Associations between Early Surgery and Postoperative Outcomes in Elderly Patients with Distal Femur Fracture: A Retrospective Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
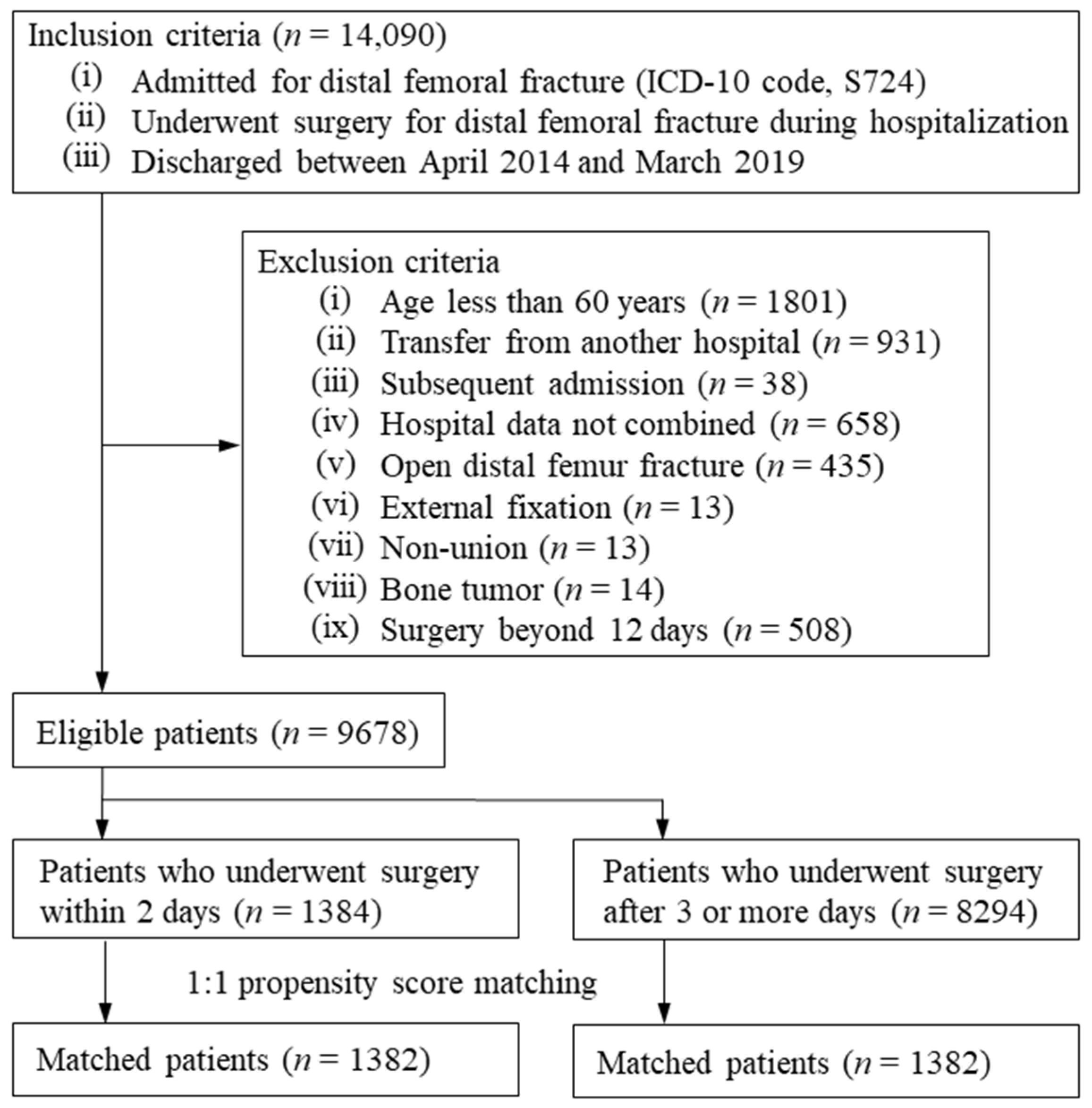
2.2. Patient Selection
2.3. Main Exposure
2.4. Outcomes
2.5. Covariates
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lundin, N.; Huttunen, T.T.; Enocson, A.; Marcano, A.I.; Felländer-Tsai, L.; Berg, H.E. Epidemiology and mortality of pelvic and femur fractures-a nationwide register study of 417,840 fractures in Sweden across 16 years: Diverging trends for potentially lethal fractures. Acta Orthop. 2021, 92, 323–328. [Google Scholar] [CrossRef]
- Jennison, T.; Divekar, M. Geriatric distal femoral fractures: A retrospective study of 30 day mortality. Injury 2019, 50, 444–447. [Google Scholar] [CrossRef] [PubMed]
- Wolf, O.; Mukka, S.; Ekelund, J.; Möller, M.; Hailer, N.P. How deadly is a fracture distal to the hip in the elderly? An observational cohort study of 11,799 femoral fractures in the Swedish Fracture Register. Acta Orthop. 2021, 92, 40–46. [Google Scholar] [CrossRef]
- Carpintero, P.; Caeiro, J.R.; Carpintero, R.; Morales, A.; Silva, S.; Mesa, M. Complications of hip fractures: A review. World J. Orthop. 2014, 5, 402–411. [Google Scholar] [CrossRef]
- Welford, P.; Jones, C.S.; Davies, G.; Kunutsor, S.K.; Costa, M.L.; Sayers, A.; Whitehouse, M.R. The association between surgical fixation of hip fractures within 24 hours and mortality: A systematic review and meta-analysis. Bone Jt. J. 2021, 103, 1176–1186. [Google Scholar] [CrossRef] [PubMed]
- Klestil, T.; Röder, C.; Stotter, C.; Winkler, B.; Nehrer, S.; Lutz, M.; Klerings, I.; Wagner, G.; Gartlehner, G.; Nussbaumer-Streit, B. Impact of timing of surgery in elderly hip fracture patients: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 13933. [Google Scholar] [CrossRef] [Green Version]
- Myers, P.; Laboe, P.; Johnson, K.J.; Fredericks, P.D.; Crichlow, R.J.; Maar, D.C.; Weber, T.G. Patient Mortality in Geriatric Distal Femur Fractures. J. Orthop. Trauma. 2018, 32, 111–115. [Google Scholar] [CrossRef]
