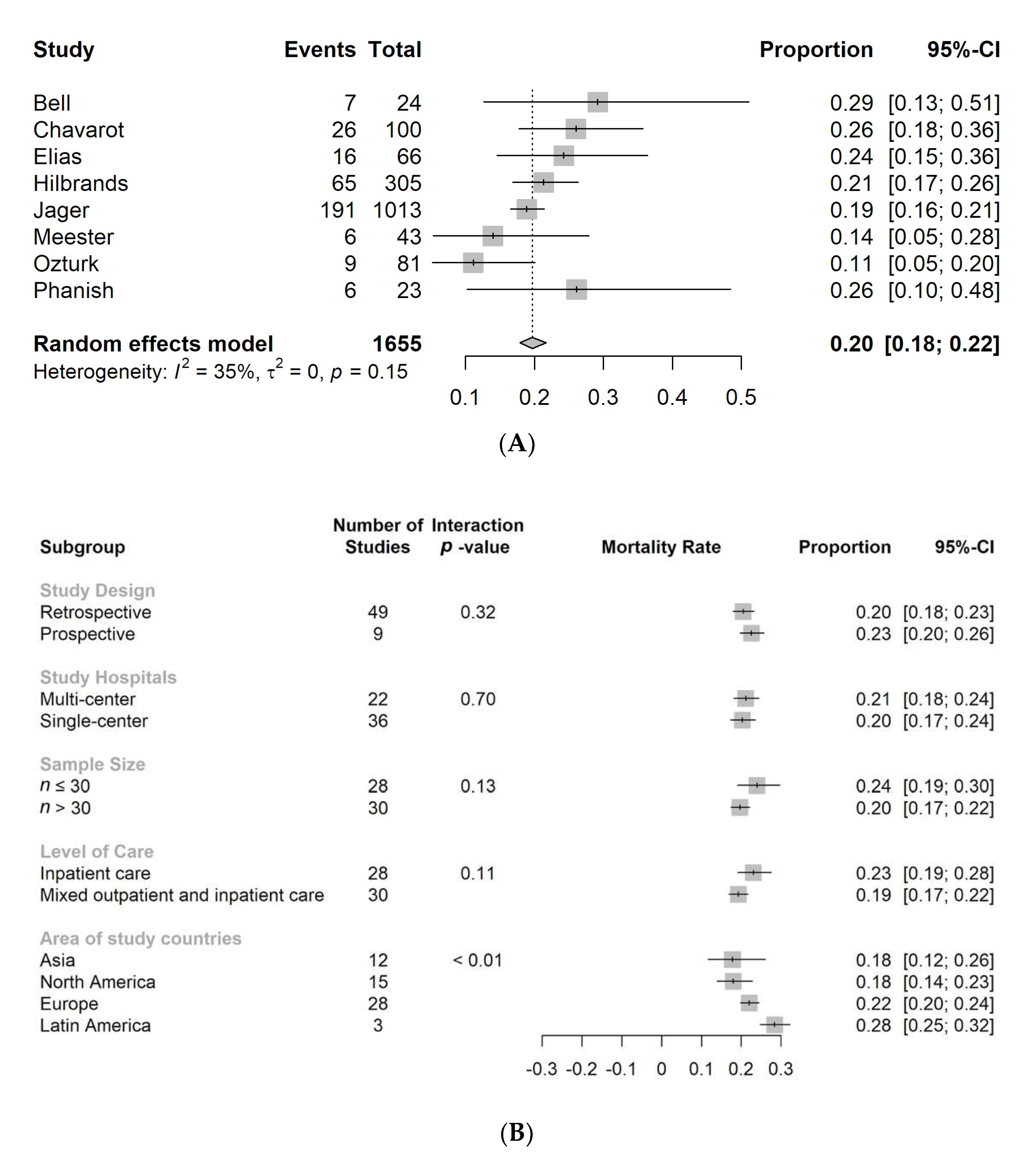
3.2. Mortality of Adult Transplant Population with COVID-19 Infection
3.3. Secondary Outcomes of Adult Transplant Population with COVID-19 Infection
3.4. Publication and Risk of Bias of Enrolled Studies
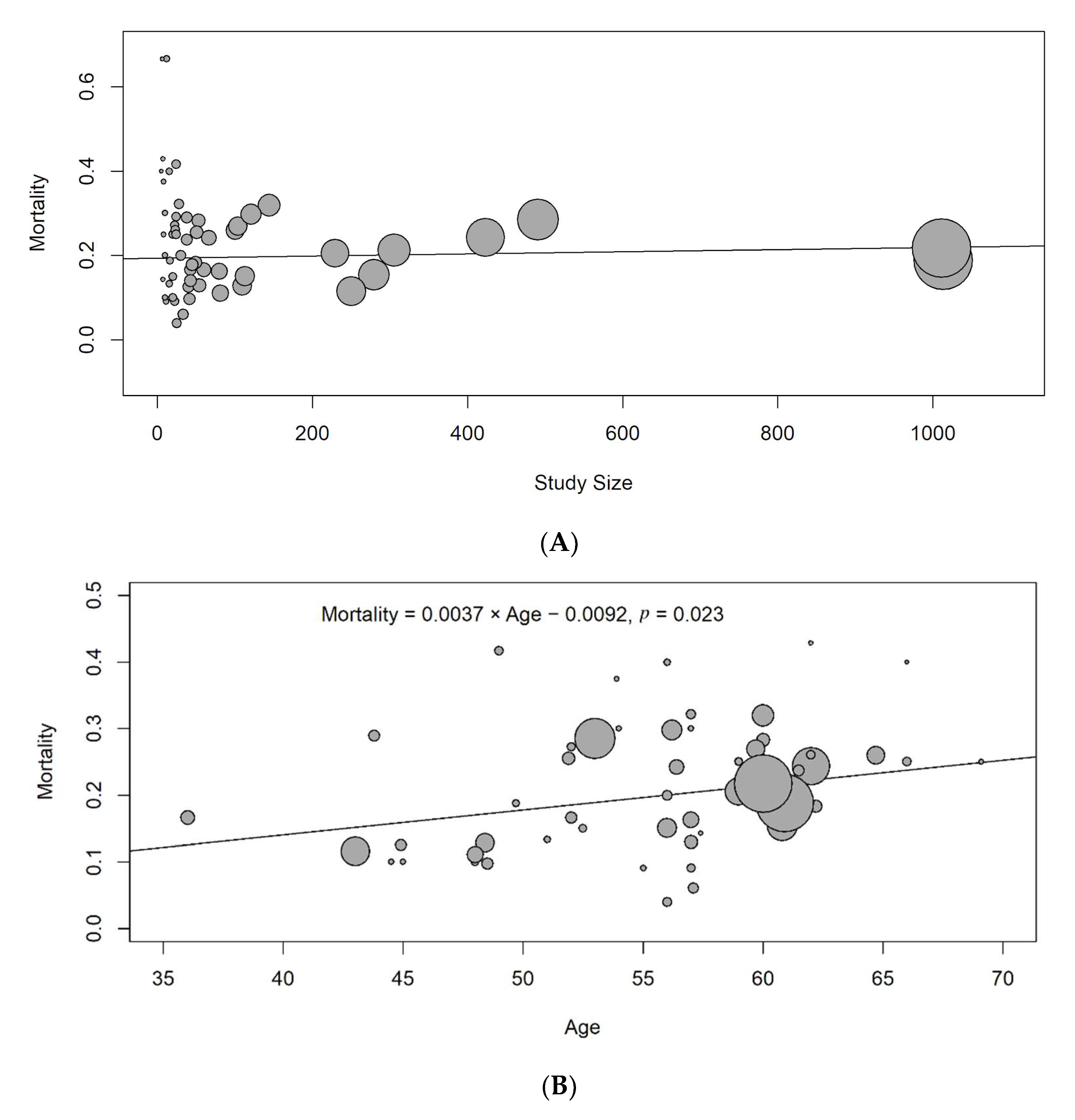
3.5. Sensitivity Analysis, Subgroup Analysis and Meta-Regression
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Perico, L.; Benigni, A.; Casiraghi, F.; Ng, L.F.P.; Renia, L.; Remuzzi, G. Immunity, endothelial injury and complement-induced coagulopathy in COVID-19. Nat. Rev. Nephrol. 2021, 17, 46–64. [Google Scholar] [CrossRef] [PubMed]
- Argenziano, M.G.; Bruce, S.L.; Slater, C.L.; Tiao, J.R.; Baldwin, M.R.; Barr, R.G.; Chang, B.P.; Chau, K.H.; Choi, J.J.; Gavin, N.; et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: Retrospective case series. BMJ 2020, 369, m1996. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, J.S.; Ng, J.H.; Ross, D.W.; Sharma, P.; Shah, H.H.; Barnett, R.L.; Hazzan, A.D.; Fishbane, S.; Jhaveri, K.D.; Abate, M.; et al. Acute kidney injury in patients hospitalized with COVID-19. Kidney Int. 2020, 98, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Gupta, S.; Hayek, S.S.; Wang, W.; Chan, L.; Mathews, K.S.; Melamed, M.L.; Brenner, S.K.; Leonberg-Yoo, A.; Schenck, E.J.; Radbel, J.; et al. Factors associated with death in critically ill patients with coronavirus disease 2019 in the US. JAMA Intern. Med. 2020, 180, 1436–1447. [Google Scholar] [CrossRef]
- Husain-Syed, F.; Ferrari, F.; Sharma, A.; Danesi, T.H.; Bezerra, P.; Lopez-Giacoman, S.; Samoni, S.; de Cal, M.; Corradi, V.; Virzì, G.M.; et al. Preoperative renal functional reserve predicts risk of acute kidney injury after cardiac operation. Ann. Thorac. Surg. 2018, 105, 1094–1101. [Google Scholar] [CrossRef] [Green Version]
- Mehrotra, A.; Rose, C.; Pannu, N.; Gill, J.; Tonelli, M.; Gill, J.S. Incidence and consequences of acute kidney injury in kidney transplant recipients. Am. J. Kidney Dis. 2012, 59, 558–565. [Google Scholar] [CrossRef]
