Predictive Modeling of Poor Outcome in Severe COVID-19: A Single-Center Observational Study Based on Clinical, Cytokine and Laboratory Profiles
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Subjects
2.2. Biological Samples
2.3. Blood Types
2.4. Variables
2.5. Cytokine and Chemokine Analysis
2.6. Hospital Protocol Treatment
2.7. Statistical Analysis
3. Results
3.1. Presenting Characteristics
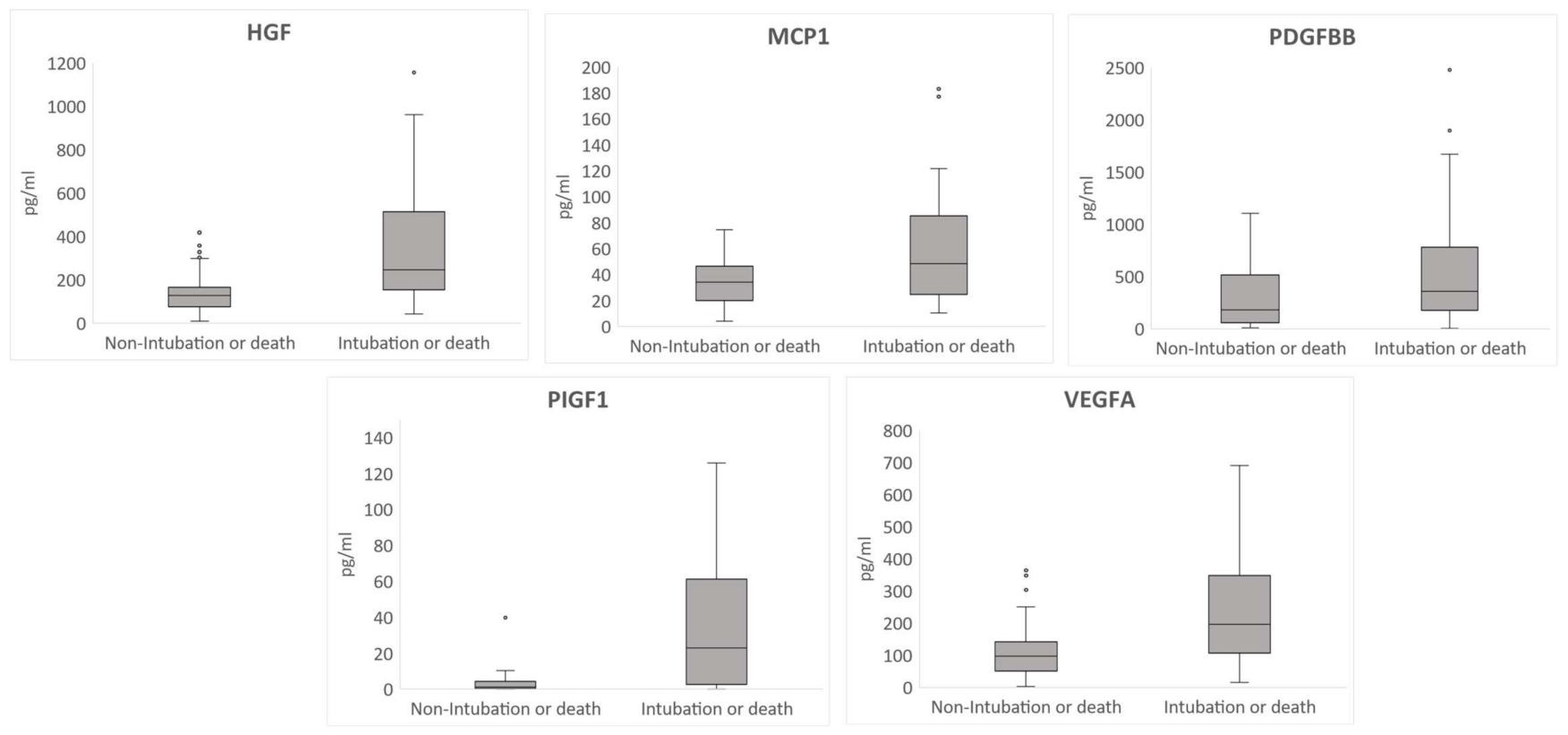
3.2. Cytokine Profile Comparison
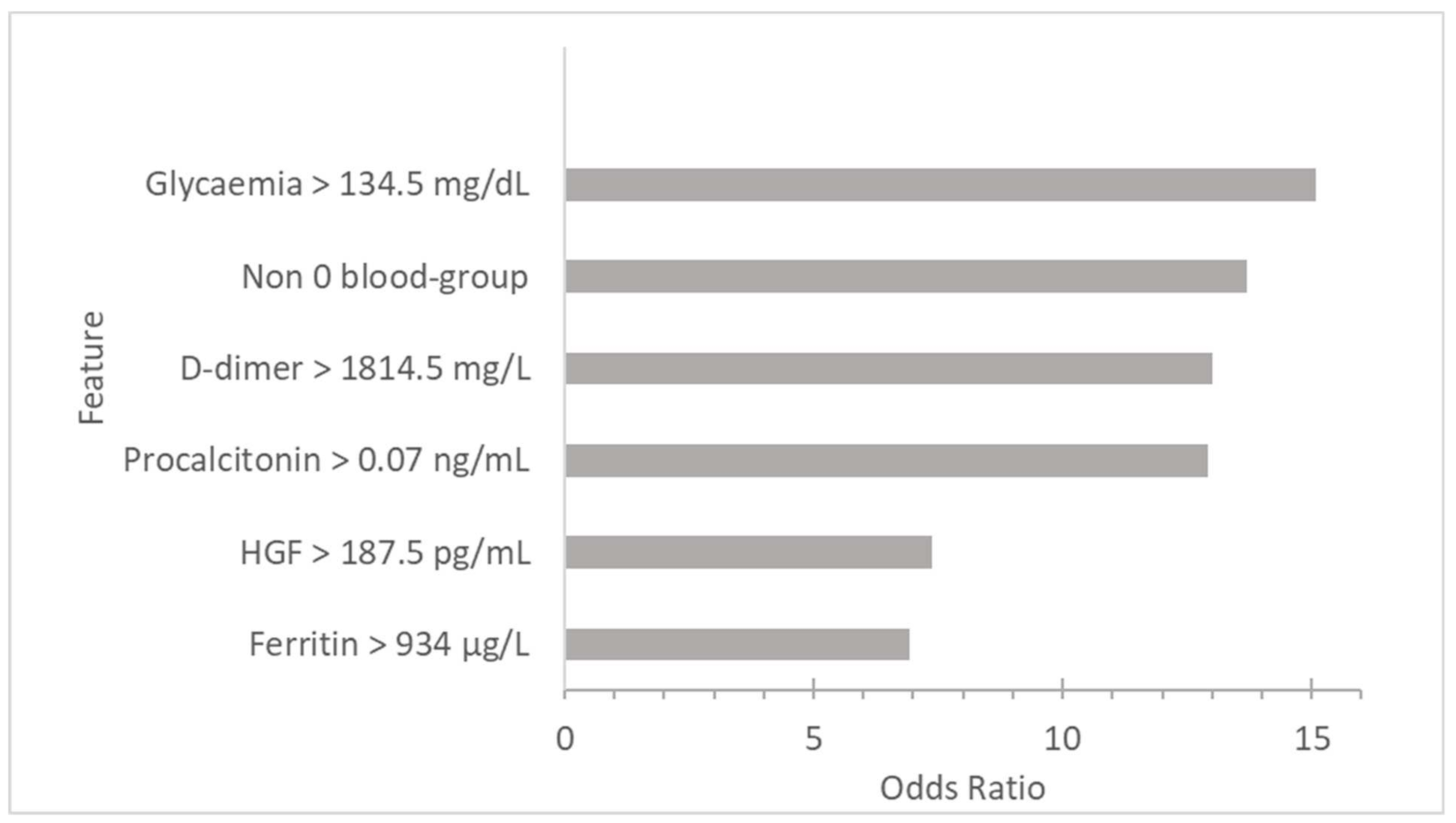
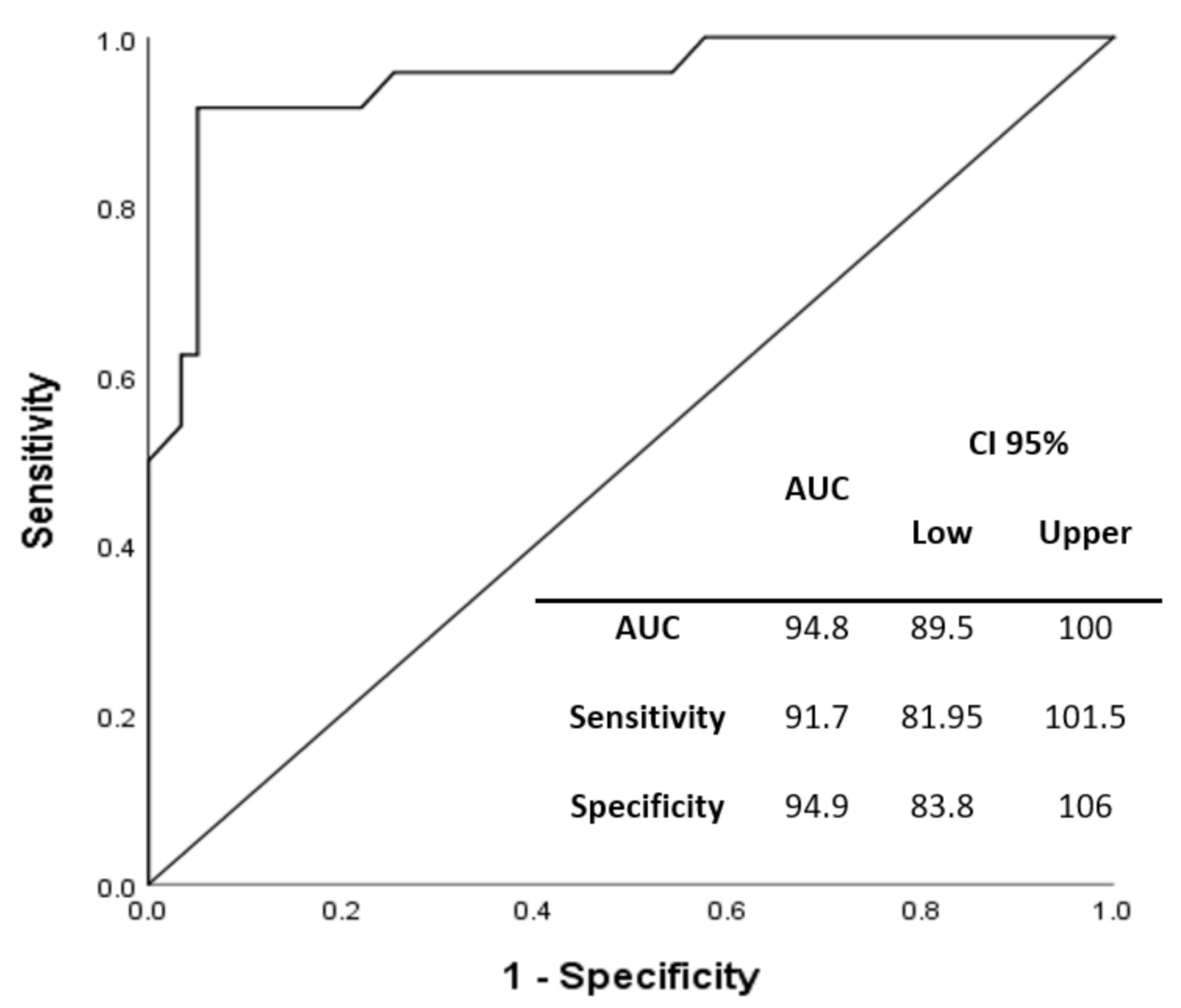
3.3. Risk Factors Associated with Poor Outcomes (Intubation or Death) in Hospitalized Patients with COVID-19
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Epidemiology Working Group for NCIP Epidemic Response CC for DC and P. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2020, 41, 145–151. [Google Scholar] [CrossRef]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; Yu, T.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Yu, T.; Tong, Y.; Ren, R.; Leung, K.S.M. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Zheng, X.; Zhao, C.; Peng, S.; Jian, S.; Liang, B.; Wang, X.; Yang, S.; Wang, C.; Peng, H.; Wang, Y. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis. J. Infect. 2020, 81, e16–25. [Google Scholar] [CrossRef]
- Ejaz, H.; Alsrhani, A.; Zafar, A.; Javed, H.; Junaid, K.; Abdalla, A.E.; Abosalif, K.O.; Ahmed, Z.; Younas, S. COVID-19 and comorbidities: Deleterious impact on infected patients. J. Infect. Public Health 2020, 13, 1833–1839. [Google Scholar] [CrossRef]
- Huang, I.; Pranata, R.; Lim, M.A.; Oehadian, A.; Alisjahbana, B. C-reactive protein, procalcitonin, D-dimer, and ferritin in severe coronavirus disease-2019: A meta-analysis. Ther. Adv. Respir. Dis. 2020, 14. [Google Scholar] [CrossRef]
