Prognostic Role of Subclinical Congestion in Heart Failure Outpatients: Focus on Right Ventricular Dysfunction
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Physical Examination and Ultrasound Analysis
2.3. Outcome Data
2.4. Statistical Analysis
3. Results
3.1. Population
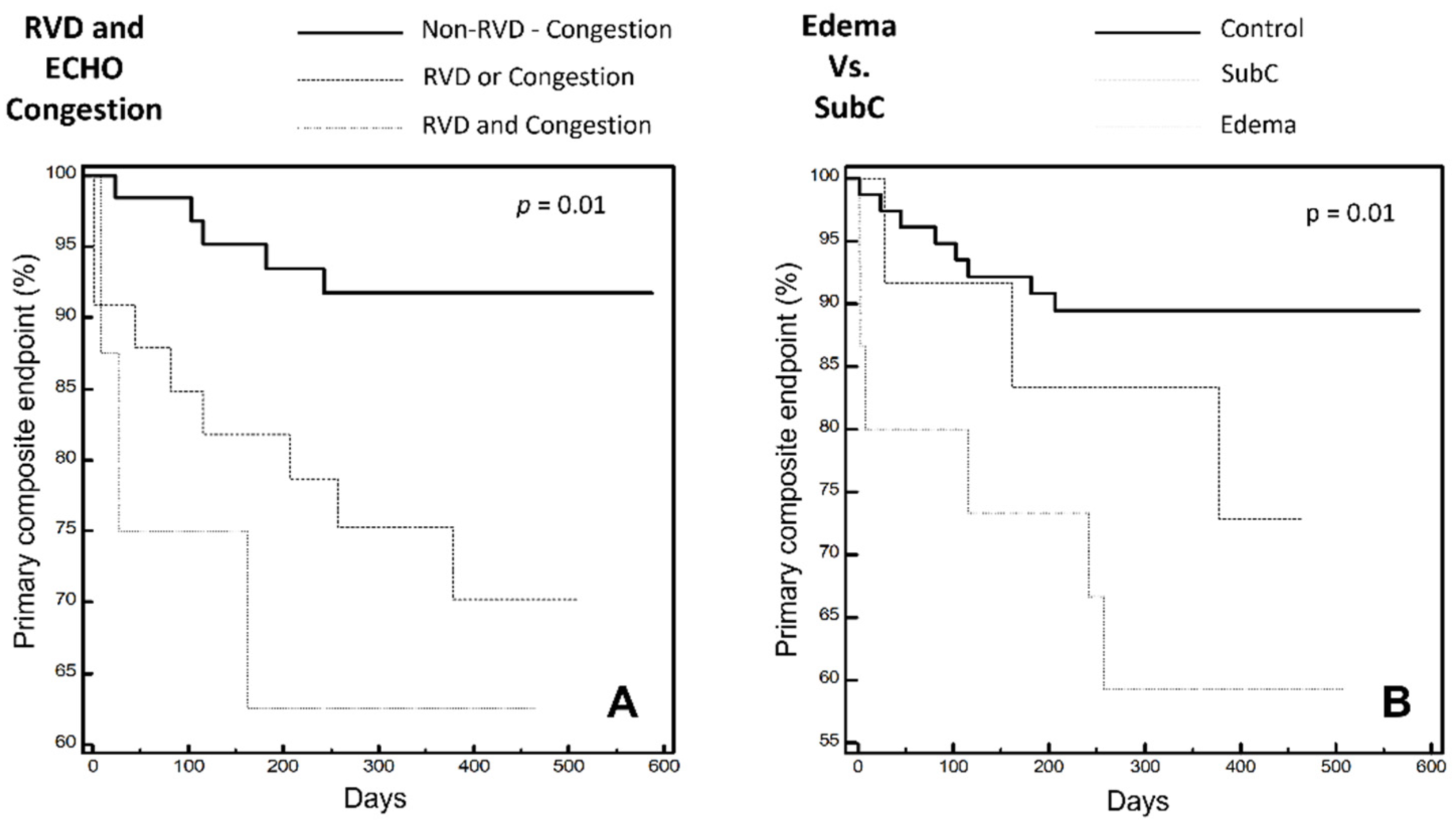
- (1)
- “Control” group, i.e., patients without clinical signs of peripheral edema nor US estimated RAP ≥ 13 mmHg;
- (2)
- “SubC” (Sub Clinical Congestion) Group i.e., patients with US estimated RAP ≥ 13 mmHg without peripheral edema;
- (3)
- “Edema” group i.e., patients with peripheral edema irrespective of US findings.
