Effectiveness of Psychological Treatments for Borderline Personality Disorder and Predictors of Treatment Outcomes: A Multivariate Multilevel Meta-Analysis of Data from All Design Types
Abstract
:1. Introduction
2. Materials and Methods
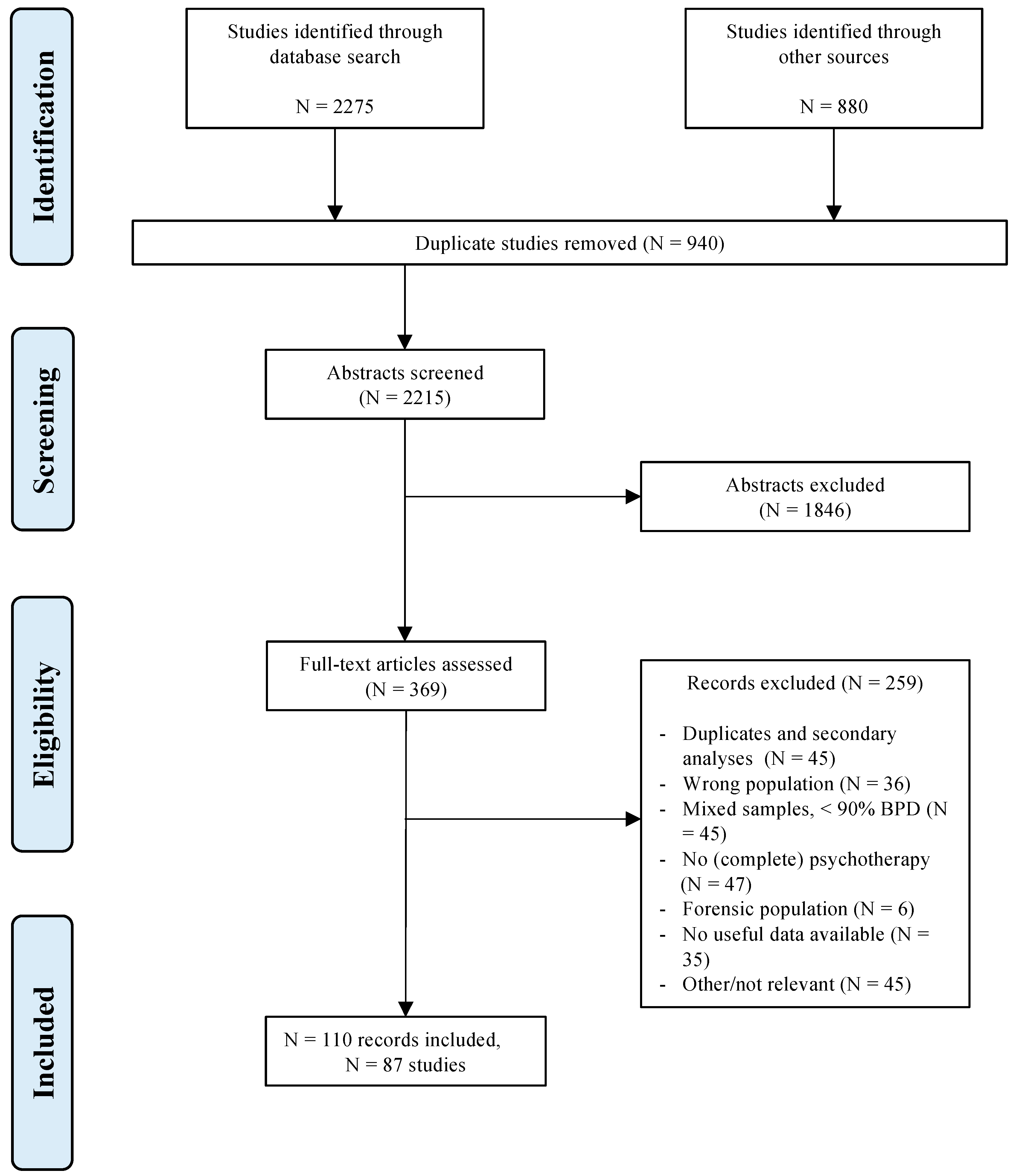
2.1. Identification and Selection of Studies
2.2. Treatment Classification
2.3. Coding of Methodological Quality
2.4. Coding of Other Characteristics
2.5. Effect Size Definition
2.6. Statistical Analysis
3. Results
3.1. Search Results
3.2. Main Analysis
3.2.1. Main Analysis Model Selection
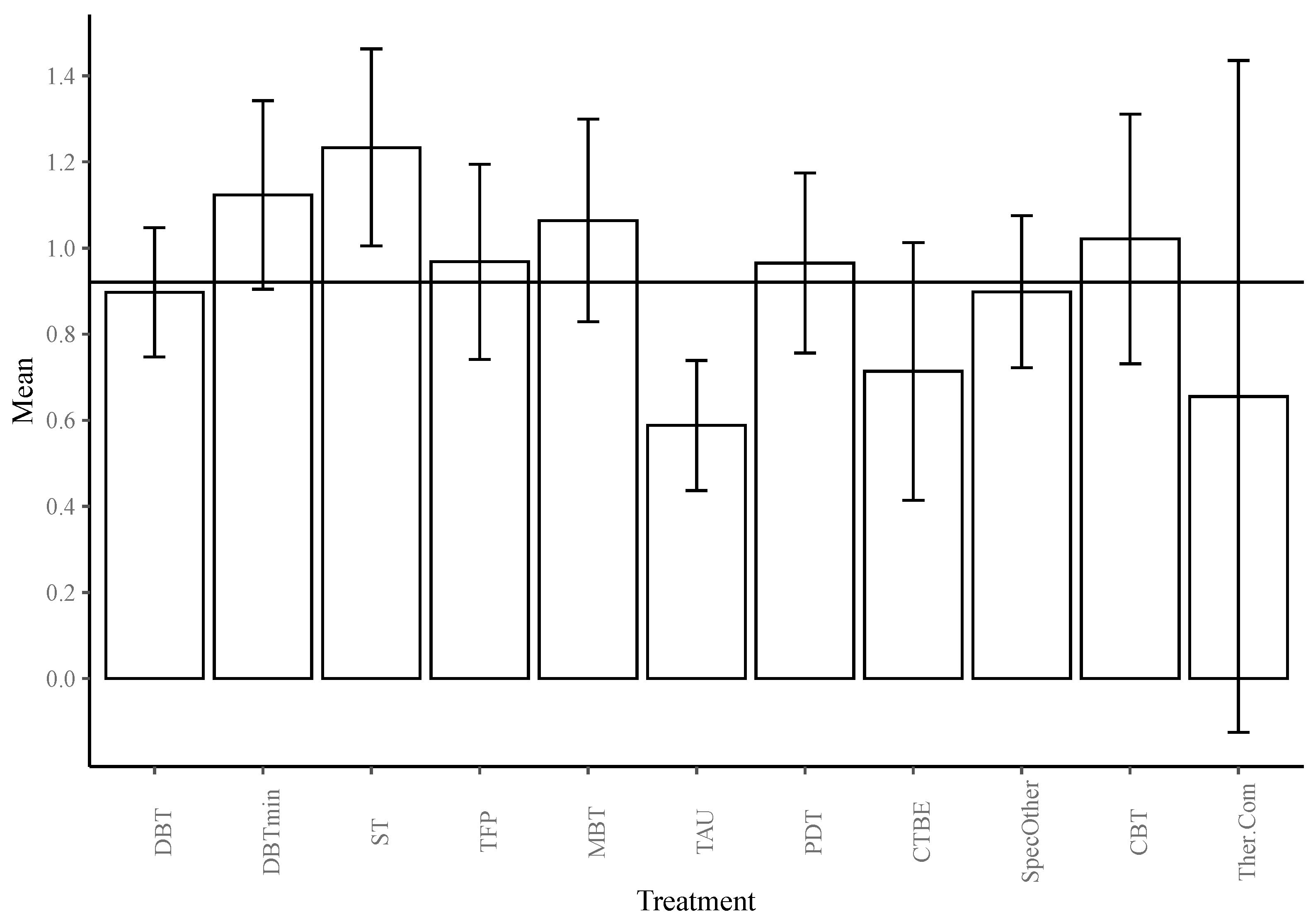
3.2.2. Deviation Contrasts
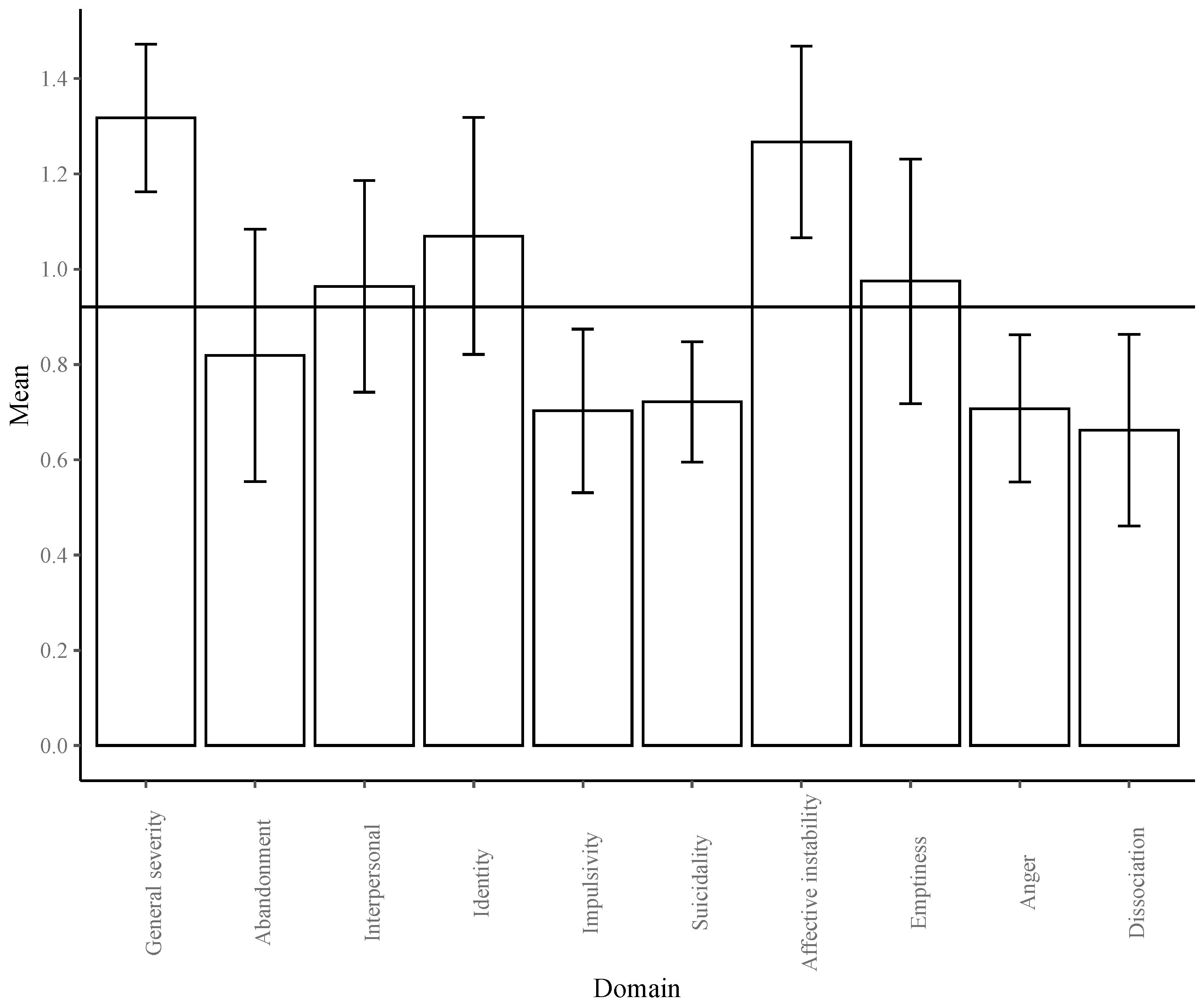
3.2.3. Treatment and BPD Interaction
3.2.4. Outliers and Bias
3.3. Sensitivity Analysis
3.3.1. Sensitivity Analysis Model Selection
3.3.2. Sensitivity Analysis Deviation Contrasts
3.3.3. Sensitivity Analysis Outliers and Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association Publishing: Washington, DC, USA, 2013; ISBN 0-89042-555-8. [Google Scholar]
- van Asselt, A.; Dirksen, C.; Arntz, A.; Severens, J. The cost of borderline personality disorder: Societal cost of illness in BPD-patients. Eur. Psychiatry 2007, 22, 354–361. [Google Scholar] [CrossRef]
- Trull, T.J.; Jahng, S.; Tomko, R.; Wood, P.K.; Sher, K.J. Revised NESARC Personality Disorder Diagnoses: Gender, Prevalence, and Comorbidity with Substance Dependence Disorders. J. Pers. Disord. 2010, 24, 412–426. [Google Scholar] [CrossRef] [PubMed]
- Coid, J.; Yang, M.; Tyrer, P.; Roberts, A.; Ullrich, S. Prevalence and correlates of personality disorder in Great Britain. Br. J. Psychiatry 2006, 188, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Tomko, R.; Trull, T.J.; Wood, P.K.; Sher, K.J. Characteristics of Borderline Personality Disorder in a Community Sample: Comorbidity, Treatment Utilization, and General Functioning. J. Pers. Disord. 2014, 28, 734–750. [Google Scholar] [CrossRef] [PubMed]