- Hundemer, G.L.; Srivastava, A.; A Jacob, K.; Krishnasamudram, N.; Ahmed, S.; Boerger, E.; Sharma, S.; Pokharel, K.K.; A Hirji, S.; Pelletier, M.; et al. Acute kidney injury in renal transplant recipients undergoing cardiac surgery. Nephrol. Dial. Transplant. 2021, 36, 185–196. [Google Scholar] [CrossRef]
- Yeo, W.-S.; Ng, Q.X. Biomarkers of immune tolerance in kidney transplantation: An overview. Pediatr. Nephrol. 2021, 1–10. [Google Scholar] [CrossRef]
- Lewis, N.M.; Chu, V.T.; Ye, D.; E Conners, E.; Gharpure, R.; Laws, R.L.; E Reses, H.; Freeman, B.D.; Fajans, M.; Rabold, E.M.; et al. Household transmission of severe acute respiratory syndrome coronavirus-2 in the United States. Clin. Infect. Dis. 2021, 73, e1805–e1813. [Google Scholar] [CrossRef]
- Marinaki, S.; Tsiakas, S.; Korogiannou, M.; Grigorakos, K.; Papalois, V.; Boletis, I. A systematic review of COVID-19 infection in kidney transplant recipients: A universal effort to preserve patients’ lives and allografts. J. Clin. Med. 2020, 9, 2986. [Google Scholar] [CrossRef]
- Choi, M.; Bachmann, F.; Naik, M.G.; Duettmann, W.; Duerr, M.; Zukunft, B.; Schwarz, T.; Corman, V.M.; Liefeldt, L.; Budde, K.; et al. Low seroprevalence of SARS-CoV-2 antibodies during systematic antibody screening and serum responses in patients after COVID-19 in a German transplant center. J. Clin. Med. 2020, 9, 3401. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Viechtbauer, W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Translator Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Higgins, J.P.T.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 6th ed.; Cochrane: Oxford, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 15 March 2021).
- Schoch, D.; Sommer, R.; Augustin, M.; Ständer, S.; Blome, C. Patient-reported outcome measures in pruritus: A systematic review of measurement properties. J. Investig. Dermatol. 2017, 137, 2069–2077. [Google Scholar] [CrossRef] [Green Version]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. 2013. Available online: http://www.ohri.ca/programs/clinicalepidemiology/oxford.asp (accessed on 15 March 2021).
