Does Additive Pressurized Carbon Dioxide Lavage Improve Cement Penetration and Bond Strength in Cemented Arthroplasty?
Abstract
:1. Introduction
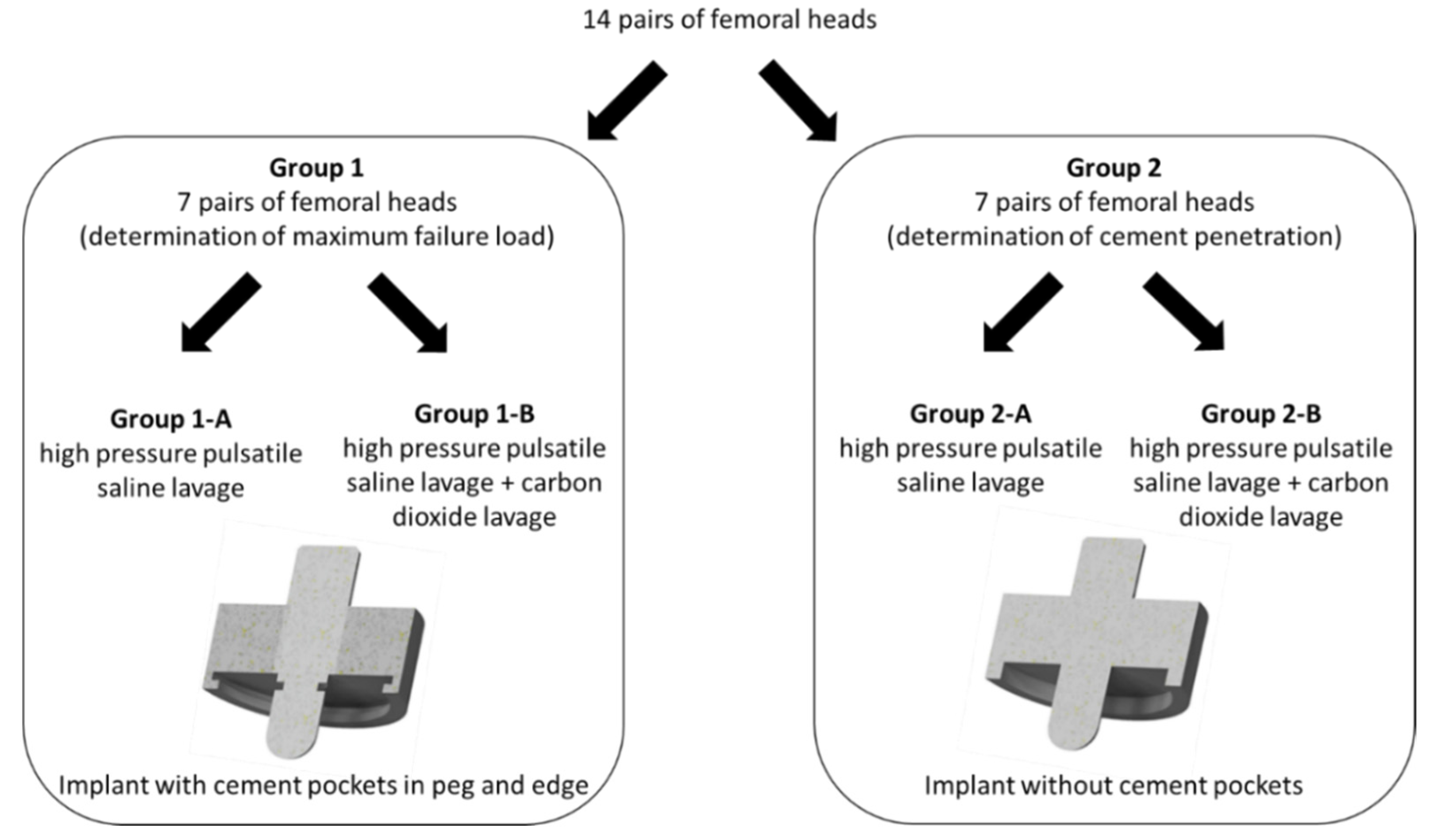
2. Materials and Methods
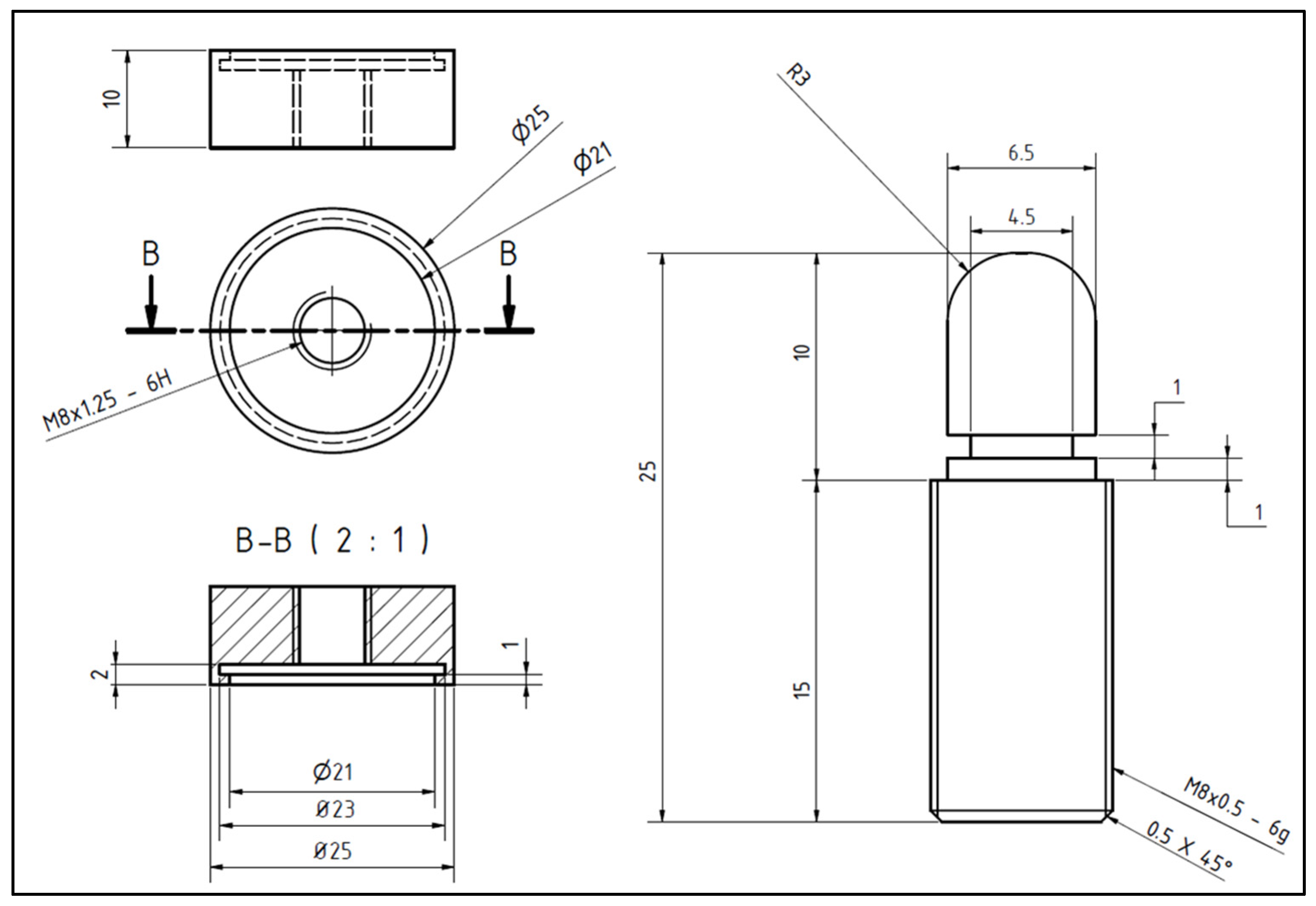
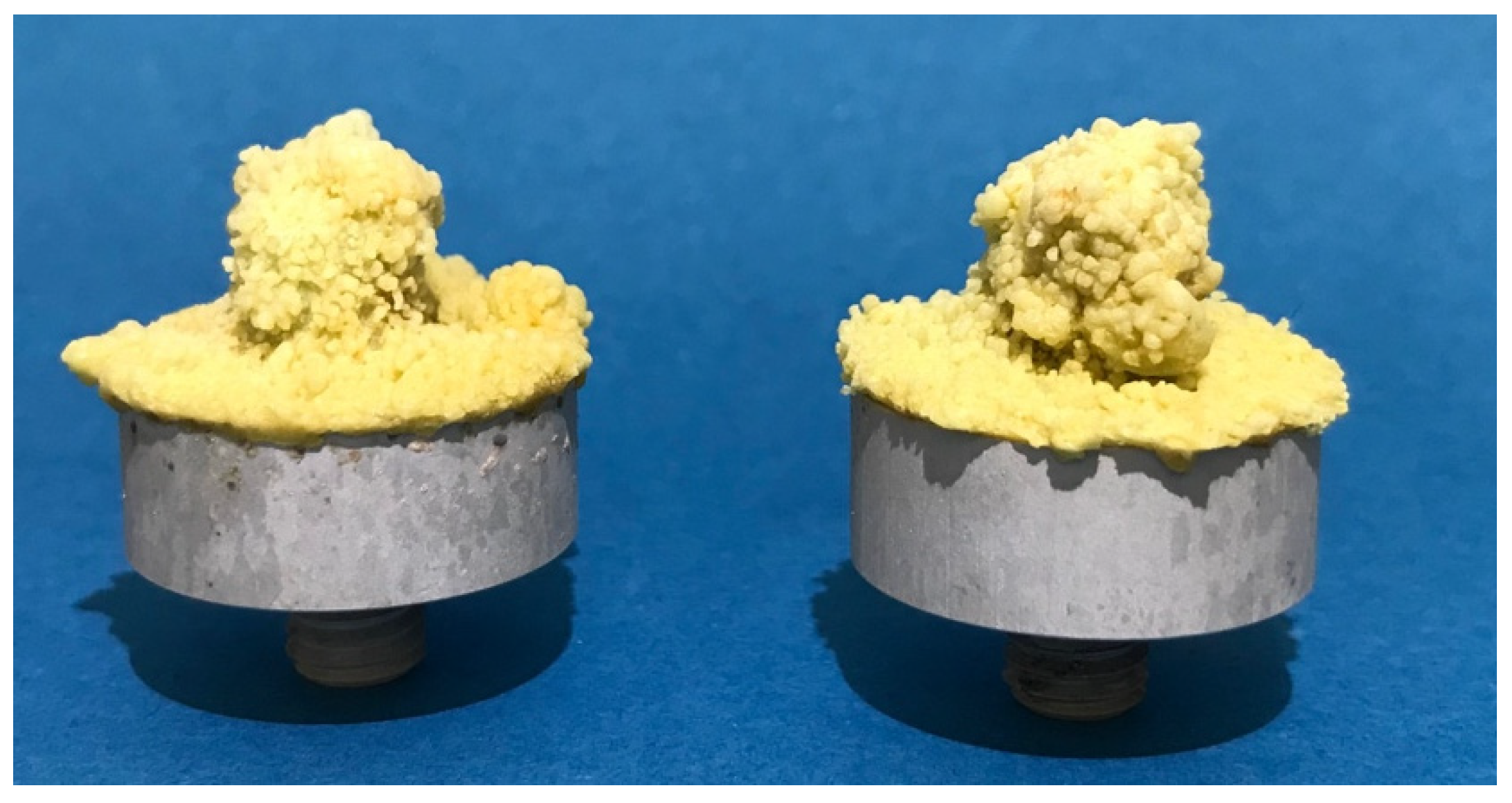
2.1. Test Setup and Preparations
2.2. Cancellous Bone Cleaning
2.3. Cementing Technique and Implantation of Test Implants
2.4. Determination of Maximum Failure Load
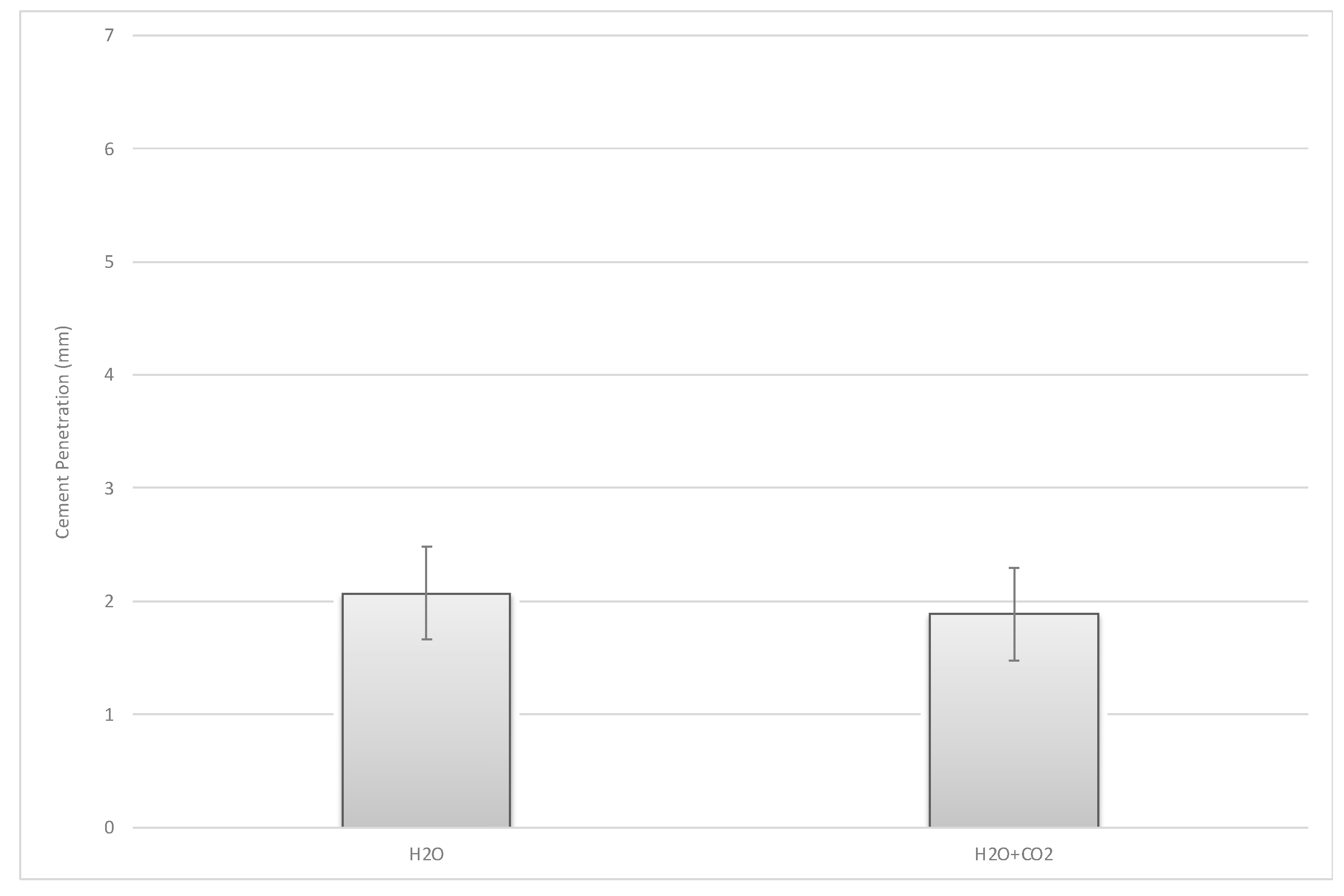
2.5. Cement Analysis/Cement Penetration
2.6. Statistics
3. Results
3.1. Bone Mineral Density
3.2. Group 1-Bond Strength of the Bone–Cement Interface
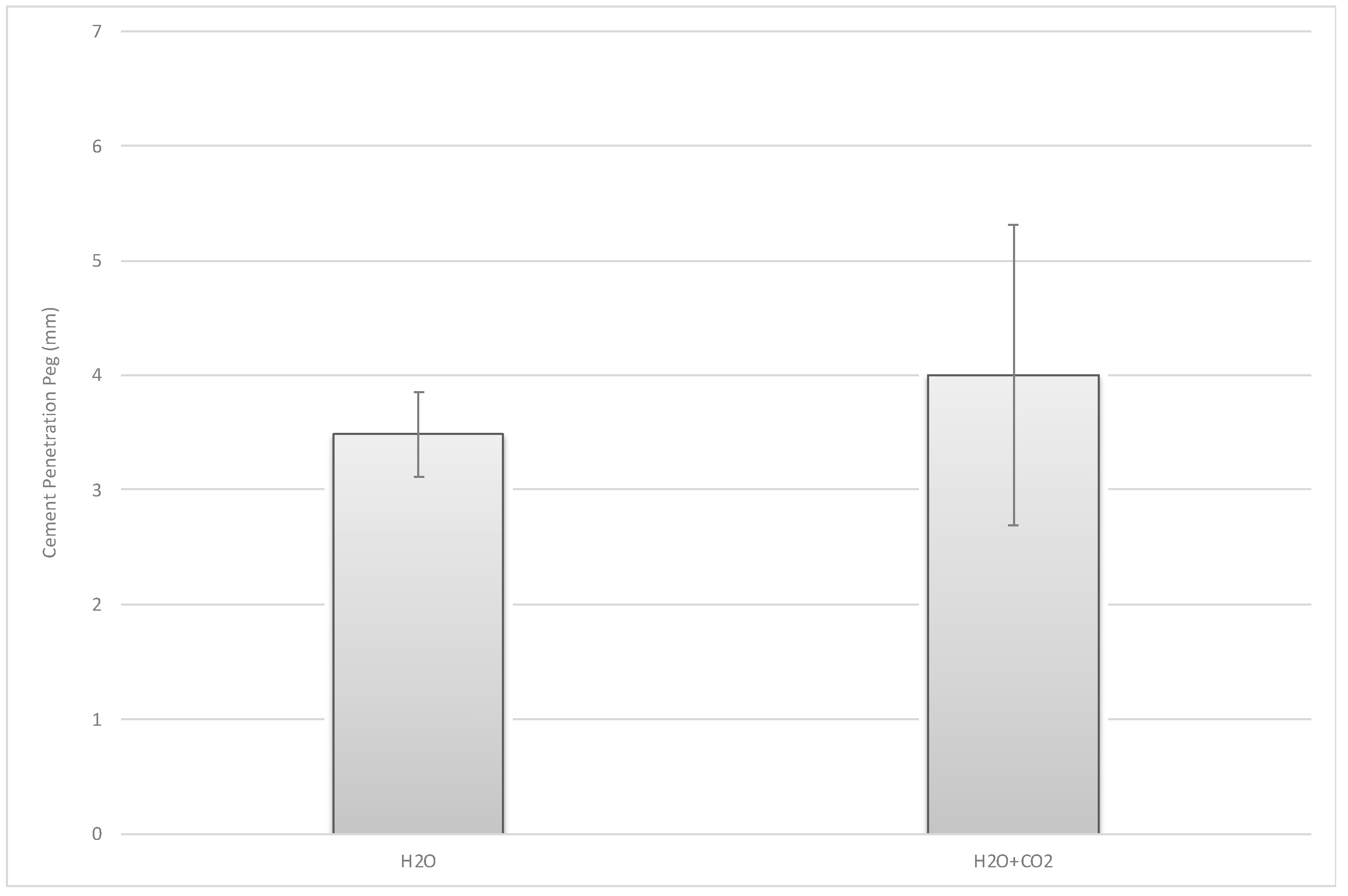
3.3. Group 2-Cement Penetration