- Black, D.W.; Blum, N.; Pfohl, B.; Hale, N. Suicidal Behavior in Borderline Personality Disorder: Prevalence, Risk Factors, Prediction, and Prevention. J. Pers. Disord. 2004, 18, 226–239. [Google Scholar] [CrossRef]
- Cleary, M.; Siegfried, N.; Walter, G. Experience, knowledge and attitudes of mental health staff regarding clients with a borderline personality disorder. Int. J. Ment. Health Nurs. 2002, 11, 186–191. [Google Scholar] [CrossRef]
- Barnicot, K.; Katsakou, C.; Bhatti, N.; Savill, M.; Fearns, N.; Priebe, S. Factors predicting the outcome of psychotherapy for borderline personality disorder: A systematic review. Clin. Psychol. Rev. 2012, 32, 400–412. [Google Scholar] [CrossRef] [PubMed]
- Barnicot, K.; Crawford, M. Dialectical behaviour therapy v. mentalisation-based therapy for borderline personality disorder. Psychol. Med. 2019, 49, 2060–2068. [Google Scholar] [CrossRef]
- Clarkin, J.F.; Levy, K.N.; Lenzenweger, M.F.; Kernberg, O.F. Evaluating Three Treatments for Borderline Personality Disorder: A Multiwave Study. Am. J. Psychiatry 2007, 164, 922–928. [Google Scholar] [CrossRef] [PubMed]
- Cristea, I.A.; Gentili, C.; Coteț, C.D.; Palomba, D.; Barbui, C.; Cuijpers, P. Efficacy of Psychotherapies for Borderline Personality Disorder. JAMA Psychiatry 2017, 74, 319–328. [Google Scholar] [CrossRef]
- Oud, M.; Arntz, A.; Hermens, M.L.; Verhoef, R.; Kendall, T. Specialized psychotherapies for adults with borderline personality disorder: A systematic review and meta-analysis. Aust. N. Z. J. Psychiatry 2018, 52, 949–961. [Google Scholar] [CrossRef]
- Storebø, O.J.; Stoffers-Winterling, J.M.; Völlm, B.A.; Kongerslev, M.T.; Mattivi, J.T.; Jørgensen, M.S.; Faltinsen, E.; Todorovac, A.; Sales, C.P.; Callesen, H.E.; et al. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst. Rev. 2020, 5, CD012955. [Google Scholar] [CrossRef] [Green Version]