- Zhao, J.; Yang, Y.; Huang, H.; Li, D.; Gu, D.; Lu, X.; Zhang, Z.; Liu, L.; Liu, T.; Liu, Y.; et al. Relationship Between the ABO Blood Group and the Coronavirus Disease 2019 (COVID-19) Susceptibility. Clin. Infect. Dis. 2020, 73, 328–331. [Google Scholar] [CrossRef]
- Liu, N.; Zhang, T.; Ma, L.; Zhang, H.; Wang, H.; Wei, W.; Pei, H.; Hao, L.I. The impact of ABO blood group on COVID-19 infection risk and mortality: A systematic review and meta-analysis. Blood Rev. 2021, 48, 100785. [Google Scholar] [CrossRef]
- Wu, B.-B.; Gu, D.-Z.; Yu, J.-N.; Yang, J.; Shen, W.-Q. Association between ABO blood groups and COVID-19 infection, severity and demise: A systematic review and meta-analysis. Infect. Genet. Evol. 2020, 84, 104485. [Google Scholar] [CrossRef]
- Golinelli, D.; Boetto, E.; Maietti, E.; Fantini, M.P. The association between ABO blood group and SARS-CoV-2 infection: A meta-analysis. PLoS ONE 2020, 15, e0239508. [Google Scholar] [CrossRef]
- Tamayo-Velasco, Á.; Martınez-Paz, P.; Peñarrubia-Ponce, M.J.; de la Fuente, I.; Pérez-Gonz ález, S.; Fernández, I.; Dueñas, C.; Gómez-Sánchez, E.; Lorenzo-López, M.; Gómez-Pesquera, E. HGF, IL-1α, and IL-27 Are Robust Biomarkers in Early Severity Stratification of COVID-19 Patients. J. Clin. Med. 2021, 10, 2017. [Google Scholar] [CrossRef]
- Tamayo-Velasco, Á.; Peñarrubia Ponce, M.J.; Álvarez, F.J.; Gonzalo-Benito, H.; de la Fuente, I.; Pérez-González, S.; Rico, L.; Jiménez García, M.T.; Sánchez Rodríguez, A.; Hijas Villaizan, M.; et al. Can the Cytokine Profile According to ABO Blood Groups Be Related to Worse Outcome in COVID-19 Patients? Yes, They Can. Front. Immunol. 2021, 12, 1–10. [Google Scholar] [CrossRef]
- Salama, C.; Han, J.; Yau, L.; Reiss, W.G.; Kramer, B.; Neidhart, J.D.; Criner, G.J.; Lewis, E.K.; Baden, R.; Pandit, L. Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N. Engl. J. Med. 2021, 384, 20–30. [Google Scholar] [CrossRef] [PubMed]
