Induction of Labor with Vaginal Dinoprostone (PGE2) in Patients with a Previous Cesarean Section: Obstetric and Neonatal Outcomes
Abstract
:1. Introduction
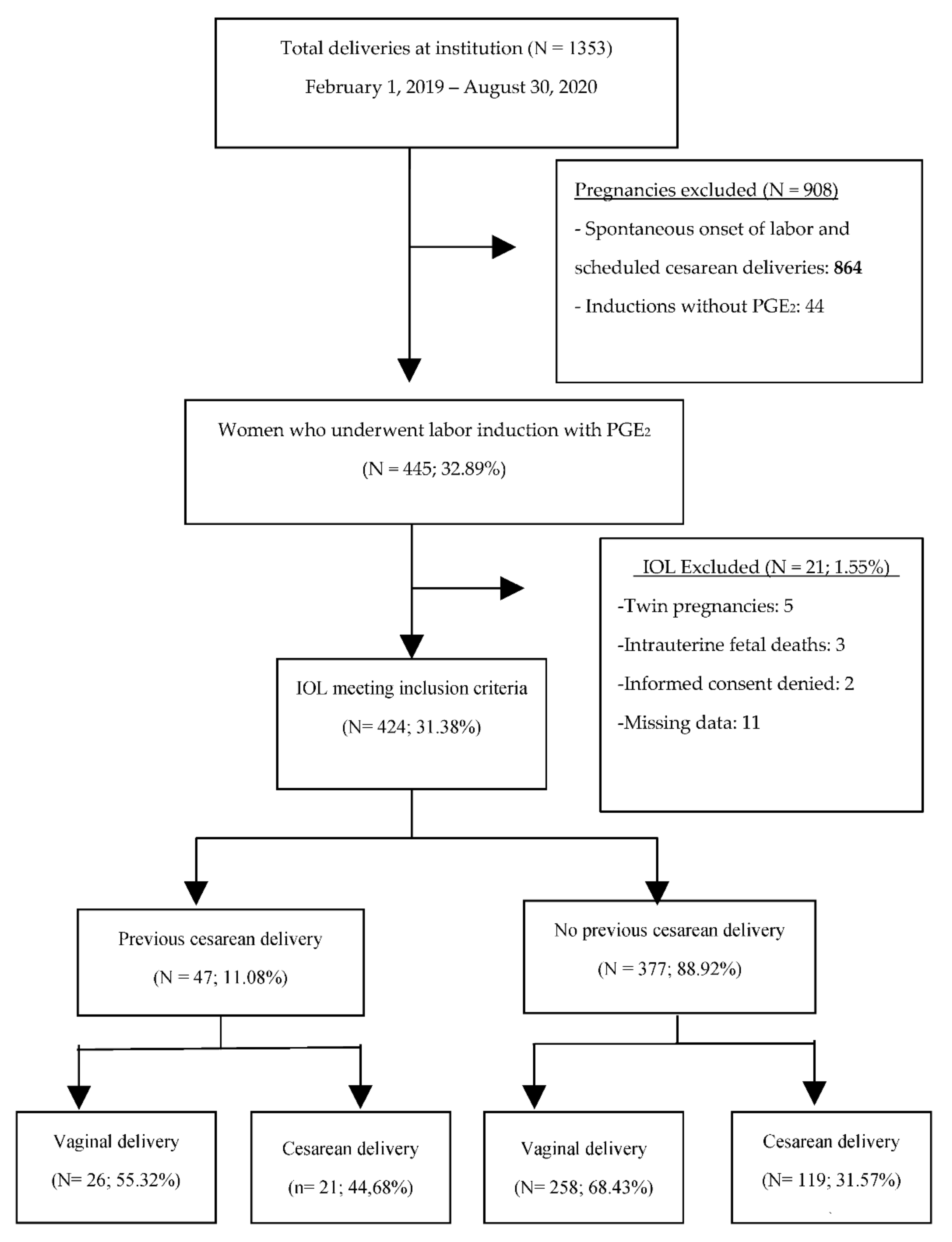
2. Materials and Methods
2.1. Information Sources
2.2. IOL Protocol at the Study Center
2.3. Statistical Analysis and Software Used
3. Results
3.1. Characteristics of the Women Undergoing IOL according to History of Previous Cesarean Delivery
3.2. Obstetric Outcomes according to History of Previous Cesarean Section
3.3. Neonatal Morbidity
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martin, J.A.; Hamilton, B.E.; Sutton, P.D.; Ventura, S.J.; Menacker, F.; Osterman, M.J. National Vital Statistics Reports Births: Final Data for 2013. Statistics 2015, 64, 1–104. [Google Scholar]
- Cunningham, F.G.; Bangdiwala, S.I.; Brown, S.S.; Dean, T.M.; Frederiksen, M.; Rowland Hogue, C.J.; King, T.; Lukacz, E.S.; Frederiksen, M.; Hogue, C.J.R.; et al. NIH consensus develop-ment conference draft statement on vaginal birth after cesarean: New insights. NIH Consens. State Sci. Statements 2010, 27, 1–42. [Google Scholar] [PubMed]
- Lydon-Rochelle, M.; Holt, V.L.; Easterling, T.R.; Martin, D.P. Risk of uterine rupture during labor among women with a prior cesarean delivery. N. Engl. J. Med. 2001, 345, 3–8. [Google Scholar] [CrossRef]
- Palatnik, A.; Grobman, W.A. Induction of labor versus expectant management for women with a prior cesarean delivery. Am. J. Obstet. Gynecol. 2015, 212, 358.e1–358.e6. [Google Scholar] [CrossRef] [PubMed]
- West, H.M.; Jozwiak, M.; Dodd, J.M. Methods of term labour induction for women with a previous caesarean section. Cochrane Database Syst. Rev. 2017, 2017, CD009792. [Google Scholar] [CrossRef]
- De Vaan, M.D.T.; ten Eikelder, M.L.G.; Jozwiak, M.; Palmer, K.R.; Davies-Tuck, M.; Bloemenkamp, K.W.M.; Mol, B.W.J.; Boulvain, M. Mechanical methods for induction of labour. Cochrane Database Syst. Rev. 2019, 2019, CD001233. [Google Scholar] [CrossRef] [Green Version]
- Birth, V.; Cesarean, A. Practice Bulletin No. 184: Vaginal Birth after Cesarean Delivery. Obstet. Gynecol. 2017, 130, e217–e233. [Google Scholar]
- Martel, M.J.; MacKinnon, C.J. No. 155-Guidelines for Vaginal Birth after Previous Caesarean Birth. J. Obstet. Gynaecol. Canada 2018, 40, e195–e207. [Google Scholar] [CrossRef]
- Wing, D.A.; Lovett, K.; Paul, R.H. Disruption of prior uterine incision following misoprostol for labor induction in women with previous cesarean delivery. Obstet. Gynecol. 1998, 91 (Suppl. 5), 828–830. [Google Scholar]