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Klug, A.; Gramlich, Y.; Hoffmann, R.; Pfeil, J.; Drees, P.; Kutzner, K.P. Trends in Total Hip Arthroplasty in Germany from 2007 to 2016: What Has Changed and Where Are We Now? Z. Orthop. Unf. 2021, 159, 173–180. [Google Scholar] [CrossRef]
- Kim, Y.H.; Park, J.W.; Jang, Y.S. Long-Term Survival (up to 34 Years) of Retained Cementless Anatomic Femoral Stem in Patients < 50 Years Old. J. Arthroplast. 2021, 36, 1388–1392. [Google Scholar] [CrossRef]
- Schmolders, J.; Amvrazis, G.; Pennekamp, P.H.; Strauss, A.C.; Friedrich, M.J.; Wimmer, M.D.; Rommelspacher, Y.; Wirtz, D.C.; Wallny, T. Thirteen year follow-up of a cementless femoral stem and a threaded acetabular cup in patients younger than fifty years of age. Int. Orthop. 2017, 41, 39–45. [Google Scholar] [CrossRef]
- Kawamura, H.; Mishima, H.; Sugaya, H.; Nishino, T.; Shimizu, Y.; Miyakawa, S. The 21- to 27-year results of the Harris-Galante cementless total hip arthroplasty. J. Orthop. Sci. 2016, 21, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Dalury, D.F. Cementless total knee arthroplasty: Current concepts review. Bone Jt. J. 2016, 98, 867–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritter, M.A.; Keating, E.M.; Sueyoshi, T.; Davis, K.E.; Barrington, J.W.; Emerson, R.H. Twenty-Five-Years and Greater, Results After Nonmodular Cemented Total Knee Arthroplasty. J. Arthroplast. 2016, 31, 2199–2202. [Google Scholar] [CrossRef] [PubMed]