3.2. Patient Characteristics
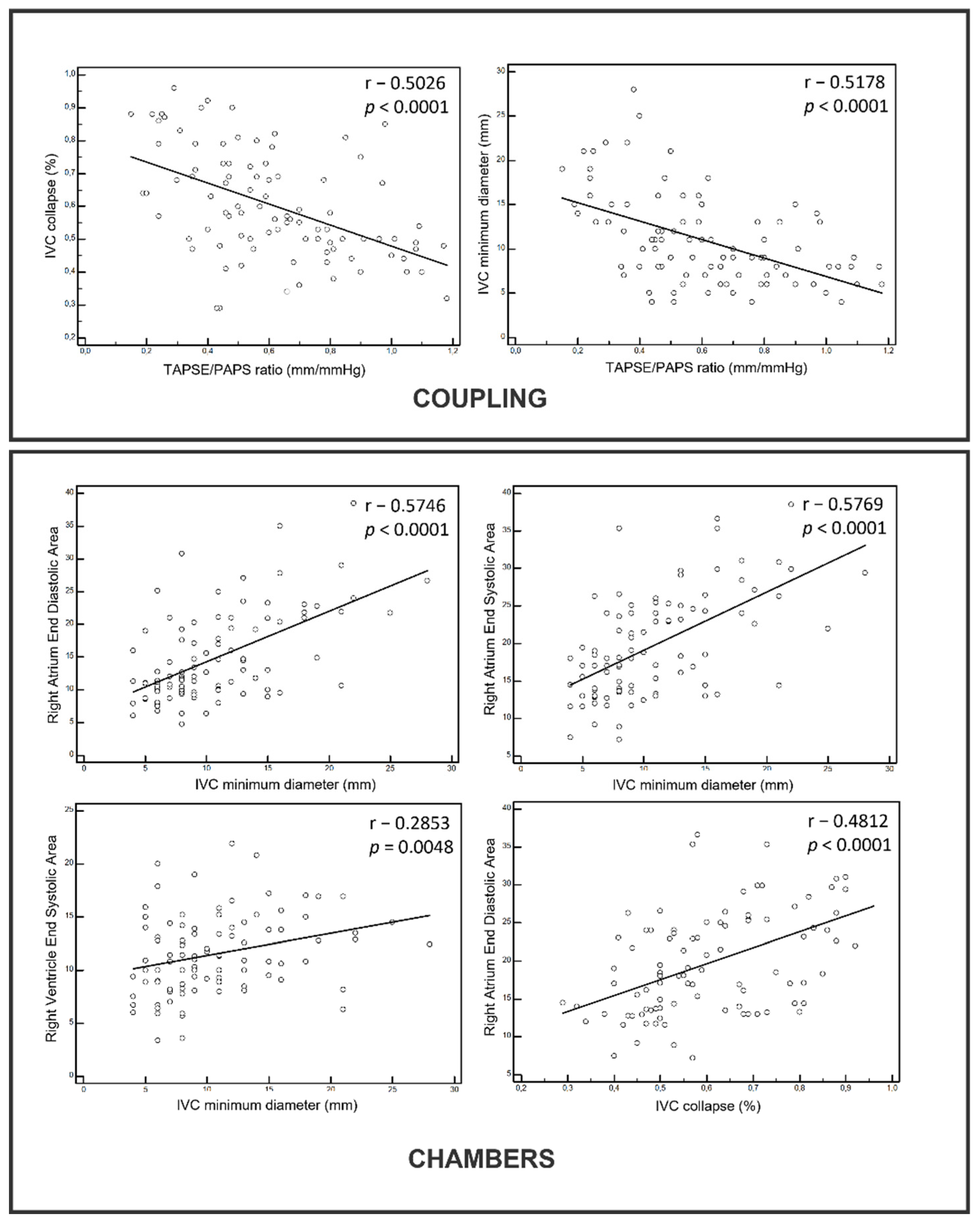
3.3. Physical Examination and Ultrasound Analysis
3.4. Outcome Data
4. Discussion
5. Conclusions
6. Limits
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bozkurt, B.; Coats, A.J.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart Fail. 2021, 23, 352–380. [Google Scholar] [CrossRef]
- Lucas, C.; Johnson, W.; Hamilton, M.A.; Fonarow, G.; Woo, M.A.; Flavell, C.M.; Creaser, J.A.; Stevenson, L.W. Freedom from congestion predicts good survival despite previous class IV symptoms of heart failure. Am. Heart J. 2000, 140, 840–847. [Google Scholar] [CrossRef]
- Pellicori, P.; Cleland, J.G.F.; Zhang, J.; Kallvikbacka-Bennett, A.; Urbinati, A.; Shah, P.; Kazmi, S.; Clark, A.L. Cardiac Dysfunction, Congestion and Loop Diuretics: Their Relationship to Prognosis in Heart Failure. Cardiovasc. Drugs Ther. 2016, 30, 599–609. [Google Scholar] [CrossRef] [Green Version]
- Thibodeau, J.; Drazner, M.H. The Role of the Clinical Examination in Patients with Heart Failure. JACC Heart Fail. 2018, 6, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Curbelo, J.; Aguilera, M.; Rodriguez-Cortes, P.; Gil-Martinez, P.; Fernández, C.S. Usefulness of inferior vena cava ultrasonography in outpatients with chronic heart failure. Clin. Cardiol. 2018, 41, 510–517. [Google Scholar] [CrossRef]
- Öhman, J.; Harjola, V.-P.; Karjalainen, P.; Lassus, J. Assessment of early treatment response by rapid cardiothoracic ultrasound in acute heart failure: Cardiac filling pressures, pulmonary congestion and mortality. Eur. Heart J.-Acute Cardiovasc. Care 2018, 7, 311–320. [Google Scholar] [CrossRef]
- Platz, E.; Merz, A.; Jhund, P.; Vazir, A.; Campbell, R.; Mcmurray, J. Dynamic changes and prognostic value of pulmonary congestion by lung ultrasound in acute and chronic heart failure: A systematic review. Eur. J. Heart Fail. 2017, 19, 1154–1163. [Google Scholar] [CrossRef] [PubMed]
- Maggioni, A.P. Epidemiology of Heart Failure in Europe. Heart Fail. Clin. 2015, 11, 625–635. [Google Scholar] [CrossRef] [PubMed]