- Aslan, H.; Unlu, E.; Agar, M.; Ceylan, Y. Uterine rupture associated with misoprostol labor induction in women with previous cesarean delivery. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004, 113, 45–48. [Google Scholar] [CrossRef]
- Sociedad Española de Ginecología y Obstetricia. Inducción del Parto; GAP SEGO: Madrid, Spain, 2013; pp. 1–23. [Google Scholar]
- Landon, M.B.; Hauth, J.C.; Leveno, K.J.; Spong, C.Y.; Leindecker, S.; Varner, M.W.; Moawad, A.H.; Caritis, S.N.; Harper, M.; Wapner, R.J.; et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N. Engl. J. Med. 2004, 16, 2581–2589. [Google Scholar] [CrossRef] [PubMed]
- Ravasia, D.J.; Wood, S.L.; Pollard, J.K. Uterine rupture during induced trial of labor among women with previous cesarean delivery. Am. J. Obstet. Gynecol. 2000, 183, 1176–1179. [Google Scholar] [CrossRef]
- Parer, J.T.; Ikeda, T.; King, T.L. The 2008 National Institute of Child Health and Human Development Report on Fetal Heart Rate Monitoring. Obstet. Gynecol. 2009, 114, 136–138. [Google Scholar] [CrossRef]
- Chiossi, G.; D’Amico, R.; Tramontano, A.L.; Sampogna, V.; Laghi, V.; Facchinetti, F. Prevalence of uterine rupture among women with one prior low transverse cesarean and women with unscarred uterus undergoing labor induction with PGE2: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0253957. [Google Scholar] [CrossRef]
- Guise, J.M.; McDonagh, M.S.; Osterweil, P.; Nygren, P.; Chan, B.K.S.; Helfand, M. Systematic review of the incidence and conse-quences of uterine rupture in women with previous caesarean section. Br. Med. J. 2004, 329, 19–23. [Google Scholar] [CrossRef] [Green Version]
- Al-Zirqi, I.; Stray-Pedersen, B.; Forsén, L.; Vangen, S. Uterine rupture after previous caesarean section. BJOG: Int. J. Obstet. Gynaecol. 2010, 117, 809–820. [Google Scholar] [CrossRef]
- Stone, J.; Lockwood, C.; Berkowitz, G.; Alvarez, M.; Lapinski, R.; Valcamonico, A.; Berkowitz, R. Use of Cervical Prostaglandin E2Gel in Patients with Previous Cesarean Section. Am. J. Perinatol. 1994, 11, 309–312. [Google Scholar] [CrossRef] [PubMed]
- Locatelli, A.; Ghidini, A.; Ciriello, E.; Incerti, M.; Bonardi, C.; Regalia, A.L. Induction of labor: Comparison of a cohort with uterine scar from previous cesarean section vs. a cohort with intact uterus. J. Matern. Neonatal Med. 2006, 19, 471–475. [Google Scholar] [CrossRef] [PubMed]
- Williams, M.A.; Luthy, D.A.; Zingheim, R.W.; Hickok, D.E. Preinduction Prostaglandin E2 Gel prior to Induction of Labor in Women with a Previous Cesarean Section. Gynecol. Obstet. Investig. 1995, 40, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Crowley, P. Contra-indications to Prostaglandin E2 Vaginal Gel: Evidence Based? J. SOGC 1996, 18, 1143–1152. [Google Scholar] [CrossRef]