- Moloney, G.B.; Pan, T.; Van Eck, C.F.; Patel, D.; Tarkin, I. Geriatric distal femur fracture: Are we underestimating the rate of local and systemic complications? Injury 2016, 47, 1732–1736. [Google Scholar] [CrossRef]
- Streubel, P.N.; Ricci, W.M.; Wong, A.; Gardner, M.J. Mortality after distal femur fractures in elderly patients. Clin. Orthop. Relat. Res. 2011, 469, 1188–1196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nyholm, A.M.; Palm, H.; Kallemose, T.; Troelsen, A.; Gromov, K.; DFDB Collaborators. No association between surgical delay and mortality following distal femoral fractures. A study from the danish fracture database collaborators. Injury 2017, 48, 2833–2837. [Google Scholar] [CrossRef]
- Larsen, P.; Ceccotti, A.A.; Elsoe, R. High mortality following distal femur fractures: A cohort study including three hundred and two distal femur fractures. Int. Orthop. 2020, 44, 173–177. [Google Scholar] [CrossRef]
- Brogan, K.; Akehurst, H.; Bond, E.; Gee, C.; Poole, W.; Shah, N.N.; McChesney, S.; Nicol, S. Delay to surgery does not affect survival following osteoporotic femoral fractures. Injury 2016, 47, 2294–2299. [Google Scholar] [CrossRef] [PubMed]
- Smolle, M.A.; Hörlesberger, N.; Maurer-Ertl, W.; Puchwein, P.; Seibert, F.J.; Leithner, A. Periprosthetic fractures of hip and knee-A morbidity and mortality analysis. Injury 2021, 52, 3483–3488. [Google Scholar] [CrossRef] [PubMed]
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef] [PubMed]
- Yasunaga, H. Real World Data in Japan: Chapter II the Diagnosis Procedure Combination Database. Ann. Clin. Epidemiol. 2019, 1, 76–79. [Google Scholar] [CrossRef]
- Yamana, H.; Moriwaki, M.; Horiguchi, H.; Kodan, M.; Fushimi, K.; Yasunaga, H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J. Epidemiol. 2017, 27, 476–482. [Google Scholar] [CrossRef]
- The Ministry of Health, Labour and Welfare, Japan: Statistical Surveys 2015. Available online: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/open_data.html (accessed on 24 September 2021).