- Herberts, P.; Malchau, H. Long-term registration has improved the quality of hip replacement: A review of the Swedish THR Register comparing 160,000 cases. Acta Orthop. Scand. 2000, 71, 111–121. [Google Scholar] [CrossRef] [Green Version]
- Malchau, H.; Herberts, P.; Eisler, T.; Garellick, G.; Soderman, P. The Swedish Total Hip Replacement Register. J. Bone Jt. Surg. Am. 2002, 84, 2–20. [Google Scholar] [CrossRef]
- German Arthroplasty Registry (EPRD)-2019 Annual Report. 2019. Available online: https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/EPRD_Jahresbericht_2019_EN_doppelseitig_F_Web-Stand-251120.pdf (accessed on 17 November 2021). [CrossRef]
- The New Zealand Joint Registry—Fifteen-year report January 1999 to December 2013. 2014, Volume 15. Available online: https://www.nzoa.org.nz/sites/default/files/NZJR2014Report.pdf (accessed on 17 November 2021).
- Gademan, M.G.J.; Van Steenbergen, L.N.; Cannegieter, S.C.; Nelissen, R.; Marang-Van De Mheen, P.J. Population-based 10-year cumulative revision risks after hip and knee arthroplasty for osteoarthritis to inform patients in clinical practice: A competing risk analysis from the Dutch Arthroplasty Register. Acta Orthop. 2021, 92, 1–5. [Google Scholar] [CrossRef] [PubMed]
- The Swedish Knee Arthroplasty Register—Anual Report 2020. 2020. Available online: http://myknee.se/pdf/SVK_2020_Eng_1.0.pdf (accessed on 17 November 2021).