- Chioncel, O.; Lainscak, M.; Seferovic, P.M.; Anker, S.D.; Crespo-Leiro, M.G.; Harjola, V.-P.; Parissis, J.; Laroche, C.; Piepoli, M.F.; Fonseca, C.; et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: An analysis of the ESC Heart Failure Long-Term Registry. Eur. J. Heart Fail. 2017, 19, 1574–1585. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Fonarow, G.C.; Greene, S.J.; DeVore, A.D.; Kavati, A.; Sikirica, S.; Albert, N.M.; Duffy, C.I.; Hill, C.L.; Patterson, J.H.; et al. Contemporary Treatment Patterns and Clinical Outcomes of Comorbid Diabetes Mellitus and HFrEF: The CHAMP-HF Registry. JACC Heart Fail. 2020, 8, 469–480. [Google Scholar] [CrossRef]
- Obokata, M.; Reddy, Y.N.V.; Melenovsky, V.; Pislaru, S.; Borlaug, B.A. Deterioration in right ventricular structure and function over time in patients with heart failure and preserved ejection fraction. Eur. Heart J. 2019, 40, 689–697. [Google Scholar] [CrossRef] [Green Version]
- Pellicori, P.; Carubelli, V.; Zhang, J.; Castiello, T.; Sherwi, N.; Clark, A.L.; Cleland, J.G. IVC diameter in patients with chronic heart failure: Relationships and prognostic significance. JACC Cardiovasc. Imaging 2013, 6, 16–28. [Google Scholar] [CrossRef]
- Pellicori, P.; Shah, P.; Cuthbert, J.; Urbinati, A.; Zhang, J.; Kallvikbacka-Bennett, A.; Clark, A.L.; Cleland, J.G. Prevalence, pattern and clinical relevance of ultrasound indices of congestion in outpatients with heart failure. Eur. J. Heart Fail. 2019, 21, 904–916. [Google Scholar] [CrossRef]
- Pham, D.D.; Drazner, M.H.; Ayers, C.R.; Grodin, J.L.; Hardin, E.A.; Garg, S.; Mammen, P.P.A.; Amin, A.; Araj, F.G.; Morlend, R.M.; et al. Identifying Discordance of Right- and Left-Ventricular Filling Pressures in Patients With Heart Failure by the Clinical Examination. Circ. Heart Fail. 2021, 14, e008779. [Google Scholar] [CrossRef]
- Yavaşi, Ö.; Ünlüer, E.E.; Kayayurt, K.; Ekinci, S.; Sağlam, C.; Sürüm, N.; Köseoğlu, M.H.; Yeşil, M. Monitoring the response to treatment of acute heart failure patients by ultrasonographic inferior vena cava collapsibility index. Am. J. Emerg. Med. 2014, 32, 403–407. [Google Scholar] [CrossRef] [PubMed]