- Mariette, X.; Hermine, O.; Resche-Rigon, M.; Porcher, R.; Ravaud, P.; Bureau, S. Effect of anakinra versus usual care in adults in hospital with COVID-19 and mild-to-moderate pneumonia (CORIMUNO-ANA-1): A randomised controlled trial. Lancet Respir. Med. 2021, 9, 295–304. [Google Scholar] [CrossRef]
- Park, C.L.; Russell, B.S.; Fendrich, M.; Finkelstein-Fox, L.; Hutchison, M.; Becker, J. Americans’ COVID-19 Stress, Coping, and Adherence to CDC Guidelines. J. Gen. Intern. Med. 2020, 35, 2296–2303. [Google Scholar] [CrossRef]
- Hu, B.; Huang, S.; Yin, L. The cytokine storm and COVID-19. J. Med. Virol. 2021, 93, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.K.; Khan, M.A.; Singh, S.K. Constitutive Inflammatory Cytokine Storm: A Major Threat to Human Health. J. Interferon Cytokine Res. 2020, 40, 19–23. [Google Scholar] [CrossRef]
- Wen, W.; Su, W.; Tang, H.; Le, W.; Zhang, X.; Zheng, Y.; Liu, X.; Xie, L.; Li, J.; Ye, J.; et al. Immune cell profiling of COVID-19 patients in the recovery stage by single-cell sequencing. Cell Discov. 2020, 6, 1–18. [Google Scholar] [CrossRef]
- Chen, G.; Wu, D.; Guo, W.; Cao, Y.; Huang, D.; Wang, H.; Wang, T.; Zhang, X.; Chen, H.; Yu, H.; et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Invest. 2020, 130, 2620–2629. [Google Scholar] [CrossRef] [Green Version]
- Zhang, B.; Zhou, X.; Zhu, C.; Song, Y.; Feng, F.; Qiu, Y.; Feng, J.; Jia, Q.; Song, Q.; Zhu, B.; et al. Immune Phenotyping Based on the Neutrophil-to-Lymphocyte Ratio and IgG Level Predicts Disease Severity and Outcome for Patients with COVID-19. Front. Mol. Biosci. 2020, 7, 157. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.B.; Xu, C.; Zhang, R.B.; Wu, M.; Pan, C.K.; Li, X.J.; Wang, Q.; Zeng, F.F.; Zhu, S. Associations of procalcitonin, C-reaction protein and neutrophil-to-lymphocyte ratio with mortality in hospitalized COVID-19 patients in China. Sci. Rep. 2020, 10, 1–10. [Google Scholar] [CrossRef]