- Bunyoz, K.I.; Malchau, E.; Malchau, H.; Troelsen, A. Has the Use of Fixation Techniques in THA Changed in This Decade? The Uncemented Paradox Revisited. Clin. Orthop. Relat. Res. 2020, 478, 697–704. [Google Scholar] [CrossRef]
- Refsum, A.M.; Nguyen, U.V.; Gjertsen, J.E.; Espehaug, B.; Fenstad, A.M.; Lein, R.K.; Ellison, P.; Hol, P.J.; Furnes, O. Cementing technique for primary knee arthroplasty: A scoping review. Acta Orthop. 2019, 90, 582–589. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niculescu, M.; Solomon, B.L.; Viscopoleanu, G.; Antoniac, I.V. Evolution of Cementation Techniques and Bone Cements in Hip Arthroplasty. Handb. Bioceram. Biocompos. 2016, 859–899. [Google Scholar] [CrossRef]
- Khan, M.; Osman, K.; Green, G.; Haddad, F.S. The epidemiology of failure in total knee arthroplasty: Avoiding your next revision. Bone Jt. J. 2016, 98, 105–112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kochbati, R.; Rbai, H.; Jlailia, M.; Makhlouf, H.; Bouguira, A.; Daghfous, M.S. Predictive factors of aseptic loosening of cemented total hip prostheses. Pan Afr. Med. J. 2016, 24, 260. [Google Scholar] [CrossRef]
- Jaeger, S.; Rieger, J.S.; Bruckner, T.; Kretzer, J.P.; Clarius, M.; Bitsch, R.G. The protective effect of pulsed lavage against implant subsidence and micromotion for cemented tibial unicompartmental knee components: An experimental cadaver study. J. Arthroplast. 2014, 29, 727–732. [Google Scholar] [CrossRef]
- Benjamin, J.B.; Gie, G.A.; Lee, A.J.; Ling, R.S.; Volz, R.G. Cementing technique and the effects of bleeding. J. Bone Jt. Surg. Br. 1987, 69, 620–624. [Google Scholar] [CrossRef]
- Vanlommel, J.; Luyckx, J.P.; Labey, L.; Innocenti, B.; De Corte, R.; Bellemans, J. Cementing the tibial component in total knee arthroplasty: Which technique is the best? J. Arthroplast. 2011, 26, 492–496. [Google Scholar] [CrossRef]
- Cawley, D.T.; Kelly, N.; McGarry, J.P.; Shannon, F.J. Cementing techniques for the tibial component in primary total knee replacement. Bone Jt. J. 2013, 95, 295–300. [Google Scholar] [CrossRef]
- Sih, G.C.; Connelly, G.M.; Berman, A.T. The effect of thickness and pressure on the curing of PMMA bone cement for the total hip joint replacement. J. Biomech. 1980, 13, 347–352. [Google Scholar] [CrossRef]
- Hampton, C.B.; Berliner, Z.P.; Nguyen, J.T.; Mendez, L.; Smith, S.S.; Joseph, A.D.; Padgett, D.E.; Rodriguez, J.A. Aseptic Loosening at the Tibia in Total Knee Arthroplasty: A Function of Cement Mantle Quality? J. Arthroplast. 2020, 35, S190–S196. [Google Scholar] [CrossRef] [PubMed]
- Fischer, C.A.; Kaszap, B.; Drexler, C.; Lehner, B.; Clarius, M. Cemented total hip arthroplasty in Germany—Update 2010. Z Orthop. Unf. 2012, 150, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Clarius, M.; Hauck, C.; Seeger, J.B.; James, A.; Murray, D.W.; Aldinger, P.R. Pulsed lavage reduces the incidence of radiolucent lines under the tibial tray of Oxford unicompartmental knee arthroplasty: Pulsed lavage versus syringe lavage. Int. Orthop. 2009, 33, 1585–1590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breusch, S.J.; Norman, T.L.; Schneider, U.; Reitzel, T.; Blaha, J.D.; Lukoschek, M. Lavage technique in total hip arthroplasty: Jet lavage produces better cement penetration than syringe lavage in the proximal femur. J. Arthroplast. 2000, 15, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Seeger, J.B.; Jaeger, S.; Bitsch, R.G.; Mohr, G.; Rohner, E.; Clarius, M. The effect of bone lavage on femoral cement penetration and interface temperature during Oxford unicompartmental knee arthroplasty with cement. J. Bone Jt. Surg. Am. 2013, 95, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Helwig, P.; Konstantinidis, L.; Hirschmuller, A.; Miltenberger, V.; Kuminack, K.; Sudkamp, N.P.; Hauschild, O. Tibial cleaning method for cemented total knee arthroplasty: An experimental study. Indian J. Orthop. 2013, 47, 18–22. [Google Scholar] [CrossRef]