- Dyack, C.; Hughes, P.F.; Simbakalia, J.B. Vaginal delivery in the grand multipara following previous lower segment cesarian section. J. Obstet. Gynaecol. Res. 1997, 23, 219–222. [Google Scholar] [CrossRef] [PubMed]
- Haas, J.; Barzilay, E.; Chayen, B.; Lebovitz, O.; Yinon, Y.; Mazaki-Tovi, S.; Harel, L. Safety of low-dose prostaglandin E2 induction in grandmultiparous women with previous cesarean delivery. J. Matern. Neonatal Med. 2013, 27, 445–448. [Google Scholar] [CrossRef]
| Variable | Previous Cesarean Delivery | p Value | |
|---|---|---|---|
| No | Yes | ||
| Maternal characteristics | |||
| Maternal age (years) * | 32.75 (5.05) | 34.21 (5.26) | 0.064 |
| Pregestational weight (kg) * | 69.01 (14.56) | 70.03 (13.99) | 0.649 |
| Antepartum weight (kg) * | 80.33 (15.03) | 80.01 (13.30) | 0.888 |
| Pregestational Body Mass Index (BMI) (kg/m2) * | 30.06 (5.27) | 29.81 (4.48) | 0.756 |
| Obstetrical characteristics | |||
| Previous cesarean delivery | |||
| Primiparity | 245 (65) | 35 (74.5) | 0.196 |
| Multiparity | 132 (35) | 12 (25.5) | |
| Preexisting or gestational diabetes | |||
| No | 342 (90.7) | 43 (91.5) | 0.049 |
| Preexisting diabetes | 3 (0.8) | 1 (2.1) | |
| Gestational diabetes | 32 (8.5) | 3 (6.4) | |
| Hypertensive disease of pregnancy | |||
| No | 343 (91) | 41 (87.2) | 0.449 |
| Chronic hypertension | 8 (2.1) | 0 (0) | |
| Gestational hypertension | 14 (3.7) | 4 (8.5) | |
| Preeclampsia | 11 (2.9) | 2 (4.3) | |
| Preeclampsia with severe features | 1 (0.3) | 0 (0) | |
| Intrauterine growth restriction (IUGR) | |||
| No | 357 (94.7) | 47 (100) | 0.106 |
| Yes | 20 (5.3) | 0 (0) | |
| Obstetrical management | |||
| Gestational age at birth (weeks) | |||
| <37 + 0 days | 13 (3.4) | 2 (4.3) | 0.890 |
| ≥37 + 0 days | 364 (96.6) | 45 (95.7) | |
| Cervical length prior to IOL, mm (CL) * | 27.7 (26.53) | 34 (29.19) | 0.116 |
| Prepartum amniotic fluid index (AFI) | |||
| Normal | 312 (82.8) | 36 (76.6) | 0.582 |
| Oligoamnios | 42 (11.1) | 7 (14.9) | |
| Hydramnios | 23 (6.1) | 4 (8.5) | |
| Bishop score upon admission * | 2.31 (1.55) | 2.08 (1.38) | 0.333 |
| Bishop score upon admission to labor * room | 5.76 (2.47) | 5.34 (2.54) | 0.264 |
| Indication for induction | |||
| Chronologically prolonged pregnancy | 121 (32.1) | 17 (36.2) | 0.869 |
| PROM | 85 (22.5) | 9 (19.1) | |
| Fetal | 92 (24.4) | 10 (21.3) | |
| Maternal | 79 (21.0) | 11 (23.4) | |
| Artificial rupture of membranes | |||