- Borges, L.; Pithon-Curi, T.C.; Curi, R.; Hatanaka, E. COVID-19 and Neutrophils: The Relationship between Hyperinflammation and Neutrophil Extracellular Traps. Mediat. Inflamm. 2020, 2020, 8829674. [Google Scholar] [CrossRef] [PubMed]
- Quartuccio, L.; Fabris, M.; Sonaglia, A.; Peghin, M.; Domenis, R.; Cifù, A.; Curcio, F.; Tascini, C. Interleukin 6, soluble interleukin 2 receptor alpha (CD25), monocyte colony-stimulating factor, and hepatocyte growth factor linked with systemic hyperinflammation, innate immunity hyperactivation, and organ damage in COVID-19 pneumonia. Cytokine 2021, 140. [Google Scholar] [CrossRef]
- Yang, Y.; Shen, C.; Li, J.; Yuan, J.; Yang, M.; Wang, F.; Li, G.; Li, Y.; Xing, L.; Peng, L.; et al. Plasma IP-10 and MCP-3 levels are highly associated with disease severity and predict the progression of COVID-19. J. Allergy Clin. Immunol. 2020, 146, 119–127. [Google Scholar] [CrossRef]
- Meizlish, M.L.; Pine, A.B.; Bishai, J.D.; Goshua, G.; Nadelmann, E.R.; Simonov, M.; Chang, C.H.; Zhang, H.; Shallow, M.; Bahel, P. A neutrophil activation signature predicts critical illness and mortality in COVID-19. MedRxiv Prepr. Serv. Health Sci. 2020, 5, 1164–1167. [Google Scholar] [CrossRef]
- Wiersinga, W.J.; Rhodes, A.; Cheng, A.C.; Peacock, S.J.; Prescott, H.C. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 2020, 324, 782–793. [Google Scholar] [CrossRef] [PubMed]
- Cooling, L. Blood Groups in Infection and Host Susceptibility. Clin. Microbiol. Rev. 2015, 28, 801–870. [Google Scholar] [CrossRef] [Green Version]
- Guillon, P.; Clément, M.; Sébille, V.; Rivain, J.G.; Chou, C.F.; Ruvoën-Clouet, N. Inhibition of the interaction between the SARS-CoV Spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology 2008, 18, 1085–1093. [Google Scholar] [CrossRef] [Green Version]