- Mueller, C.; McDonald, K.; de Boer, R.A.; Maisel, A.; Cleland, J.G.; Kozhuharov, N.; Coats, A.J.; Metra, M.; Mebazaa, A.; Ruschitzka, F.; et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur. J. Heart Fail. 2019, 21, 715–731. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Curbelo, J.; Rodriguez-Cortes, P.; Aguilera, M.; Gil-Martinez, P.; Martín, D.; Fernandez, C.S. Comparison between inferior vena cava ultrasound, lung ultrasound, bioelectric impedance analysis, and natriuretic peptides in chronic heart failure. Curr. Med Res. Opin. 2019, 35, 705–713. [Google Scholar] [CrossRef]
- Lindenfeld, J.; Zile, M.R.; Desai, A.S.; Bhatt, K.; Ducharme, A.; Horstmanshof, D.; Krim, S.R.; Maisel, A.; Mehra, M.R.; Paul, S.; et al. Haemodynamic-guided management of heart failure (GUIDE-HF): A randomised controlled trial. Lancet 2021, 398, 991–1001. [Google Scholar] [CrossRef]
- Khan, A.; Khan, D.; Shadi, M.; MacDougall, K.; Lafferty, J. Utilization of Ultrasound to Assess Volume Status in Heart Failure. J. Clin. Med. Res. 2020, 12, 230–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pellicori, P.; Platz, E.; Dauw, J.; ter Maaten, J.M.; Martens, P.; Pivetta, E.; Cleland, J.G.; McMurray, J.J.; Mullens, W.; Solomon, S.D.; et al. Ultrasound imaging of congestion in heart failure: Examinations beyond the heart. Eur. J. Heart Fail. 2021, 23, 703–712. [Google Scholar] [CrossRef]
- Schmeißer, A.; Rauwolf, T.; Groscheck, T.; Fischbach, K.; Kropf, S.; Luani, B.; Tanev, I.; Hansen, M.; Meißler, S.; Schäfer, K.; et al. Predictors and prognosis of right ventricular function in pulmonary hypertension due to heart failure with reduced ejection fraction. ESC Heart Fail. 2021, 8, 2968–2981. [Google Scholar] [CrossRef] [PubMed]
- Ghio, S.; Guazzi, M.; Scardovi, A.B.; Klersy, C.; Clemenza, F.; Carluccio, E.; Temporelli, P.L.; Rossi, A.; Faggiano, P.; Traversi, E.; et al. Different correlates but similar prognostic implications for right ventricular dysfunction in heart failure patients with reduced or preserved ejection fraction. Eur. J. Heart Fail. 2017, 19, 873–879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gorter, T.M.; Hoendermis, E.S.; Van Veldhuisen, D.J.; Voors, A.A.; Lam, C.S.P.; Geelhoed, B.; Willems, T.P.; Van Melle, J.P. Right ventricular dysfunction in heart failure with preserved ejection fraction: A systematic review and meta-analysis. Eur. J. Heart Fail. 2016, 18, 1472–1487. [Google Scholar] [CrossRef] [PubMed]