- Arntz, A.; Mensink, K.; Cox, W.; Verhoef, R.; van Emmerik, A.; Grasman, R. Dropout from Psychological Treatment for Borderline Personality Disorder: A Multilevel Survival Meta-Analysis. Psychol. Med. 2018. in preparation. [Google Scholar]
- Farrell, J.M.; Shaw, I.A.; Webber, M.A. A schema-focused approach to group psychotherapy for outpatients with borderline personality disorder: A randomized controlled trial. J. Behav. Ther. Exp. Psychiatry 2009, 40, 317–328. [Google Scholar] [CrossRef] [PubMed]
- Omar, H.; Tejerina-Arreal, M.; Crawford, M.J. Are recommendations for psychological treatment of borderline personality disorder in current UK guidelines justified? Systematic review and subgroup analysis. Pers. Ment. Health 2014, 8, 228–237. [Google Scholar] [CrossRef]
- Bloom, J.M.; Woodward, E.N.; Susmaras, T.; Pantalone, D.W. Use of Dialectical Behavior Therapy in Inpatient Treatment of Borderline Personality Disorder: A Systematic Review. Psychiatr. Serv. 2012, 63, 881–888. [Google Scholar] [CrossRef] [PubMed]
- Arntz, A.; Stupar-Rutenfrans, S.; Bloo, J.; van Dyck, R.; Spinhoven, P. Prediction of treatment discontinuation and recovery from Borderline Personality Disorder: Results from an RCT comparing Schema Therapy and Transference Focused Psychotherapy. Behav. Res. Ther. 2015, 74, 60–71. [Google Scholar] [CrossRef]
- Gunderson, J.G.; Daversa, M.T.; Grilo, C.M.; McGlashan, T.H.; Zanarini, M.C.; Shea, M.T.; Skodol, A.E.; Yen, S.; Sanislow, C.A.; Bender, D.S.; et al. Predictors of 2-Year Outcome for Patients With Borderline Personality Disorder. Am. J. Psychiatry 2006, 163, 822–826. [Google Scholar] [CrossRef]