- Kalteis, T.; Pforringer, D.; Herold, T.; Handel, M.; Renkawitz, T.; Plitz, W. An experimental comparison of different devices for pulsatile high-pressure lavage and their relevance to cement intrusion into cancellous bone. Arch. Orthop. Trauma Surg. 2007, 127, 873–877. [Google Scholar] [CrossRef] [PubMed]
- Ritter, M.A.; Herbst, S.A.; Keating, E.M.; Faris, P.M. Radiolucency at the bone-cement interface in total knee replacement. The effects of bone-surface preparation and cement technique. J. Bone Jt. Surg. Am. 1994, 76, 60–65. [Google Scholar] [CrossRef]
- Goldstein, W.M.; Gordon, A.; Goldstein, J.M.; Berland, K.; Branson, J.; Sarin, V.K. Improfement of Cement mantle thickness with pressurized carbon dioxide lavage. In Proceedings of the 20th Annual Meeting of the International Society for Technology in Arthroplasty, Paris, France, 3–6 October 2007. [Google Scholar]
- Gapinski, Z.A.; Yee, E.J.; Kraus, K.R.; Deckard, E.R.; Meneghini, R.M. The Effect of Tourniquet Use and Sterile Carbon Dioxide Gas Bone Preparation on Cement Penetration in Primary Total Knee Arthroplasty. J. Arthroplast. 2019, 34, 1634–1639. [Google Scholar] [CrossRef]
- Boontanapibul, K.; Ruangsomboon, P.; Charoencholvanich, K.; Pornrattanamaneewong, C. Effectiveness Testing of Combined Innovative Pressurized Carbon Dioxide Lavage and Pulsatile Normal Saline Irrigation to Enhance Bone Cement Penetration in Total Knee Replacement: A Cadaveric Study. J. Med. Assoc. Thai. 2016, 99, 1198–1202. [Google Scholar]
- Ravenscroft, M.J.; Charalambous, C.P.; Mills, S.P.; Woodruff, M.J.; Stanley, J.K. Bone-cement interface strength in distal radii using two medullary canal preparation techniques: Carbon dioxide jet cleaning versus syringed saline. Hand Surg. 2010, 15, 95–98. [Google Scholar] [CrossRef]
- Knappe, K.; Stadler, C.; Innmann, M.; Schonhoff, M.; Gotterbarm, T.; Renkawitz, T.; Jaeger, S. Does Pressurized Carbon Dioxide Lavage Improve Bone Cleaning in Cemented Arthroplasty? Appl. Sci. 2021, 11, 6103. [Google Scholar] [CrossRef]
- Martinez, M.R.G.; Ruiz, G.M.V.; Perez, J.M.R.; Perez, R.L. Air embolism after cleaning the intramedullary canal with a high pressure CO2 wash in hip fracture. Rev. Esp. Anestesiol. Reanim. 2013, 60, 353–354. [Google Scholar] [CrossRef]
- Lax-Prez, R.; Ferrero-Manzanal, F.; Marin-Penia, O.; Murcia-Asensio, A. Gas embolism after the use of the CarboJet lavage system during hip hemiarthroplasty. Clinical case and literature review. Acta Ortop. Mex. 2014, 28, 45–48. [Google Scholar]
- Clarius, M.; Seeger, J.B.; Jaeger, S.; Mohr, G.; Bitsch, R.G. The importance of pulsed lavage on interface temperature and ligament tension force in cemented unicompartmental knee arthroplasty. Clin. Biomech. 2012, 27, 372–376. [Google Scholar] [CrossRef] [PubMed]
- Schwarze, M.; Schonhoff, M.; Beckmann, N.A.; Eckert, J.A.; Bitsch, R.G.; Jager, S. Femoral Cementation in Knee Arthroplasty—A Comparison of Three Cementing Techniques in a Sawbone Model Using the ATTUNE Knee. J. Knee Surg. 2021, 34, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Yushkevich, P.A.; Piven, J.; Hazlett, H.C.; Smith, R.G.; Ho, S.; Gee, J.C.; Gerig, G. User-guided 3D active contour segmentation of anatomical structures: Significantly improved efficiency and reliability. Neuroimage 2006, 31, 1116–1128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G * Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- German Arthroplasty Registry (EPRD)—2021 Annual Report. 2021. Available online: https://www.eprd.de/fileadmin/user_upload/Dateien/Publikationen/Berichte/Jahresbericht2021_2021-10-25_F.pdf (accessed on 17 November 2021). [CrossRef]
- Watts, N.; Adger, W.N.; Ayeb-Karlsson, S.; Bai, Y.; Byass, P.; Campbell-Lendrum, D.; Colbourn, T.; Cox, P.; Davies, M.; Depledge, M.; et al. The Lancet Countdown: Tracking progress on health and climate change. Lancet 2017, 389, 1151–1164. [Google Scholar] [CrossRef] [Green Version]