- Abolghasemi, S.; Mardani, M.; Sali, S.; Honarvar, N.; Baziboroun, M. COVID-19 and kidney transplant recipients. Transpl. Infect. Dis. 2020, 22, e13413. [Google Scholar] [CrossRef]
- Abrishami, A.; Samavat, S.; Behnam, B.; Arab-Ahmadi, M.; Nafar, M.; Taheri, M.S. Clinical course, imaging features, and outcomes of COVID-19 in kidney transplant recipients. Eur. Urol. 2020, 78, 281–286. [Google Scholar] [CrossRef]
- Akalin, E.; Azzi, Y.; Bartash, R.; Seethamraju, H.; Parides, M.; Hemmige, V.; Ross, M.; Forest, S.; Goldstein, D.Y.; Ajaimy, M.; et al. Covid-19 and kidney transplantation. N. Engl. J. Med. 2020, 382, 2475–2477. [Google Scholar] [CrossRef]
- Alberici, F.; Delbarba, E.; Manenti, C.; Econimo, L.; Valerio, F.; Pola, A.; Maffei, C.; Possenti, S.; Zambetti, N.; Moscato, M.; et al. A single center observational study of the clinical characteristics and short-term outcome of 20 kidney transplant patients admitted for SARS-CoV2 pneumonia. Kidney Int. 2020, 97, 1083–1088. [Google Scholar] [CrossRef]
- Azzi, Y.; Parides, M.; Alani, O.; Loarte-Campos, P.; Bartash, R.; Forest, S.; Colovai, A.; Ajaimy, M.; Liriano-Ward, L.; Pynadath, C.; et al. COVID-19 infection in kidney transplant recipients at the epicenter of pandemics. Kidney Int. 2020, 98, 1559–1567. [Google Scholar] [CrossRef]
- Banerjee, D.; Popoola, J.; Shah, S.; Ster, I.C.; Quan, V.; Phanish, M. COVID-19 infection in kidney transplant recipients. Kidney Int. 2020, 97, 1076–1082. [Google Scholar] [CrossRef]
- Bell, S.; Campbell, J.; McDonald, J.; O’Neill, M.; Watters, C.; Buck, K.; Cousland, Z.; Findlay, M.; Lone, N.I.; Metcalfe, W.; et al. COVID-19 in patients undergoing chronic kidney replacement therapy and kidney transplant recipients in Scotland: Findings and experience from the Scottish renal registry. BMC Nephrol. 2020, 21, 419. [Google Scholar] [CrossRef]
- Benotmane, I.; Perrin, P.; Vargas, G.G.; Bassand, X.; Keller, N.; Lavaux, T.; Ohana, M.; Bedo, D.; Baldacini, C.; Sagnard, M.; et al. Biomarkers of cytokine release syndrome predict disease severity and mortality from COVID-19 in kidney transplant recipients. Transplantation 2021, 105, 158–169. [Google Scholar] [CrossRef]
- Bossini, N.; Alberici, F.; Delbarba, E.; Valerio, F.; Manenti, C.; Possenti, S.; Econimo, L.; Maffei, C.; Pola, A.; Terlizzi, V.; et al. Kidney transplant patients with SARS-CoV-2 infection: The Brescia Renal COVID task force experience. Arab. Archaeol. Epigr. 2020, 20, 3019–3029. [Google Scholar] [CrossRef]
- Caillard, S.; Anglicheau, D.; Matignon, M.; Durrbach, A.; Greze, C.; Frimat, L.; Thaunat, O.; Legris, T.; Moal, V.; Westeel, P.F.; et al. An initial report from the French SOT COVID Registry suggests high mortality due to COVID-19 in recipients of kidney transplants. Kidney Int. 2020, 98, 1549–1558. [Google Scholar] [CrossRef]
- Chavarot, N.; Gueguen, J.; Bonnet, G.; Jdidou, M.; Trimaille, A.; Burger, C.; Amrouche, L.; Weizman, O.; Pommier, T.; Aubert, O.; et al. COVID-19 severity in kidney transplant recipients is similar to nontransplant patients with similar comorbidities. Arab. Archaeol. Epigr. 2021, 21, 1285–1294. [Google Scholar] [CrossRef]
- Chen, T.Y.; Farghaly, S.; Cham, S.; Tatem, L.L.; Sin, J.H.; Rauda, R.; Ribisi, M.; Sumrani, N. COVID-19 pneumonia in kidney transplant recipients: Focus on immunosuppression management. Transpl. Infect. Dis. 2020, 22, e13378. [Google Scholar] [CrossRef] [PubMed]
- Coll, E.; Fernández-Ruiz, M.; Sánchez-Álvarez, J.E.; Martínez-Fernández, J.R.; Crespo, M.; Gayoso, J.; Bada-Bosch, T.; Oppenheimer, F.; Moreso, F.; López-Oliva, M.O.; et al. COVID-19 in transplant recipients: The Spanish experience. Am. J. Transplant. 2021, 21, 1825–1837. [Google Scholar] [CrossRef] [PubMed]
- Craig-Schapiro, R.; Salinas, T.; Lubetzky, M.; Abel, B.T.; Sultan, S.; Lee, J.R.; Kapur, S.; Aull, M.J.; Dadhania, D.M. COVID-19 outcomes in patients waitlisted for kidney transplantation and kidney transplant recipients. Arab. Archaeol. Epigr. 2021, 21, 1576–1585. [Google Scholar] [CrossRef] [PubMed]
- Cravedi, P.; Mothi, S.S.; Azzi, Y.; Haverly, M.; Farouk, S.S.; Pérez-Sáez, M.J.; Redondo-Pachón, M.D.; Murphy, B.; Florman, S.; Cyrino, L.G.; et al. COVID-19 and kidney transplantation: Results from the TANGO International Transplant Consortium. Arab. Archaeol. Epigr. 2020, 20, 3140–3148. [Google Scholar] [CrossRef]
- Cristelli, M.P.; Viana, L.A.; Dantas, M.T.; Martins, S.B.; Fernandes, R.; Nakamura, M.R.; Santos, D.W.; Taddeo, J.B.; Azevedo, V.F.; Foresto, R.D.; et al. The full spectrum of COVID-19 development and recovery among kidney transplant recipients. Transplantation 2021, 105, 1433–1444. [Google Scholar] [CrossRef]