- Gregory, R.J.; Chlebowski, S.; Kang, D.; Remen, A.L.; Soderberg, M.G.; Stepkovitch, J.; Virk, S. A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychother. Theory Res. Pract. Train. 2008, 45, 28–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thormählen, B. Patient Factors Predicting Dropout from Supportive-Expressive Psychotherapy for Patients with Personality Disorders. Psychother. Res. 2003, 13, 493–509. [Google Scholar] [CrossRef]
- Zanarini, M.C.; Frankenburg, F.R.; Hennen, J.; Reich, D.B.; Silk, K.R. Prediction of the 10-Year Course of Borderline Personality Disorder. Am. J. Psychiatry 2006, 163, 827–832. [Google Scholar] [CrossRef]
- Kliem, S.; Kröger, C.; Kosfelder, J. Dialectical behavior therapy for borderline personality disorder: A meta-analysis using mixed-effects modeling. J. Consult. Clin. Psychol. 2010, 78, 936–951. [Google Scholar] [CrossRef] [Green Version]
- Cuijpers, P.; van Straten, A.; Bohlmeijer, E.; Hollon, S.D.; Andersson, G. The effects of psychotherapy for adult depression are overestimated: A meta-analysis of study quality and effect size. Psychol. Med. 2009, 40, 211–223. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agresti, A.; Coull, B.A. Approximate is Better than “Exact” for Interval Estimation of Binomial Proportions. Am. Stat. 1998, 52, 119–126. [Google Scholar] [CrossRef]
- Morris, S.B. Estimating Effect Sizes From Pretest-Posttest-Control Group Designs. Organ. Res. Methods 2008, 11, 364–386. [Google Scholar] [CrossRef]
- Cheung, M.W.-L. Modeling dependent effect sizes with three-level meta-analyses: A structural equation modeling approach. Psychol. Methods 2014, 19, 211–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viechtbauer, W. Conducting Meta-Analyses in R with the Metafor Package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- Bartoń, K. MuMIn: Multi-Model Inference. R Package Version 1.43.6. 2013. Available online: https://CRAN.R-project.org/package=MuMIn (accessed on 23 November 2021).