- Hoiland, R.L.; Fergusson, N.A.; Mitra, A.R.; Griesdale, D.E.; Devine, D.V.; Stukas, S.; Cooper, J.; Thiara, S.; Foster, D.; Chen, L.Y.; et al. The association of ABO blood group with indices of disease severity and multiorgan dysfunction in COVID-19. Blood Adv. 2020, 4, 4981–4989. [Google Scholar] [CrossRef]
- Amundadottir, L.; Kraft, P.; Stolzenberg-Solomon, R.Z.; Fuchs, C.S.; Petersen, G.M.; Arslan, A.A.; Bueno-de-Mesquita, H.B.; Gross, M.; Helzlsouer, K.; Jacobs, E.J.; et al. Genome-wide association study identifies variants in the ABO locus associated with susceptibility to pancreatic cancer. Nat. Genet. 2009, 41, 986–990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caricchio, R.; Gallucci, M.; Dass, C.; Zhang, X.; Gallucci, S.; Fleece, D. Preliminary predictive criteria for COVID-19 cytokine storm. Ann. Rheum. Dis. 2021, 80, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Tampe, D.; Winkler, M.S.; Korsten, P.; Hakroush, S.; Moerer, O.; Tampe, B. Response to: ‘Correspondence on “Preliminary predictive criteria for COVID-19 cytokine storm”’ by Tampe et al. Ann. Rheum. Dis. 2021. [Google Scholar] [CrossRef] [PubMed]
| Intubation or Death (n = 40) | Non-Intubation or Death (n = 68) | p | |
|---|---|---|---|
| Age. Years (median (IQR)) | 72.5 (15.25) | 72.5 (16.75) | 0.195 |
| Male (n (%)) | 22 (55) | 37 (54.4) | 0.953 |
| -Blood group (n (%)) | |||
| O Blood group | 8 (20) | 27 (39.7) | 0.035 |
| -Comorbidities (n (%)) | |||
| Smoking | 4 (10) | 5 (7.4) | 0.631 |
| Coronary disease | 4 (10) | 6 (8.8) | 0.839 |
| Atrial fibrillation | 5 (12.5) | 7 (10.3) | 0.725 |
| Diabetes | 1 (2.5) | 0 (0) | 0.190 |
| Neurological disease | 1 (2.5) | 1 (1.5) | 0.702 |
| Stroke | 0 (0) | 1 (1.5) | 0.441 |
| Hypertension | 20 (50) | 30 (44.1) | 0.554 |
| Liver disease | 2 (5) | 0 (0) | 0.063 |
| Obesity | 7 (17.5) | 3 (4.4) | 0.023 |
| COPD | 3 (7.5) | 4 (5.9) | 0.742 |
| Kidney disease | 2 (5) | 1 (1.5) | 0.281 |
| -Laboratory (median (IQR)) | |||
| Glycaemia (mg/dL) | 174.5 (103.75) | 96 (35) | <0.001 |