- Sasabuchi, Y.; Matsui, H.; Lefor, A.K.; Fushimi, K.; Yasunaga, H. Timing of surgery for hip fractures in the elderly: A retrospective cohort study. Injury 2018, 49, 1848–1854. [Google Scholar] [CrossRef]
- Pincus, D.; Ravi, B.; Wasserstein, D.; Huang, A.; Paterson, J.M.; Nathens, A.B.; Kreder, H.J.; Jenkinson, R.J.; Wodchis, W.P. Association Between Wait Time and 30-Day Mortality in Adults Undergoing Hip Fracture Surgery. JAMA 2017, 318, 1994–2003. [Google Scholar] [CrossRef] [Green Version]
- Ogawa, T.; Yoshii, T.; Moriwaki, M.; Morishita, S.; Oh, Y.; Miyatake, K.; Nazarian, A.; Shiba, K.; Okawa, A.; Fushimi, K.; et al. Association between Hemiarthroplasty vs Total Hip Arthroplasty and Major Surgical Complications among Patients with Femoral Neck Fracture. J. Clin. Med. 2020, 9, 3203. [Google Scholar] [CrossRef]
- Shigematsu, K.; Nakano, H.; Watanabe, Y. The eye response test alone is sufficient to predict stroke outcome—Reintroduction of Japan Coma Scale: A cohort study. BMJ Open. 2013, 3, e002736. [Google Scholar] [CrossRef] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Wada, T.; Yasunaga, H.; Yamana, H.; Matsui, H.; Matsubara, T.; Fushimi, K.; Nakajima, S. Development and validation of a new ICD-10-based trauma mortality prediction scoring system using a Japanese national inpatient database. Inj. Prev. 2017, 23, 263–267. [Google Scholar] [CrossRef] [PubMed]
- Austin, P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat. Med. 2009, 28, 3083–3107. [Google Scholar] [CrossRef] [Green Version]
- Edwin, L.; Barbara, S. PSMATCH2: Stata Module to Perform Full Mahalanobis and Propensity Score Matching, Common Support Graphing, and Covariate Imbalance Testing; Statistical Software Components: Boston, MA, USA, 2003. [Google Scholar]
- Kammerlander, C.; Riedmüller, P.; Gosch, M.; Zegg, M.; Kammerlander-Knauer, U.; Schmid, R.; Roth, T. Functional outcome and mortality in geriatric distal femoral fractures. Injury 2012, 43, 1096–1101. [Google Scholar] [CrossRef] [PubMed]
- Brox, W.T.; Roberts, K.C.; Taksali, S.; Wright, D.G.; Wixted, J.J.; Tubb, C.C.; Patt, J.C.; Templeton, K.J.; Dickman, E.; Adler, R.A.; et al. The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on Management of Hip Fractures in the Elderly. J. Bone Jt. Surg. Am. 2015, 97, 1196–1199. [Google Scholar] [CrossRef]
- Lévesque, L.E.; Hanley, J.A.; Kezouh, A.; Suissa, S. Problem of immortal time bias in cohort studies: Example using statins for preventing progression of diabetes. BMJ 2010, 340, 907–911. [Google Scholar] [CrossRef] [Green Version]