- Neath, A.A.; Cavanaugh, J.E. The Bayesian information criterion: Background, derivation, and applications. Wiley Interdiscip. Rev. Comput. Stat. 2012, 4, 199–203. [Google Scholar] [CrossRef]
- Holm, S. A Simple Sequentially Rejective Multiple Test Procedure. Scand. J. Stat. 1979, 6, 65–70. [Google Scholar]
- Fernández-Castilla, B.; Declercq, L.; Jamshidi, L.; Beretvas, S.N.; Onghena, P.; Noortgate, W.V.D. Detecting Selection Bias in Meta-Analyses with Multiple Outcomes: A Simulation Study. J. Exp. Educ. 2021, 89, 125–144. [Google Scholar] [CrossRef]
- Fleiss, J.L. Measuring nominal scale agreement among many raters. Psychol. Bull. 1971, 76, 378–382. [Google Scholar] [CrossRef]
- Linehan, M.M.; Comtois, K.A.; Murray, A.M.; Brown, M.Z.; Gallop, R.J.; Heard, H.L.; Korslund, K.E.; Tutek, D.A.; Reynolds, S.K.; Lindenboim, N. Two-Year Randomized Controlled Trial and Follow-up of Dialectical Behavior Therapy vs Therapy by Experts for Suicidal Behaviors and Borderline Personality Disorder. Arch. Gen. Psychiatry 2006, 63, 757–766. [Google Scholar] [CrossRef]
- Zanarini, M.C.; Frankenburg, F.R.; Hennen, J.; Reich, D.B.; Silk, K.R. The McLean Study of Adult Development (MSAD): Overview and Implications of the First Six Years of Prospective Follow-Up. J. Pers. Disord. 2005, 19, 505–523. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGlashan, T.H.; Grilo, C.M.; Sanislow, C.A.; Ralevski, E.; Morey, L.C.; Gunderson, J.G.; Skodol, A.E.; Shea, M.T.; Zanarini, M.C.; Bender, D.; et al. Two-Year Prevalence and Stability of Individual DSM-IV Criteria for Schizotypal, Borderline, Avoidant, and Obsessive-Compulsive Personality Disorders: Toward a Hybrid Model of Axis II Disorders. Am. J. Psychiatry 2005, 162, 883–889. [Google Scholar] [CrossRef] [Green Version]
- von Klipstein, L.; Borsboom, D.; Arntz, A. The exploratory value of cross-sectional partial correlation networks: Predicting relationships between change trajectories in borderline personality disorder. PLoS ONE 2021, 16, e0254496. [Google Scholar] [CrossRef] [PubMed]
- Costa, P. Personality stability and its implications for clinical psychology. Clin. Psychol. Rev. 1986, 6, 407–423. [Google Scholar] [CrossRef]
- Kievit, R.A.; Frankenhuis, W.E.; Waldorp, L.J.; Borsboom, D. Simpson’s paradox in psychological science: A practical guide. Front. Psychol. 2013, 4, 513. [Google Scholar] [CrossRef] [Green Version]
- Simpson, E.H. The Interpretation of Interaction in Contingency Tables. J. R. Stat. Soc. Ser. B (Methodol.) 1951, 13, 238–241. [Google Scholar] [CrossRef]
- Bach, B.; First, M.B. Application of the ICD-11 classification of personality disorders. BMC Psychiatry 2018, 18, 351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lachin, J.M. Fallacies of last observation carried forward analyses. Clin. Trials 2016, 13, 161–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lau, J.; Ioannidis, J.P.A.; Terrin, N.; Schmid, C.; Olkin, I. The case of the misleading funnel plot. BMJ 2006, 333, 597–600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems (11th ed.). Available online: https://icd.who.int/ (accessed on 23 November 2021).
- Meuldijk, D.; McCarthy, A.; Bourke, M.E.; Grenyer, B.F.S. The value of psychological treatment for borderline personality disorder: Systematic review and cost offset analysis of economic evaluations. PLoS ONE 2017, 12, e0171592. [Google Scholar] [CrossRef]
- Wetzelaer, P.; Lokkerbol, J.; Arntz, A.; van Asselt, T.; Smit, F.; Evers, S. Cost-effectiveness and Budget Impact of Specialized Psychotherapy for Borderline Personality Disorder: A Synthesis of the Evidence. J. Ment. Health Policy Econ. 2017, 20, 177–190. [Google Scholar]
