Temporal Trends and Outcome of Patients with Acute Coronary Syndrome and Prior Myocardial Infarction
Abstract
:1. Introduction
2. Material and Methods
Statistical Analysis
3. Results
3.1. Prior MI vs. No Prior MI
3.2. Early vs. Late Period in Patients with Prior MI
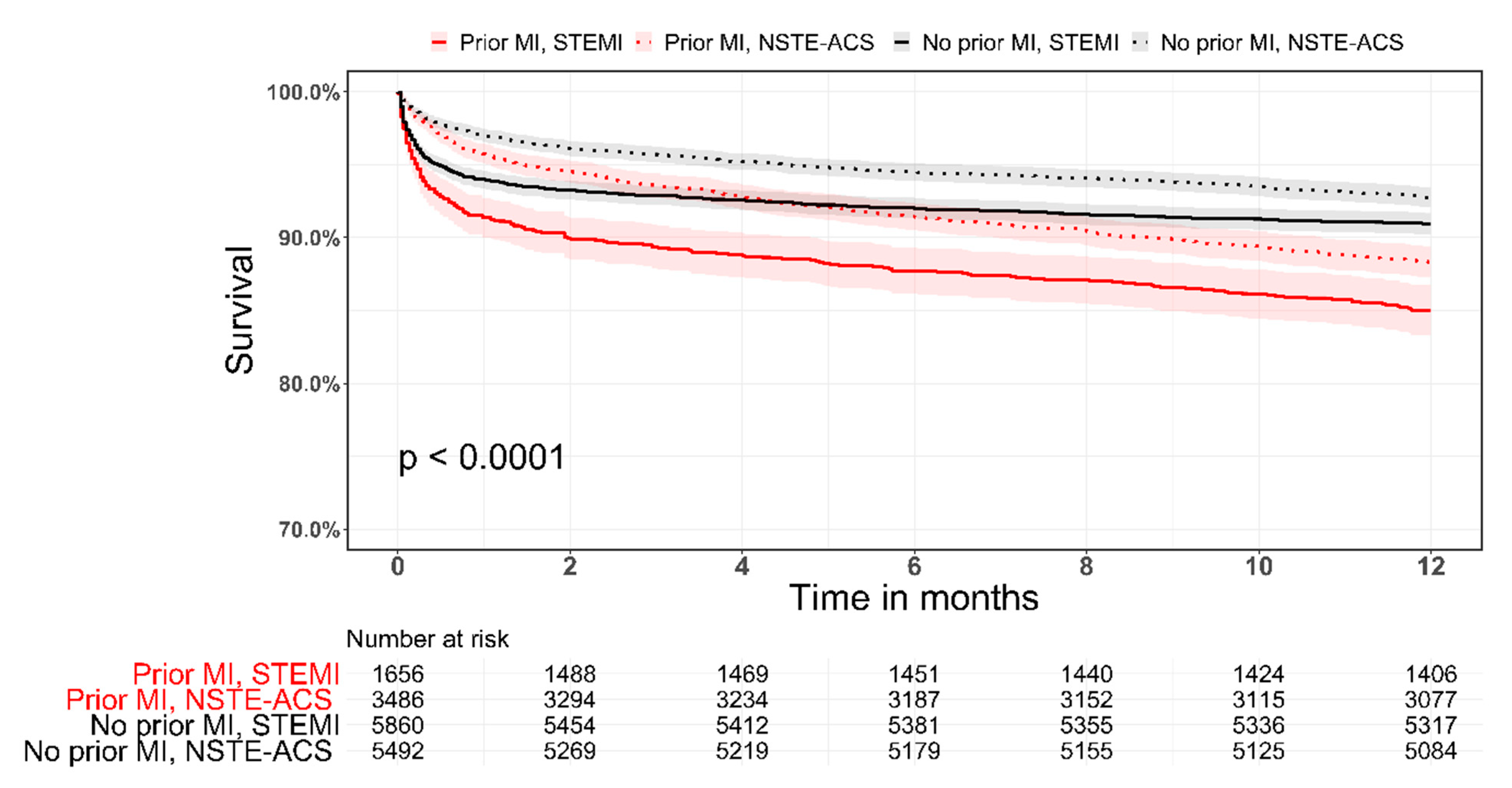
3.3. Clinical Outcomes
3.4. STEMI and NSTE-ACS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jernberg, T.; Hasvold, P.; Henriksson, M.; Hjelm, H.; Thuresson, M.; Janzon, M. Cardiovascular risk in post-myocardial infarction patients: Nationwide real world data demonstrate the importance of a long-term perspective. Eur. Heart J. 2015, 36, 1163–1170. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scirica, B.M.; Bonaca, M.P.; Braunwald, E.; De Ferrari, G.M.; Isaza, D.; Lewis, B.S.; Mehrhof, F.; Merlini, P.A.; Murphy, S.A.; Sabatine, M.S.; et al. Vorapaxar for secondary prevention of thrombotic events for patients with previous myocardial infarction: A prespecified subgroup analysis of the TRA 2 P-TIMI 50 trial. Lancet 2012, 380, 1317–1324. [Google Scholar] [CrossRef]
- Bonaca, M.P.; Bhatt, D.L.; Cohen, M.; Steg, P.G.; Storey, R.F.; Jensen, E.C.; Magnani, G.; Bansilal, S.; Fish, M.P.; Im, K.; et al. Long-Term Use of Ticagrelor in Patients with Prior Myocardial Infarction. N. Engl. J. Med. 2015, 372, 1791–1800. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeh, R.W.; Kereiakes, D.J.; Steg, P.G.; Windecker, S.; Rinaldi, M.J.; Gershlick, A.H.; Cutlip, D.E.; Cohen, D.J.; Tanguay, J.F.; Jacobs, A.; et al. Benefits and risks of extended duration dual antiplatelet therapy after PCI in patients with and without acute myocardial infarction. J. Am. Coll. Cardiol. 2015, 65, 2211–2221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eisen, A.; Harrington, R.A.; Stone, G.W.; Steg, P.G.; Gibson, C.M.; Hamm, C.W.; Price, M.J.; Prats, J.; Deliargyris, E.N.; Mahaffey, K.W.; et al. Cangrelor compared with clopidogrel in patients with prior myocardial infarction–Insights from the CHAMPION trials. Int. J. Cardiol. 2018, 250, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Radovanovic, D.; Maurer, L.; Bertel, O.; Witassek, F.; Urban, P.; Stauffer, J.-C.; Pedrazzini, G.; Erne, P. Treatment and outcomes of patients with recurrent myocardial infarction: A prospective observational cohort study. J. Cardiol. 