- Demir, E.; Uyar, M.; Parmaksiz, E.; Sinangil, A.; Yelken, B.; Dirim, A.B.; Merhametsiz, O.; Yadigar, S.; Ucar, Z.A.; Ucar, A.R.; et al. COVID-19 in kidney transplant recipients: A multicenter experience in Istanbul. Transpl. Infect. Dis. 2020, 22, e13371. [Google Scholar] [CrossRef]
- Devresse, A.; Belkhir, L.; Vo, B.; Ghaye, B.; Scohy, A.; Kabamba, B.; Goffin, E.; De Greef, J.; Mourad, M.; De Meyer, M.; et al. COVID-19 infection in kidney transplant recipients: A single-center case series of 22 cases from Belgium. Kidney Med. 2020, 2, 459–466. [Google Scholar] [CrossRef]
- Dheir, H.; SİPAHİ, S.; Yaylaci, S.; Çetin, E.S.; Genç, A.B.; Firat, N.; Köroğlu, M.; Muratdaği, G.; Tomak, Y.; Özmen, K.; et al. Clinical course of COVID-19 disease in immunosuppressed renal transplant patients. Turk. J. Med. Sci. 2021, 51, 428–434. [Google Scholar] [CrossRef]
- Elec, A.D.; Oltean, M.; Goldis, P.; Cismaru, C.; Lupse, M.; Muntean, A.; Elec, F.I. COVID-19 after kidney transplantation: Early outcomes and renal function following antiviral treatment. Int. J. Infect. Dis. 2021, 104, 426–432. [Google Scholar] [CrossRef]
- Elhadedy, M.A.; Marie, Y.; Halawa, A. COVID-19 in renal transplant recipients: Case series and a brief review of current evidence. Nephron 2020, 145, 1–7. [Google Scholar] [CrossRef]
- Elias, M.; Pievani, D.; Randoux, C.; Louis, K.; Denis, B.; DeLion, A.; Le Goff, O.; Antoine, C.; Greze, C.; Pillebout, E.; et al. COVID-19 infection in kidney transplant recipients: Disease incidence and clinical outcomes. J. Am. Soc. Nephrol. 2020, 31, 2413–2423. [Google Scholar] [CrossRef]
- Favà, A.; Cucchiari, D.; Montero, N.; Toapanta, N.; Centellas, F.J.; Vila-Santandreu, A.; Coloma, A.; Meneghini, M.; Manonelles, A.; Sellarés, J.; et al. Clinical characteristics and risk factors for severe COVID-19 in hospitalized kidney transplant recipients: A multicentric cohort study. Arab. Archaeol. Epigr. 2020, 20, 3030–3041. [Google Scholar] [CrossRef]
- Fernández-Ruiz, M.; Andrés, A.; Loinaz, C.; Delgado, J.F.; López-Medrano, F.; Juan, R.S.; González, E.; Polanco, N.; Folgueira, M.D.; Lalueza, A.; et al. COVID-19 in solid organ transplant recipients: A single-center case series from Spain. Arab. Archaeol. Epigr. 2020, 20, 1849–1858. [Google Scholar] [CrossRef]
- Georgery, H.; Devresse, A.; Scohy, A.; Kabamba, B.; Darius, T.; Buemi, A.; De Greef, J.; Belkhir, L.; Yombi, J.-C.; Goffin, E.; et al. The second wave of COVID-19 disease in a kidney transplant recipient cohort: A single-center experience in Belgium. Transplantation 2021, 105, e41–e42. [Google Scholar] [CrossRef]
- Gupta, A.; Kute, V.B.; Patel, H.V.; Engineer, D.P.; Banerjee, S.; Modi, P.R.; Rizvi, S.J.; Mishra, V.V.; Patel, A.H.; Navadiya, V. Feasibility of convalescent plasma therapy in kidney transplant recipients with severe COVID-19: A single-center prospective cohort study. Exp. Clin. Transplant. 2021, 19, 304–309. [Google Scholar] [CrossRef] [PubMed]
- Hardesty, A.; Pandita, A.; Vieira, K.; Rogers, R.; Merhi, B.; Osband, A.J.; Aridi, J.; Shi, Y.; Bayliss, G.; Cosgrove, C.; et al. Coronavirus disease 2019 in kidney transplant recipients: Single-center experience and case-control study. Transplant. Proc. 2021, 53, 1187–1193. [Google Scholar] [CrossRef]
- Hilbrands, L.B.; Duivenvoorden, R.; Vart, P.; Franssen, C.F.M.; Hemmelder, M.H.; Jager, K.J.; Kieneker, L.M.; Noordzij, M.; Pena, M.J.; de Vries, H.; et al. COVID-19-related mortality in kidney transplant and dialysis patients: Results of the ERACODA collaboration. Nephrol. Dial. Transplant. 2020, 35, 1973–1983. [Google Scholar] [CrossRef] [PubMed]
- The Columbia University Kidney Transplant Program. Early description of coronavirus 2019 disease in kidney transplant recipients in New York. J. Am. Soc. Nephrol. 2020, 31, 1150–1156. [Google Scholar] [CrossRef] [PubMed]
- Jager, K.J.; Kramer, A.; Chesnaye, N.C.; Couchoud, C.; Sánchez-Álvarez, J.E.; Garneata, L.; Collart, F.; Hemmelder, M.H.; Ambühl, P.; Kerschbaum, J.; et al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020, 98, 1540–1548. [Google Scholar] [CrossRef]
- Katz-Greenberg, G.; Yadav, A.; Gupta, M.; Martinez-Cantarin, M.P.; Gulati, R.; Ackerman, L.; Belden, K.; Singh, P. Outcomes of COVID-19-positive kidney transplant recipients: A single-center experience. Clin. Nephrol. 2020, 94, 318–321. [Google Scholar] [CrossRef] [PubMed]
- Kumaresan, M.; Babu, M.; Parthasarathy, R.; Matthew, M.; Kathir, C.; Rohit, A. Clinical profile of SARS-CoV-2 infection in kidney transplant patients-A single centre observational study. Indian J. Transplant. 2020, 14, 288. [Google Scholar] [CrossRef]
- Kute, V.B.; Bhalla, A.K.; Guleria, S.; Ray, D.S.; Bahadur, M.M.; Shingare, A.; Hegde, U.; Gang, S.; Raju, S.; Patel, H.V.; et al. Clinical profile and outcome of COVID-19 in 250 kidney transplant recipients: A multicenter cohort study from India. Transplantation 2021, 105, 851–860. [Google Scholar] [CrossRef]