- van den Noortgate, W.; López, J.; Marín-Martínez, F.; Sánchez-Meca, J. Three-level meta-analysis of dependent effect sizes. Behav. Res. Methods 2012, 45, 576–594. [Google Scholar] [CrossRef] [Green Version]
- van den Noortgate, W.; López, J.; Marín-Martínez, F.; Sánchez-Meca, J. Meta-analysis of multiple outcomes: A multilevel approach. Behav. Res. Methods 2014, 47, 1274–1294. [Google Scholar] [CrossRef]
- Asay, T.P.; Lambert, M.J.; Gregersen, A.T.; Goates, M.K. Using patient-focused research in evaluating treatment outcome in private practice. J. Clin. Psychol. 2002, 58, 1213–1225. [Google Scholar] [CrossRef] [PubMed]
- Lincoln, T.; Jung, E.; Wiesjahn, M.; Schlier, B. What is the minimal dose of cognitive behavior therapy for psychosis? An approximation using repeated assessments over 45 sessions. Eur. Psychiatry 2016, 38, 31–39. [Google Scholar] [CrossRef]
| Variable | df | Log-Likelihood | p | |
|---|---|---|---|---|
| Full Model | 106 | −281.410 | ||
| Treatment | 156.326 | 34 | −359.572 | <0.001 *** |
| BPD Domain | 248.573 | 35 | −405.696 | <0.001 *** |
| Treatment * BPD domain | 116.105 | 44 | −339.462 | <0.001 *** |
| Setting | 2.504 | 104 | −282.662 | 0.286 |
| Format | 2.944 | 104 | −282.882 | 0.229 |
| Quality | 0.021 | 105 | −281.420 | 0.885 |
| Trial type | 1.213 | 104 | −282.016 | 0.545 |
| Publication year | 0.005 | 105 | −281.412 | 0.942 |
| Country of testing | 1.020 | 104 | −281.919 | 0.601 |
| Male proportion | 0.041 | 105 | −281.430 | 0.839 |
| Analysis type | 20.043 | 103 | −291.431 | <0.001 *** |
| Mean age | 11.553 | 105 | −287.186 | 0.001 ** |
| Medication policy | 0.358 | 105 | −281.588 | 0.550 |
| Substance use exclusion | 1.185 | 104 | −282.002 | 0.548 |
| Assessment type | 2.100 | 103 | −282.653 | 0.553 |
| Outcome type | 8.902 | 105 | −285.860 | 0.003 ** |
| Final Model | 24 | −353.108 | ||
| Treatment | 69.982 | 14 | −388.099 | <0.001 *** |
| BPD Domain | 132.254 | 15 | −419.235 | <0.001 *** |
| Outcome type | 11.757 | 23 | −358.986 | 0.001 ** |
| Mean age | 5.413 | 23 | −355.814 | 0.020 * |
| Contrast | Mean | 95% CI | ∆g | ∆g (se) | ∆g (t) | ∆g (p) | ∆g (p’) |
|---|---|---|---|---|---|---|---|
| Average Age | (B) −0.021 | [−0.039, −0.003] | (se) 0.009 | (t) −2.333 | 0.020 * | ||
| Treatment | |||||||
| DBT | 0.897 | [0.747, 1.047] | −0.024 | 0.062 | −0.381 | 0.352 | 1.000 |
| DBTmin | 1.123 | [0.904, 1.342] | 0.203 | 0.098 | 2.063 | 0.020 * | 0.178 |
| ST | 1.233 | [1.005, 1.462] | 0.313 | 0.104 | 3.013 | 0.001 ** | 0.014 * |
| TFP | 0.968 | [0.741, 1.194] | 0.047 | 0.096 | 0.492 | 0.311 | 1.000 |
| MBT | 1.064 | [0.829, 1.299] | 0.143 | 0.108 | 1.328 | 0.092 | 0.646 |
| TAU | 0.588 | [0.437, 0.739] | −0.333 | 0.064 | −5.165 | <0.001 *** | <0.001 *** |
| PDT | 0.965 | [0.756, 1.174] | 0.045 | 0.091 | 0.490 | 0.312 | 1.000 |
| CTBE | 0.714 | [0.414, 1.013] | −0.207 | 0.132 | −1.571 | 0.058 | 0.467 |
| Spec. Other | 0.898 | [0.722, 1.075] | −0.022 | 0.079 | −0.279 | 0.390 | 1.000 |
| CBT | 1.021 | [0.731, 1.311] | 0.100 | 0.136 | 0.737 | 0.231 | 1.000 |
| Th. Com | 0.655 | [−0.125, 1.435] | −0.265 | 0.368 | −0.722 | 0.235 | 1.000 |
| Grand Mean | 0.921 | ||||||
| BPD Domain | |||||||
| General severity | 1.317 | [1.162, 1.472] | 0.397 | 0.057 | 6.966 | <0.001 *** | <0.001 *** |
| Abandonment | 0.819 | [0.554, 1.084] | −0.102 | 0.106 | −0.960 | 0.169 | 0.506 |
| Interpersonal | 0.964 | [0.742, 1.186] | 0.044 | 0.085 | 0.517 | 0.303 | 0.596 |
| Identity Disturbance | 1.069 | [0.821, 1.318] | 0.149 | 0.099 | 1.509 | 0.066 | 0.264 |
| Impulsivity | 0.703 | [0.531, 0.874] | −0.218 | 0.060 | −3.620 | <0.001 *** | 0.001 ** |
| Suicidality/Self-injury | 0.722 | [0.595, 0.848] | −0.199 | 0.046 | −4.336 | <0.001 *** | <0.001 *** |
| Affective Instability | 1.267 | [1.066, 1.468] | 0.346 | 0.074 | 4.659 | <0.001 *** | <0.001 *** |