2016, 68, 498–503. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, L.; Shah, B.R.; Nam, A.; Holmes, D.; Alexander, K.P.; Bhatt, D.L.; Ho, P.M.; Peterson, E.D.; He, B.; Roe, M.T. Implications of prior myocardial infarction for patients presenting with an acute myocardial infarction. Am. Heart J. 2014, 167, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Nichols, M.; Townsend, N.; Scarborough, P.; Rayner, M. Trends in age-specific coronary heart disease mortality in the European Union over three decades: 1980–2009. Eur. Heart J. 2013, 34, 3017–3027. [Google Scholar] [CrossRef] [PubMed]
- Nichols, M.; Townsend, N.; Scarborough, P.; Rayner, M. Cardiovascular disease in Europe: Epidemiological update. Eur. Heart J. 2013, 34, 3028–3034. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.S.; Johnston, S.C. Global variation in the relative burden of stroke and ischemic heart disease. Circulation 2011, 124, 314–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hammer, Y.; Eisen, A.; Hasdai, D.; Goldenberg, I.; Shlomo, N.; Cohen, T.; Beigel, R.; Kornowski, R.; Iakobishvili, Z. Comparison of Outcomes in Patients With Acute Coronary Syndrome Presenting With Typical Versus Atypical Symptoms. Am. J. Cardiol. 2019, 124, 1851–1856. [Google Scholar] [CrossRef] [PubMed]
- Di Martino, M.; Kirchmayer, U.; Agabiti, N.; Bauleo, L.; Fusco, D.; Perucci, C.A.; Davoli, M. The impact of time-window bias on the assessment of the long-term effect of medication adherence: The case of secondary prevention after myocardial infarction. BMJ Open 2015, 5, e007866. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kikkert, W.J.; Zwinderman, A.H.; Vis, M.M.; Baan, J.J.; Koch, K.T.; Peters, R.J.; de Winter, R.J.; Piek, J.J.; Tijssen, J.G.P.; Henriques, J.P.S. Timing of mortality after severe bleeding and recurrent myocardial infarction in patients with ST-segment-elevation myocardial infarction. Circ. Cardiovasc. Interv. 2013, 6, 391–398. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Prior MI | No Prior MI | |||||
|---|---|---|---|---|---|---|
| Early | Late | p Value | Early | Late | p Value | |
| n = 2826 | n = 2491 | n = 6899 | n = 4718 | |||
| Age (years) | 66.7 ± 12.6 | 66.6 ± 12.3 | 0.829 | 62.6 ± 13.2 | 62.7 ± 12.9 | 0.518 |