- Gorter, T.M.; Van Veldhuisen, D.J.; Voors, A.A.; Hummel, Y.M.; Lam, C.S.; Berger, R.M.; Van Melle, J.P.; Hoendermis, E.S. Right ventricular-vascular coupling in heart failure with preserved ejection fraction and pre- vs. post-capillary pulmonary hypertension. Eur. Heart J.-Cardiovasc. Imaging 2017, 19, 425–432. [Google Scholar] [CrossRef]

| Population Characteristics | Total Pop (n 104) | Control (n 77) | SubC (n 12) | Edema (n 15) | p-Value |
|---|---|---|---|---|---|
| Sex (male) | 72 (69%) | 54 (70%) | 9 (75%) | 9 (60%) | ns |
| Age (years) | 73 ± 11 | 70 ± 11 | 75 ± 11 | 81 ± 4 | <0.01 # |
| Weight (Kg) | 76 ± 15 | 76 ± 15 | 77 ± 21 | 74 ± 14 | ns |
| Height (cm) | 170 ± 9 | 170 ± 9 | 171 ± 6 | 170 ± 11 | ns |
| BMI (Kg/m2) | 26 ± 4 | 26 ± 4 | 26.4 ±7.0 | 25.5 ±3.3 | ns |
| BSA (m2) | 1.86 ± 0.20 | 1.86 ± 0.21 | 1.89 ±0.21 | 1.85 ±0.22 | ns |
| NYHA class | <0.001 | ||||
| I | 29 (28%) | 25 (32%) | 3 (25%) | 1 (7%) | |
| II | 54 (52%) | 44 (57%) | 5 (42%) | 5 (33%) | |
| III | 20 (19%) | 8 (10%) | 4 (33%) | 8 (53%) | |
| IV | 1 (1%) | 0 (0%) | 0 (0%) | 1 (7%) | |
| LVEF < 40% | 44 (42%) | 34 (44%) | 5 (42%) | 5 (33%) | ns |
| Etiology | <0.01 | ||||
| Ischemic | 35 (34%) | 24 (31%) | 5 (42%) | 6 (40%) | |
| Valvular | 13 (12%) | 6 (8%) | 2 (17%) | 5 (33%) | |
| Idiopathic | 38 (37%) | 36 (47%) | 2 (17%) | 0 (0%) | |
| Miscellaneous | 18 (17%) | 11 (14%) | 3 (25%) | 4 (27%) | |
| Months since HF diagnosis | 45 (16–106) | 49 (19–107) | 16 (7–81) | 19 (15–61) | ns |
| Comorbidities | |||||
| Stroke in past | 5 (5%) | 4 (5%) | 1 (8%) | 0 (0%) | ns |
| Previous cardiac surgery | 15 (14%) | 13 (17%) | 0 (0%) | 2 (13%) | ns |
| Previous mitral valve repair or clip | 9 (8%) | 6 (8%) | 2 (17%) | 1 (7%) | ns |
| Diabetes | 26 (25%) | 19 (25%) | 3 (25%) | 4 (27%) | ns |
| History of cancer | 16 (15%) | 10 (13%) | 3 (25%) | 3 (20%) | ns |
| Hypertension | 71 (68%) | 49 (64%) | 10 (83%) | 12 (80%) | ns |
| Peripheral artery disease | 5 (5%) | 4 (5%) | 0 (0%) | 1 (7%) | ns |
| History of atrial fibrillation | 43 (42%) | 24 (31%) | 7 (58%) | 12 (80%) | <0.001 |
| Permanent atrial fibrillation | 25 (24%) | 12 (16%) | 5 (42%) | 8 (53%) | <0.001 |
| Therapy | |||||
| ACEi | 68 (65%) | 50 (65%) | 7 (58%) | 11 (73%) | ns |