| Emptiness | 0.975 | [0.718, 1.231] | 0.054 | 0.102 | 0.530 | 0.298 | 0.596 |
| Anger | 0.707 | [0.553, 0.862] | −0.213 | 0.051 | −4.211 | <0.001 *** | <0.001 *** |
| Dissociation | 0.662 | [0.461, 0.863] | −0.258 | 0.076 | −3.411 | <0.001 *** | 0.002 ** |
| Grand Mean | 0.921 | ||||||
| Outcome Type | |||||||
| Continuous | 0.752 | [0.631, 0.873] | −0.123 | 0.050 | −2.451 | 0.007** | 0.015* |
| Dichotomous | 1.089 | [0.885, 1.293] | 0.123 | 0.050 | 2.451 | 0.007** | 0.015* |
| Grand Mean | 0.920 | ||||||
| Domain | Mean (g) | 95% CI | ∆g | ∆g (se) | ∆g (t) | ∆g (p) | ∆g (p’) |
|---|---|---|---|---|---|---|---|
| General Severity (n = 80) | |||||||
| DBT | 1.400 | [1.028, 1.772] | 0.016 | 0.179 | 0.087 | 0.466 | 1.000 |
| DBTmin | 1.689 | [1.109, 2.269] | 0.304 | 0.264 | 1.154 | 0.126 | 0.883 |
| ST | 1.331 | [0.923, 1.739] | −0.053 | 0.197 | −0.269 | 0.394 | 1.000 |
| MBT | 1.361 | [0.936, 1.785] | −0.024 | 0.199 | −0.119 | 0.453 | 1.000 |
| TAU | 0.641 | [0.335, 0.946] | −0.743 | 0.148 | −5.035 | <0.001 *** | 0.001 ** |
| PDT | 1.627 | [1.129, 2.125] | 0.243 | 0.230 | 1.058 | 0.147 | 0.883 |
| Spec. Other | 1.482 | [1.070, 1.895] | 0.098 | 0.195 | 0.502 | 0.309 | 1.000 |
| CBT | 1.544 | [0.896, 2.192] | 0.160 | 0.293 | 0.544 | 0.294 | 1.000 |
| Grand Mean | 1.384 | ||||||
| Abandonment (n = 8) | |||||||
| ST | 0.689 | [0.355, 1.024] | 0.234 | 0.128 | 1.832 | 0.063 | 0.190 |
| TAU | 0.466 | [−0.035, 0.967] | 0.011 | 0.153 | 0.071 | 0.473 | 0.473 |
| Spec. Other | 0.210 | [−0.316, 0.735] | −0.245 | 0.157 | −1.561 | 0.090 | 0.190 |
| Grand Mean | 0.455 | ||||||
| Interpersonal (n = 17) | |||||||
| DBT | 0.789 | [−0.217, 1.794] | −0.060 | 0.416 | −0.144 | 0.444 | 1.000 |
| ST | 0.742 | [0.075, 1.409] | −0.106 | 0.318 | −0.334 | 0.372 | 1.000 |
| TAU | 0.645 | [−0.011, 1.301] | −0.203 | 0.315 | −0.645 | 0.265 | 1.000 |
| Spec. Other | 0.946 | [0.081, 1.810] | 0.097 | 0.373 | 0.260 | 0.400 | 1.000 |
| CBT | 1.121 | [−0.524, 2.766] | 0.272 | 0.622 | 0.438 | 0.335 | 1.000 |
| Grand Mean | 0.849 | ||||||
| Identity (n = 14) | |||||||
| ST | 1.157 | [0.533, 1.782] | 0.587 | 0.289 | 2.032 | 0.035 * | 0.139 |
| TAU | 0.299 | [−0.300, 0.897] | −0.272 | 0.255 | −1.064 | 0.156 | 0.468 |
| Spec. Other | 0.648 | [−0.037, 1.334] | 0.078 | 0.284 | 0.274 | 0.395 | 0.523 |
| CBT | 0.177 | [−1.521, 1.876] | −0.393 | 0.593 | −0.663 | 0.261 | 0.523 |
| Grand Mean | 0.570 | ||||||
| Impulsivity (n = 50) | |||||||
| DBT | 0.610 | [0.367, 0.853] | 0.010 | 0.102 | 0.096 | 0.462 | 1.000 |
| DBTmin | 0.851 | [0.451, 1.251] | 0.251 | 0.184 | 1.364 | 0.090 | 0.629 |
| ST | 0.587 | [0.238, 0.937] | −0.013 | 0.157 | −0.080 | 0.468 | 1.000 |
| TFP | 0.487 | [0.149, 0.825] | −0.113 | 0.138 | −0.816 | 0.210 | 1.000 |
| TAU | 0.320 | [0.098, 0.542] | −0.280 | 0.104 | −2.691 | 0.005 ** | 0.041 * |
| PDT | 0.597 | [0.222, 0.973] | −0.003 | 0.156 | −0.017 | 0.493 | 1.000 |
| Spec. Other | 0.736 | [0.421, 1.052] | 0.136 | 0.138 | 0.988 | 0.164 | 0.986 |
| CBT | 0.611 | [0.079, 1.143] | 0.011 | 0.235 | 0.047 | 0.481 | 1.000 |
| Grand Mean | 0.600 | ||||||
| Suicidality (n = 184) | |||||||
| DBT | 0.563 | [0.424, 0.702] | −0.083 | 0.079 | 1.054 | 0.147 | 1.000 |
| DBTmin | 0.711 | [0.466, 0.957] | 0.065 | 0.124 | 0.526 | 0.300 | 1.000 |
| ST | 1.161 | [0.669, 1.653] | 0.515 | 0.229 | 2.253 | 0.013 * | 0.128 |
| TFP | 0.522 | [0.199, 0.845] | −0.124 | 0.144 | −0.858 | 0.196 | 1.000 |
| MBT | 0.872 | [0.612, 1.132] | 0.226 | 0.130 | 1.733 | 0.042 * | 0.358 |
| TAU | 0.393 | [0.225, 0.560] | −0.253 | 0.090 | −2.826 | 0.003 ** | 0.029 * |
| PDT | 0.512 | [0.128, 0.897] | −0.134 | 0.183 | −0.730 | 0.233 | 1.000 |
| CTBE | 0.380 | [0.046, 0.713] | −0.266 | 0.151 | −1.763 | 0.040 | 0.358 |
| Spec. Other | 0.593 | [0.390, 0.797] | −0.053 | 0.104 | −0.508 | 0.306 | 1.000 |