- Lubetzky, M.; Aull, M.J.; Craig-Schapiro, R.; Lee, J.R.; Marku-Podvorica, J.; Salinas, T.; Gingras, L.; Lee, J.B.; Sultan, S.; Kodiyanplakkal, R.P.; et al. Kidney allograft recipients, immunosuppression, and coronavirus disease-2019: A report of consecutive cases from a New York City transplant center. Nephrol. Dial. Transplant. 2020, 35, 1250–1261. [Google Scholar] [CrossRef]
- Lum, E.; Bunnapradist, S.; Multani, A.; Beaird, O.E.; Carlson, M.; Gaynor, P.; Kotton, C.; Abdalla, B.; Danovitch, G.; Kendrick, E.; et al. Spectrum of coronavirus disease 2019 outcomes in kidney transplant recipients: A single-center experience. Transplant. Proc. 2020, 52, 2654–2658. [Google Scholar] [CrossRef]
- Mamode, N.; Ahmed, Z.; Jones, G.; Banga, N.; Motallebzadeh, R.; Tolley, H.; Marks, S.; Stojanovic, J.; Khurram, M.A.; Thuraisingham, R.; et al. Mortality rates in transplant recipients and transplantation candidates in a high-prevalence COVID-19 environment. Transplantation 2021, 105, 212–215. [Google Scholar] [CrossRef]
- Maritati, F.; Cerutti, E.; Zuccatosta, L.; Fiorentini, A.; Finale, C.; Ficosecco, M.; Cristiano, F.; Capestro, A.; Balestra, E.; Taruscia, D.; et al. SARS-CoV-2 infection in kidney transplant recipients: Experience of the Italian Marche region. Transpl. Infect. Dis. 2020, 22, e13377. [Google Scholar] [CrossRef]
- De Meester, J.; De Bacquer, D.; Naesens, M.; Meijers, B.; Couttenye, M.M.; De Vriese, A.S.; For the NBVN Kidney Registry Group. Incidence, characteristics, and outcome of COVID-19 in adults on kidney replacement therapy: A regionwide registry study. J. Am. Soc. Nephrol. 2021, 32, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Mella, A.; Mingozzi, S.; Gallo, E.; Lavacca, A.; Rossetti, M.; Clari, R.; Randone, O.; Maffei, S.; Salomone, M.; Imperiale, D.; et al. Case series of six kidney transplanted patients with COVID-19 pneumonia treated with tocilizumab. Transpl. Infect. Dis. 2020, 22, e13348. [Google Scholar] [CrossRef]
- Meziyerh, S.; Van Der Helm, D.; de Vries, A. Vulnerabilities in kidney transplant recipients with COVID-19: A single center experience. Transpl. Int. 2020, 33, 1557–1561. [Google Scholar] [CrossRef]
- Mohamed, I.H.; Chowdary, P.B.; Shetty, S.; Sammartino, C.; Sivaprakasam, R.; Lindsey, B.; Thuraisingham, R.; Yaqoob, M.M.; Khurram, M.A. Outcomes of renal transplant recipients with SARS-CoV-2 infection in the eye of the storm: A comparative study with waitlisted patients. Transplantation 2021, 105, 115–120. [Google Scholar] [CrossRef]
- Molaei, H.; Khedmat, L.; Nemati, E.; Rostami, Z.; Saadat, S.H. Iranian kidney transplant recipients with COVID-19 infection: Clinical outcomes and cytomegalovirus coinfection. Transpl. Infect. Dis. 2021, 23, 13455. [Google Scholar] [CrossRef]
- Monfared, A.; Dashti-Khavidaki, S.; Jafari, R.; Jafari, A.; Ramezanzade, E.; Lebadi, M.; Haghdar-Saheli, Y.; Aghajanzadeh, P.; Khosravi, M.; Movassaghi, A.; et al. Clinical characteristics and outcome of COVID-19 pneumonia in kidney transplant recipients in Razi hospital, Rasht, Iran. Transpl. Infect. Dis. 2020, 22, e13420. [Google Scholar] [CrossRef]
- Montagud-Marrahi, E.; Cofan, F.; Torregrosa, J.; Cucchiari, D.; Ventura-Aguiar, P.; Revuelta, I.; Bodro, M.; Piñeiro, G.J.; Esforzado, N.; Ugalde, J.; et al. Preliminary data on outcomes of SARS-CoV-2 infection in a Spanish single center cohort of kidney recipients. Arab. Archaeol. Epigr. 2020, 20, 2958–2959. [Google Scholar] [CrossRef]
- Nair, V.; Jandovitz, N.; Hirsch, J.S.; Nair, G.; Abate, M.; Bhaskaran, M.; Grodstein, E.; Berlinrut, I.; Hirschwerk, D.; Cohen, S.L.; et al. COVID-19 in kidney transplant recipients. Arab. Archaeol. Epigr. 2020, 20, 1819–1825. [Google Scholar] [CrossRef] [PubMed]
- Oto, O.A.; Ozturk, S.; Turgutalp, K.; Arici, M.; Alpay, N.; Merhametsiz, O.; Sipahi, S.; Ogutmen, M.B.; Yelken, B.; Altiparmak, M.R.; et al. Predicting the outcome of COVID-19 infection in kidney transplant recipients. BMC Nephrol. 2021, 22, 100. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, S.; Turgutalp, K.; Arici, M.; Odabas, A.R.; Altiparmak, M.R.; Aydin, Z.; Cebeci, E.; Basturk, T.; Soypacaci, Z.; Sahin, G.; et al. Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: A nationwide analysis from Turkey. Nephrol. Dial. Transplant. 2020, 35, 2083–2095. [Google Scholar] [CrossRef] [PubMed]
- Phanish, M.; Ster, I.C.; Ghazanfar, A.; Cole, N.; Quan, V.; Hull, R.; Banerjee, D. Systematic review and meta-analysis of COVID-19 and kidney transplant recipients, the South West London kidney transplant network experience. Kidney Int. Rep. 2021, 6, 574–585. [Google Scholar] [CrossRef] [PubMed]