| Creatine (mg/dL) | 0.9 (0.56) | 0.81 (0.21) | 0.042 |
| Total bilirubin (mg/dL) | 0.5 (0.57) | 0.5 (0.3) | 0.292 |
| Leukocytes (×109/L) | 7.87 (7.83) | 6.12 (3.45) | 0.001 |
| Lymphocytes (×109/L) | 605 (552.5) | 1000 (512.5) | <0.001 |
| Neutrophil (×109/L) | 6.74 (7.38) | 4.19 (2.99) | <0.001 |
| Procalcitonin (ng/mL) | 0.23 (0.4) | 0.06 (0.14) | <0.001 |
| Platelet (×109/L) | 211.5 (107.5) | 199 (115) | 0.611 |
| CRP (mg/L) | 97 (153) | 78 (99.75) | 0.166 |
| Ferritin (µg/L) | 1456 (1246.5) | 646 (864.75) | 0.003 |
| D-dimer (mg/L) | 1594.5 (9282) | 630 (564.5) | <0.001 |
| LDH (mmol/L) | 365 (179) | 300 (720) | <0.001 |
| -Hospital meters (median (IQR)) | |||
| Length of hospital stay (days) | 22 (28) | 8 (6) | <0.001 |
| Length of ICU stay (days) | 14 (13) | 0 (0) | |
| Cut-Off Value | Reference Value | Sensitivity (%) | Specificity (%) | AUC | CI 95% | ||
|---|---|---|---|---|---|---|---|
| Low | High | ||||||
| Glycaemia | 134.5 mg/dL | 70–110 | 82.5 | 85.3 | 89 | 82.5 | 95.5 |
| Creatine | 1.19 mg/dL | 0.7–1.1 | 32.5 | 91.2 | 61.7 | 50.5 | 72.9 |
| Leukocytes | 9.94 × 109/L | 4.5–11.5 | 37.5 | 95.6 | 68.4 | 57.5 | 79.4 |
| Lymphocytes | 0.8 × 109/L | 1.3–4 | 0.05 | 98.5 | 23.2 | 0.128 | 0.336 |
| Neutrophil | 5.48 × 109/L | 2–7.5 | 67.5 | 73.5 | 75.2 | 65.3 | 85.1 |
| Procalcitonin | 0.07 ng/mL | <0.1 | 97.4 | 54.8 | 78.2 | 69.3 | 87.1 |
| CRP | 145 mg/L | <10 | 38.5 | 80.9 | 58.1 | 46.5 | 69.6 |
| Ferritin | 934 µg/L | <307 | 72 | 61.8 | 70.3 | 57.4 | 83.2 |
| D-dimer | 1814.5 mg/L | <120 | 67 | 78.5 | 74.6 | 64 | 85.3 |
| LDH | 326 nmol/L | <225 | 70 | 76.5 | 71.5 | 61.1 | 82 |
| HGF | 187.5 pg/mL | - | 72.5 | 72.1 | 75.2 | 65.7 | 84.8 |
| IL-15 | 29.6 pg/mL | - | 22.5 | 80.9 | 39 | 27.4 | 50.7 |
| MCP1 | 56.77 pg/mL | - | 42.5 | 86.8 | 62.6 | 51.2 | 74 |