| Unmatched Cohort | Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Early Surgery (≤2 Days) n = 1384 | Delayed Surgery (≥3 Days) n = 8294 | ASD | Early Surgery (≤2 Days) n = 1382 | Delayed Surgery (≥3 Days) n = 1382 | ASD | |
| Age (years), mean (SD) | 81.3 (9.4) | 81.1 (9.3) | 2.3 | 81.3 (9.4) | 81.4 (9.5) | 0.7 |
| Female sex, n (%) | 1227 (88.7) | 7515 (90.6) | 6.4 | 1225 (88.6) | 1214 (87.8) | 2.6 |
| Body mass index (kg/m2), n (%) | ||||||
| <18.5 | 264 (19.1) | 1495 (18.0) | 2.7 | 264 (19.1) | 262 (19.0) | 0.4 |
| 18.5–24.9 | 718 (51.9) | 4384 (52.9) | 2 | 716 (51.8) | 701 (50.7) | 2.2 |
| 25.0–29.9 | 235 (17.0) | 1478 (17.8) | 2.2 | 235 (17.0) | 252 (18.2) | 3.2 |
| ≥30 | 64 (4.6) | 399 (4.8) | 0.9 | 64 (4.6) | 69 (5.0) | 1.7 |
| Missing | 103 (7.4) | 538 (6.5) | 3.8 | 103 (7.5) | 98 (7.1) | 1.4 |
| Smoking history, n (%) | ||||||
| Non-smoker | 1189 (85.9) | 7080 (85.4) | 1.6 | 1187 (85.9) | 1182 (85.5) | 1.0 |
| Current/past smoker | 96 (6.9) | 602 (7.3) | 1.3 | 96 (6.9) | 99 (7.2) | 0.8 |
| Missing | 99 (7.2) | 612 (7.4) | 0.9 | 99 (7.2) | 101 (7.3) | 0.6 |
| Unconscious at admission, n (%) | 186 (13.4) | 979 (11.8) | 4.9 | 184 (13.3) | 180 (13.0) | 0.9 |
| Home medical care use, n (%) | 107 (7.7) | 693 (8.4) | 2.3 | 107 (7.7) | 106 (7.7) | 0.3 |
| Admission from nursing home, n (%) | 246 (17.8) | 1281 (15.4) | 6.3 | 245 (17.7) | 232 (16.8) | 2.5 |
| Ambulance use, n (%) | 796 (57.5) | 5129 (61.8) | 8.8 | 795 (57.5) | 794 (57.5) | 0.1 |
| Admission on weekend, n (%) | 182 (13.2) | 3444 (41.5) | 67.1 | 182 (13.2) | 183 (13.2) | 0.2 |
| Calendar year, n (%) | ||||||
| 2014 | 282 (20.4) | 1862 (22.4) | 5.1 | 282 (20.4) | 274 (19.8) | 1.4 |
| 2015 | 284 (20.5) | 1750 (21.1) | 1.4 | 284 (20.5) | 311 (22.5) | 4.8 |
| 2016 | 280 (20.2) | 1633 (19.7) | 1.4 | 280 (20.3) | 250 (18.1) | 5.5 |
| 2017 | 278 (20.1) | 1595 (19.2) | 2.2 | 276 (20.0) | 291 (21.1) | 2.7 |
| 2018 | 260 (18.8) | 1454 (17.5) | 3.3 | 260 (18.8) | 256 (18.5) | 0.7 |
| Comorbidities, n (%) | ||||||
| Dementia | ||||||
| Absent | 861 (62.2) | 5239 (63.2) | 2 | 860 (62.2) | 855 (61.9) | 0.7 |
| Mild | 261 (18.9) | 1702 (20.5) | 4.2 | 260 (18.8) | 273 (19.8) | 2.4 |
| Moderate/severe | 262 (18.9) | 1353 (16.3) | 6.9 | 262 (19.0) | 254 (18.4) | 1.5 |
| Myocardial infarction | 4 (0.3) | 80 (1.0) | 8.6 | 4 (0.3) | 5 (0.4) | 0.9 |
| Chronic heart failure | 69 (5.0) | 609 (7.3) | 9.8 | 69 (5.0) | 68 (4.9) | 0.3 |
| Peripheral vascular disease | 11 (0.8) | 98 (1.2) | 3.9 | 11 (0.8) | 14 (1.0) | 2.2 |
| Cerebrovascular disease | 120 (8.7) | 783 (9.4) | 2.7 | 120 (8.7) | 115 (8.3) | 1.3 |
| Chronic pulmonary disease | 39 (2.8) | 286 (3.4) | 3.6 | 39 (2.8) | 38 (2.7) | 0.4 |
| Rheumatic disease | 44 (3.2) | 436 (5.3) | 10.3 | 44 (3.2) | 37 (2.7) | 2.5 |