| No | 292 (77.5) | 38 (80.9) | 0.597 |
| Yes | 85 (22.5) | 9 (19.1) | |
| Oxytocin use | |||
| No | 90 (24.5) | 11 (23.4) | 0.866 |
| Yes | 277 (75.5) | 36 (76.6) | |
| Analgesia regional | |||
| No | 35 (9.3) | 1 (2.1) | 0.097 |
| Yes | 342 (90.7) | 46 (97.9) | |
| Total duration of IOL (minutes) * | 1236.38 (657.23) | 1335.08 (623.75) | 0.330 |
| Birth weight (kg) * | 3227.8 (498.3) | 3199.3 (441.7) | 0.709 |
| Variable | Previous Cesarean Delivery | Univariate Analysis | Multivariate Analysis ** | |||
|---|---|---|---|---|---|---|
| No | Yes | OR/MD 95% CI | p Value | OR/MD 95% CI | p Value | |
| Bishop score >6 after PGE2 | ||||||
| No | 165 (43.8) | 22 (46.8) | 0.88 (0.48, 1.62) | 0.692 | 1.14 (0.57, 2.31) | 0.706 |
| Yes | 212 (56.2) | 25 (53.2) | ||||
| Duration of dilatation (min) * | 359.93 (229.82) | 362.19 (216.52) | −2.26 (−72.80, 68.28) | 0.950 | −19.40 (−76.76, 37.96) | 0.506 |
| Duration third stage of labor (min) * | 94.22 (81.36) | 94.08 (60.81) | 0.15 (−32.82, 33.12) | 0.993 | 7.09 (−19.80, 34.17) | 0.606 |
| Type of delivery | ||||||
| Vaginal delivery | 258 (68.4) | 26 (55.3) | 1.75 (0.95, 3.24) | 0.074 | 1.40 (0.68, 2.86) | 0.358 |
| Cesarean delivery | 119 (31.6) | 21 (44.7) | ||||
| Meconium | ||||||
| No | 324 (85.9) | 40 (85.1) | 1.07 (0.45, 2.51) | 0.877 | 1.27 (0.52, 3.11) | 0.591 |
| Yes | 53 (14.1) | 7 (14.9) | ||||
| Intrapartum fever | ||||||
| No | 357 (94.9) | 44 (93.6) | 0.78 (0.22, 2.74) | 0.699 | 0.83 (0.22, 3.08) | 0.784 |
| Yes | 19 (5.1) | 3 (6.4) | ||||
| CTG 1: NICHD 2 2 | ||||||
| No | 253 (70.3) | 28 (65.1) | 1.27 (0.65, 2.47) | 0.487 | 1.07 (0.54, 2.13) | 0.844 |
| Yes | 107 (29.7) | 15 (34.9) | ||||
| CTG 1: NICHD 2 3 | ||||||
| No | 253 (70.3) | 28 (65.1) | 2.13 (0.67, 6.76) | 0.201 | 3.03 (0.87, 10.54) | 0.082 |
| Yes | 107 (29.7) | 15 (34.9) | ||||
| Postpartum hemorrhage a | ||||||
| No | 349 (93.3) | 42 (89.4) | 1.66 (0.60, 4.57) | 0.325 | 1.62 (0.56, 4.65) | 0.371 |
| Yes | 25 (6.7) | 5 (10.6) | ||||
| Uterine rupture b | ||||||
| No | 375 (100) | 45 (95.7) | ||||
| Yes | 0 (0) | 2 (4.3) | NC | 0.993 | NC | 0.979 |
| Blood loss > 3.5 (1) | ||||||
| No | 351 (94.4) | 47 (100) | NC | 0.997 | NC | 0.997 |
| Yes | 21 (5.6) | 0 (0) | ||||
| ICU 3 admission | ||||||
| No | 372 (99.5) | 47 (100) | 0 (NC) | 0.998 | 0 (NC) | 0.997 |
| Yes | 2 (0.5) | 0 (0) | ||||
| Need for transfusion | ||||||
| No | 362 (97.3) | 46 (97.9) | 0.78 (0.09, 6.29) | 0.821 | 0.67 (0.07, 6.06) | 0.721 |
| Yes | 10 (2.7) | 1 (2.1) | ||||
| Variable | Previous Cesarean | Univariate Analysis | Multivariate Analysis ** | |||