| Gender (male) | 2244 (79.4) | 2072 (83.2) | 0.001 | 5178 (75.1) | 3579 (75.9) | 0.334 |
| Dyslipidemia | 2050 (72.5) | 2208 (88.6) | <0.001 | 3649 (53.0) | 3089 (65.7) | <0.001 |
| Hypertension | 1852 (65.5) | 2025 (81.3) | <0.001 | 3467 (50.3) | 2718 (57.8) | <0.001 |
| Active smoker | 805 (28.5) | 896 (36.0) | <0.001 | 2654 (38.5) | 1959 (41.5) | 0.002 |
| Diabetes mellitus | 1186 (42.0) | 1279 (51.3) | <0.001 | 2043 (29.6) | 1598 (33.9) | <0.001 |
| Prior CABG | 697 (24.7) | 554 (22.2) | 0.041 | 300 (4.3) | 110 (2.3) | <0.001 |
| Prior PCI | 1637 (57.9) | 2072 (83.2) | <0.001 | 691 (10.0) | 378 (8.0) | <0.001 |
| Chronic kidney disase | 519 (18.4) | 464 (18.6) | 0.944 | 476 (6.9) | 390 (8.3) | 0.007 |
| PVD | 432 (15.3) | 312 (12.5) | 0.004 | 449 (6.5) | 212 (4.5) | <0.001 |
| Stroke/TIA | 320 (11.4) | 307 (12.3) | 0.332 | 450 (6.5) | 304 (6.4) | 0.876 |
| History of heart failure | 564 (20) | 457 (18.3) | 0.146 | 204 (3.0) | 143 (3.0) | 0.861 |
| Baseline medications | ||||||
| Aspirin | 1880 (82.1) | 1873 (79.2) | 0.013 | 1811 (32.3) | 1468 (33.2) | 0.339 |
| P2Y12 inhibitors | 356 (15.6) | 629 (27.8) | <0.001 | 146 (2.6) | 229 (5.3) | <0.001 |
| ACE-I/ARB | 630 (57.2) | 1468 (69.2) | <0.001 | 739 (27.4) | 1539 (37.6) | <0.001 |
| Beta blockers | 1413 (62.0) | 1526 (67.7) | <0.001 | 1361 (24.2) | 1038 (24.8) | 0.699 |
| Statins | 1467 (64.4) | 1822 (81.9) | <0.001 | 1590 (28.3) | 1731 (45.3) | <0.001 |
| Prior MI | No Prior MI | |||||
|---|---|---|---|---|---|---|
| Early | Late | p Value | Early | Late | p Value | |
| n = 2826 | n = 2491 | n = 6899 | n = 4718 | |||
| ST elevation at presentation | 983 (34.8) | 711 (28.5) | <0.001 | 3743 (54.3) | 2250 (47.7) | <0.001 |
| Admission Killip III/IV | 306 (10.8) | 154 (6.6) | <0.001 | 425 (6.2) | 202 (4.5) | <0.001 |
| Revascularization therapy | ||||||
| Primary PCI | 563 (19.9) | 386 (21.4) | 0.048 | 2426 (35.2) | 1382 (38.1) | <0.001 |
| Any PCI | 918 (58.9) | 1545 (62.0) | 0.053 | 2809 (73.1) | 3460 (73.3) | 0.836 |
| CABG | 111 (7.0) | 89 (3.6) | <0.001 | 256 (6.8) | 264 (5.6) | 0.021 |
| Number of diseased vessels | ||||||
| 1 | 245 (18.7) | 497 (24.2) | <0.001 | 1277 (36.4) | 1591 (37.8) | 0.031 |
| 2 | 456 (34.9) | 635 (30.9) | 1152 (32.8) | 1275 (30.3) | ||
| 3 | 573 (43.8) | 847 (41.2) | 908 (25.9) | 1091 (25.9) | ||