| ARB | 14 (13%) | 10 (13%) | 3 (25%) | 1 (7%) | ns |
| BetaB | 96 (91%) | 72 (94%) | 12 (100%) | 12 (80%) | ns |
| Ivabradine | 12 (11%) | 11 (14%) | 1 (8%) | 0 (0%) | ns |
| Digoxin | 5 (5%) | 3 (4%) | 1 (8%) | 1 (7%) | ns |
| MRA | 48 (46%) | 34 (44%) | 7 (58%) | 7 (47%) | ns |
| NTG | 7 (7%) | 5 (6%) | 2 (17%) | 0 (0%) | ns |
| Warfarin | 34 (33%) | 18 (23%) | 6 (50%) | 10 (67%) | <0.001 |
| NOACs | 9 (8%) | 4 (5%) | 2 (17%) | 3 (20%) | <0.05 |
| Statins | 53 (50%) | 42 (55%) | 7 (58%) | 4 (27%) | ns |
| Furosemide | 83 (80%) | 59 (77%) | 10 (83%) | 14 (93%) | ns |
| Amiodarone | 24 (23%) | 17 (22%) | 2 (17%) | 5 (33%) | ns |
| ARNI | 9 (8%) | 7 (9%) | 1 (8%) | 1 (7%) | ns |
| ICD | 34 (32%) | 30 39%) | 2 (17%) | 2 (13%) | ns |
| CRT | 9 (8%) | 8 (10%) | 1 (8%) | 0 (0%) | ns |
| Population Characteristics | Total Pop (n 104) | Control (n 77) | SubC (n 12) | Edema (n 15) | p-Value |
|---|---|---|---|---|---|
| Blood tests | |||||
| Hematocrit (%) | 41.3 (39.1–43.9) | 41.2 (39.1–44.0) | 41.2 (39.0–43.8) | 41.0 (38.9–43.5) | ns |
| Hemoglobin (g/dL) | 13.7 (12.7–14.6) | 13.7 (12.7–14.6) | 13.2 ± 1.7 | 11.9 (11.3–13.5) | <0.01 |
| Creatinine (mg/dL) | 1.2 (1.0–1.5) | 1.2 (1.0–1.5) | 1.2 (1.1 -1.3) | 1.4 (1.1–1.6) | ns |
| eGFR MDRD (mL/min/1.73 m2) | 57 (46–73) | 58 (47–77) | 56 (48–65) | 55 (46–66) | ns |
| NTproBNP pg/mL | 944 (237–1755) | 716 (192–1548) | 1361 (764–2172) | 2116 (1111–4945) | ns |
| Sodium (mEq/L) | 141 (139–143) | 141 (140–143) | 142 (141–143) | 141 (138–144) | ns |
| Potassium (mEq/L) | 4.5 (4.2–4.9) | 4.5 (4.2–4.8) | 4.5 (4.4–4.8) | 4.5 (4.3–4.9) | ns |
| Population Characteristics | Total Pop (n 104) | Control (n 77) | SubC (n 12) | Edema (n 15) | p-Value |
|---|---|---|---|---|---|
| Vital signs | |||||
| Heart rate (bpm) | 69 ± 13 | 70 ± 12 | 69 ± 10 | 69 ± 16 | ns |
| Systolic blood pressure | 127 ± 17 | 129 ± 16 | 123 ± 13 | 125 ± 21 | ns |
| Diastolic blood pressure | 75 ± 10 | 76 ± 10 | 72 ± 7 | 74 ± 12 | ns |
| Physical examination | |||||
| Pulmonary congestion | 8 (8%) | 1 (1%) | 2 (17%) | 5 (33%) | <0.001 |
| Peripheral congestion | 15 (14%) | 0 (0%) | 0 (0%) | 15 (100%) | <0.001 |
| Elevated CVP | 30 (29%) | 11 (14%) | 6 (50%) | 13 (87%) | <0.001 |