|---|---|---|---|---|---|---|
| No | Yes | OR 95% CI | p Value | OR 95% CI | p Value | |
| APGAR < 7 at 1 min | ||||||
| No | 367 (97.3) | 45 (95.7) | 1.63 (0.35, 7.68) | 0.536 | 1.25 (0.23, 6.76) | 0.799 |
| Yes | 10 (2.7) | 2 (4.3) | ||||
| APGAR < 7 at 5 min | ||||||
| No | 376 (99.7) | 46 (97.9) | 8.17 (0.50, 132.90) | 0.140 | NC | 0.999 |
| Yes | 1 (0.3) | 1 (2.1) | ||||
| Admission to neonatal unit | ||||||
| No | 337 (89.4) | 41 (87.2) | 0.81 (0.32, 2.03) | 0.655 | 0.90 (0.32, 2.53) | 0.844 |
| Yes | 40 (10.6) | 6 (12.8) | ||||
| REA III-IV | ||||||
| No | 370 (98.1) | 43 (91.5) | 4.92 (1.38, 17.48) | 0.014 | 3.91 (0.83, 18.36) | 0.084 |
| Yes | 7 (1.9) | 4 (8.5) | ||||
| U. artery pH < 7.20 at birth | ||||||
| No | 333 (91.7) | 35 (81.4) | 2.54 (1.08, 5.96) | 0.033 | 2.32 (0.91, 5.89) | 0.077 |
| Yes | 30 (8.3) | 8 (18.6) | ||||
| U. artery pH < 7.10 at birth | ||||||
| No | 362 (99.7) | 41 (95.3) | 17.66 (1.57, 199.00) | 0.020 | NC | 0.892 |
| Yes | 1 (0.3) | 2 (4.7) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
López-Jiménez, N.; García-Sánchez, F.; Pailos, R.H.; Rodrigo-Álvaro, V.; Pascual-Pedreño, A.; Moreno-Cid, M.; Hernández-Martínez, A.; Molina-Alarcón, M. Induction of Labor with Vaginal Dinoprostone (PGE2) in Patients with a Previous Cesarean Section: Obstetric and Neonatal Outcomes. J. Clin. Med. 2021, 10, 5221. https://doi.org/10.3390/jcm10225221
López-Jiménez N, García-Sánchez F, Pailos RH, Rodrigo-Álvaro V, Pascual-Pedreño A, Moreno-Cid M, Hernández-Martínez A, Molina-Alarcón M. Induction of Labor with Vaginal Dinoprostone (PGE2) in Patients with a Previous Cesarean Section: Obstetric and Neonatal Outcomes. Journal of Clinical Medicine. 2021; 10(22):5221. https://doi.org/10.3390/jcm10225221
Chicago/Turabian StyleLópez-Jiménez, Nuria, Fiamma García-Sánchez, Rafael Hernández Pailos, Valentin Rodrigo-Álvaro, Ana Pascual-Pedreño, María Moreno-Cid, Antonio Hernández-Martínez, and Milagros Molina-Alarcón. 2021. "Induction of Labor with Vaginal Dinoprostone (PGE2) in Patients with a Previous Cesarean Section: Obstetric and Neonatal Outcomes" Journal of Clinical Medicine 10, no. 22: 5221. https://doi.org/10.3390/jcm10225221
APA StyleLópez-Jiménez, N., García-Sánchez, F., Pailos, R. H., Rodrigo-Álvaro, V., Pascual-Pedreño, A., Moreno-Cid, M., Hernández-Martínez, A., & Molina-Alarcón, M. (2021). Induction of Labor with Vaginal Dinoprostone (PGE2) in Patients with a Previous Cesarean Section: Obstetric and Neonatal Outcomes. Journal of Clinical Medicine, 10(22), 5221. https://doi.org/10.3390/jcm10225221