- Pierrotti, L.C.; Junior, J.O.R.; Freire, M.P.; Machado, D.J.B.; Moreira, R.M.; Ventura, C.G.; Litvoc, M.N.; Nahas, W.C.; David-Neto, E. COVID-19 among kidney-transplant recipients requiring hospitalization: Preliminary data and outcomes from a single-center in Brazil. Transpl. Int. 2020, 33, 1837–1842. [Google Scholar] [CrossRef]
- Rodriguez-Cubillo, B.; De La Higuera, M.A.M.; Lucena, R.; Franci, E.V.; Hurtado, M.; Romero, N.C.; Moreno, A.R.; Valencia, D.; Velo, M.; Fornie, I.S.; et al. Should cyclosporine be useful in renal transplant recipients affected by SARS-CoV-2? Arab. Archaeol. Epigr. 2020, 20, 3173–3181. [Google Scholar] [CrossRef]
- De Sandes-Freitas, T.V.; Cristelli, M.P.; Neri, B.D.O.; Guedes, A.L.M.D.O.; Esmeraldo, R.D.M.; Garcia, V.D.; Prá, R.L.D.; Suassuna, J.H.R.; Rioja, S.D.S.; Zanocco, J.A.; et al. The unpredictable outcome of SARS-CoV-2 in kidney transplant recipients with HIV-infection. Transplantation 2021, 105, e9–e10. [Google Scholar] [CrossRef]
- Santeusanio, A.D.; Menon, M.C.; Liu, C.; Bhansali, A.; Patel, N.; Mahir, F.; Rana, M.; Tedla, F.; Mahamid, A.; Fenig, Y.; et al. Influence of patient characteristics and immunosuppressant management on mortality in kidney transplant recipients hospitalized with coronavirus disease 2019 (COVID-19). Clin. Transplant. 2021, 35, e14221. [Google Scholar] [CrossRef]
- Shrivastava, P.; Prashar, R.; Khoury, N.; Patel, A.; Yeddula, S.; Kitajima, T.; Nagai, S.; Samaniego, M. Acute kidney injury in a predominantly African American cohort of kidney transplant recipients with COVID-19 infection. Transplantation 2021, 105, 201–205. [Google Scholar] [CrossRef]
- Tejada, C.D.J.; Zachariah, M.; Cruz, A.B.V.; Hussein, S.; Wipula, E.; Meeks, N.; Wolff, J.; Chandrasekar, P.H. Favorable outcome of COVID-19 among African American (AA) renal transplant recipients in Detroit. Clin. Transplant. 2021, 35, e14169. [Google Scholar] [CrossRef]
- Trujillo, H.; Caravaca-Fontán, F.; Sevillano, Á.; Gutiérrez, E.; Fernández-Ruiz, M.; López-Medrano, F.; Hernández, A.; Aguado, J.M.; Praga, M.; Andrés, A. Tocilizumab use in kidney transplant patients with COVID-19. Clin. Transplant. 2020, 34. [Google Scholar] [CrossRef]
- Villa, L.; Krüger, T.; Seikrit, C.; Mühlfeld, A.S.; Kunter, U.; Werner, C.; Kleines, M.; Schulze-Hagen, M.; Dreher, M.; Kersten, A.; et al. Time on previous renal replacement therapy is associated with worse outcomes of COVID-19 in a regional cohort of kidney transplant and dialysis patients. Medicine 2021, 100, e24893. [Google Scholar] [CrossRef]
- Villanego, F.; Mazuecos, A.; Pérez-Flores, I.M.; Moreso, F.; Andrés, A.; Jiménez-Martín, C.; Molina, M.; Canal, C.; Sánchez-Cámara, L.A.; Zárraga, S.; et al. Predictors of severe COVID-19 in kidney transplant recipients in the different epidemic waves: Analysis of the Spanish Registry. Arab. Archaeol. Epigr. 2021, 21, 2573–2582. [Google Scholar] [CrossRef]
- Willicombe, M.; Gleeson, S.; Clarke, C.; Dor, F.; Prendecki, M.; Lightstone, L.; Lucisano, G.; McAdoo, S.; Thomas, D.; on behalf of the ICHNT Renal COVID Group. Identification of Patient Characteristics Associated With SARS-CoV-2 Infection and Outcome in Kidney Transplant Patients Using Serological Screening. Transplantation 2021, 105, 151–157. [Google Scholar] [CrossRef]
- Zhu, L.; Gong, N.; Liu, B.; Lu, X.; Chen, D.; Chen, S.; Shu, H.; Ma, K.; Xu, X.; Guo, Z.; et al. Coronavirus disease 2019 pneumonia in immunosuppressed renal transplant recipients: A summary of 10 confirmed cases in Wuhan, China. Eur. Urol. 2020, 77, 748–754. [Google Scholar] [CrossRef]
- Meyerowitz-Katz, G.; Merone, L. A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. Int. J. Infect. Dis. 2020, 101, 138–148. [Google Scholar] [CrossRef]
- Chen, Y.-T.; Shao, S.-C.; Hsu, C.-K.; Wu, I.-W.; Hung, M.-J.; Chen, Y.-C. Incidence of acute kidney injury in COVID-19 infection: A systematic review and meta-analysis. Crit. Care 2020, 24, 1–4. [Google Scholar] [CrossRef]
- Levin, A.T.; Hanage, W.P.; Owusu-Boaitey, N.; Cochran, K.B.; Walsh, S.P.; Meyerowitz-Katz, G. Assessing the age specificity of infection fatality rates for COVID-19: Systematic review, meta-analysis, and public policy implications. Eur. J. Epidemiol. 2020, 35, 1123–1138. [Google Scholar] [CrossRef]
- Gleeson, S.E.; Formica, R.N.; Marin, E.P. Outpatient management of the kidney transplant recipient during the SARS-CoV-2 virus pandemic. Clin. J. Am. Soc. Nephrol. 2020, 15, 892–895. [Google Scholar] [CrossRef]
- Beran, A.; Zink, E.; Mhanna, M.; Abugharbyeh, A.; Do, J.H.; Duggan, J.; Assaly, R. Transmissibility and viral replication of SARS-COV-2 in immunocompromised patients. J. Med. Virol. 2021, 93, 4156–4160. [Google Scholar] [CrossRef]