| Ultrasound parameters | |||||
| LVEF (%) | 40 ± 11 | 40 ± 11 | 40 ± 12 | 42 ± 13 | |
| TAPSE (mm) | 20 ± 5 | 21 ± 5 | 18 ± 7 | 18 ± 6 | <0.05 |
| PAPS (mmHg) | 35 ± 11 | 26 ± 5 | 47 ± 14 | 47 ± 11 | <0.001 * |
| TAPSE/PAPS | 0.63 ± 0.26 | 0.71 ± 0.23 | 0.43 ± 0.24 | 0.40 ± 0.16 | <0.001 * |
| S’VD (cm/sec) | 10.6 ± 2.8 | 11.0 ± 2.7 | 8.9 ± 3.2 | 10.0 ± 3.1 | = 0.05 |
| RV end-diastolic area (cm2) | 19.1 ± 4.6 | 18.7 ± 5.0 | 20.1 ± 3.8 | 20.0 ± 2.6 | ns |
| RV end-systolic area (cm2) | 11.5 ± 3.7 | 10.9 ± 3.7 | 13.4 ± 4.0 | 13.0 ± 2.5 | < 0.05 # |
| RV FAC | 0.40 ± 0.13 | 45 ± 13 | 33 ± 16 | 35 ± 11 | <0.05 |
| RA end-diastolic area (cm2) | 14.8 ± 6.7 | 12.4 ± 4.5 | 20.5 ± 8.9 | 21.5 ± 7.0 | 0.001 * |
| RA end-systolic area (cm2) | 19.6 ± 6.8 | 17.4 ± 5.1 | 24.8 ± 8.5 | 25.7 ± 6.9 | 0.001 * |
| IVC Min (mm) | 11 ± 5 | 8 ± 3 | 19 ± 4 | 22 ± 5 | <0.001 ° |
| IVC Max (mm) | 17 ± 5 | 15 ± 4 | 24 ± 3 | 16 ± 4 | <0.001 * |
| IVC collapse (%) | 40 ± 16 | 45 ± 13 | 22 ± 12 | 25 ± 11 | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vecchi, A.L.; Muccioli, S.; Marazzato, J.; Mancinelli, A.; Iacovoni, A.; De Ponti, R. Prognostic Role of Subclinical Congestion in Heart Failure Outpatients: Focus on Right Ventricular Dysfunction. J. Clin. Med. 2021, 10, 5423. https://doi.org/10.3390/jcm10225423
Vecchi AL, Muccioli S, Marazzato J, Mancinelli A, Iacovoni A, De Ponti R. Prognostic Role of Subclinical Congestion in Heart Failure Outpatients: Focus on Right Ventricular Dysfunction. Journal of Clinical Medicine. 2021; 10(22):5423. https://doi.org/10.3390/jcm10225423
Chicago/Turabian StyleVecchi, Andrea Lorenzo, Silvia Muccioli, Jacopo Marazzato, Antonella Mancinelli, Attilio Iacovoni, and Roberto De Ponti. 2021. "Prognostic Role of Subclinical Congestion in Heart Failure Outpatients: Focus on Right Ventricular Dysfunction" Journal of Clinical Medicine 10, no. 22: 5423. https://doi.org/10.3390/jcm10225423
APA StyleVecchi, A. L., Muccioli, S., Marazzato, J., Mancinelli, A., Iacovoni, A., & De Ponti, R. (2021). Prognostic Role of Subclinical Congestion in Heart Failure Outpatients: Focus on Right Ventricular Dysfunction. Journal of Clinical Medicine, 10(22), 5423. https://doi.org/10.3390/jcm10225423