| In-hospital complications | ||||||
| Pulmonary edema (Killip-3) | 324 (11.5) | 150 (6.0) | <0.001 | 501 (7.3) | 135 (2.9) | <0.001 |
| Cardiogenic shock (Killip-4) | 136 (4.8) | 67 (2.7) | <0.001 | 233 (3.4) | 138 (2.9) | 0.189 |
| Re-MI | 66 (2.4) | 25 (1.0) | <0.001 | 101 (1.5) | 31 (0.7) | <0.001 |
| Stent thrombosis | 19 (1.6) | 18 (0.7) | 0.017 | 18 (0.7) | 24 (0.5) | 0.433 |
| Free wall rupture | 6 (0.2) | 1 (0.0) | 0.176 | 46 (0.7) | 6 (0.1) | <0.001 |
| MR moderate—severe | 84 (3.0) | 39 (1.6) | 0.001 | 137 (2.0) | 65 (1.4) | 0.016 |
| Sustained VT (>125 bpm) | 58 (2.1) | 32 (1.3) | 0.037 | 105 (1.7) | 53 (1.1) | 0.081 |
| Primary VF | 55 (2.0) | 25 (1.0) | 0.006 | 156 (2.3) | 76 (1.6) | 0.016 |
| Acute renal failure | 251 (8.9) | 155 (6.2) | <0.001 | 393 (5.7) | 214 (4.5) | 0.006 |
| Treatment at discharge | ||||||
| Aspirin | 2540 (92.4) | 2305 (95.2) | <0.001 | 6318 (93.7) | 4441 (96.3) | <0.001 |
| P2Y12 inhibitors | 1526 (56.5) | 2133 (88.4) | <0.001 | 4191 (62.7) | 4098 (89.1) | <0.001 |
| Statins | 2144 (78.5) | 2315 (96.4) | <0.001 | 5160 (76.8) | 4361 (95.7) | <0.001 |
| ACE/ARBs | 1077 (38.1) | 1894 (76.0) | <0.001 | 2436 (35.3) | 3490 (74.0) | <0.001 |
| Beta blockers | 2183 (79.8) | 1967 (85.2) | <0.001 | 5246 (77.9) | 3509 (80.1) | 0.007 |
| Referral to cardiac rehabilitation | 350 (33.2) | 1007 (49.6) | <0.001 | 1047 (42.2) | 2269 (58.7) | <0.001 |
| Prior MI | No Prior MI | |||||
|---|---|---|---|---|---|---|
| Early | Late | p Value | Early | Late | p Value | |
| n = 1809 | n = 1809 | n = 4490 | n = 4490 | |||
| Re MI/Angina | 96 (11.2) | 83 (6.4) | <0.001 | 151 (8.6) | 128 (4.2) | <0.001 |
| MACE * (30 days) | 356 (19.7) | 203 (11.3) | <0.001 | 696 (15.5) | 396 (8.9) | <0.001 |
| 30-day mortality | 89 (4.9) | 91 (5.1) | 0.860 | 228 (5.1) | 146 (3.3) | <0.001 |
| 1-year mortality | 218 (12.1) | 188 (10.9) | 0.272 | 396 (8.9) | 288 (6.7) | <0.001 |
| Prior MI | No Prior MI | |||||
|---|---|---|---|---|---|---|
| Early | Late | p Value | Early | Late | p Value | |
| n = 2826 | n = 2491 | n = 6899 | n = 4718 | |||
| Re-MI/angina (30 days) | 131 (12.0) | 102 (6.7) | <0.001 | 230 (9.0) | 129 (4.2) | <0.001 |
| MACE * (30 days) | 593 (21.0) | 261 (10.6) | <0.001 | 1119 (16.2) | 413 (8.8) | <0.001 |
| 30-days mortality | 182 (6.5) | 110 (4.5) | 0.003 | 362 (5.3) | 155 (3.3) | <0.001 |