- Chan, S.; Pascoe, E.M.; Clayton, P.A.; McDonald, S.P.; Lim, W.H.; Sypek, M.P.; Palmer, S.C.; Isbel, N.M.; Francis, R.S.; Campbell, S.B.; et al. Infection-related mortality in recipients of a kidney transplant in Australia and New Zealand. Clin. J. Am. Soc. Nephrol. 2019, 14, 1484–1492. [Google Scholar] [CrossRef] [PubMed]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345. [Google Scholar] [CrossRef] [PubMed]
- Kim, L.; Garg, S.; O’Halloran, A.; Whitaker, M.; Pham, H.; Anderson, E.J.; Armistead, I.; Bennett, N.M.; Billing, L.; Como-Sabetti, K.; et al. Risk factors for intensive care unit admission and in-hospital mortality among hospitalized adults identified through the US coronavirus disease 2019 (COVID-19)-associated hospitalization surveillance network (COVID-NET). Clin. Infect. Dis. 2021, 72, e206–e214. [Google Scholar] [CrossRef] [PubMed]
- Atkins, J.L.; Masoli, J.A.H.; Delgado, J.; Pilling, L.C.; Kuo, C.-L.; Kuchel, G.A.; Melzer, D. Preexisting comorbidities predicting COVID-19 and mortality in the UK biobank community cohort. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020, 75, 2224–2230. [Google Scholar] [CrossRef]
- Cardinal, H.; Dieudé, M.; Hébert, M.-J. Endothelial dysfunction in kidney transplantation. Front. Immunol. 2018, 9, 1130. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Fang, J.-T.; Yang, C.-W. Endothelial dysfunction for acute kidney injury in coronavirus disease 2019: How concerned should we be? Nephron 2021, 145, 513–517. [Google Scholar] [CrossRef]
- A Kellum, J.; van Till, J.W.O.; Mulligan, G. Targeting acute kidney injury in COVID-19. Nephrol. Dial. Transplant. 2020, 35, 1652–1662. [Google Scholar] [CrossRef]
- Chang, R.; Elhusseiny, K.M.; Yeh, Y.-C.; Sun, W.-Z. COVID-19 ICU and mechanical ventilation patient characteristics and outcomes—A systematic review and meta-analysis. PLoS ONE 2021, 16, e0246318. [Google Scholar] [CrossRef]
- Thakur, B.; Dubey, P.; Benitez, J.; Torres, J.P.; Reddy, S.; Shokar, N.; Aung, K.; Mukherjee, D.; Dwivedi, A.K. A systematic review and meta-analysis of geographic differences in comorbidities and associated severity and mortality among individuals with COVID-19. Sci. Rep. 2021, 11, 1–13. [Google Scholar] [CrossRef]
- Basuki, W.; Pramudya, D.; Adiwinoto, R.D. Cyclosporine a improves outcome of kidney transplant recipients with coronav irus disease 2019: A meta-analysis. New Armen. Med. J. 2020, 14, 100–106. [Google Scholar]


| Study | Design | Country | Location | NOS | Age (Mean, y/o) | Sample Size | Outcome | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mortality | ICU | MV | AKI | KRT | Graft Loss | |||||||
| Abolghasemi [19] | RC | Iran | Multi-center | 6 | 49 | 24 | 10 | 12 | NR | NR | NR | NR |
| Abrishami [20] | RC | Iran | Single-center | 5 | 47.6 | 12 | 8 | 10 | 9 | NR | NR | NR |
| Akalin [21] | RC | USA | Single-center | 5 | 36 | 60 | 10 | NR | 11 | NR | 6 | NR |
| Alberici [22] | RC | Italy | Single-center | 5 | 59 | 20 | 5 | 4 | 0 | 6 | 1 | NR |
| Azzi [23] | PC | USA | Single-center | 5 | 59 | 229 | 47 | NR | NR | NR | NR | NR |
| Azzi [23] | PC | USA | Single-center | 5 | 61 | 79 ## | NR | NR | 28 | 18 | 18 | 5 |
| Banerjee [24] | RC | UK | Multi-center | 6 | 57.4 | 7 | 1 | 4 | 2 | 4 | 3 | NR |
| Bell [25] | RC | Scotland (Scottish Renal Registry) | Multi-center | 7 | NR | 24 | 7 | NR | NR | NR | NR | NR |
| Benotmane [26] | RC | France | Single-center | 5 | 62.2 | 49 | 9 | 14 | 2 | 31 | 4 | NR |
| Bossini [27] | RC | Italy | Multi-center | 6 | 60 | 53 | 15 | 10 | 9 | 15 | 3 | NR |
| Caillard [28] | RC | France (nationwide registry) | Multi-center | 6 | 60.8 | 279 | 43 | 88 | 72 | 106 | 27 | 9 |
| Chavarot [29] | RC | France | Multi-center | 7 | 64.7 | 100 | 26 | 34 | 29 | NR | NR | NR |
| Chen [30] | RC | USA | Single-center | 5 | 56 | 30 | 6 | NR | 7 | NR | 4 | NR |
| Coll [31] | RC | Spain | Multi-center | 6 | 62 | 423 | 103 | 57 | 36 | NR | NR | NR |
| Craig-Schapiro [32] | RC | USA, NY | Single-center | 6 | 57 | 80 | 13 | NR | 16 | 25 | 4 | 4 |
| Cravedi [33] | RC | USA | Multi-center | 6 | 60 | 144 | 46 | NR | 42 | 74 | NR | NR |
| Cristelli [34] | PC | Brazil | Single-center | 5 | 53 | 491 | 140 | NR | 156 | 229 | 155 | NR |
| Demir [35] | RC | Turkey | Multi-center | 6 | 44.9 | 40 | 5 | 7 | 6 | 14 | NR | NR |
| Devresse [36] | PC | USA | Single-center | 5 | 57 | 22 | 2 | 2 | 2 | 5 | 0 | NR |
| Dheir [37] | RC | Turkey | Single-center | 5 | 48 | 20 | 2 | NR | 2 | 5 | 2 | NR |
| Elec [38] | RC | Romania | Single-center | 5 | 52 | 42 | 7 | 8 | NR | 10 | N | NR |
| Elhadedy [39] | RC | UK | Multi-center | 6 | 50.1 | 8 | 0 | 1 | 1 | 2 | 1 | 0 |
| Elias [40] | PC | France | Multi-center | 7 | 56.4 | 66 | 16 | 15 | 15 | 28 | 7 | NR |
| Favà [41] | RC | Spain | Multi-center | 6 | 59.7 | 104 | 28 | NR | 14 | 47 | NR | NR |