| PDGFBB | 182.5 pg/ml | - | 77.5 | 52.9 | 61.7 | 50.7 | 72.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gorgojo-Galindo, Ó.; Martín-Fernández, M.; Peñarrubia-Ponce, M.J.; Álvarez, F.J.; Ortega-Loubon, C.; Gonzalo-Benito, H.; Martínez-Paz, P.; Miramontes-González, J.P.; Gómez-Sánchez, E.; Poves-Álvarez, R.; et al. Predictive Modeling of Poor Outcome in Severe COVID-19: A Single-Center Observational Study Based on Clinical, Cytokine and Laboratory Profiles. J. Clin. Med. 2021, 10, 5431. https://doi.org/10.3390/jcm10225431
Gorgojo-Galindo Ó, Martín-Fernández M, Peñarrubia-Ponce MJ, Álvarez FJ, Ortega-Loubon C, Gonzalo-Benito H, Martínez-Paz P, Miramontes-González JP, Gómez-Sánchez E, Poves-Álvarez R, et al. Predictive Modeling of Poor Outcome in Severe COVID-19: A Single-Center Observational Study Based on Clinical, Cytokine and Laboratory Profiles. Journal of Clinical Medicine. 2021; 10(22):5431. https://doi.org/10.3390/jcm10225431
Chicago/Turabian StyleGorgojo-Galindo, Óscar, Marta Martín-Fernández, María Jesús Peñarrubia-Ponce, Francisco Javier Álvarez, Christian Ortega-Loubon, Hugo Gonzalo-Benito, Pedro Martínez-Paz, José Pablo Miramontes-González, Esther Gómez-Sánchez, Rodrigo Poves-Álvarez, and et al. 2021. "Predictive Modeling of Poor Outcome in Severe COVID-19: A Single-Center Observational Study Based on Clinical, Cytokine and Laboratory Profiles" Journal of Clinical Medicine 10, no. 22: 5431. https://doi.org/10.3390/jcm10225431
APA StyleGorgojo-Galindo, Ó., Martín-Fernández, M., Peñarrubia-Ponce, M. J., Álvarez, F. J., Ortega-Loubon, C., Gonzalo-Benito, H., Martínez-Paz, P., Miramontes-González, J. P., Gómez-Sánchez, E., Poves-Álvarez, R., Jorge-Monjas, P., Tamayo, E., Heredia-Rodríguez, M., & Tamayo-Velasco, Á. (2021). Predictive Modeling of Poor Outcome in Severe COVID-19: A Single-Center Observational Study Based on Clinical, Cytokine and Laboratory Profiles. Journal of Clinical Medicine, 10(22), 5431. https://doi.org/10.3390/jcm10225431