- Thiel, C.L.; Eckelman, M.; Guido, R.; Huddleston, M.; Landis, A.E.; Sherman, J.; Shrake, S.O.; Copley-Woods, N.; Bilec, M.M. Environmental impacts of surgical procedures: Life cycle assessment of hysterectomy in the United States. Environ. Sci. Technol. 2015, 49, 1779–1786. [Google Scholar] [CrossRef]
- Rizan, C.; Steinbach, I.; Nicholson, R.; Lillywhite, R.; Reed, M.; Bhutta, M.F. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann. Surg. 2020, 272, 986–995. [Google Scholar] [CrossRef]
- Hanada, M.; Hotta, K.; Furuhashi, H.; Matsuyama, Y. Intraoperative bacterial contamination in total hip and knee arthroplasty is associated with operative duration and peeling of the iodine-containing drape from skin. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Ravi, B.; Jenkinson, R.; O’Heireamhoin, S.; Austin, P.C.; Aktar, S.; Leroux, T.S.; Paterson, M.; Redelmeier, D.A. Surgical duration is associated with an increased risk of periprosthetic infection following total knee arthroplasty: A population-based retrospective cohort study. EClinicalMedicine 2019, 16, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Teo, B.J.X.; Yeo, W.; Chong, H.C.; Tan, A.H.C. Surgical site infection after primary total knee arthroplasty is associated with a longer duration of surgery. J. Orthop. Surg. (Hong Kong) 2018, 26, 2309499018785647. [Google Scholar] [CrossRef] [Green Version]
- Held, M.B.; Boddapati, V.; Sarpong, N.O.; Cooper, H.J.; Shah, R.P.; Geller, J.A. Operative Duration and Short-Term Postoperative Complications after Unicompartmental Knee Arthroplasty. J. Arthroplast. 2021, 36, 905–909. [Google Scholar] [CrossRef] [PubMed]
- Orland, M.D.; Lee, R.Y.; Naami, E.E.; Patetta, M.J.; Hussain, A.K.; Gonzalez, M.H. Surgical Duration Implicated in Major Postoperative Complications in Total Hip and Total Knee Arthroplasty: A Retrospective Cohort Study. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2020, 4, e20 00043. [Google Scholar] [CrossRef] [PubMed]
- Zweymuller, K.A. Bony ongrowth on the surface of HA-coated femoral implants: An X-ray analysis. Z. Orthop. Unf. 2012, 150, 27–31. [Google Scholar] [CrossRef]
- Robertson, D.M.; Pierre, L.; Chahal, R. Preliminary observations of bone ingrowth into porous materials. J. Biomed. Mater. Res. 1976, 10, 335–344. [Google Scholar] [CrossRef]
- Albrektsson, T.; Johansson, C. Osteoinduction, osteoconduction and osseointegration. Eur. Spine J. 2001, 10, S96–S101. [Google Scholar] [CrossRef] [Green Version]
- Hu, C.; Ashok, D.; Nisbet, D.R.; Gautam, V. Bioinspired surface modification of orthopedic implants for bone tissue engineering. Biomaterials 2019, 219, 119366. [Google Scholar] [CrossRef]






Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knappe, K.; Stadler, C.; Innmann, M.M.; Schonhoff, M.; Gotterbarm, T.; Renkawitz, T.; Jaeger, S. Does Additive Pressurized Carbon Dioxide Lavage Improve Cement Penetration and Bond Strength in Cemented Arthroplasty? J. Clin. Med. 2021, 10, 5361. https://doi.org/10.3390/jcm10225361
Knappe K, Stadler C, Innmann MM, Schonhoff M, Gotterbarm T, Renkawitz T, Jaeger S. Does Additive Pressurized Carbon Dioxide Lavage Improve Cement Penetration and Bond Strength in Cemented Arthroplasty? Journal of Clinical Medicine. 2021; 10(22):5361. https://doi.org/10.3390/jcm10225361
Chicago/Turabian StyleKnappe, Kevin, Christian Stadler, Moritz M. Innmann, Mareike Schonhoff, Tobias Gotterbarm, Tobias Renkawitz, and Sebastian Jaeger. 2021. "Does Additive Pressurized Carbon Dioxide Lavage Improve Cement Penetration and Bond Strength in Cemented Arthroplasty?" Journal of Clinical Medicine 10, no. 22: 5361. https://doi.org/10.3390/jcm10225361
APA StyleKnappe, K., Stadler, C., Innmann, M. M., Schonhoff, M., Gotterbarm, T., Renkawitz, T., & Jaeger, S. (2021). Does Additive Pressurized Carbon Dioxide Lavage Improve Cement Penetration and Bond Strength in Cemented Arthroplasty? Journal of Clinical Medicine, 10(22), 5361. https://doi.org/10.3390/jcm10225361