| CBT | 0.765 | [0.428, 1.103] | 0.119 | 0.164 | 0.729 | 0.234 | 1.000 |
| Th. Com | 0.633 | [−0.180, 1.446] | −0.013 | 0.379 | −0.035 | 0.487 | 1.000 |
| Grand Mean | 0.646 | ||||||
| Affective Instability (n = 27) | |||||||
| DBT | 1.070 | [0.491, 1.649] | −0.234 | 0.291 | −0.806 | 0.215 | 0.860 |
| DBTmin | 2.569 | [1.562, 3.576] | 1.265 | 0.433 | 2.919 | 0.004 ** | 0.030 * |
| ST | 1.324 | [0.648, 2.000] | 0.019 | 0.306 | 0.064 | 0.475 | 1.000 |
| TFP | 0.920 | [0.030, 1.811] | −0.384 | 0.389 | −0.988 | 0.167 | 0.837 |
| TAU | 0.705 | [0.187, 1.223] | −0.599 | 0.249 | −2.402 | .013 * | 0.078 |
| Spec. Other | 1.209 | [0.563, 1.856] | −0.095 | 0.305 | −0.311 | 0.379 | 1.000 |
| CBT | 1.333 | [−0.446, 3.131] | 0.028 | 0.754 | 0.038 | 0.485 | 1.000 |
| Grand Mean | 1.304 | ||||||
| Emptiness (n = 9) | |||||||
| ST | 1.118 | [0.519, 1.718] | 0.431 | 0.218 | 1.975 | 0.048 * | 0.096 |
| TAU | 0.311 | [−0.257, 0.880] | −0.376 | 0.166 | −2.264 | 0.032 * | 0.096 |
| Spec. Other | 0.631 | [−0.065, 1.328] | −0.056 | 0.191 | −0.291 | 0.390 | 0.390 |
| Grand Mean | 0.687 | ||||||
| Anger (n = 102) | |||||||
| DBT | 0.418 | [0.294, 0.541] | −0.116 | 0.068 | −1.704 | 0.046 | 0.229 |
| DBTmin | 0.829 | [0.569, 1.088] | 0.295 | 0.121 | 2.434 | 0.008 ** | 0.059 |
| ST | 0.679 | [0.372, 0.986] | 0.146 | 0.141 | 1.035 | 0.152 | 0.303 |
| TFP | 0.626 | [0.356, 0.897] | 0.093 | 0.125 | 0.747 | 0.228 | 0.303 |
| TAU | 0.234 | [0.073, 0.394] | −0.300 | 0.081 | −3.677 | <0.001 *** | 0.002 ** |
| PDT | 0.400 | [0.216, 0.585] | −0.133 | 0.090 | −1.469 | 0.073 | 0.238 |
| CTBE | 0.306 | [−0.010, 0.622] | −0.227 | 0.144 | −1.573 | 0.060 | 0.238 |
| Spec. Other | 0.773 | [0.490, 1.057] | 0.240 | 0.132 | 1.826 | 0.035 * | 0.213 |
| Grand Mean | 0.533 | ||||||
| Dissociation (n = 23) | |||||||
| DBT | 0.411 | [0.224, 0.599] | −0.011 | 0.085 | −0.133 | 0.448 | 0.737 |
| ST | 0.472 | [0.216, 0.728] | 0.049 | 0.105 | 0.470 | 0.322 | 0.737 |
| TAU | 0.316 | [0.039, 0.592] | −0.107 | 0.107 | −1.001 | 0.165 | 0.659 |
| Spec. Other | 0.491 | [0.251, 0.731] | 0.069 | 0.098 | 0.702 | 0.246 | 0.737 |
| Grand Mean | 0.422 | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rameckers, S.A.; Verhoef, R.E.J.; Grasman, R.P.P.P.; Cox, W.R.; van Emmerik, A.A.P.; Engelmoer, I.M.; Arntz, A. Effectiveness of Psychological Treatments for Borderline Personality Disorder and Predictors of Treatment Outcomes: A Multivariate Multilevel Meta-Analysis of Data from All Design Types. J. Clin. Med. 2021, 10, 5622. https://doi.org/10.3390/jcm10235622
Rameckers SA, Verhoef REJ, Grasman RPPP, Cox WR, van Emmerik AAP, Engelmoer IM, Arntz A. Effectiveness of Psychological Treatments for Borderline Personality Disorder and Predictors of Treatment Outcomes: A Multivariate Multilevel Meta-Analysis of Data from All Design Types. Journal of Clinical Medicine. 2021; 10(23):5622. https://doi.org/10.3390/jcm10235622
Chicago/Turabian StyleRameckers, Sophie A., Rogier E. J. Verhoef, Raoul P. P. P. Grasman, Wouter R. Cox, Arnold A. P. van Emmerik, Izabella M. Engelmoer, and Arnoud Arntz. 2021. "Effectiveness of Psychological Treatments for Borderline Personality Disorder and Predictors of Treatment Outcomes: A Multivariate Multilevel Meta-Analysis of Data from All Design Types" Journal of Clinical Medicine 10, no. 23: 5622. https://doi.org/10.3390/jcm10235622
APA StyleRameckers, S. A., Verhoef, R. E. J., Grasman, R. P. P. P., Cox, W. R., van Emmerik, A. A. P., Engelmoer, I. M., & Arntz, A. (2021). Effectiveness of Psychological Treatments for Borderline Personality Disorder and Predictors of Treatment Outcomes: A Multivariate Multilevel Meta-Analysis of Data from All Design Types. Journal of Clinical Medicine, 10(23), 5622. https://doi.org/10.3390/jcm10235622