| Fernández-Ruiz [42] | RC | Spain | Single-center | 5 | 69.1 | 8 | 2 | 0 | 0 | NR | NR | NR |
| Georgery [43] | RC | Belgium | Single-center | 5 | 60.6 | 45 | 8 | 14 | 14 | NR | NR | NR |
| Gupta [44] | PC | India | Single-center | 5 | 44.5 | 10 | 1 | NR | NR | NR | NR | NR |
| Hardesty [45] | RC | USA | Single-center | 6 | 55 | 11 | 1 | NR | 3 | 1 | 1 | NR |
| Hilbrands [46] | PC | Europe, ERACODA collaboration | Multi-center | 7 | 60 | 305 | 65 | 57 | 49 | 30+ | 30 | NR |
| Husain [47] | RC | USA, NY (Columbia University Vagelos College of Physicians and Surgeons) | Single-center | 5 | 51 | 15 | 2 | NR | 4 | 6 | NR | NR |
| Jager [48] | PC | Europe, ERA-EDTA Registry | Multi-center | 7 | 60.9 | 1013 | 191 | NR | NR | NR | NR | NR |
| Katz-Greenberg [49] | RC | USA, Philadelphia | Single-center | 5 | 52.5 | 20 | 3 | NR | 4 | 9 | 1 | 1 |
| Kumaresan [50] | RC | India | Single-center | 5 | 49.7 | 16 | 3 | NR | 3 | 1 | 1 | NR |
| Kute [51] | RC | India | Multi-center | 6 | 43 | 250 | 29 | 53 | 30 | 121 | 24 | 12 |
| Lubetzky [52] | RC | USA | Single-center | 5 | 57 | 54 | 7 | NR | 11 | 21 | 3 | 3 |
| Lum [53] | RC | USA | Single-center | 5 | 48.5 | 41 | 4 | 9 | 8 | 11 | 4 | 1 |
| Mamode [54] | RC | UK | Multi-center | 5 | 56.2 | 121 | 36 | 30 | 22 | NR | 19 | 15 |
| Maritati [55] | RC | Italy | Single-center | 5 | 66 | 5 | 2 | NR | 3 | 1 | 1 | NR |
| Meester [56] | PC | Belgium (NBVN Kidney Registry Group) | Multi-center | 7 | NR | 43 | 6 | NR | NR | NR | NR | NR |
| Mella [57] | RC | Italy | NR | 5 | 55.5 | 6 | 4 | NR | 2 | NR | NR | NR |
| Meziyerh [58] | RC | Netherlands | Single-center | 5 | 56 | 15 | 6 | 6 | 5 | NR | NR | NR |
| Mohamed [59] | PC | UK | Single-center | 6 | 57 | 28 | 9 | 5 | NR | 14 | 2 | NR |
| Molaei [60] | RC | Iran | Single-center | 5 | 59.6 | 10 | 2 | 4 | 4 | 7 | NR | NR |
| Monfared [61] | RC | Iran | Single-center | 5 | 52 | 22 | 6 | NR | 5 | 12 | NR | NR |
| Montagud-Marrahi [62] | RC | Spain | Single-center | 5 | 57.1 | 33 | 2 | 13 | 2 | NR | NR | 1 |
| Nair [63] | RC | USA, NY | Single-center | 5 | 57 | 10 | 3 | 5 | 4 | 5 | 1 | NR |
| Oto [64] | RC | Turkey | Multi-center | 6 | 48.4 | 109 | 14 | 22 | 19 | 46 | 4 | NR |
| Ozturk [65] | RC | Turkey | Multi-center | 7 | 48 | 81 | 9 | 17 | 14 | NR | NR | NR |
| Phanish [66] | RC | UK | Multi-center | 7 | 62 | 23 | 6 | 9 | 6 | 13 | 4 | 2 |
| Pierrotti [67] | RC | Brazil | Single-center | 5 | 51.9 | 51 | 13 | 23 | 17 | 30 | 19 | 0 |
| Rodriguez-Cubillo [68] | RC | Spain | Single-center | 5 | 66 | 24 | 6 | NR | 5 | 14 | 3 | 0 |
| Sandes-Freitas [69] | RC | Brazil (National registry) | Multi-center | 6 | 53.9 | 8 | 3 | 4 | 4 | 4 | 4 | 2 |
| Santeusanio [70] | RC | USA | Single-center | 5 | 43.8 | 38 | 11 | NR | 14 | 22 | 12 | 12 |
| Shrivastava [71] | RC | USA | Single-center | 5 | 61.5 | 38 | 9 | 13 | 9 | 27 | 6 | NR |
| Tejada [72] | RC | USA, Detroit Medical Center | Single-center | 5 | 56 | 25 | 1 | 4 | 1 | 16 | NR | NR |
| Trujillo [73] | RC | Spain | Single-center | 5 | 54 | 10 | 3 | NR | 0 | 8 | NR | NR |
| Villa [74] | RC | Germany | Single-center | 6 | 62 | 7 | 3 | NR | 3 | 4 | NR | NR |
| Villanego [75] | PC | Spain (prospectively filled registry) | Multi-center | 6 | 60 | 1011 | 220 | 140 | NR | NR | NR | NR |
| Willicombe [76] | RC + PC # | UK, London | Single-center | 5 | 56 | 113 | 17 | NR | NR | NR | NR | NR |
| Zhu [77] | RC | China | Multi-center | 6 | 45 | 10 | 1 | NR | 0 | 6 | 0 | NR |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.-J.; Kuo, G.; Lee, T.H.; Yang, H.-Y.; Wu, H.H.; Tu, K.-H.; Tian, Y.-C. Incidence of Mortality, Acute Kidney Injury and Graft Loss in Adult Kidney Transplant Recipients with Coronavirus Disease 2019: Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5162. https://doi.org/10.3390/jcm10215162
Chen J-J, Kuo G, Lee TH, Yang H-Y, Wu HH, Tu K-H, Tian Y-C. Incidence of Mortality, Acute Kidney Injury and Graft Loss in Adult Kidney Transplant Recipients with Coronavirus Disease 2019: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(21):5162. https://doi.org/10.3390/jcm10215162
Chicago/Turabian StyleChen, Jia-Jin, George Kuo, Tao Han Lee, Huang-Yu Yang, Hsin Hsu Wu, Kun-Hua Tu, and Ya-Chung Tian. 2021. "Incidence of Mortality, Acute Kidney Injury and Graft Loss in Adult Kidney Transplant Recipients with Coronavirus Disease 2019: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 21: 5162. https://doi.org/10.3390/jcm10215162
APA StyleChen, J.-J., Kuo, G., Lee, T. H., Yang, H.-Y., Wu, H. H., Tu, K.-H., & Tian, Y.-C. (2021). Incidence of Mortality, Acute Kidney Injury and Graft Loss in Adult Kidney Transplant Recipients with Coronavirus Disease 2019: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(21), 5162. https://doi.org/10.3390/jcm10215162