| Peptic ulcer | 40 (2.9) | 264 (3.2) | 1.7 | 40 (2.9) | 41 (3.0) | 0.4 |
| Mild liver dysfunction | 46 (3.3) | 389 (4.7) | 7 | 46 (3.3) | 40 (2.9) | 2.2 |
| Diabetes mellitus without complications | 225 (16.3) | 1571 (18.9) | 7.1 | 224 (16.2) | 197 (14.3) | 5.1 |
| Diabetes mellitus with complications | 21 (1.5) | 239 (2.9) | 9.3 | 21 (1.5) | 23 (1.7) | 1 |
| Hemiplegia | 14 (1.0) | 57 (0.7) | 3.5 | 14 (1.0) | 15 (1.1) | 0.8 |
| Renal dysfunction | 28 (2.0) | 307 (3.7) | 10.1 | 28 (2.0) | 41 (3.0) | 5.6 |
| Malignancy | 37 (2.7) | 277 (3.3) | 3.9 | 37 (2.7) | 35 (2.5) | 0.8 |
| Severe liver dysfunction | 3 (0.2) | 9 (0.1) | 2.7 | 3 (0.2) | 4 (0.3) | 1.8 |
| Charlson comorbidity index | 0.7 (1.0) | 0.9 (1.1) | 17.9 | 0.7 (1.0) | 0.7 (0.9) | 1.1 |
| Trauma mortality prediction score, mean (SD) | 3.6 (1.5) | 3.5 (1.5) | 4.5 | 3.6 (1.5) | 3.6 (1.7) | 1.1 |
| ICU/HCU at admission, n (%) | 59 (4.3) | 195 (2.4) | 10.7 | 57 (4.1) | 56 (4.1) | 0.4 |
| Periprosthetic fracture, n (%) | 92 (6.6) | 672 (8.1) | 5.6 | 92 (6.7) | 94 (6.8) | 0.6 |
| Operation, n (%) | ||||||
| Treatment with plating | 772 (55.8) | 4813 (58.0) | 4.5 | 772 (55.9) | 799 (57.8) | 3.9 |
| Treatment with nailing | 462 (33.4) | 2684 (32.4) | 2.2 | 460 (33.3) | 429 (31.0) | 4.8 |
| Treatment with arthroplasty | 9 (0.7) | 36 (0.4) | 2.9 | 9 (0.7) | 6 (0.4) | 3 |
| Treatment unknown | 141 (10.2) | 761 (9.2) | 3.4 | 141 (10.2) | 148 (10.7) | 1.7 |
| Academic hospital, n (%) | 219 (15.8) | 1206 (14.5) | 3.6 | 219 (15.8) | 216 (15.6) | 0.6 |
| Teaching hospital, n (%) | 1064 (76.9) | 6298 (75.9) | 2.2 | 1062 (76.8) | 1047 (75.8) | 2.6 |
| Tertiary hospital, n (%) | 447 (32.3) | 2226 (26.8) | 12 | 445 (32.2) | 457 (33.1) | 1.9 |
| Hospital beds, n (%) | ||||||
| <200 | 196 (14.2) | 1307 (15.8) | 4.5 | 196 (14.2) | 202 (14.6) | 1.2 |
| 200–399 | 528 (38.2) | 3335 (40.2) | 4.2 | 527 (38.1) | 532 (38.5) | 0.7 |
| 400–599 | 463 (33.5) | 2398 (28.9) | 9.8 | 462 (33.4) | 458 (33.1) | 0.6 |
| 600–799 | 160 (11.6) | 900 (10.9) | 2.2 | 160 (11.6) | 152 (11.0) | 1.8 |
| >800 | 37 (2.7) | 354 (4.3) | 8.7 | 37 (2.7) | 38 (2.7) | 0.4 |
| Hospital volume, n (%) | 5.0 (2.4) | 4.5 (2.4) | 19.1 | 5.0 (2.4) | 5.0 (2.6) | 1.0 |
| Unmatched Cohort | Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Early Surgery (≤2 Days) n = 1384 | Delayed Surgery (≥3 Days) n = 8294 | Early Surgery (≤2 Days) n = 1382 | Delayed Surgery (≥3 Days) n = 1382 | Risk Difference (95% CI) | p-Value | |
| Primary outcome | ||||||
| 30-day mortality, n (%) | 12 (0.9) | 41 (0.5) | 12 (0.9) | 12 (0.9) | 0.0 (−0.7 to 0.7) | >0.999 |
| Secondary outcomes | ||||||