| 1-year mortality | 409 (14.6) | 250 (10.7) | <0.001 | 622 (9.1) | 305 (6.8) | <0.001 |
| Prior MI | No Prior-MI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| STEMI | NSTE-ACS | STEMI | NSTE-ACS | |||||||||
| Early | Late | p Value | Early | Late | p Value | Early | Late | p Value | Early | Late | p Value | |
| n = 983 | n = 711 | n = 1838 | n = 1780 | n = 983 | n = 711 | n = 3153 | n = 2468 | |||||
| Re-MI/angina (30 days) | 51 (15.8) | 33 (7.7) | 0.001 | 80 (10.4) | 69 (6.3) | 0.002 | 124 (9.7) | 61 (4.1) | <0.001 | 106 (8.4) | 68 (4.3) | <0.001 |
| MACE * | 239 (24.3) | 91 (12.9) | <0.001 | 352 (19.2) | 170 (9.7) | <0.001 | 646 (17.3) | 210 (9.4) | <0.001 | 473 (15.0) | 203 (8.3) | <0.001 |
| (30 days) | ||||||||||||
| 30-days mortality | 96 (9.8) | 47 (6.7) | 0.032 | 85 (4.6) | 63 (3.6) | 0.155 | 256 (6.9) | 96 (4.3) | <0.001 | 106 (3.4) | 59 (2.4) | 0.049 |
| 1-year mortality | 160 (16.4) | 88 (13.0) | 0.068 | 246 (13.5) | 162 (9.7) | 0.001 | 373 (10.0) | 157 (7.3) | 0.001 | 249 (7.9) | 148 (6.3) | 0.023 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orvin, K.; Shechter, A.; Zahger, D.; Shklovski, V.; Ovdat, T.; Beigel, R.; Kornowski, R.; Eisen, A. Temporal Trends and Outcome of Patients with Acute Coronary Syndrome and Prior Myocardial Infarction. J. Clin. Med. 2021, 10, 5580. https://doi.org/10.3390/jcm10235580
Orvin K, Shechter A, Zahger D, Shklovski V, Ovdat T, Beigel R, Kornowski R, Eisen A. Temporal Trends and Outcome of Patients with Acute Coronary Syndrome and Prior Myocardial Infarction. Journal of Clinical Medicine. 2021; 10(23):5580. https://doi.org/10.3390/jcm10235580
Chicago/Turabian StyleOrvin, Katia, Alon Shechter, Doron Zahger, Vitaly Shklovski, Tal Ovdat, Roy Beigel, Ran Kornowski, and Alon Eisen. 2021. "Temporal Trends and Outcome of Patients with Acute Coronary Syndrome and Prior Myocardial Infarction" Journal of Clinical Medicine 10, no. 23: 5580. https://doi.org/10.3390/jcm10235580
APA StyleOrvin, K., Shechter, A., Zahger, D., Shklovski, V., Ovdat, T., Beigel, R., Kornowski, R., & Eisen, A. (2021). Temporal Trends and Outcome of Patients with Acute Coronary Syndrome and Prior Myocardial Infarction. Journal of Clinical Medicine, 10(23), 5580. https://doi.org/10.3390/jcm10235580