| In-hospital mortality, n (%) | 21 (1.5) | 106 (1.3) | 21 (1.5) | 21 (1.5) | 0.0 (−0.9 to 0.9) | >0.999 |
| Composite outcome, n (%) | 187 (13.5) | 1383 (16.7) | 186 (13.5) | 237 (17.1) | −3.7 (−6.5 to −0.9) | 0.007 |
| Length of hospital stay (days), mean (SD) | 42 (42) | 53 (36) | 42 (42) | 50 (36) | −8.4 (−11.8 to −5.0) | <0.001 |
| Length of time from surgery to discharge (days), mean (SD) | 41 (42) | 48 (36) | 41 (42) | 45 (36) | −4.5 (−7.9 to −1.0) | 0.011 |
| In-hospital costs (US dollars), mean (SD) | 16,099 (10,721) | 18,844 (10,803) | 16,101 (10,729) | 18,202 (9859) | −2101 (−2991 to −1212) | <0.001 |
| Early Surgery | Delayed Surgery | Risk Difference (95% CI) | p-Value | |
|---|---|---|---|---|
| Admission on weekend | ||||
| 30-day mortality, n (%) | 1/182 (0.5) | 2/183 (1.1) | −0.5 (−2.4 to 1.3) | 0.571 |
| Charlson comorbidity index ≥ 1 | ||||
| 30-day mortality, n (%) | 4/652 (0.6) | 6/670 (0.9) | −0.3 (−1.2 to 0.7) | 0.552 |
| Hospital size < 400 beds | ||||
| 30-day mortality, n (%) | 5/723 (0.7) | 8/734 (1.1) | −0.4 (−1.4 to 0.6) | 0.415 |
| Hospital volume < 4 | ||||
| 30-day mortality, n (%) | 5/548 (0.9) | 5/578 (0.9) | −0.0 (−1.1 to 1.2) | 0.933 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamamoto, N.; Ohbe, H.; Tomita, Y.; Yorifuji, T.; Nakajima, M.; Sasabuchi, Y.; Miyamoto, Y.; Matsui, H.; Noda, T.; Yasunaga, H. Associations between Early Surgery and Postoperative Outcomes in Elderly Patients with Distal Femur Fracture: A Retrospective Cohort Study. J. Clin. Med. 2021, 10, 5800. https://doi.org/10.3390/jcm10245800
Yamamoto N, Ohbe H, Tomita Y, Yorifuji T, Nakajima M, Sasabuchi Y, Miyamoto Y, Matsui H, Noda T, Yasunaga H. Associations between Early Surgery and Postoperative Outcomes in Elderly Patients with Distal Femur Fracture: A Retrospective Cohort Study. Journal of Clinical Medicine. 2021; 10(24):5800. https://doi.org/10.3390/jcm10245800
Chicago/Turabian StyleYamamoto, Norio, Hiroyuki Ohbe, Yosuke Tomita, Takashi Yorifuji, Mikio Nakajima, Yusuke Sasabuchi, Yuki Miyamoto, Hiroki Matsui, Tomoyuki Noda, and Hideo Yasunaga. 2021. "Associations between Early Surgery and Postoperative Outcomes in Elderly Patients with Distal Femur Fracture: A Retrospective Cohort Study" Journal of Clinical Medicine 10, no. 24: 5800. https://doi.org/10.3390/jcm10245800
APA StyleYamamoto, N., Ohbe, H., Tomita, Y., Yorifuji, T., Nakajima, M., Sasabuchi, Y., Miyamoto, Y., Matsui, H., Noda, T., & Yasunaga, H. (2021). Associations between Early Surgery and Postoperative Outcomes in Elderly Patients with Distal Femur Fracture: A Retrospective Cohort Study. Journal of Clinical Medicine, 10(24), 5800. https://doi.org/10.3390/jcm10245800






